Abstract
Background
African Americans are disproportionately burdened by HIV. The African American church is an influential institution with potential to increase reach of HIV prevention interventions in Black communities.
Purpose
This study examined HIV testing rates in African American churches in the Taking It to the Pews pilot project. Using a community-engaged approach, church leaders delivered religiously-tailored HIV education and testing materials/activities (e.g., sermons, brochures/bulletins, testimonials) to church and community members.
Methods
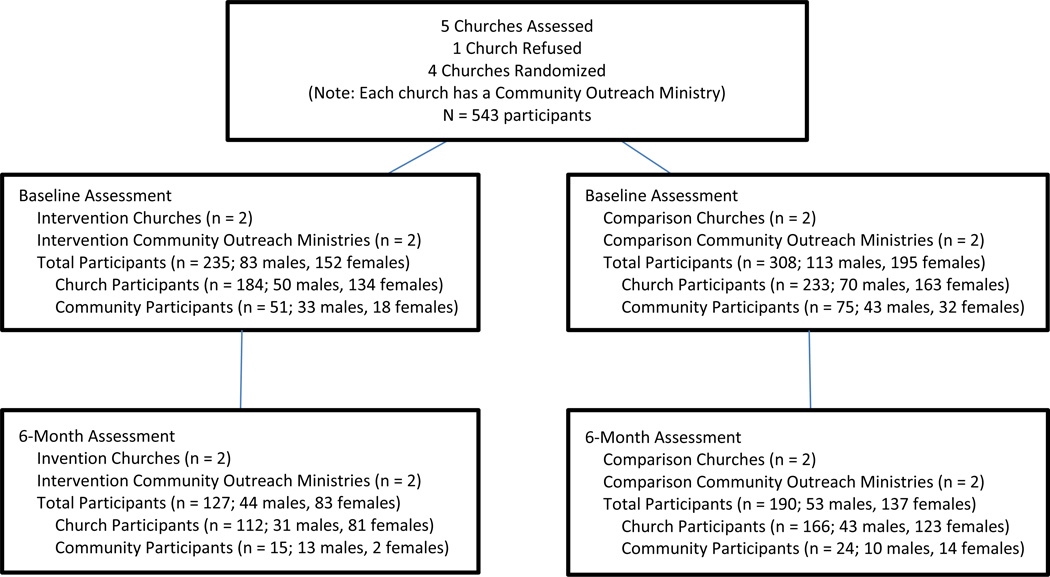
Four African American churches (N=543 participants) located in the Kansas City metropolitan area were randomized to intervention and comparison groups. Receipt of an HIV test was assessed at baseline and 6 months.
Results
Findings indicated intervention participants were 2.2 times more likely to receive an HIV test than comparisons at 6 months. Church leaders delivered about 2 tools per month.
Conclusions
Church-based HIV testing interventions are feasible and have potential to increase HIV testing rates in African American communities.
Keywords: HIV/AIDS, African Americans/Blacks, faith-based, testing/screening, community-based participatory research, access to care
INTRODUCTION
African Americans represent nearly 45% of new HIV cases each year (1–2). Due to delayed HIV diagnosis, African Americans tend to enter HIV treatment at advanced stages and die from AIDS sooner than Whites (1). Goals of the National HIV/AIDS Strategy include having 90% of persons living with HIV be aware of their HIV-positive status and expanding community-level HIV testing approaches in high-risk communities to reduce the spread of HIV (3). Also, CDC guidelines promote universal, routine screening of all individuals aged 13 to 64 in health care settings (4). However, many African Americans have limited access to health care due to a myriad of barriers (e.g., mistrust of providers, lack of insurance). Increasing reach of routine HIV testing to African Americans in medical and community settings will be critical to achieving national goals.
The Black Church is a powerful institution with a history of mobilizing African American communities for social change (5) and has many strengths that could help extend HIV testing to more African Americans. Studies indicate fairly stable church attendance among African Americans (6–8), and most attend church weekly (7). Also, most Black churches have regular weekly services (5, 9); similar religious activities (e.g., testimonials, preaching) (5, 9); support for healthy lifestyles (9–12); and accessible meeting spaces (5, 9, 13). Many also have outreach ministries (e.g., food pantries, utility assistance, recovery programs) that could extend reach of HIV testing to underserved community members who may be at great risk for HIV (9, 11).
Studies suggest many African American faith leaders are willing to provide HIV education and testing for their church/community members (14–17); however, their reported challenges in doing so have included church capacity issues (e.g., lack of HIV training, church-appropriate HIV materials, time, and resources), controversial church issues (e.g., condom use, premarital sex, homophobia), and HIV stigma (18–22). Possibly because of these challenges, only two intervention case studies in Black church settings have reported on HIV testing outcomes (23–24). These studies demonstrated trained church leaders could work with health departments to provide HIV testing in church and community settings and could encourage church and community members to get tested. Yet, longitudinal, multi-arm, church-based HIV testing intervention studies have been nonexistent.
We report on 6-month findings from the Taking It to the Pews pilot intervention study aimed to increase HIV testing rates over 12 months among African American church members and community members served through church outreach ministries from November 2010 to June 2012. Guided by the theory of planned behavior (25), Taking It to the Pews aimed to increase HIV testing intentions and rates by: a) influencing behavioral beliefs on importance of HIV testing using pastoral sermons, responsive readings, risk checklists, and facilitated discussions; b) changing normative beliefs and reducing stigma related to receipt of HIV testing using print and video testimonials, educational games, and the Taking It to the Pews slogan (“Take Someone’s Hand, Get Tested Together”); and c) enhancing behavioral control, access, and empowerment to get tested by providing HIV testing during church services with pastors modeling receipt of HIV testing, HIV screeners describing the testing process to congregants, and the church celebrating reaching goals on number of members tested. Also guided by a social-ecological model (26–28), Taking It to the Pews intervention activities and materials were delivered through individual, social, and community level church outlets. Combined with a community-based participatory research approach (17, 29), these models provided a framework for religiously-tailored intervention development and delivery by church leaders through existing multilevel church outlets to increase HIV testing reach and access. This study tested the multilevel, religiously-tailored Taking It to the Pews intervention (see full description elsewhere) (9, 17, 30) against a non-tailored HIV information comparison group.
METHODS
To address HIV-related church issues noted above, this study’s community-based participatory research approach engaged local health, academic, and African American faith organization partners in the Kansas City metropolitan area who identified: a) HIV testing as the most appropriate church-based prevention strategy instead of condom use promotion and b) need to understand church influence/reach on church members and underserved community members. Faith leaders also determined the intervention should consist of church leaders delivering religiously-tailored HIV education, testing, and compassion messages/activities via a Taking It to the Pews HIV Tool Kit through existing church outlets (9, 17). Additionally, they were engaged in intervention development (e.g., wrote sermon guides and resource cards, developed games), implementation, evaluation, and interpretation of results. They also identified five churches with interests in community health for study recruitment, of which one declined due to other commitments.
Four churches (two intervention and two comparison churches; average of 225 adult members each) were recruited based on size (≥ 150 African American adult church members), having a pastor and two church members (church health liaisons) willing to assist with study delivery, and having an outreach ministry (e.g., food pantries, recovery programs) that served ≥ 50 community members monthly. Participants at these churches were screened on a first-come, first-served basis and deemed eligible if they were aged 18 to 64 and either: a) a church member (attending church ≥ once/month) or b) a community member receiving church outreach ministries (≥ 4 times/year). Participants completed baseline and 6-month surveys after church services and during church outreach activities. They received $10 for completing each survey. Study procedures were approved by the University of Missouri-Kansas City Institutional Review Board and have been reported in detail elsewhere (30).
The research team trained Taking It to the Pews church health liaisons to deliver one to two culturally and religiously-tailored HIV Tool Kit materials/activities through multilevel church outlets including: a) individual-interpersonal contact (self-help HIV testing materials, HIV testing resource cards, phone/text reminders about HIV testing events); b) ministry groups (HIV educational games, printed/video testimonials, facilitated discussions); c) church services (sermons, responsive readings, church bulletins, church HIV stigma video, pastor-modeled receipt of HIV testing, HIV testing events), and d) community outreach ministries (brochures, resource tables, posters). Comparison churches’ health liaisons were trained to deliver non-tailored tools (HIV brochures and testing event announcements). Researchers trained church health liaisons on how to coordinate their churches’ HIV testing events with local health agencies. At six months, all churches had coordinated one HIV testing event during church services and one during outreach activities.
The outcome measure was receipt of an HIV test (last 6 months). Analyses of this measure was conducted using a logistic regression model (IBM SPSS version 20 and R version 2.12.1) with experimental condition as fixed-effect terms; churches nested in experimental condition were included as random effect terms. Due to the significant attrition of participants across groups, the outcome was examined using simple imputation, which yielded results similar to using complete case analysis. Therefore, results are reported from complete case analysis with participants who completed surveys at baseline and six months.
RESULTS
Participants (N = 543; 417 church and 126 community members; mean age of 42.3 [SD = 13.5]) were mostly female, single, Baptist, and highly religious (85% prayed daily, 79% attended church weekly). Overall, 74% reported receipt of an HIV test at some point in their lifetime.
Among baseline participants, 58% (n = 317) completed 6-month follow-up surveys. Five of these participants did not respond to baseline and last 6 months HIV testing items; therefore, the 6-month analysis included responses from 312 participants. Intervention and comparison group baseline characteristics were similar, except for sexual identity, as shown in Table 1. There were no significant differences between 6-month completers and noncompleters on baseline data for receipt of HIV testing and exposure measures. Differential attrition occurred similarly across churches at 6 months on demographic measures; noncompleters tended to be younger, male, have less education and income, and be community members.
Table 1.
Baseline Participant Demographics and Lifetime HIV Testing by Experimental Group; Taking It to the Pews
| Survey measures | Intervention Group | Comparison Group | |||||
|---|---|---|---|---|---|---|---|
| Church Members |
Community Members |
Overall | Church Members |
Community Members |
Overall | p | |
| Age | .27 | ||||||
| 18–29 | 25.1% (46) | 23.1% (12) | 24.7% (58) | 22.6% (54) | 17.3% (13) | 21.3% (67) | |
| 30–49 | 39.3% (72) | 36.5% (19) | 38.7% (91) | 37.7% (90) | 41.3% (31) | 38.5% (121) | |
| 50–64 | 34.4% (63) | 40.4% (21) | 35.7% (84) | 36.8% (88) | 41.3% (31) | 37.9% (119) | |
| Gender | .78 | ||||||
| Male | 27.3% (50) | 63.5% (33) | 35.3% (83) | 29.3% (70) | 57.3% (43) | 36.0% (113) | |
| Female | 72.7% (133) | 36.5% (19) | 64.7% (152) | 68.2% (163) | 42.7% (32) | 62.1% (195) | |
| Sexual identity | .01 | ||||||
| Heterosexual | 84.7% (155) | 65.4% (34) | 80.4% (189) | 89.5% (214) | 80% (60) | 87.3% (274) | |
| Homosexual | 1.1% (2) | -- | 0.9% (2) | 2.1% (5) | 4% (3) | 2.5% (8) | |
| Bisexual | -- | 7.7% (4) | 1.7% (4) | 0.4% (1) | 2.7% (2) | 1% (3) | |
| Choose not to answer |
11.4% (21) | 25.0% (13) | 14.5% (34) | 3.7% (9) | 12% (9) | 5.7% (18) | |
| Marital status | .73 | ||||||
| Single/separated/ divorced/widowed |
56.8% (104) | 82.7% (43) | 62.6% (147) | 52.7% (126) | 81.3% (61) | 59.6% (187) | |
| Co-habiting/married | 42.7% (78) | 17.3% (9) | 37.0% (87) | 44.8% (107) | 17.4% (13) | 38.3% (120) | |
| Monthly income | .10 | ||||||
| $0–$1,000 | 9.8% (18) | 50.0% (26) | 18.7% (44) | 8.8% (21) | 46.7% (35) | 17.8% (56) | |
| $1,001–$2,000 | 14.2% (26) | 5.8% (30) | 12.3% (29) | 18.4% (44) | 18.7% (14) | 18.5% (58) | |
| $2,001–$2,500 | 7.7% (14) | 1.9% (1) | 6.4% (15) | 13.0% (31) | 5.3% (4) | 11.1% (35) | |
| $2,501–$3,000 | 14.8% (27) | 7.7% (4) | 13.2% (31) | 11.7% (28) | 4.0% (3) | 9.9% (31) | |
| More than $3,000 | 42.6% (78) | 13.5% (7) | 36.2% (85) | 37.7% (90) | 8.0% (6) | 30.6% (96) | |
| Don’t know | 9.8% (18) | 21.2% (11) | 12.3% (29) | 7.9% (19) | 14.7% (11) | 9.6% (30) | |
| Ever tested for HIV | .12 | ||||||
| Yes | 71.2% (131) | 74.5% (38) | 71.9% (169) | 72.8% (174) | 86.7% (65) | 76.1% (239) | |
| No | 27.7% (51) | 23.5% (12) | 26.8% (63) | 24.7% (59) | 9.3% (7) | 21% (66) | |
The proportion of participants reporting receipt of an HIV test (last 6 months) increased significantly in both intervention and comparison groups at 6-month follow-up, as shown in Table 2. Yet, the odds of intervention participants reporting receipt of an HIV test at the 6-month follow-up were 2.2 times greater than for comparison participants (p = .06). When adjusted for baseline reported receipt of an HIV test (last 6 months), intervention participants were 2.6 times more likely to report receipt of an HIV test than comparisons. Among participants reporting non-receipt of an HIV test (last 6 months) at baseline, receipt of an HIV test at 6-month follow-up was 3.3 times more likely for intervention participants than comparisons. Additionally, at 6-month follow-up, a larger proportion of intervention group church members reported receipt of an HIV test than comparison group church members (46% and 26%, respectively), and intervention community members reported similar rates of HIV testing as comparison community members (53% vs 50%, respectively). However, a factorial model (i.e., intervention/comparison × church member/community member) examining the differential impact on church versus community members failed to reach statistical significance.
Table 2.
HIV Testing (last 6 months) at Baseline and 6-month Follow-up by Experimental Group; Taking It to the Pews
| Treatment Group |
HIV Testing Baseline |
HIV Testing 6-month F/U |
p | OR (95% CI) |
p | AORa (95% CI) |
p | ORb (95% CI) |
p |
|---|---|---|---|---|---|---|---|---|---|
| Comparison | 19% | 28% | .012 | 2.2 (0.97,5.10) | .06 | 2.6 (1.2, 6.1) | .000 | 3.3 (1.6, 7.1) | .001 |
| Intervention | 23% | 47% | .001 |
Note. AOR = adjusted odds ratio; CI = confidence interval; F/U = follow-up
Adjusted for reported receipt of an HIV test (last 6 months) at baseline, gender, and sexual identity
Inclusive of only participants with reported non-receipt of an HIV test (last 6 months) at baseline
Intervention and comparison church health liaisons delivered about two tools per month. Intervention church health liaisons reports of tools delivered most frequently matched intervention church participants frequently reported exposure to tools (sermons, church bulletins, brochures, posters, resource tables). Intervention church members reported exposure to an average of 7 tools; whereas, intervention community members reported exposure to an average of 4 tools, mostly brochures, posters, and resource tables.
DISCUSSION
This study, guided by a community-based participatory research approach, demonstrated that church leaders can deliver HIV testing interventions and increase HIV screening rates among African American church populations. Also, findings indicated the Taking It to the Pews intervention was markedly more impactful on participants who reported that they had not received an HIV test in the last 6 months at baseline.
This study highlights several practice and research implications related to expanding reach and capacity of church-based HIV testing services. Regarding practice, the current study achieved significant increases in receipt of church-based HIV testing in intervention and comparison groups. This suggests convenient access to testing in influential settings, such as churches, is critical in considering reach of HIV testing services. Also, although community members’ receipt of an HIV test (around 50%) was similar across intervention and comparison groups at 6 months, their HIV testing rates overall were higher than church members, suggesting access to church-based HIV testing for community members during outreach ministry events could greatly benefit community populations. However, further studies are needed on how to increase community members’ exposure to church-based HIV testing intervention strategies and, most importantly, how to increase exposure to marginalized African American populations most at risk for HIV, including men who have sex with men. Additionally, church leaders feasibly delivered two tools per month, suggesting that use of church-tailored HIV tool kit materials/activities implemented through existing multilevel church outlets may be a scalable strategy to increase reach of church-based HIV testing services. Regarding reach of the study, almost 50% of participating churches’ adult membership (within CDC’s recommended 18 to 64 age range for routine testing) (4) was recruited, and 25% of the sample were community members, demonstrating recruitment possibilities for church-based HIV testing studies.
Yet, several limitations exist. This pilot study included a small number of participating churches, which likely limited the analysis on differential intervention effects on church and community members. Also, due to use of first-come, first-served recruitment strategies, participant selection bias was possible with participants most ready for HIV testing. Additionally, our participants were largely made up of African American middle-aged women. This is not surprising, since other African American church studies have had an overrepresentation of middle-aged women (13, 17, 27, 28), and women tend to attend church more frequently than men (6, 7). Yet, there is certainly a need for future research on church-based HIV testing among younger African American heterosexual men and men who have sex with men, groups that are of greatest risk for HIV. Furthermore, the study incurred substantial participant attrition at 6 months, especially among participants who tended to be younger, male, and less educated/lower income. Most of these characteristics (male, less educated, lower income) were highly representative of our community participants, who at times were difficult to contact due to their transience and irregular contact with participating churches. Further research is needed on strategies to retain church-affiliated populations, especially community members. Also, further examination is needed regarding which intervention materials and strategies may be most salient in cost-effectively increasing rates of HIV testing in church-community settings. Future studies with an appropriately powered clustered, randomized design will further assist in understanding feasibility and impact of a scalable, church-based Taking It to the Pews intervention on HIV testing rates on African American church members and the community members they serve.
Figure 1.
Flow of Churches and Participants through Completion of 6-Month Assessment; Taking It to the Pews
Contributor Information
Jannette Berkley-Patton, School of Medicine, Biomedical and Health Informatics Department, University of Missouri-Kansas City, Kansas City, MO.
Carole Bowe Thompson, School of Medicine, Biomedical and Health Informatics Department, University of Missouri-Kansas City, Kansas City, MO.
Erin Moore, Psychology Department, Stetson University, DeLand, FL.
Starlyn Hawes, Center for Healthcare Improvement for Addictions, Mental Illness, and Medically Vulnerable Populations, University of Washington Medical Center, Seattle, Washington.
Stephen Simon, School of Medicine, Department of Biomedical and Health Informatics, University of Missouri-Kansas City, Kansas City, MO.
Kathy Goggin, Health Services and Outcomes Research, Children's Mercy Hospitals and Clinics, Kansas City, MO.
David Martinez, Clinical Psychology Training Consortium, Brown University Medical School, Providence, RI.
Marcie Berman, School of Medicine, Biomedical and Health Informatics Department, University of Missouri-Kansas City, Kansas City, MO.
Alexandria Booker, School of Medicine, Biomedical and Health Informatics Department, University of Missouri-Kanas City, Kansas City, MO.
REFERENCES
- 1.Centers for Disease Control and Prevention. [Accessibility verified October 22, 2015];HIV Surveillance Report, 2013. 2015 25 http://www.cdc.gov/hiv/library/reports/surveillance. [Google Scholar]
- 2.Centers for Disease Control and Prevention. [Accessibility verified October 22, 2015];Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV Surveillance Supplemental Report. 2012 17(4) Available at http://www.cdc.gov/hiv/topics/surveillance/resources/reports/#supplemental. [Google Scholar]
- 3.The White House Office of National AIDS Policy. [Accessibility verified October 22, 2015];National HIV/AIDS strategy for the United States. Available at http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf.
- 4.Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55(RR-14) [PubMed] [Google Scholar]
- 5.Lincoln CE, Mamiya LH. The Black Church and the African American Experience. Durham, NC: Duke University Press; 1990. [Google Scholar]
- 6.Barna Group. [Accessibility verified April 20, 2015];New statistics on church attendance and avoidance. Available at https://www.barna.org/barna-update/congregations/45-new-statistics-on-church-attendance-and-avoidance.
- 7.Pew Research Center. Pew Forum on Religion and Public Life. A religious portrait of African Americans, U.S. Religious Landscape Survey. Washington, DC: [Accessibility verified October 10, 2014]. Available at http://www.pewforum.org/2009/01/30/a-religious-portrait-of-african-americans. [Google Scholar]
- 8.Pew Research Center. America’s Changing Religious Landscape. Washington, DC: 2015. May, [Accessibility verified May 20, 2015]. Available at http://www.pewforum.org/files/2015/05/RLS-05-08-full-report.pdf. [Google Scholar]
- 9.Berkley-Patton J, Martinez D, Bowe-Thompson C, et al. Examining church capacity to develop and disseminate a religiously-appropriate HIV tool kit with African American churches. J Urban Health. 2013;90:482–499. doi: 10.1007/s11524-012-9740-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davis DT, Bustamante A, Brown CP, et al. The urban church and cancer control: A source of social influence in minority communities. Public Health Rep. 1994;109:500–506. [PMC free article] [PubMed] [Google Scholar]
- 11.Derose KP, Mendel PJ, Palar K, et al. Religious congregations’ involvement in HIV: A case study approach. AIDS Behav. 2011;15:1220–1232. doi: 10.1007/s10461-010-9827-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor RJ, Chatters LM, Levin J. Religion in the lives of African Americans: Social, psychological, and health perspectives. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 13.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: Evidence and lessons learned. Ann Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- 14.Smith J, Simmons E, Mayer KH. HIV/AIDS and the Black Church: What are the barriers to prevention services? J Natl Med Assoc. 2005;97:1682–1685. [PMC free article] [PubMed] [Google Scholar]
- 15.Derose KP, Mendel PJ, Palar K, Kanouse DE, Bluthenal RN, Castaneda LW, et al. Religious congregations’ involvement in HIV: A case study approach. AIDS Behav. 2011;15(6):1220–1232. doi: 10.1007/s10461-010-9827-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayers JR. The quagmire of HIV/AIDS related issues which haunt the church. J Pastoral Care. 1995;49:201–210. doi: 10.1177/002234099504900209. [DOI] [PubMed] [Google Scholar]
- 17.Berkley-Patton J, Bowe-Thompson C, Bradley-Ewing A, et al. Taking It to the Pews: a CBPR-guided HIV awareness and screening project with Black Churches. AIDS Educ Prev. 2010;22:218–237. doi: 10.1521/aeap.2010.22.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart JM. Pastor and lay leader perceptions of barriers and supports to HIV ministry maintenance in an African American church. J Relig Health. 2014;53(2):317–325. doi: 10.1007/s10943-012-9627-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pryor JB, Gaddist B, Johnson-Arnold L. Stigma as a barrier to HIV-related activities among African-American churches in South Carolina. J Prev Interven in Comm. 2015;43:223–234. doi: 10.1080/10852352.2014.973279. [DOI] [PubMed] [Google Scholar]
- 20.Fullilove MT, Fullilove RE. Stigma as an obstacle to AIDS action: The case of the African American community. Am Behav Scientist. 1999;42:1117–1129. [Google Scholar]
- 21.Buseh AG, Stevens PE, McManus P, Addison J, Morgan S, Millon-Underwood S. Challenges and opportunities for HIV prevention and care: Insights from focus groups of HIV-infected African American men. J Assoc of Nurses in AIDS Care. 2006;17:3–15. doi: 10.1016/j.jana.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 22.Berkley-Patton J, Hawes S, Moore E, et al. Examining facilitators and barriers to HIV testing in African American churches using a community-based participatory research approach. Oral presentation at the 33rd Annual Meeting & Scientific Sessions of the Society of Behavioral Medicine; Apr 2012; New Orleans, LA. [Google Scholar]
- 23.Agate L, Cato-Watson D, Mullins JM, et al. Churches United to Stop HIV (CUSH): A faith-based HIV prevention initiative. J Natl Med Assoc. 2005;97:60S–63S. [PMC free article] [PubMed] [Google Scholar]
- 24.MacMaster SA, Jones JL, Rasch R, Crawford SL, Thompson S, Sanders E. Evaluation of a faith-based culturally relevant program for African American substance users at risk for HIV in the Southern United States. Res on Soc Work Pract. 2007;17:229–238. doi: 10.1093/hsw/32.2.151. [DOI] [PubMed] [Google Scholar]
- 25.Ajzen I. The Theory of Planned Behavior. Org Beh Hum Decision Processes. 1991;50:179–211. [Google Scholar]
- 26.Bronfenbrenner U. The Ecology of Human Development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 27.Campbell MK, Demark-Wahnefried W, Symons M, et al. Fruit and vegetable consumption and prevention of cancer: The Black Churches United for Better Health Project. Am J Public Health. 1999;89:1390–1396. doi: 10.2105/ajph.89.9.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Resnicow K, Campbell M, Carr C, et al. Body and Soul: A dietary intervention conducted through African-American churches. Am J Prev Med. 2004;27:97–105. doi: 10.1016/j.amepre.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Israel BA, Eng E, Schulz AJ, Parker EA. Introduction to methods in community-based participatory research for health. In: Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods in Community-based Participatory Research for Health. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- 30.Berkley-Patton J, Moore E, Berman M, et al. Assessment of HIV stigma in a U.S. faith-based HIV education and screening intervention. J of the Int AIDS Soc. 2013;16(Suppl 2) doi: 10.7448/IAS.16.3.18644. 1 8644. [DOI] [PMC free article] [PubMed] [Google Scholar]