Abstract
Background
Thousands of neurosurgical emergencies are transferred yearly to tertiary care facilities to assume a higher level of care. Several studies have examined how neurosurgical transfers influence patient outcomes, but characteristics of potentially avoidable transfers have yet to be investigated.
Objective
To identify whether potentially avoidable transfers represent a significant portion of transfers to a tertiary neurosurgical facility.
Methods
In this cohort study, we evaluated 916 neurosurgical patients transferred to a tertiary care facility over a 2-year period. Transfers were classified as potentially avoidable when no neurosurgical diagnostic test, intervention, or intensive monitoring was deemed necessary (n=180). The remaining transfers were classified as justifiable (n=736). The main outcomes and measures were age, sex, diagnosis, insurance status, intervention, distance of transfer, length of hospital and intensive care unit (ICU) stay, mortality, discharge disposition, and cost.
Results
Nearly 20% of transfers were identified as being potentially avoidable. While some of these patients had suffered devastating, irrecoverable neurologic insults, many had innocuous conditions that did not require transfer to a higher level of care. Justifiable transfers tend to involve patients with non-traumatic intracranial hemorrhage and cranial neoplasm. Both groups were admitted to the intensive care unit at the same rate (approximately 70% of patients). Finally, the direct transportation cost of potentially avoidable transfers was $1.46 million over 2 years.
Conclusion
This study identified frequency and expense of potentially avoidable transfers. There is a need for closer examination of the clinical and financial implications of potentially avoidable transfers.
Keywords: healthcare utilization, medical economics, patient transfer
In the event of a perceived emergency, patients typically present to their local emergency department or acute care facility. Neurosurgical emergencies requiring a higher level of care or medical expertise can be transferred under the protection of the Emergency Medical Treatment and Active Labor Act (EMTALA) to a tertiary care facility with an intensive care unit (ICU) and a neurosurgeon available for potential intervention.1,2 As such, neurosurgery services at tertiary care facilities receive a high volume of patients from outside hospital transfers.3–5 Potential drawbacks to transferring neurosurgical patients include cost, disruptions in care, and displacement of patients and families from home, sometimes hundreds of miles away.
Several studies have examined how neurosurgical transfers influence patient outcomes, with transfer distance and delay in neurosurgical intervention associated with worse outcomes.6,7 However, to our knowledge, investigations to identify a group of potentially avoidable transfers have yet to be performed. The aims of this study were to describe patterns of neurosurgical transfers to a tertiary care facility, identify potentially avoidable transfers, and assess the direct transportation costs of potentially avoidable transfers. We postulated that potentially avoidable transfers would form 2 distinct groups; namely, those patients with devastating and irreversible neurologic injury, and those with innocuous conditions not requiring higher levels of care. We discuss a potential framework that assures safe local care while avoiding transfers to a higher acuity facility.
METHODS
Patient Selection and Data Collection
A query of hospital billing records performed in February 2015 returned all patients admitted to the neurosurgical service at the University of Alabama at Birmingham (UAB) over a 2-year period, from July 1, 2012, through July 1, 2014. Of the 5531 patients admitted to the neurosurgery service over 2 years, 943 patients were coded as being transferred from an outside facility; examination of the individual electronic medical records confirmed 916 transferred patients. There were no missing data. Data collected for each transferred patient included: patient demographics (age, gender, and diagnosis-related group), surgical procedure(s), insurance status, hospital length of stay, intensive care unit length of stay, admitting floor or unit, discharge disposition, and mortality. Clinical status on admission was also reviewed. Additionally, the location of the outside hospital was found in the electronic medical record (EMR), and the shortest route (in miles) to UAB Hospital was calculated using Google Maps. If the transferring hospital was not identified, the nearest local hospital or the patient’s home address was considered to be the transferring location. Patients were transferred from 108 different hospitals. Transportation via air versus ground was not reliably recorded in the EMR; thus, all transfers were assumed to be via ground ambulance.
In dichotomizing the transfers as requiring tertiary care or not, the overall goal was to identify those patients who could have been sufficiently and safely triaged and managed at the originating facility. Initial screening for justifiable transfers was performed by first identifying all patients who underwent any neurosurgical or invasive procedure during admission. Patients who underwent diagnostic testing that is not widely available (eg, long-term electroencephalography, CT myelogram) were also classified as justifiable transfers. The EMR was reviewed for each remaining transfer. Potentially avoidable transfers were identified as those with patients who were discharged without any further diagnostic or therapeutic intervention, who were dead on arrival, or for whom comfort care measures were instituted immediately on arrival. Clinical status of patients was also considered in determination of whether the transfer was potentially avoidable, though resources of the originating site were not. It was assumed that the patient’s condition on arrival to our hospital was similar to their condition at the originating site, unless otherwise noted in the medical record. Patients who required specialized medical or surgical intervention, though not neurosurgical intervention, were also considered as justifiable transfers (eg, patient with clinically insignificant traumatic subarachnoid hemorrhage and multiple other traumatic injuries). The outcomes of interest included length of hospital and ICU stay, mortality, discharge disposition, insurance status, and cost. The exposure of interest was the potential avoidability of transfer. The following predictors were evaluated: age, sex, diagnosis (DRG code), insurance status, intervention, and distance of transfer. The follow-up period spanned the patient’s hospitalization and ended with hospital discharge; as such, there were no missing data.
Within this cohort study, we additionally performed a retrospective case-control analysis to identify factors associated with potentially avoidable transfers. For these analyses, cases were defined as potentially avoidable transfers and controls were defined as transfers requiring tertiary care (“justifiable transfers”). Predictors evaluated were age, sex, diagnosis, insurance status, intervention, and distance of transfer.
Bias
As this is a retrospective study, the following steps were taken to mitigate the potential for bias. The individual(s) collecting outcome data were blinded to potential avoidability of transfer. Potential avoidability of transfer was determined prior to consideration of transfer distance. A single population—specifically, all patients transferred to the neurosurgery service at UAB Hospital during the specified time period—was used to select both cohorts, so as to decrease selection bias. To lessen recall bias, none of the variables analyzed in this study relied on the patient’s or clinician’s memory; all data was derived expressly from medical and billing records. Two complete academic years were selected as the study period to minimize any bias introduced from seasonal variation in transfer patterns, trainee experience, and pathology.
Statistics
We performed analyses of our data using univariate statistical methods. To perform parametric and non-parametric univariate statistical analyses, we used 2-tailed unpaired t tests and Wilcoxon rank-sum tests, respectively. To examine the proportional differences of patient outcomes (number of patients with neurosurgical intervention and discharge status) as a function of length of stay, we used the chi-square test, or Fisher’s exact test when the assumptions for the chi-square test were not tenable. To compare proportional differences of gender, mortality, and percent of patients admitted to the ICU, we used Fisher’s exact test. To compare proportional differences of medical insurance type, admission reasons, and subcategories of admission reasons, we used chi-square tests. To compare ages by admission categories, we used two-way ANOVAs correcting for multiple comparisons with Bonferroni’s multiple comparison tests. To compare each hospital’s rate of potentially avoidable transfers to the entire cohort’s rate (19.7%), we used one-group test for binomial proportion. Odds ratios were calculated for each admission reason, using incidence of each admission reason for both justifiable transfers and potentially avoidable transfers. The odds ratio was calculated as the odds of the transfer being potentially avoidable. These statistical analyses were performed using GraphPad Prism (Version 6.02, La Jolla, California) and IBM SPSS Statistics (Version 22, Armonk, New York).
University of Alabama at Birmingham Institutional Review Board approval was obtained (IRB X141021004). This manuscript was created following the STROBE checklist for cohort studies.
RESULTS
Description of Transferred Patients
A total of 5531 patients were admitted to the neurosurgery service during the study period, with 916 patients transferred from outside hospitals. Transfers represent 16.6% of all patients admitted to the neurosurgery service. All 916 patients were included in the final analyses. Table 1 shows the patient demographics. Neurosurgical intervention was performed in 84.2% of transferred patients with a median hospital stay of 7 days (IQR 25–75: 4–13). The 15.8% of patients who did not have neurosurgical intervention had significantly shorter hospital stays (median = 2 days, IQR 25–75: 1–3; P < .0001 by Wilcoxon rank-sum test) and comprised a significantly smaller proportion of patients who stayed in the hospital longer than 3 days. Those without neurosurgical intervention with a hospital stay of 1 day were most commonly admitted for trauma (33.8%), neoplasm (12.3%), non-traumatic intracranial hemorrhage (10.8%), and spinal fractures (10.8%).
Table 1.
Demographic Data of Transfer Patients
| Total (N = 916) | |
|---|---|
| Male, (%) | 427 (46.6%) |
| Age | 57 ± 17.1 (2–97) |
| Mortality, (%) | 86 (9.4%) |
| Admission bed type, (%) | |
| ICU | 668 (72.9%) |
| Floor | 238 (26.0%) |
| Surgery | 10 (1.1%) |
| Distance Transferred (mi.) | 86 ± 89.9 (0–1970) |
| Admission reason, (%) | |
| Non-traumatic intracranial hemorrhage | 357 (39.0%) |
| Neoplasm | 145 (15.8%) |
| Trauma | 109 (11.9%) |
| Non-traumatic spine | 90 (9.8%) |
| Infection | 40 (4.4%) |
| Ischemic stroke | 31 (3.4%) |
| Unruptured aneurysm | 29 (3.2%) |
| Shunt-related | 20 (2.2%) |
| Hydrocephalus | 17 (1.9%) |
| Headache | 13 (1.4%) |
| Other | 65 (7.1%) |
| Insurance type, (%) | |
| Uninsured/Charity care | 106 (11.6%) |
| Private | 258 (28.2%) |
| Medicare | 409 (44.7%) |
| Medicaid | 97 (10.6%) |
| VA | 22 (2.4%) |
| Other | 24 (2.6%) |
Age and distance transferred presented as mean ± standard deviation with range of values.
Other: cerebrovascular NOS, cerebral edema NOS, altered mental status, sepsis, convulsions/seizures, multiple sclerosis, trigeminal neuralgia, syncope, dizziness, other brain conditions
NOS ICU = intensive care unit; NOS = not otherwise specified
Twenty-nine of the 86 patients who died did so on the first hospital day. Several of these patients were dead on arrival. Cause of death was mostly related to non-traumatic intracranial hemorrhage (68.1%) followed by trauma (8.8%), stroke (8.8%), neoplasm (6.6%), unruptured aneurysm (2.2%; death due to aneurysm rupture in one and hydrocephalus from giant aneurysm mass effect in the other), non-traumatic spine-related (2.2%), and infection (1.1%).
Potentially Avoidable Transfers
The transferred patients were dichotomized as justifiable transfers (JT; n=736) and potentially avoidable transfers (PAT; n=180). PATs comprised 19.7% of all transfers. Mortality was significantly greater (21.1% vs 6.5%; P < .0001), and the median length of stay was significantly shorter (1 vs 7 days; P < .0001) in the PAT group (Table 2). The 2 groups were admitted to ICUs at a similarly high rate (70.0% vs 73.7%, P = .35), but the PAT group had a significantly shorter median length of ICU stay (1 vs 4 days; P < .0001; Table 2). Potentially avoidable transfers were least likely to occur on Thursdays (9.5%) and most likely to occur on Saturdays (20.8%) and Sundays (21.0%). However, there was no statistically significant difference in rate of PATs by day of week on chi-square analysis (P = .30).
Table 2.
Comparison of Cohorts
| Justifiable Transfers | Potentially Avoidable | P-value | |
|---|---|---|---|
| No. | 736 | 180 | |
| Age in years | 55.5 ± 16.5 | 61.3 ± 19.1 | < 0.0001 |
| Males, % | 46.7 | 46.1 | 0.93 |
| Mortality, % | 6.5 (N=48) | 21.1 (N=38) | < 0.0001 |
| Insurance types, % | 0.045 | ||
| Uninsured/Charity care | 11.8 (N=87) | 10.6 (N=19) | 0.70 |
| Private | 29.6 (N=218) | 22.2 (N=40) | 0.052 |
| Medicare | 42.0 (N=309) | 55.6 (N=100) | 0.001 |
| Medicaid | 11.1 (N=82) | 8.3 (N=15) | 0.34 |
| VA | 2.6 (N=19) | 1.7 (N=3) | 0.60 |
| Other | 2.9 (N=21) | 1.7 (N=3) | 0.60 |
| Hospital LOS in days (IQR) | 7 (4–14) | 1 (1–3) | < 0.0001 |
| Admitted to ICU, % | 73.7 | 70.0 | 0.35 |
| ICU LOS in days (IQR) | 4 (2–9) | 1 (0–1) | < 0.0001 |
| Transfer distance in miles (IQR) | 70 (46–110) | 66 (46–108.8) | 0.56 |
Age represented as mean ± standard deviation. Hospital LOS, ICU LOS, and transfer distance represented as median with IQR.
ICU = intensive care unit; LOS = length of stay; IQR = interquartile range
The medical insurance type was significantly different between the 2 groups (Table 2), though this may be an effect of differences in patient age. PATs were more likely to have Medicare (odds ratio 1.73; 95% CI: 1.24–2.40; P < .01) and less likely to have private insurance (odds ratio 0.68; 95% CI: 0.46–0.99; P = .05). There was no difference between JTs and PATs in rates of being uninsured (P = 0.70), Medicaid (P = .34), and Veterans Affairs medical care (P = .60).
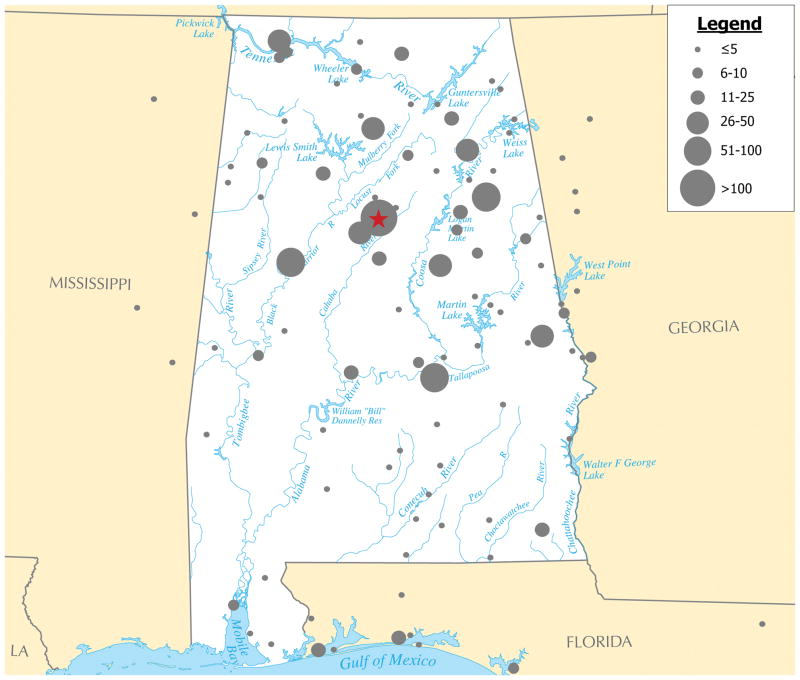
Patients were transferred from various originating hospitals across the state of Alabama, eastern Mississippi, western Georgia, and northwest Florida (Figure 1). The median transfer distance for the PAT group was 66 miles (IQR: 46–109), while it was 70 miles (IQR: 46–110) for the JT group (P = .56; Table 2). Of the various originating hospitals that transferred at least 10 patients, there was a significant difference of transfer rates of PATs across the various hospitals (P < .0001 by chi-square). Compared to the entire cohort’s rate of PATs at 19.7%, some hospitals’ transfers contained a significantly higher proportion of PATs than others (range 0–52.6%).
Figure 1.
Patients transferred to a tertiary care neurosurgery service were from various originating hospitals. Illustration shows approximate patient number and geographical distribution of originating hospitals across the state of Alabama (in white), eastern Mississippi, western Georgia, and northwest Florida. The red star represents the tertiary care neurosurgery service at the University of Alabama at Birmingham, and grey circles represent each area’s originating hospitals, with the approximate number of patients reflected by increasing circle diameters (see legend).
Next, we compared patient demographics to determine if there were characteristics that could help identify potentially avoidable transfers. There was no gender difference between groups (P = 0.93), but the PAT group was significantly older (61.3 vs 55.5 years; P < .0001; Table 2). Because we surmised that PATs formed 2 distinct groups (those with innocuous pathology and the moribund), we separated the PAT group into those patients who expired and those who survived to discharge. PATs who expired were significantly more likely to have non-traumatic intracranial hemorrhage (OR 7.71, 95% CI: 3.20–18.77; Table 3). As shown in Table 3, PATs who survived were significantly more likely to be transferred for trauma (OR 7.22, 95% CI: 4.64–11.24) and headache (OR 4.60, 95% CI: 1.52–13.89) and significantly less likely to be transferred for non-traumatic intracranial hemorrhage (OR 0.31, 95% CI: 0.20–0.49). Additionally, surviving PATs with non-traumatic intracranial hemorrhages (specifically, subdural hematoma and epidural hematoma) and traumatic skull fractures were significantly older than those of JTs (P < .05, Table 4).
Table 3.
Comparison of Admission Reason Between Cohorts
| Justifiable Transfers | Potentially Avoidable Transfers | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N=736 | All N=180 | Living N=142 | Expired N=38 | ||||
|
| |||||||
| N | N | OR (95% CI) | N | OR (95% CI) | N | OR (95% CI) | |
| Admission reason | |||||||
| Non-traumatic Hemorrhage † | 300 (40.8%) | 57 (31.7%) | 0.67 (0.48–0.95) | 25 (17.6%) | 0.31 (0.20–0.49) | 32 (22.5%) | 7.71 (3.20–18.77) |
| ICH | 70 (9.5%) | 27 (15.0%) | 13 (9.2%) | 14 (36.8%) | |||
| SAH | 182 (24.7%) | 16 (8.9%) | 3 (2.1%) | 13 (34.2%) | |||
| SDH | 44 (6.0%) | 14 (7.8%) | 9 (6.3%) | 5 (13.2%) | |||
| EDH | 3 (0.4%) | ||||||
| Cranial Neoplasm | 127 (17.3%) | 18 (10.0%) | 0.53 (0.32–0.90) | 18 (12.7%) | 0.70 (0.41–1.18) | 0 | Undefined |
| Trauma †† | 53 (7.2%) | 56 (31.1%) | 5.82 (3.82–8.87) | 51 (35.9%) | 7.22 (4.64–11.24) | 5 (13.2%) | 1.95 (0.73–5.21) |
| SDH | 29 (3.9%) | 26 (14.4%) | 22 (15.5%) | 4 (10.5%) | |||
| SAH | 4 (0.5%) | 17 (9.4%) | 17 (12.0%) | 0 | |||
| Skull Fracture | 11 (1.5%) | 5 (2.8%) | 5 (3.5%) | 0 | |||
| Non-traumatic Spine | 69 (9.4%) | 21 (11.7%) | 1.28 (0.76–2.14) | 21 (14.8%) | 1.68 (0.99–2.84) | 0 | Undefined |
| Fracture | 36 (4.9%) | 17 (9.4%) | 17 (12.0%) | ||||
| Neoplasm | 12 (1.6%) | 0 | 0 | ||||
| Infection | 8 (1.1%) | 0 | 0 | ||||
| Cranial Infection | 40 (5.4%) | 0 | Undefined | 0 | Undefined | 0 | Undefined |
| Ischemic Stroke | 31 (4.2%) | 0 | Undefined | 0 | Undefined | 0 | Undefined |
| Unruptured Aneurysm | 24 (3.3%) | 5 (2.8%) | 0.84 (0.32–2.25) | 5 (3.5%) | 1.08 (0.41–2.89) | 0 | Undefined |
| Shunt-related | 20 (2.7%) | 0 | Undefined | 0 | Undefined | 0 | Undefined |
| Hydrocephalus | 16 (2.2%) | 1 (0.6%) | 0.25 | 1 (0.7%) | 0.32 | 0 | Undefined |
| Headache | 7 (1.0%) | 6 (3.3%) | 3.59 (1.19–10.82) | 6 (4.2%) | 4.60 (1.52–13.89) | 0 | Undefined |
| Other | 49 (6.7%) | 16 (8.9%) | 1.37 (0.76–2.47) | 15 (10.6%) | 1.66 (0.90–3.04) | 1 (2.6%) | 0.10 |
Table 4.
Comparison of Age by Admission Reason Between Cohorts
| Justifiable Transfers | Potentially Avoidable Transfers | |||
|---|---|---|---|---|
| All | Living | Expired | ||
| Admission reason | ||||
| Non-traumatic Hemorrhage † | 56.1 ± 14.3 | 64.7 ± 16.2 ** | 69.4 ± 17.8 *** | 60.97 ± 13.9 |
| ICH | 55.7 ±16.6 | 61.0 ± 16.8 | 62.8 ± 20.0 | 59.3 ± 13.7 |
| SAH | 54.9 ± 13.0 | 62.4 ± 14.7 | 78.0 ± 9.5 * | 58.9 ± 13.4 |
| SDH | 61.9 ± 13.8 | 74.4 ± 13.4 * | 76.1 ± 13.4 * | 71.2 ± 14.3 |
| EDH | 53.3 ± 27.6 | |||
| Cranial Neoplasm | 54.9 ± 14.7 | 58.7 ± 17.8 | 58.7 ± 17.8 | |
| Trauma †† | 61.3 ± 21.7 | 64.0 ± 21.5 | 63.9 ± 21.7 | 66.0 ± 21.4 |
| SDH | 72.6 ± 10.7 | 68.8 ± 19.1 | 68.4 ± 19.2 | 71.3 ± 20.7 |
| SAH | 65.8 ± 23.7 | 61.7 ± 24.8 | 61.7 ± 24.8 | |
| Skull Fracture | 41.8 ± 15.9 | 72.2 ± 13.1 ** | 72.2 ± 13.1 ** | |
| Non-traumatic Spine | 58.5 ± 16.5 | 63.8 ± 19.9 | 63.8 ± 19.9 | |
| Fracture | 59.3 ± 17.8 | 67.2 ± 18.7 | 67.2 ± 18.7 | |
| Neoplasm | 55.5 ± 15.6 | |||
| Infection | 54.5 ± 15.8 | |||
| Cranial Infection | 50.7 ± 17.5 | |||
| Ischemic Stroke | 57.3 ± 13.2 | |||
| Unruptured Aneurysm | 61.3 ± 19.1 | 53.0 ± 13.1 | 53.0 ± 13.1 | |
| Shunt-related | 46.1 ± 18.4 | |||
| Hydrocephalus | 56.5 ± 14.5 | 42 | 42 | |
| Headache | 28.1 ± 7.9 | 41.0 ± 12.7 | 41.0 ± 12.7 | |
| Other | 49.4 ± 20.3 | 50.9 ± 16.4 | 50.3 ± 16.8 | 61 |
Cost of Potentially Avoidable Transfers
We calculated the direct cost of transferring patients by using the UAB Critical Care Transport billing rates for transfers. For ground transportation, there is a base fee of $6160 plus a $24.64 per mile charge. For air transfers, there is a base fee of $11 760 plus a $122.08 per mile charge. Given inconsistent representation of transfer method in the electronic medical record, it was assumed that all patients were transferred by ground for the purposes of this study. The total direct transportation cost of transferring PATs from an outside hospital to our tertiary care center over a 2-year period was $1.46 million.
DISCUSSION
In this study, our intent was to acquire pilot data to understand whether potentially avoidable transfers represented a real issue worthy of future research. To that end, there was no intent to broaden the scope to include factors such as local resources, locoregional policy, transfer decisions, and natural history of patients not transferred to a tertiary neurosurgical facility. We capitalized on a large dataset with 916 patients transferred to the neurosurgical service over a 2-year period. We hypothesized that potentially avoidable transfers would form 2 distinct groups, those with benign pathology not requiring intervention and those with catastrophic neurologic injury for which intervention is futile. Our results supported our initial hypothesis. Surviving PATs were more likely to involve older patients and those with trauma and headache and less likely to have non-traumatic intracranial hemorrhage. In contrast, PATs who died were more likely to have non-traumatic intracranial hemorrhage. Increasing age was significantly associated with potentially avoidable transfers, and may either contribute to worse outcomes or to overly cautious transfers to a tertiary care facility. Our findings were consistent with prior studies showing that intracranial hemorrhage and trauma comprises a large proportion of neurosurgical transfers.4,8 While most prior studies examined transfers of trauma patients.6,7,9 our study was unique in that we included all patients transferred to the neurosurgical service, thus capturing a large number of patients transferred for neoplasms, spine-related complaints, and other non-traumatic pathology. Finally, we found that PATs were more likely to have Medicare and less likely to have private insurance, which we did not initially postulate.
Our study dovetails with the recently published report from Emory University regarding neurosurgical transfers.4 Our population underwent procedural intervention at a higher rate (84% vs 68%) but was transferred to an ICU at a nearly identical rate of 73%. The composition of diagnoses had some notable differences; while 15% of transfers to both UAB and Emory were for tumor, Emory had a higher proportion of intracerebral hemorrhage and subarachnoid hemorrhage, and UAB had a significant cohort of traumatic injury. At both centers, >90% of transfers were for cranial pathology. Our study replicates many findings reported by Holland et al and adds information about potential avoidability of some of these transfers.4 Additionally, we examine the direct transportation cost of potentially avoidable transfers.
We found that it cost $1.46 million to physically transport PATs from an outside hospital to our tertiary care facility over a 2-year period. This sum is an underestimation of the total direct and indirect costs not accounted for in this study. We assumed that all patients were transferred by ground ambulance, while ongoing prospective data collection suggests that approximately 20% of our transfers actually arrive via air (fixed wing aircraft or helicopter; unpublished data, Kuhn et al, 2016). We did not include the cost of admission to and diagnostic workup at both facilities. Moreover, this sum does not account for duplication of diagnostic laboratory and imaging testing, costs associated with inappropriate ICU admission, and prolonged hospital stay as a result of transfer. PATs were admitted to intensive care units at the same rate as justifiable transfers (about 70% of patients), but almost half of these PATs to the ICU were determined to be stable and discharged home the same or next day. With limited ICU beds, these PATs are occupying a valuable resource that may prevent others with neurosurgical problems from receiving adequate care. This opportunity cost is not quantified in our analysis. PATs take an economic and emotional toll on patients’ families and loved ones, some being displaced hundreds of miles from home.
Limitations of Design and Scope
We did not consider local resources such as on-call neurosurgeons, critical care intensivists, diagnostic/imaging capabilities, and ability to appropriately manage the patient’s condition. We did not consider underlying dynamics including regional hospital bed availability, patient/family desires, and previously established care at UAB. We uniformly assumed that outside hospitals were unable to provide MRI, long-term EEG, and other resources that they may, in fact, have. By classifying those transfers as justifiable, we may have overestimated the true number of PATs. On the other hand, patients who underwent surgery due to convenience and not necessarily medical necessity were classified as JTs; this underestimates the true number of PATs. With retrospectively collected data, it is difficult to quantify how many patients deteriorated en route, how many patients at originating sites were never transferred (and their outcomes), and how often patients were denied transfer. Nor did we evaluate the effect of existing cross-community policy and relationships. Finally, we did not examine the actual communication between transferring and accepting physicians to identify other factors influencing transfer. These are all important factors to consider in future studies of potentially avoidable transfers.
As focus on efficiency and quality within the healthcare system increases, identification of unnecessary expenditure of limited healthcare resources comes to the forefront. While potentially avoidable transfers may increase the burden on the healthcare system, denying transfer can unnecessarily endanger patients. Physicians at originating sites are presumably requesting transfer due to real or perceived inability to care for a given patient. We need to improve our ability to identify and address the specific concerns of physicians at originating sites. At our institution, transfers are accepted (or denied) by the attending physician during weekdays and by the chief resident on weeknights and weekends. Triage of potential transfers may vary across institutions based on who is responsible for that process and the experience level of that individual. An ideal transfer system identifies patients needing a higher level of care or specialized services (high sensitivity), but does not transfer patients who can be adequately managed at the originating site (high specificity). We present these data as justification for further and more in-depth study of unnecessary transfers in an effort to utilize the “right-size” resources and save money across the health system.
To achieve the goal of using the “right-size” resources, it will be necessary to (a) establish guidelines based on clinical and imaging criteria to identify patients who could be safely managed locally vs those who would benefit from a transfer to a tertiary care facility and (b) negotiate cross-institution and payer policies to work within those guidelines. Telemedicine offers a spectrum of services that may be well suited to address some of these issues. The term “telemedicine” encompasses a broad range of services and tools including universal imaging repositories, 2-way video, augmented reality interactive video, email, smartphone applications, and other wireless services. Effective use of a telemedical tool requires that the tool have sufficient technical performance, the ability to transmit needed expertise, and the ability of the originating site to utilize the transmitted expertise. Many of these technologies are already widely available, though often underrecognized and underutilized. For example, our hospital is a member of a 15-hospital statewide imaging network to allow for remote review of imaging studies, yet this is rarely utilized in clinical practice. We have demonstrated the successful use of Virtual Interactive Presence and Augmented Reality (VIPAR), an iPad-based, interactive 2-way video tool, in long-distance intraoperative guidance and telecollaboration.10,11 There are significant legal hurdles in implementation and use of certain telemedical tools, including patient privacy, assurance of quality, and distribution of liability.12–16 Hall and McGraw argue that these issues can be addressed with the development of a comprehensive regulatory framework for telemedicine overseen and enforced by the Federal Trade Commission.16 Telemedical tools have been successfully implemented in acute stroke care17–19 and ST-elevation myocardial infarction,20–22 and those fields can provide a rubric for paradigms in neurosurgery.
Further investigation of justifiability of transfer should consider the detailed clinical state of the patient, the likely change in that state over time, the resources at the originating site, the technical features of cross-institution communication systems (such as telemedical solutions), the capability of transferring expertise using communication technology, and the capability of the originating site to use transmitted expertise. We also propose that payers should be significantly involved, since they assume the brunt of the cost associated with transfer.
Our process and analytic methods are likely applicable across numerous specialties, including other surgical subspecialties at our institution. The physical cost of transportation is likely similar at other tertiary care facilities across the country. However, average transfer distance may vary based on the catchment area for the tertiary care facility in question, as seen in comparing our results to those of Holland et al.4 Our results are more likely to be generalizable to other tertiary care facilities located in regions with a low density of tertiary hospitals and large geographic referral regions, as seen by similarities between our results and those of Holland et al.4
CONCLUSION
Potentially avoidable transfers are a substantial burden to patients, their families, and the healthcare system. Identification of patients who can appropriately receive subspecialty management at a distance has the potential for considerable cost savings and improved healthcare efficiency. Our results suggest that potentially avoidable transfers fall into 2 groups: lesions with a benign natural history and irreversible, devastating neurologic insults. These findings warrant validation at other centers. Future studies should investigate the impact of telemedical tools, improved cross-community communication, and care policy on the incidence and cost of potentially avoidable transfers.
Acknowledgments
We thank Laura Lee Demmons and UAB Critical Care Transport for the cost of patient transport.
Footnotes
Disclosures: This work was supported by the Kaul Foundation, NIH grants F30AG046088, the National Center for Advancing Translational Sciences (UL1TR00165), and the UAB Medical Scientist Training Program (T32GM008361). The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
References
- 1.Fell MJ. The Emergency Medical Treatment and Active Labor Act of 1986: providing protection from discrimination in access to emergency medical care. Spec Law Dig Health Care Law. 1996;(204):9–42. [PubMed] [Google Scholar]
- 2.Peth HA. The Emergency Medical Treatment and Active Labor Act (EMTALA): guidelines for compliance. Emerg Med Clin North Am. 2004;22(1):225–240. doi: 10.1016/S0733-8627(03)00123-8. [DOI] [PubMed] [Google Scholar]
- 3.Byrne RW, Bagan BT, Slavin KV, Curry D, Koski TR, Origitano TC. Neurosurgical emergency transfers to academic centers in Cook County: a prospective multicenter study. Neurosurgery. 2008;62(3):709–716. doi: 10.1227/01.neu.0000317320.79106.7e. discussion 709–716. [DOI] [PubMed] [Google Scholar]
- 4.Holland CM, McClure EW, Howard BM, Samuels OB, Barrow DL. Interhospital Transfer of Neurosurgical Patients to a High-Volume Tertiary Care Center: Opportunities for Improvement. Neurosurgery. 2015;77(2):200–206. doi: 10.1227/NEU.0000000000000752. discussion 206–207. [DOI] [PubMed] [Google Scholar]
- 5.Spain DA, Bellino M, Kopelman A, et al. Requests for 692 transfers to an academic level I trauma center: implications of the emergency medical treatment and active labor act. J Trauma. 2007;62(1):63–67. doi: 10.1097/TA.0b013e31802d9716. discussion 67–68. [DOI] [PubMed] [Google Scholar]
- 6.Joosse P, Saltzherr T-P, van Lieshout WAM, et al. Impact of secondary transfer on patients with severe traumatic brain injury. J Trauma Acute Care Surg. 2012;72(2):487–490. doi: 10.1097/TA.0b013e318226ed59. [DOI] [PubMed] [Google Scholar]
- 7.Lind CRP, Heppner PA, Robins TM, Mee EW. Transfer of intubated patients with traumatic brain injury to Auckland City Hospital. ANZ J Surg. 2005;75(10):858–862. doi: 10.1111/j.1445-2197.2005.03574.x. [DOI] [PubMed] [Google Scholar]
- 8.Walcott BP, Coumans J-V, Mian MK, Nahed BV, Kahle KT. Interfacility helicopter ambulance transport of neurosurgical patients: observations, utilization, and outcomes from a quaternary level care hospital. PLoS ONE. 2011;6(10):e26216. doi: 10.1371/journal.pone.0026216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joseph B, Friese RS, Sadoun M, et al. The BIG (brain injury guidelines) project: defining the management of traumatic brain injury by acute care surgeons. J Trauma Acute Care Surg. 2014;76(4):965–969. doi: 10.1097/TA.0000000000000161. [DOI] [PubMed] [Google Scholar]
- 10.Davis MC, Can DD, Pindrik J, Rocque BG, Johnston JM. Virtual Interactive Presence in Global Surgical Education: International Collaboration Through Augmented Reality. World Neurosurg. 2016;86:103–111. doi: 10.1016/j.wneu.2015.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shenai MB, Dillavou M, Shum C, et al. Virtual interactive presence and augmented reality (VIPAR) for remote surgical assistance. Neurosurgery. 2011;68(1 Suppl Operative):200–207. doi: 10.1227/NEU.0b013e3182077efd. discussion 207. [DOI] [PubMed] [Google Scholar]
- 12.Szalados JE. Anesthesia in remote locations: medicolegal risks and strategies for minimizing liability. Int Anesthesiol Clin. 2009;47(2):105–131. doi: 10.1097/AIA.0b013e31819342f9. [DOI] [PubMed] [Google Scholar]
- 13.Wallace S, Sibson L, Stanberry B, et al. The legal and risk management conundrum of telemedicine. J Telemed Telecare. 1999;5(Suppl 1):S8–S9. doi: 10.1258/1357633991932748. [DOI] [PubMed] [Google Scholar]
- 14.Stanberry B. Legal ethical and risk issues in telemedicine. Comput Methods Programs Biomed. 2001;64(3):225–233. doi: 10.1016/s0169-2607(00)00142-5. [DOI] [PubMed] [Google Scholar]
- 15.Yang YT, Silverman RD. Mobile health applications: the patchwork of legal and liability issues suggests strategies to improve oversight. Health Aff Proj Hope. 2014;33(2):222–227. doi: 10.1377/hlthaff.2013.0958. [DOI] [PubMed] [Google Scholar]
- 16.Hall JL, McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff Proj Hope. 2014;33(2):216–221. doi: 10.1377/hlthaff.2013.0997. [DOI] [PubMed] [Google Scholar]
- 17.Itrat A, Taqui A, Cerejo R, et al. Telemedicine in Prehospital Stroke Evaluation and Thrombolysis: Taking Stroke Treatment to the Doorstep. JAMA Neurol. 2016;73(2):162–168. doi: 10.1001/jamaneurol.2015.3849. [DOI] [PubMed] [Google Scholar]
- 18.Lyerly MJ, Wu T-C, Mullen MT, et al. The effects of telemedicine on racial and ethnic disparities in access to acute stroke care. J Telemed Telecare. 2016;22(2):114–120. doi: 10.1177/1357633X15589534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanders KA, Patel R, Kiely JM, Gwynn MW, Johnston LH. Improving Telestroke Treatment Times in an Expanding Network of Hospitals. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2016;25(2):288–291. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 20.Rasmussen MB, Frost L, Stengaard C, et al. Diagnostic performance and system delay using telemedicine for prehospital diagnosis in triaging and treatment of STEMI. Heart Br Card Soc. 2014;100(9):711–715. doi: 10.1136/heartjnl-2013-304576. [DOI] [PubMed] [Google Scholar]
- 21.Stowens JC, Sonnad SS, Rosenbaum RA. Using EMS Dispatch to Trigger STEMI Alerts Decreases Door-to-Balloon Times. West J Emerg Med. 2015;16(3):472–480. doi: 10.5811/westjem.2015.4.24248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanguay A, Dallaire R, Hébert D, Bégin F, Fleet R. Rural Patient Access to Primary Percutaneous Coronary Intervention Centers is Improved by a Novel Integrated Telemedicine Prehospital System. J Emerg Med. 2015;49(5):657–664. doi: 10.1016/j.jemermed.2015.05.009. [DOI] [PubMed] [Google Scholar]