Abstract
Proprioception is essential for shoulder neuromuscular control and shoulder stability. Exercise of the rotator cuff and scapulothoracic muscles is an important part of shoulder rehabilitation. The purpose of this study was to investigate the effect of rotator cuff and scapulothoracic muscle exercises on shoulder joint position sense. Thirty-six healthy subjects were recruited and randomly assigned into either a control or training group. The subjects in the training group received closed-chain and open-chain exercises focusing on rotator cuff and scapulothoracic muscles for four weeks. Shoulder joint position sense errors in elevation, including the humerothoracic, glenohumeral and scapulothoracic joints, was measured. After four weeks of exercise training, strength increased overall in the training group, which demonstrated the effect of exercise on the muscular system. However, the changes in shoulder joint position sense errors in any individual joint of the subjects in the training group were not different from those of the control subjects. Therefore, exercises specifically targeting individual muscles with low intensity may not be sufficient to improve shoulder joint position sense in healthy subjects. Future work is needed to further investigate which types of exercise are more effective in improving joint position sense, and the mechanisms associated with those changes.
Keywords: proprioception, joint position sense, strengthening exercise, scapular muscles, rotator cuff
1. Introduction
Proprioception includes afferent inputs of joint position sense (JPS), kinesthesia and sensation of resistance. These afferent inputs originate from muscle spindles and Golgi tendon organs in the musculotendinous structures as well as mechanoreceptors in the joint capsule, ligament and tissue surrounding the joint (Riemann & Lephart, 2002). Proprioception is involved in reflex arcs contributing to joint stabilization (Borsa, Lephart, Kocher, & Lephart, 1994) and automatic movement (Riemann & Lephart, 2002) as well as motor planning and strategy (Riemann & Lephart, 2002).
Proprioception input is essential for the central nervous system to regulate neuromuscular control in order to maintain functional joint stability, especially for the shoulder complex, which relies heavily on muscular contractions for stability. Subjects with shoulder pathologies, such as shoulder impingement syndrome (Anderson & Wee, 2011; Machner et al., 2003), anterior glenohumeral dislocation history (Smith & Brunolli, 1989), and shoulder instability (Lephart, Warner, Borsa, & Fu, 1994) have demonstrated proprioception deficits. It is possible that injured or loose ligaments, capsules, and muscles affect proprioception afferent input. Proprioception deficits may result in impaired neuromuscular control, which could ultimately lead to muscle imbalance and joint instability. The microinjuries resulting from joint instability can aggravate these proprioception deficits. This vicious cycle may be a factor in the development of chronic shoulder pain and the high recurrent rate of shoulder dislocation (Lephart et al., 1994).
Impaired neuromuscular control in patients with shoulder pathologies can include an abnormal contribution of the rotator cuff and scapulothoracic muscles. Previous studies have reported an increase in electromyography (EMG) of the upper trapezius as well as a decrease in EMG of the rotator cuff, lower trapezius, and serratus anterior (Lin, Hsieh, Cheng, Chen, & Lai, 2011; Ludewig & Cook, 2000; Reddy, Mohr, Pink, & Jobe, 2000). Exercises focusing on strengthen the rotator cuff and scapulothoracic muscles are typically recommended for shoulder rehabilitation and training (Cricchio & Frazer, 2011; Reinold, Escamilla, & Wilk, 2009). In order to restore the balance and coordination between muscles, those exercises are performed with shoulder movements in which the rotator cuff and scapulothoracic muscles show high muscle activity, with lower levels of deltoid, upper trapezius or pectoralis major activity (mainly open-chain exercises, except the exercise for serratus anterior) (Decker, Tokish, Ellis, Torry, & Hawkins, 2003; Ellenbecker & Cools, 2010; Reinold et al., 2007; Reinold et al., 2004). Closed-chain exercise, on the other hand, can generate higher muscle activation level of serratus anterior (Decker, Hintermeister, Faber, & Hawkins, 1999) and it has also been suggested that closed-chain exercise can facilitate co-contraction of the rotator cuff and scapulothoracic muscles, which is essential for joint stability (Myers & Oyama, 2009; Ubinger, Prentice, & Guskiewicz, 1999).
Although the effects of exercise training on proprioception are not clear, it has been postulated that exercise can enhance proprioception by modulating the sensitivity of muscle spindles or helping subjects pay more attention to joint position (Ashton-Miller, Wojtys, Huston, & Fry-Welch, 2001; Swanik, Lephart, Giannantonio, & Fu, 1997). Most exercises used in previous studies were advanced exercises for athletic training and were categorized into specific types of exercise. The effect of the exercises on shoulder JPS in healthy subjects has been explored with the use of open-chain exercises (Padua, Guskiewicz, Prentice, Schneider, & Shields, 2004; Rogol, Ernst, & Perrin, 1998; Salles et al., 2015), closed-chain exercises (Padua et al., 2004; Rogol et al., 1998), plyometric training (Heiderscheit, McLean, & Davies, 1996; Swanik et al., 2002), and proprioceptive neuromuscular facilitation (Padua et al., 2004). However, the results of exercise training are not consistent, even within the same type of exercises (Heiderscheit et al., 1996; Padua et al., 2004; Rogol et al., 1998; Salles et al., 2015; Swanik et al., 2002).
There are two main limitations in previous studies. First, to our knowledge, only one study used specific exercises targeting the rotator cuff and scapulothoracic muscles with open-chain exercises in a healthy population (Padua et al., 2004). However, in clinical practice, rehabilitation exercises typically contain both open-chain and closed-chain exercises (Cricchio & Frazer, 2011; Reinold et al., 2009). It is still unknown if strengthening exercises for rotator cuff and scapulothoracic muscles have improved the shoulder proprioception. Secondly, previous studies have investigated JPS using the positions of internal and external rotation (Heiderscheit et al., 1996; Padua et al., 2004; Rogol et al., 1998; Salles et al., 2015; Swanik et al., 2002). Although this testing position is easy to perform and is a functional position for overhead athletes, it blocks scapular movement and is not a functional motion for the general population. In addition, scapular JPS has not been investigated in previous exercise training studies.
Therefore, due to the limitations of the exercise and assessment protocols in previous studies, the purpose of the present study was to examine the effects of rotator cuff and scapulothoracic muscle strengthening exercises on shoulder JPS during arm elevation motion in healthy subjects in order to understand the JPS adaptation to exercises. We hypothesized that JPS errors of the humerothoracic (HT), glenohumeral (GH) and scapulothoracic (ST) joints would decrease after rotator cuff and scapulothoracic muscle strengthening exercise training. We also hypothesized that the strength of the rotator cuff and scapulothoracic muscles would increase after the exercise training.
2. Methods
2.1. Subjects
Thirty-six healthy subjects were recruited from the University of Oregon. Subject exclusion criteria for the study were as follows: 1) prior shoulder and cervical surgery; 2) presence of shoulder and neck pain and injuries; 3) history of cervical or shoulder pain or pathology in past 3 years; 4) a concussion within the past 12 months or a history of 3 or more concussions; 5) brain injury and neurological impairment; 6) history of seizures; 7) taking anti-seizure and anti-depressive medication; 8) pacemaker and other magnetic implant; 9) pregnancy and 10) participation in NCAA sports that involves the extensive use of the upper extremity. The study was approved by the Office for Protection of Human Subjects at the University of Oregon and all subjects signed an informed consent form.
2.2. Procedure
Subjects were randomly assigned into either a control or training group during their first visit to the lab. The age, height and weight of subjects in both groups were similar, with no significant between group differences. (Table 1). JPS of the dominant shoulder was assessed at baseline and 4-5 weeks later for both groups. For the control subjects, these were only two visits for JPS assessment. For the subjects in the training group, in addition to the two JPS assessments, there were two visits for exercise intensity evaluation, and 12 visits for exercise training.
Table 1.
Subject characteristics: means (standard deviations)
| Training (n = 18) |
Control (n = 18) |
p | |
|---|---|---|---|
| Age (y) | 20.3 (1.9) | 21.1 (3.9) | 0.42 |
| Height (cm) | 167 (10) | 168 (10) | 0.77 |
| Weight (kg) | 67.3 (12.3) | 65.8 (14.0) | 0.73 |
| Sex | 9M, 9F | 8M, 10F | |
| Dominant side | 16R, 2L | 16R, 2L |
* Independent t test was used to examine the difference between groups. M: male, F: female. R: right-hand dominant, L: left-hand dominant.
2.3. Exercise training
The subjects in the control group were instructed to maintain their normal activities of daily living, while the subjects in the training group were trained three times per week for four weeks, with an average duration of 30 minutes per session. All training sections were supervised to ensure compliance with the training protocol.
The exercise training protocol consisted of open-chain and closed-chain exercises. The open-chain exercises included full can, sidelying external rotation, diagonal exercise, and prone full can at 100° of abduction. These exercises were chosen because they specifically generate higher level of activation of the rotator cuff, lower trapezius or serratus anterior (Cools et al., 2007; Reinold et al., 2009; Reinold et al., 2007; Reinold et al., 2004). A ten repetition maximum (RM) was tested during the two visits of exercise intensity evaluation to determine the exercise intensity used in the open-chain exercises for each exercise and each subject. Sandbags and dumbbells were used to provide the resistance for the open-chain exercises. This was assessed before the first visit of the exercise training and measured again at week three, before the seventh training section. The strengthening training consisted of three sets of 10 repetitions using variable resistance: one set at 50% of the 10 RM, one at 75% of the 10 RM, and one at 100% of the 10 RM (Padua et al., 2004).
The closed-chain exercises consisted of a push-up with plus and balance exercises. These exercises were believed to facilitate the co-contraction of shoulder muscles (Myers & Oyama, 2009; Ubinger et al., 1999) as well as strengthen the serratus anterior (Reinold et al., 2009). The subjects performed the push-up with plus for 15 – 40 repetitions per visit and progressed from a quadruped position to the push-up on toes, depending on the ability of the subjects. The push-up with plus emphasized shoulder protraction (plus) at the end of the push-up. For the balance exercise, subjects maintained the push-up position with their hands on an exercise ball or a wobble board with five repetitions and 15 seconds for each repetition. This exercise progressed from a wobble board to an exercise ball and from a quadruped position to a push-up on the toes to a one-arm push-up (Padua et al., 2004). The interval between sets was one minute. There was a rest period of three minutes between each exercise.
The subjects in the training group were asked to perform home exercises including full can, bilateral external rotation with the arm at the side, and push up with plus. For the first two weeks, they were asked to perform 10 repetitions per day for seven days a week for each home exercise. For the last two weeks, the frequency was 20 repetitions per day, seven days a week. A resistance band (TheraBand, the Hygenic Corporation, Akron, OH, USA) was used to provide resistance in the exercise of full can and bilateral external rotation.
2.4. Force measurement
In order to confirm the effect of the exercise, a maximum voluntary contraction (MVC) of the rotator cuff and scapular muscles during a five-second isometric contraction were measured at both JPS assessment visits. Four specific testing positions were conducted with three trials for each testing position, including 90° of elevation, external rotation, horizontal abduction, and 135° of elevation. There were approximately 30 seconds of rest between trials and one minute of rest between positions. A handheld dynamometer micro FET2 (Hoggan Scientific, Salt lake city, UT, USA) was used to measure all the forces during MVC, except the MVC force at the position of 90° of elevation. The handheld dynamometer was positioned at the wrist joint to provide resistance. The force of external rotation for posterior rotator cuff muscles was tested with the arm at the side and 90° of elbow flexion (Alpert, Pink, Jobe, McMahon, & Mathiyakom, 2000). The force of horizontal abduction for lower trapezius was tested in a prone position with horizontal abduction in 120° of elevation in line with the fibers of the lower trapezius and the thumb pointing upward (Ekstrom, Soderberg, & Donatelli, 2005). The force of 135° of elevation for the serratus anterior was measured with 135° of abduction in the scapular plane (Ekstrom et al., 2005). The dynamometer recorded the peak force during the muscle contraction.
The force of 90° of elevation for the deltoid and supraspinatus was measured with abduction in the scapular plane at 90° of humeral elevation with neutral axial rotation (Ludewig & Cook, 2000; Reinold et al., 2007). In order to provide stable resistance, a load cell (Lebow, Troy, MI, USA) mounted on the wall was used to measure the force at 90° of elevation, instead of the handheld dynamometer. The wrist joint was placed beneath the load cell. The force measured by the load cell was calculated by the mean of the middle 1.5 seconds of the muscle contraction.
2.5. JPS measurement
JPS was tested with an active position reposition task on the dominant shoulder. There were three target positions of HT elevation in the scapular plane (50°, 70°, and 90°). Each target position was repeated four times, resulting in 12 trials. Kinematics of HT and GH and ST joints was measured with a magnetic tracking device (Polhemus Liberty, Colchester, VT, USA). Using the definition proposed by the ISB, the thoracic anatomic coordinate system was derived from T8, C7, the xiphoid process and the jugular notch. The digitization points for the scapula were the root of the scapular spine, inferior angle of the scapula, and laterodorsal point of the acromion. The humeral coordinate system was defined with the second option in the ISB proposed standard, which includes the center of the humeral head, medial epicondyle, lateral epicondyle, ulnar styloid process and medial styloid process (Wu et al., 2005). The center of the humeral head was calculated using a least squares algorithm and was defined as the point that moved the least during several small arcs of motion (Veeger, 2000). The HT joint was defined as the humeral coordinate system with respect to the thoracic coordinate system. The GH joint was calculated from the humeral coordinate system with respect to the scapular coordinate system. The ST joint was derived from the scapular coordinate system with respect to thoracic coordinate system. The subject was fitted with a head mounted display (Z800, eMagine, Bellevue, WA, USA) (Figure 1). The display blocked the visual feedback for the shoulder motion as well as displayed the target angle and real-time HT angle of the subject.
Figure 1.
Testing position and sensor placement
The visual and auditory guides during testing motion were controlled by a customized LabVIEW program (Version 2012, National Instruments, Austin, TX, USA) and the protocol was modified from the protocol of King et al. (2013). At the beginning of the trial, a black screen was displayed and the subject was asked to relax with the arm at their side. Two white lines were then shown on the black screen, indicating the boundary of the predetermined target position (±1° from the target). For all target angles, the white lines were always set at the same position of the screen. The subject was instructed to elevate the arm with the elbow extended and thumb pointing up. A dynamic red line, representing real-time HT angles of the subject, appeared on the screen when the HT angle was within 10 degrees of the target. Additionally, when the subject deviated more than five degrees from the scapular plane (35 degrees anterior to the frontal plane), a vertical green line would appear on the side of the screen, which prompted the subject to move away from the line and back into the scapular plane.
The subject was instructed to elevate the arm until the red line was positioned between the white lines, with no green line displayed. After the subject had maintained the red line between the white lines for one second, the target disappeared and only a black screen was left. For the rest of the trial, the display remained black, thus removing all visual feedback. The subjects were instructed to hold their arms at the target position and memorize their arm position (three seconds) until they heard verbal instructions from the computer, indicating that they should return their arm to the side. After relaxing the arm at the side for two seconds, another verbal cue from the computer prompted the subject to reposition their shoulder to the target position, without any visual guide. When the subjects believed the target had been reached, they pushed a button on a wireless trigger with their contralateral hand. This would trigger the computer to instruct the subject to relax their arm to the side, at which point the trial ended. Between the trials, a blue screen was displayed with a countdown timer and instructions to keep the arm at the side during the break. No feedback related to the accuracy of performance was provided to the subjects. Before the JPS assessment, the subjects practiced to elevate their arm in the scapular plane for three to five times and had three to five JPS practice trials to ensure they understood the visual and auditory cues of the JPS assessment.
2.6. Data reduction
Because the plane of elevation and axial rotation were controlled, only the errors of elevation were considered for the HT and GH joints. The errors (θe) is the difference between the angles at the present target position and repositioned position. For the ST joint, because it is hard to constrain scapular motion in one dimension, we chose to use the helical angle to represent ST motion. The helical angle is the rotation angle about the helical axis (Woltring, Huiskes, de Lange, & Veldpaus, 1985). Although the helical axis is not aligned with the anatomic axes, the helical angle can represent the ST three-dimensional angular motion. The error of the scapular helical angle (θe) was derived from the rotation matrix at the repositioned position with respect to that at presented target position.
Constant and variable errors were calculated to represent accuracy and precision of JPS respectively (King et al., 2013; Schmidt & Lee, 2005), where n is number of repetition for each target angle, which was four in this present study.
2.7. Statistical analysis
The MVC force measures at each testing position were averaged across three trials. The percentage change of the force was calculated, which is the force change from the pre-training to post-training divided by the force at the pre-training. An independent t test was used to examine the differences in the percentage change of the forces between the two groups.
The change scores of the constant and variable errors from pre-training to post-training were calculated. A two-way, mixed-effects analysis of variance (ANOVA) was used to examine the effect of exercise on the shoulder JPS. The dependent variables were the change scores of the constant and variable errors of the HT, GH and ST joints at each target angle. Angle was within subject effect, which had three levels: 50°, 70°, and 90°. The between-subject effect was group, control and training groups. If there was an interaction effect, pairwise comparisons were conducted. The significance level was set at 0.05.
3. Results
All the subjects in the control group completed two JPS assessments. One subject in the training group did not finish the exercise training and the second JPS assessment due to personal reasons. All other subjects in the training group completed all the training sections and the two JPS assessments. It resulted in 18 subjects in the control group and 17 subjects in the training group.
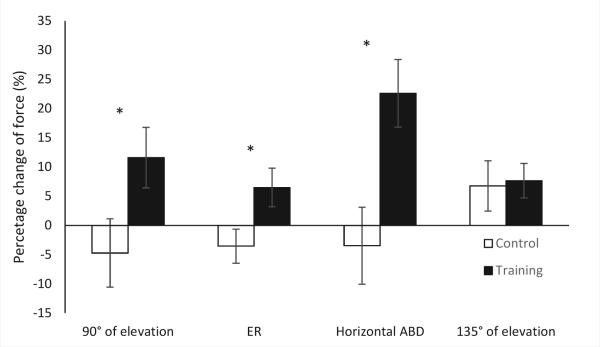
For MVC force measures, significant group differences were found in the percentage force change of 90° of elevation, external rotation and horizontal abduction (p = 0.046, p = 0.029, and p = 0.006, respectively). There was no difference between groups at 135° of elevation (p = 0.868) (Figure 2).
Figure 2.
The percentage changes of the forces from pre-training to post-training in control and training groups. The maximum voluntary contraction force of 90° of elevation for the deltoid and supraspinatus was measured with abduction (ABD) in the scapular plane at 90° of humeral elevation with neutral axial rotation. The force of external rotation (ER) for posterior rotator cuff muscles was tested with the arm at the side and 90° of elbow flexion. The force of horizontal abduction for lower trapezius was tested in a prone position with horizontal abduction in 120° of elevation. The force of 135° of elevation for the serratus anterior was measured with 135° of abduction in the scapular plane. (*p < 0.05)
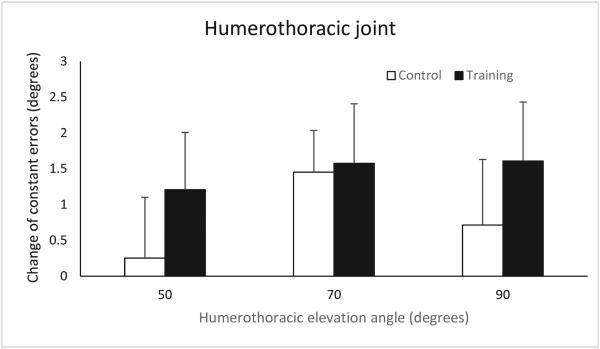
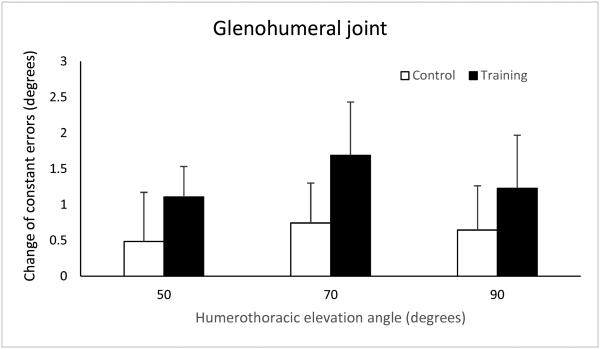
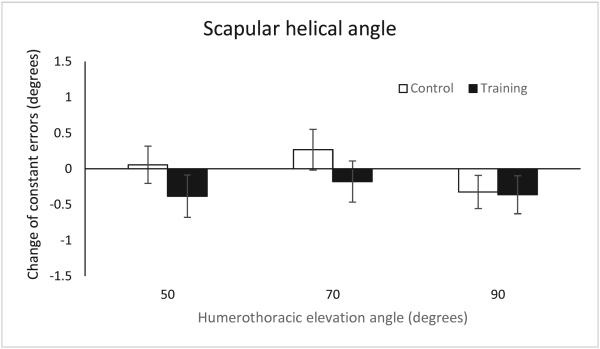
The average of the plane of elevation was 36.7° in the pre-training test and 36.6° in the post-training test. For constant errors of the HT joint, there was no significant group by angle interaction (p = 0.796), within-subject effect of angle (p = 0.522) and between-subject effect of group (p = 0.431) (Figure 3a). For GH constant errors, there was also no significant interaction effect (p = 0.927), angle effect (p = 0.705) and group effect (p = 0.303) (Figure 3b). For ST constant errors, there was also no significant interaction effect (p = 0.656), angle effect (p = 0.315) and group effect (p = 0.225) (Figure 3c).
Figure 3.
Means and standard errors of the changes of the constant errors after the exercise training in (a) humerothoracic joint, (b) glenohumeral joint, and (c) scapulothoracic joint
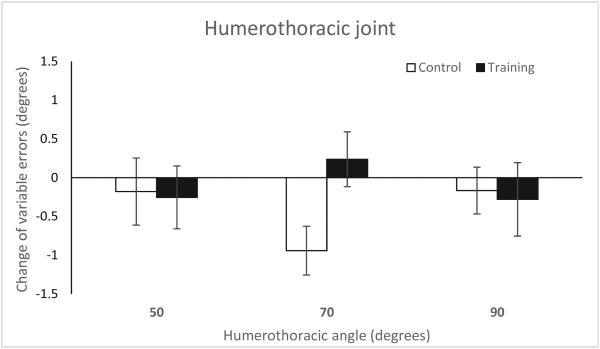
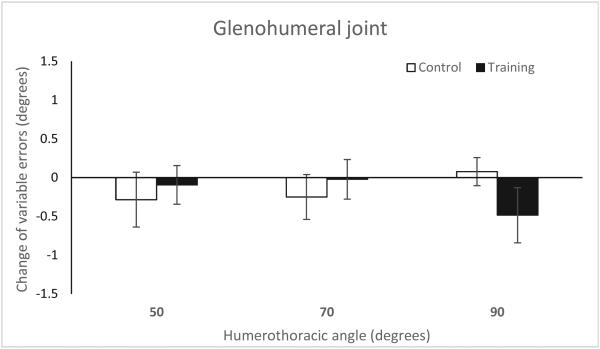
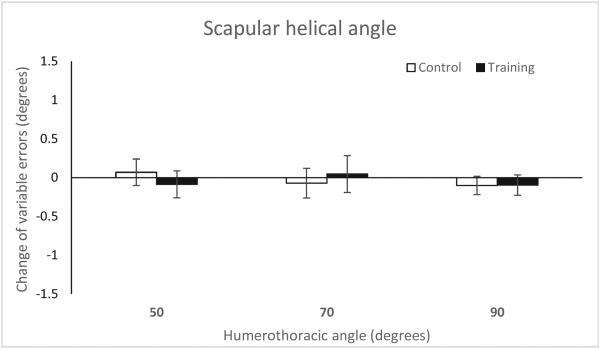
For the variable errors, in HT joint, there was no significant interaction of group and angle (p = 0.184), within-subject effect of angle (p = 0.928) and between-subject effect of group (p = 0.294) (Figure 4a). For GH variable errors, there was also no significant difference in interaction effect (p = 0.327), angle effect (p = 0.971) and group effect (p = 0.836) (Figure 4b). For ST variable errors, there was also no significant difference in interaction effect (p = 0.699), angle effect (p = 0.800) and group effect (p = 0.937) (Figure 4c).
Figure 4.
Means and standard errors of the changes of the variable errors after the exercise training in (a) humerothoracic joint, (b) glenohumeral joint, and (c) scapulothoracic joint
4. Discussion
It has been recommended that rehabilitation programs include exercises to restore the sensorimotor control of patients with shoulder injuries (Borsa et al., 1994; Myers, Wassinger, & Lephart, 2006; Reinold et al., 2009). Since JPS is important for shoulder neuromuscular control, we examined the effect of four weeks of rotator cuff and scapulothoracic muscle strengthening exercises on shoulder JPS in healthy subjects. After four weeks, although most of the force changes in the training group were significantly greater than those of the control groups, there were no significant differences in the changes of constant errors and variable errors between the control and training groups. In other words, the results showed there was an effect of exercises on shoulder muscle forces (the motor system) but the exercise did not affect JPS (the sensory system). Thus the results partially supported our hypothesis.
Although the mechanisms associated with the effect of exercise on proprioception have not been identified, exercises with active contraction are considered to be proprioceptive training because the muscle spindles and Golgi tendon organs are stimulated during active contraction (Röijezon, Clark, & Treleaven, 2015). Strengthening exercises of rotator cuff and scapulothoracic muscles is typically part of shoulder proprioception rehabilitation protocol (Borsa et al., 1994). In previous studies, the exercises were categorized as open-chain and closed-chain exercises. However, the effects of exercises on JPS were not consistent.
Most shoulder strengthening exercises are open-chain exercises, in which a distal segment of the arm is free moving and does not support body weight (Lephart & Henry, 1996). Rogol et al. (1998) and Salles et al. (2015) trained healthy subjects with exercises involving multiple joints and large muscle groups. They found that JPS improved after training. Salles et al. (2015) also demonstrated the group trained with higher intensity (eight to nine RM) showed more improvement, compared to the group with 12 – 13 RM. However, Padua et al. (2004) chose open-chain exercises targeting rotator cuff and scapulothoracic muscles, as in the present study, but found no effect on JPS in healthy college-age subjects, although the average rotational torque significantly increased. Considering the results of the present study and these previous studies, open-chain exercise involving multiple joints and large muscle groups with high intensity, such as the exercises used in the studies of Salles et al. (2015) and Rogol et al. (1998), may be more effective in improving JPS.
Closed-chain exercises occur when the distal segment is fixed and supports body weight. Because the loading is usually axial and causes compression in the joint, closed-chain exercises are thought to promote co-contraction of the rotator cuff and scapulothoracic muscles, and to facilitate proprioception inputs (Davies & Dickoff-Hoffman, 1993; Lephart & Henry, 1996). If the distal segment is placed on an unstable surface, the exercise would also trigger feedback and feedforward corrective movements (Röijezon et al., 2015). While Rogol et al. (1998) found six weeks of a standard push-up improved JPS in healthy subjects, Padua et al. (2004) found no changes in JPS after five weeks of training with balance exercise on an unstable surface. Push-up exercises involve more dynamic multiple muscle contraction than the closed-chain exercises on an unstable surface. In our training protocol, the weight bearing over the shoulders was not as high as the intensity used by Rogol et al. (1998). Therefore, according to the results of the present study and previous studies for proprioception training, the intensity of dynamic muscle contraction may be more important than the training of sensory feedback and feedforward during the exercise.
Although in the present study strengthening exercises for rotator cuff and scapulothoracic muscles did not improve JPS in healthy subjects, there may still be an effect of strengthening exercise on JPS in subjects with shoulder injuries. Both Dilek et al. (2015) and Naughton et al. (2005) found the JPS improved after exercise training in the patients with shoulder impingement syndrome and patients with shoulder posterior dislocation. Therefore, because chronic pain and effusion may influence JPS centrally and peripherally (Röijezon et al., 2015), by reducing pain and decreasing symptoms with exercises (Littlewood, Ashton, Chance-Larsen, May, & Sturrock, 2012), JPS may be restored in patients with shoulder injuries. Future work is needed to investigate the mechanism of the improvement of JPS in the patients and whether the mechanism of improvement comes from the re-training of the sensorimotor system.
We investigated whether JPS during a functional activity would improve after open-chain and closed-chain exercise training, which facilitate proprioception during the exercise. While most previous studies used a protocol involving shoulder internal and external rotation. (Heiderscheit et al., 1996; Padua et al., 2004; Rogol et al., 1998; Salles et al., 2015; Swanik et al., 2002), in the present study, we chose to test JPS in shoulder elevation in the scapular plane. The movement of elevation is more functional than the movement of internal and external for the general population. This testing position of internal and external rotation may also block scapular movement and only test the GH joint. A systematic review and meta-analysis for the effects of shoulder injuries on proprioception showed that the difference in JPS between subjects with shoulder injuries and healthy subjects were found in external rotation and abduction (Fyhr, Gustavsson, Wassinger, & Sole, 2015), especially at a higher angle of abduction (Anderson & Wee, 2011). Shoulder abduction requires the coordination of the humerus and scapula. Thus, we tested the JPS of HT joint as well as the JPS of GH and ST joints. Although we did not find the difference in JPS after exercise training, future research may still need to investigate the effect of treatment on JPS of individual joints in shoulder abduction.
The duration of the exercise training may help explain why we found no improvement after the training. Although most of the force measures increased after the training, four weeks may not be sufficient for sensory adaptation. Moreover, for force measurement, although subjects were asked whether they needed more time for rest and whether they felt muscle fatigue or soreness, it is possible muscle fatigue influenced the results. Another limitation is that the subjects in the present study were young healthy students. The result of this present study may not be generalized to an older or injured population.
5. Conclusion
After four weeks of a rotator cuff and scapular strengthening training protocol, involving both closed-chain and open-chain exercises, subjects did not demonstrate improvements in JPS, compared to those in a control group. This is in contrast to previous studies (Rogol et al., 1998; Salles et al., 2015), which have demonstrated improvements with exercise including multiple large muscle group and higher intensity. Therefore, the types and intensity of the exercise may explain why there was no improvement in JPS in the present study. Future work is needed to investigate which types of exercise are more effective in improving JPS, and the mechanisms associated with those changes.
Highlights.
Subjects completed four weeks of open and closed chain shoulder exercises.
This comprehensive protocol resulted in significant increases in shoulder strength.
However, no improvements in shoulder joint position sense were observed.
It still remains to be seen whether joint position sense is modifiable in patients.
Acknowledgements
This study was supported by Evonuk Memorial Graduate Fellowship and partially funded by NIH grant 5R01AR063713-04. The authors would like to thank Kirby Tobin and David Phillips for their assistance with protocol testing.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alpert SW, Pink MM, Jobe FW, McMahon PJ, Mathiyakom W. Electromyographic analysis of deltoid and rotator cuff function under varying loads and speeds. Journal of Shoulder and Elbow Surgery. 2000;9:47–58. doi: 10.1016/s1058-2746(00)90009-0. [DOI] [PubMed] [Google Scholar]
- Anderson VB, Wee E. Impaired joint proprioception at higher shoulder elevations in chronic rotator cuff pathology. Archives of Physical Medicine and Rehabilitation. 2011;92:1146–1151. doi: 10.1016/j.apmr.2011.02.004. [DOI] [PubMed] [Google Scholar]
- Ashton-Miller JA, Wojtys EM, Huston LJ, Fry-Welch D. Can proprioception really be improved by exercises? Knee Surgery, Sports Traumatology, Arthroscopy. 2001;9:128–136. doi: 10.1007/s001670100208. [DOI] [PubMed] [Google Scholar]
- Borsa PA, Lephart SM, Kocher MS, Lephart SP. Functional assessment and rehabilitation of shoulder proprioception for glenohumeral instability. Journal of Sport Rehabilitation. 1994;3:84–104. [Google Scholar]
- Cools AM, Dewitte V, Lanszweert F, Notebaert D, Roets A, Soetens B, Cagnie B, Witvrouw EE. Rehabilitation of scapular muscle balance: which exercises to prescribe? American Journal of Sports Medicine. 2007;35:1744–1751. doi: 10.1177/0363546507303560. [DOI] [PubMed] [Google Scholar]
- Cricchio M, Frazer C. Scapulothoracic and scapulohumeral exercises: A narrative review of electromyographic studies. Journal of Hand Therapy. 2011;24:322–334. doi: 10.1016/j.jht.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Davies GJ, Dickoff-Hoffman S. Neuromuscular testing and rehabilitation of the shoulder complex. The Journal of Orthopaedic and Sports Physical Therapy. 1993;18:449–458. doi: 10.2519/jospt.1993.18.2.449. [DOI] [PubMed] [Google Scholar]
- Decker MJ, Hintermeister RA, Faber KJ, Hawkins RJ. Serratus anterior muscle activity during selected rehabilitation exercises. The American Journal of Sports Medicine. 1999;27:784–791. doi: 10.1177/03635465990270061601. [DOI] [PubMed] [Google Scholar]
- Decker MJ, Tokish JM, Ellis HB, Torry MR, Hawkins RJ. Subscapularis muscle activity during selected rehabilitation exercises. American Journal of Sports Medicine. 2003;31:126–134. doi: 10.1177/03635465030310010601. [DOI] [PubMed] [Google Scholar]
- Dilek B, Gulbahar S, Gundogdu M, Ergin B, Manisali M, Ozkan M, Akalin E. Efficacy of proprioceptive exercises in patients with subacromial impingement syndrome: A single-blinded randomized controlled study. American Journal of Physical Medicine and Rehabilitation. 2015 doi: 10.1097/PHM.0000000000000327. [DOI] [PubMed] [Google Scholar]
- Ekstrom RA, Soderberg GL, Donatelli RA. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. Journal of Electromyography and Kinesiology. 2005;15:418–428. doi: 10.1016/j.jelekin.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Ellenbecker TS, Cools A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: an evidence-based review. British Journal of Sports Medicine. 2010;44:319–327. doi: 10.1136/bjsm.2009.058875. [DOI] [PubMed] [Google Scholar]
- Fyhr C, Gustavsson L, Wassinger C, Sole G. The effects of shoulder injury on kinaesthesia: a systematic review and meta-analysis. Manual Therapy. 2015;20:28–37. doi: 10.1016/j.math.2014.08.006. [DOI] [PubMed] [Google Scholar]
- Heiderscheit BC, McLean KP, Davies GJ. The effects of isokinetic vs. plyometric training on the shoulder internal rotators. The Journal of Orthopaedic and Sports Physical Therapy. 1996;23:125–133. doi: 10.2519/jospt.1996.23.2.125. [DOI] [PubMed] [Google Scholar]
- King J, Harding E, Karduna A. The shoulder and elbow joints and right and left sides demonstrate similar joint position sense. Journal of Motor Behavior. 2013;45:479–486. doi: 10.1080/00222895.2013.832136. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Henry TJ. The physiological basis for open and closed kinetic chain rehabilitation for the upper extremity. Journal of Sport Rehabilitation. 1996;5:71–87. [Google Scholar]
- Lephart SM, Warner JJP, Borsa PA, Fu FH. Proprioception of the shoulder joint in healthy, unstable, and surgically repaired shoulders. Journal of Shoulder and Elbow Surgery. 1994;3:371–380. doi: 10.1016/S1058-2746(09)80022-0. [DOI] [PubMed] [Google Scholar]
- Lin J.-j., Hsieh S-C, Cheng W-C, Chen WC, Lai Y. Adaptive patterns of movement during arm elevation test in patients with shoulder impingement syndrome. Journal of Orthopaedic Research. 2011;29:653–657. doi: 10.1002/jor.21300. [DOI] [PubMed] [Google Scholar]
- Littlewood C, Ashton J, Chance-Larsen K, May S, Sturrock B. Exercise for rotator cuff tendinopathy: a systematic review. Physiotherapy. 2012;98:101–109. doi: 10.1016/j.physio.2011.08.002. [DOI] [PubMed] [Google Scholar]
- Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Physical Therapy. 2000;80:276–291. [PubMed] [Google Scholar]
- Machner A, Merk H, Becker R, Rohkohl K, Wissel H, Pap G. Kinesthetic sense of the shoulder in patients with impingement syndrome. Acta Orthopaedica Scandinavica. 2003;74:85–88. doi: 10.1080/00016470310013716. [DOI] [PubMed] [Google Scholar]
- Myers JB, Oyama S. Sensorimotor training for shoulder injury: Literature review. Athletic Training & Sports Health Care. 2009;1:199–208. [Google Scholar]
- Myers JB, Wassinger CA, Lephart SM. Sensorimotor contribution to shoulder stability: Effect of injury and rehabilitation. Manual Therapy. 2006;11:197–201. doi: 10.1016/j.math.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Naughton J, Adams R, Maher C. Upper-body wobbleboard training effects on the post-dislocation shoulder. Physical Therapy in Sport. 2005;6:31–37. [Google Scholar]
- Padua DA, Guskiewicz KM, Prentice WE, Schneider RE, Shields EW. The effect of select shoulder exercises on strength, active angle reproduction, single-arm balance, and functional performance. Journal of Sport Rehabilitation. 2004;13:75–95. [Google Scholar]
- Reddy AS, Mohr KJ, Pink MM, Jobe FW. Electromyographic analysis of the deltoid and rot tor cuff muscles in persons with subacromial impingement. Journal of Shoulder and Elbow Surgery. 2000;9:519–523. doi: 10.1067/mse.2000.109410. [DOI] [PubMed] [Google Scholar]
- Reinold MM, Escamilla RF, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. The Journal of Orthopaedic and Sports Physical Therapy. 2009;39:105–117. doi: 10.2519/jospt.2009.2835. [DOI] [PubMed] [Google Scholar]
- Reinold MM, Macrina LC, Wilk KE, Fleisig GS, Dun S, Barrentine SW, Ellerbusch MT, Andrews JR. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. Journal of Athletic Training. 2007;42:464–469. [PMC free article] [PubMed] [Google Scholar]
- Reinold MM, Wilk KE, Fleisig GS, Zheng N, Barrentine SW, Chmielewski T, Cody RC, Jameson GG, Andrews JR. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. The Journal of Orthopaedic and Sports Physical Therapy. 2004;34:385–394. doi: 10.2519/jospt.2004.34.7.385. [DOI] [PubMed] [Google Scholar]
- Riemann BL, Lephart SM. The sensorimotor system, part II: The role of proprioception in motor control and functional joint stability. Journal of Athletic Training. 2002;37:80–84. [PMC free article] [PubMed] [Google Scholar]
- Rogol IM, Ernst G, Perrin DH. Open and closed kinetic chain exercises improve shoulder joint reposition sense equally in healthy subjects. Journal of Athletic Training. 1998;33:315. [PMC free article] [PubMed] [Google Scholar]
- Röijezon U, Clark NC, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Manual Therapy. 2015;20:368–377. doi: 10.1016/j.math.2015.01.008. [DOI] [PubMed] [Google Scholar]
- Salles JI, Velasques B, Cossich V, Nicoliche E, Ribeiro P, Amaral MV, Motta G. Strength training and shoulder proprioception. Journal of Athletic Training. 2015;50:277–280. doi: 10.4085/1062-6050-49.3.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt RA, Lee TD. Motor control and learning: a behavioral emphasis. Human Kinetics; Champaign, IL: 2005. [Google Scholar]
- Smith RL, Brunolli J. Shoulder kinesthesia after anterior glenohumeral joint dislocation. Physical Therapy. 1989;69:106–112. doi: 10.1093/ptj/69.2.106. [DOI] [PubMed] [Google Scholar]
- Swanik CB, Lephart SM, Giannantonio FP, Fu FH. Reestablishing proprioception and neuromuscular control in the ACL-injured athlete. Journal of Sport Rehabilitation. 1997;5:162–206. [Google Scholar]
- Swanik KA, Lephart SM, Swanik CB, Lephart SP, Stone DA, Fu FH. The effects of shoulder plyometric training on proprioception and selected muscle performance characteristics. Journal of Shoulder and Elbow Surgery. 2002;11:579–586. doi: 10.1067/mse.2002.127303. [DOI] [PubMed] [Google Scholar]
- Ubinger ME, Prentice WE, Guskiewicz KM. Effect of closed kinetic chain training on neuromuscular control in the upper extremity. Journal of Sport Rehabilitation. 1999;8:184–194. [Google Scholar]
- Veeger HE. The position of the rotation center of the glenohumeral joint. Journal of Biomechanics. 2000;33:1711–1715. doi: 10.1016/s0021-9290(00)00141-x. [DOI] [PubMed] [Google Scholar]
- Woltring HJ, Huiskes R, de Lange A, Veldpaus FE. Finite centroid and helical axis estimation from noisy landmark measurements in the study of human joint kinematics. Journal of Biomechanics. 1985;18:379–389. doi: 10.1016/0021-9290(85)90293-3. [DOI] [PubMed] [Google Scholar]
- Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X, Werner FW, Buchholz B. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: shoulder, elbow, wrist and hand. Journal of Biomechanics. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]