Abstract
Background
Specific phobia (SP) is the most common anxiety disorder among children with Williams syndrome (WS); prevalence rates derived from DSM-based diagnostic interviews range from 37% – 56%. We evaluated the effects of gender, age, intellectual abilities, and/or behaviour regulation difficulties on the likelihood that a child with WS would be diagnosed with SP.
Methods
194 6 – 17-year-olds with WS were evaluated. To best characterize the relations between the predictors and the probability of a SP diagnosis, we explored not only possible linear effects but also curvilinear effects.
Results
No gender differences were detected. As age increased, the likelihood of receiving a SP diagnosis decreased. As IQ increased, the probability of receiving a SP diagnosis also decreased. Behaviour regulation difficulties were the strongest predictor of a positive diagnosis. A quadratic relation was detected: The probability of receiving a SP diagnosis gradually rose as behaviour regulation difficulties increased. However, once behaviour regulation difficulties approached the clinical range, the probability of receiving a SP diagnosis asymptoted at a high level.
Conclusion
Children with behaviour regulation difficulties in or just below the clinical range were at the greatest risk of developing SP. These findings highlight the value of large samples and the importance of evaluating for nonlinear effects to provide accurate model specification when characterizing relations among a dependent variable and possible predictors.
Keywords: Williams syndrome, specific phobia, behaviour regulation, curvilinear effects, intellectual disability, anxiety, logistic regression, Behavior Rating Inventory of Executive Functioning (BRIEF)
Specific phobia (SP) is the most common anxiety disorder among children (e.g., Beesdo et al. 2009). This diagnosis is made when a child demonstrates marked and excessive fear of a specific situation or object over a period of at least six months, causing interference in his or her everyday life and/or significant distress (American Psychiatric Association 2000, 2013). In the largest US epidemiological study of Diagnostic and Statistical Manual of Mental Disorders (DSM)-based disorders in children, Shaffer et al. (1996) found that 1.3% of 9 – 17-year-olds met diagnostic criteria for SP. In smaller general-population samples of children, point-prevalence rates of SP have ranged from 2% – 9%, with most estimates at about 3% (Weiss & Last 2001). Relative to the general population, SP is more common in individuals with developmental disabilities. In the largest community-based study of children and young adults with intellectual disabilities (ID), Dekker and Koot (2003) found that SP was the most frequent anxiety disorder, with a prevalence rate of 6.8% based on DSM-IV criteria including impairment in everyday functioning.
The prevalence of SP is considerably higher among children with certain neurodevelopmental disorders associated with ID (see Grahame & Rodgers, 2014 for review), including Williams syndrome (WS). WS, which occurs in 1/7500 live births (Strømme et al. 2002), is caused by a deletion of ~26 genes on chromosome 7q11.23 (Hillier et al. 2003) and is associated with ID and specific cognitive and personality profiles (see Mervis & Morris 2007 for review). SP is the most common anxiety disorder among children with WS; prevalence rates range from 37% – 56% based on DSM-based diagnostic interviews (Dykens 2003; Kennedy et al. 2006; Leyfer et al. 2006; Dodd & Porter 2009; Leyfer et al. 2009; Woodruff-Borden et al. 2010; Green et al. 2012; Zarchi et al. 2014). Direct comparisons of SP prevalence rates have documented that the rate for individuals with WS was significantly higher than for the general population (Leyfer et al. 2009; Zarchi et al. 2014) and for the Dekker and Koot (2003) sample of individuals with ID of mixed etiology (Leyfer et al. 2009). In the present study, we focused on a large cross-sectional sample of children with WS in order to better understand possible predictors of SP.
Predictors of Specific Phobia
Gender and age have been evaluated as possible predictors of SP both for children in the general population and for children with ID. In most general-population samples, the rate of SP was higher for females than for males (see Weiss & Last 2001; LeBeau et al. 2010 for review), although the difference often was not significant. Based on a literature review focused on individuals in the general population, LeBeau et al. (2010) noted that several types of SPs had higher prevalence rates among children than adults. Findings from a longitudinal study of clinically-referred 5 – 18-year-olds from the general population indicated that 69% of those who initially met diagnostic criteria for SP no longer did so 3 – 4 years later (Last et al. 1996). These findings suggest that for individuals in the general population, rate of SP may decline over time. In contrast, a different pattern of results was observed for the epidemiological study of 7 – 20-year-olds with ID. Dekker and Koot (2003) found no significant differences in rate of SP for females vs. males, 7 – 12-year-olds vs. 13 – 20-year-olds, or children with IQs of 50 – 80 vs. children with IQs of 30 – 49. This suggests that for individuals with ID rate of SP may remain stable as a function of age and IQ. Nevertheless, the rate is higher for individuals who have IQs of 80 or below than for children in the general population suggesting that diagnosis of SP may be related to IQ.
For individuals with WS, gender, age, and/or IQ were considered as possible predictors of a DSM-IV-TR diagnosis of SP in two cross-sectional studies (Kennedy et al. 2006; Leyfer et al. 2006) and one longitudinal study (Woodruff-Borden et al. 2010) and of a DSM-IV diagnosis of SP in one cross-sectional study (Dodd & Porter 2009). Relations between these factors and SP diagnosis did not reach statistical significance. However, the lack of significant differences for age and IQ might be due to insufficient power. Dodd and Porter (2009) reported that 37% of the 30 children in their sample but only 20% of the 20 adults met diagnostic criteria for SP. Leyfer et al. (2006) found a prevalence rate of 61% for 44 7 – 10-year-olds and 54% for 35 11 – 16-year-olds. Leyfer et al. also found that mean IQ was 5 points higher for children who did not have a SP diagnosis than for those who did. These trends for age and IQ highlight the importance of large samples to better understand the factors related to SP.
Behavioural Regulation and Specific Phobia
Difficulties in emotional regulation are thought to be related to the development and preservation of anxiety disorders, including SP (Thompson 2001; Jacob et al. 2011). When presented with a particular environmental stressor, individuals who have anxiety disorders may not be able to engage in an appropriate response or may be unable to suppress an inappropriate response (Thayler & Lane 2000). These patterns suggest deficits in effective self-regulatory strategies. These deficits may be related to difficulty in shifting attention from threatening stimuli (Amstadter 2008) and more generally in behaviour regulation (ability to shift cognitive sets, monitor, and inhibit behaviours and emotions), which supports processes that facilitate appropriate self-regulation (Gioia et al. 2000). In keeping with these difficulties, Dekker and Koot (2003) proposed that individuals with ID may have trouble coping with frightening situations, which in turn is likely to increase the risk of developing a SP.
Difficulties in behavioural regulation (Woodruff-Borden et al. 2010; Hocking et al. 2015) are common among individuals with WS, as are emotional problems (e.g. Davies et al. 1998; Klein-Tasman et al. 2015; Pérez-García et al. in press). For children with WS, impairment in metacognition (ability to initiate, plan, and maintain future-oriented problem solving in working memory; Gioia et al. 2000) and behavioural regulation have been reported. Woodruff-Borden et al. (2010) considered the relations of metacognition and behavioural regulation with SP in 33 children with WS as part of their longitudinal study of the stability of a diagnosis of SP. No differences in metacognition were found in children with and without SP, and no significant individual differences were detected. However, children with SP had significantly worse behavioural regulation abilities than did children without this diagnosis. Individual differences in behavioural regulation abilities were detected. In the present study, we sought to further characterise the relation between behavioural regulation difficulties and SP for children with WS.
The Present Study
Given the high prevalence of SP in children with WS and their heterogeneity in intellectual abilities (e.g. Pitts & Mervis 2016) and behavioural regulation, further consideration of cognitive and behavioural factors that may be related to the presence or absence of SP is warranted. In the present study, we focused on a large cross-sectional sample of children with WS aged 6 – 17 years (N = 194). We considered age, gender, intellectual abilities, and behavioural regulation difficulties as possible predictors of SP diagnosis. A block-wise logistic regression analysis was conducted. We first addressed whether the probability that a child would be diagnosed with SP varied as a function of age and/or gender. We next determined if the probability of receiving a SP diagnosis varied as a function of intellectual abilities and/or behavioural regulation. In order to best characterise this relation, possible curvilinear effects (nonlinear patterns) were explored.
Method
Participants
The final sample included 194 children (100 girls, 94 boys) with WS, aged 6.01 – 17.98 years (M = 10.72, SD = 3.38). This was a community-based sample representing 38 states in the US, 2 Canadian provinces, and the UK. Most participants were recruited for a study of language, cognitive, and behavioural development conducted at the University of Louisville; the remaining participants were recruited for a study of executive function and emotion regulation at the University of Wisconsin-Milwaukee. The procedures were approved by the universities’ Institutional Review Boards. Some children were assessed multiple times as part of a longitudinal study. For these children, data from the most recent assessment were used. The inclusion criteria were: (1) genetically-confirmed classic-length deletion of the WS region and (2) either no anxiety disorder diagnosis or SP diagnosis without any other anxiety diagnosis. Five additional children who met inclusion criteria were excluded from the final sample because examination of standardised Cook’s Distance identified these children as inappropriately influential cases (see Data Analysis).
Materials
Anxiety Disorders Interview Schedule: Parent Version (ADIS-P; Silverman & Albano 1996)
The ADIS-P for DSM-IV is a semi-structured parent interview used to assess the presence of anxiety and related disorders in children. The ADIS-P has demonstrated favourable psychometric properties with typically developing children (Silverman et al. 2001) and children with ASD (e.g. Storch et al. 2012; Wood et al. 2009).
Behavior Rating Inventory of Executive Functioning, parent form (BRIEF; Gioia et al. 2000)
The BRIEF is a questionnaire used to evaluate executive functioning behaviours of children. We focused on the Behavioural Regulation Index (BRI), which measures the child’s ability to inhibit prepotent behaviours, monitor his or her emotions and behaviours, and shift cognitive processes and attention. For the general-population, mean T-score is 50 (SD = 10), with a range from 30 – 100. Higher scores are associated with greater difficulties. T-scores of 65 and above are considered by the test authors to be clinically elevated. The BRI scale showed high internal consistency (Cronbach’s α = .94 – .96) and good test-retest reliability (.80 – .84) for both the norming and clinical samples (Gioia et al. 2000).
Kaufman Brief Intelligence Test, second edition (KBIT-2; Kaufman & Kaufman 2004)
The KBIT-2 IQ Composite measures general intelligence and is based on performance on verbal and nonverbal scales. For the general-population, mean standard score (SS) is 100 (SD = 15), with a range from 40 – 160. IQ Composite demonstrated high internal consistency (α = .92) and good test-retest reliability (.88 – .89) for the norming sample (Kaufman & Kaufman, 2004).
Procedures
Parents completed the BRIEF. The ADIS-P was administered to the parents by a clinical psychology doctoral student, a licensed clinical psychologist, or a developmental paediatrician. Consistent with DSM-IV-TR criteria, a SP diagnosis was made only if the phobia caused both interference and distress in the child. The child’s developmental level was considered in determining if diagnostic criteria for SP was met. All interview protocols were reviewed by a licensed clinical psychologist; agreement on whether or not the participant should be diagnosed with SP was 100%. Each child was administered the KBIT-2 according to the standardised procedures.
Data Analysis
To evaluate if the likelihood that a child would be diagnosed with SP varied as a function of his or her age, gender, intellectual abilities, and/or behaviour regulation difficulties, logistic regressions were conducted. Logistic regression measures the likelihood of a binary variable occurring (e.g. presence or absence of SP diagnosis). The following equation is estimated in logistic regression:
The dependent variable, or logit, is the natural logarithm of the odds of a child receiving a diagnosis of SP. The intercept, b0, is the log odds of a positive diagnosis of SP for the average child in the sample. The slope, b1, is the effect of X1 (the first independent variable) on the log odds of a positive diagnosis. To allow for a more intuitive exploration of the nature of the effects, logits can be converted to conditional probabilities using the following equation:
This conversion allows effects to be interpreted in terms of the predicted probabilities (% chance) that a child would be diagnosed with SP.
Presence or absence of SP was the dependent variable. KBIT-2 IQ Composite and BRIEF BRI T-score were included as independent variables. Age and gender were included as covariates. Gender was recoded so that female was the reference group (female = 0; male = 1). As is recommended for continuous variables (Osborne 2015, 2017), age, IQ Composite, and BRI T-scores were each converted to a standard normal distribution (i.e., transformed to Z-scores with a mean of 0 and SD of 1). Converting the variables to the same metric allows for the effects of the predictors to be directly compared and centers each continuous variable on the sample mean. Z-scored variables can also be converted back to the original metric by:
Logistic regression assumes that independent variables are additive in nature. This assumption may be violated if interactions or curvilinear effects are present but not modeled. Evaluating the data for possible interactions and nonlinear effects helps to ensure correct model specification. Furthermore, inclusion of these effects often yields more accurate models of the data (Osborne 2015, 2017). Therefore, possible curvilinear (quadratic) effects of IQ Composite and BRI T-score were examined. Testing for curvilinear effects allowed us to explore whether a nonlinear relation was present between intellectual abilities and/or behavioural regulation difficulties and rate of diagnosis of SP.
Variables were entered block-wise. After each block, likelihood ratio tests evaluated whether the added blocks of variables significantly improved the model fit. Age and gender were included in block 1. The linear main effects of IQ Composite and BRI T-score were included in block 2. Squared versions of IQ Composite and BRI T-score were entered in block 3.
Logistic regression is particularly impacted by influential cases when evaluating interaction terms and curvilinear trends (Osborne 2015, 2017). In order to evaluate the presence of influential cases, a preliminary regression for the full quadratic model was conducted. Cook’s Distance was calculated and then converted to a standard normal distribution. Five cases were considered to have inappropriate levels of influence (standardised Cook’s Distance greater than |3.5| SDs from the mean; see Osborne 2017) and were removed from the sample.
Correlations between predictors confirmed that no collinearity issues were present.1
Results
Descriptive Statistics
Based on the ADIS-P interview, 108 of the 194 children (55.67%) met diagnostic criteria for SP. These included 49 of the 94 boys (52.13%) and 59 of the 100 girls (59.00%). Descriptive statistics for age, IQ Composite, and BRI T-score are reported in Table 1. IQ Composite varied from moderate-to-severe ID to average for the general population, with a mean in the borderline range. BRI T-scores varied from average for the general population to clinical, with a mean in the elevated range.
Table 1.
Descriptive Statistics for Age, KBIT-2 IQ Composite, and BRIEF Behavior Regulation Index (BRI) T-score as a Function of Specific Phobia Diagnosis
| No Anxiety (N = 86) | Specific Phobia (N = 108) | Full Sample (N = 194) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Range | Mean | Median | SD | Range | Mean | Median | SD | |
| Age | 11.38 | 10.47 | 3.56 | 6.01 – 17.98 | 10.19 | 9.35 | 3.15 | 6.03 – 17.95 | 10.72 | 10.04 | 3.38 |
| IQ Composite | 77.06 | 80.00 | 15.22 | 47 – 106 | 71.31 | 71.50 | 13.99 | 40 – 104 | 73.75 | 73.50 | 14.80 |
| BRI T-score | 60.69 | 59.50 | 11.61 | 39 – 91 | 65.42 | 64.00 | 9.46 | 46 – 88 | 63.32 | 62.00 | 10.70 |
Logistic Regression
Block 1: Age and Gender
Whether or not the likelihood of receiving a diagnosis of SP varied as a function of age and gender was evaluated. Entry of age and gender into the model significantly improved model fit (null −2 log likelihood (−2LL) = 266.40, final −2LL = 259.21, χ2(2) = 7.19, p < .027). As indicated in block 1 of Table 2, the likelihood of receiving a SP diagnosis was significantly related to age (p < .014).2 No significant gender differences were detected (p < .26).3
Table 2.
Linear and Quadratic Logistic Regression Analyses of the Effects of Age, Gender, IQ Composite, and BRI T-score on Probability of Receiving a Specific Phobia Diagnosis
| B | SE | Wald (df=1) |
P-value | Odds Ratio | 95 % CI | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Block 1: COVARIATES | |||||||
| aAge | −0.37 | 0.15 | 6.09 | 0.014 | 0.69 | 0.52 | 0.93 |
| Gender | −0.33 | 0.30 | 1.26 | 0.262 | 0.72 | 0.40 | 1.28 |
| Intercept | 0.40 | 0.21 | 3.65 | 0.056 | 1.49 | ||
| Block 2: LINEAR MODEL | |||||||
| aAge | −0.41 | 0.16 | 6.81 | 0.009 | 0.66 | 0.48 | 0.90 |
| Gender | −0.41 | 0.31 | 1.73 | 0.188 | 0.67 | 0.36 | 1.22 |
| aIQ Composite | −0.42 | 0.17 | 6.39 | 0.011 | 0.66 | 0.47 | 0.91 |
| aBRI T-score | 0.41 | 0.17 | 6.02 | 0.014 | 1.51 | 1.09 | 2.09 |
| Intercept | 0.45 | 0.22 | 4.28 | 0.038 | 1.57 | ||
|
Block 3: QUADRATIC MODEL |
|||||||
| aAge | −0.36 | 0.16 | 4.90 | 0.027 | 0.70 | 0.51 | 0.96 |
| Gender | −0.45 | 0.32 | 1.99 | 0.158 | 0.64 | 0.34 | 1.19 |
| aIQ Composite | −0.49 | 0.18 | 7.76 | 0.005 | 0.61 | 0.43 | 0.86 |
| aBRI T-score | 0.56 | 0.19 | 8.73 | 0.003 | 1.74 | 1.21 | 2.52 |
| aBRI T-score2 | −0.45 | 0.16 | 7.79 | 0.005 | 0.64 | 0.47 | 0.88 |
| Intercept | 0.86 | 0.27 | 10.33 | 0.001 | 2.37 | ||
All continuous variables were z-scored.
Note: BRI = Behavior Regulation Index; CI = Confidence Interval
To better explore the nature of the effect of age, logits were converted to conditional probabilities. As indicated in Figure 1, as age increased, the likelihood of receiving a diagnosis of SP decreased. For example, after controlling for gender, a child aged 7 years (1 SD below the sample mean age) had a 68% chance of receiving a SP diagnosis whereas a child aged 14 years (1 SD above the sample mean age) had a 51% chance of receiving a SP diagnosis.
Figure 1.
Predicted probability of receiving diagnosis of specific phobia as a function of chronological age after controlling for gender. Age in years is displayed on the bottom x-axis and the corresponding z-scored ages are displayed on the top x-axis. (Note: Logits were converted to conditional probabilities.)
Block 2: Linear Main Effects
Age and gender were retained as covariates. IQ Composite and BRI T-score were entered to evaluate the linear effects. Model fit significantly improved (−2LL = 243.71, χ2(2) = 15.54, p < .001). As indicated in block 2 of Table 2, the linear effects of IQ, BRI, and age were significant predictors of SP diagnosis, after controlling for all other variables. Thus, age, IQ, and BRI T-score each differed significantly as a function of SP diagnosis, after holding all other variables constant.
Block 3: Quadratic Model
Possible curvilinear relations between the probability of receiving a diagnosis of SP and intellectual abilities or behaviour regulation difficulties were explored. Squared versions of IQ Composite and BRI T-score were created and entered separately in block 3. When the quadratic term for IQ was entered into the equation, the −2LL reduced from 243.71 to 241.81. Model fit did not improve (χ2(1) = 1.91, p < .17). The quadratic term was not significant (b = −0.19, SEb = 0.15, p < .18). To improve model specification, the quadratic effect of IQ was removed.
Next, the curvilinear effect of BRI T-score was considered. When the BRI quadratic term was included the −2LL reduced from 243.71 to 234.66, significantly improving the model (χ2(1) = 9.08, p < .003). Thus, the quadratic effect of BRI was retained. As indicated in block 3 of Table 2, there were significant linear effects of age, IQ Composite, and BRI T-score and a significant quadratic effect of BRI T-score. Examination of the regression coefficients suggested that BRI T-score was the strongest predictor of the presence or absence of SP.
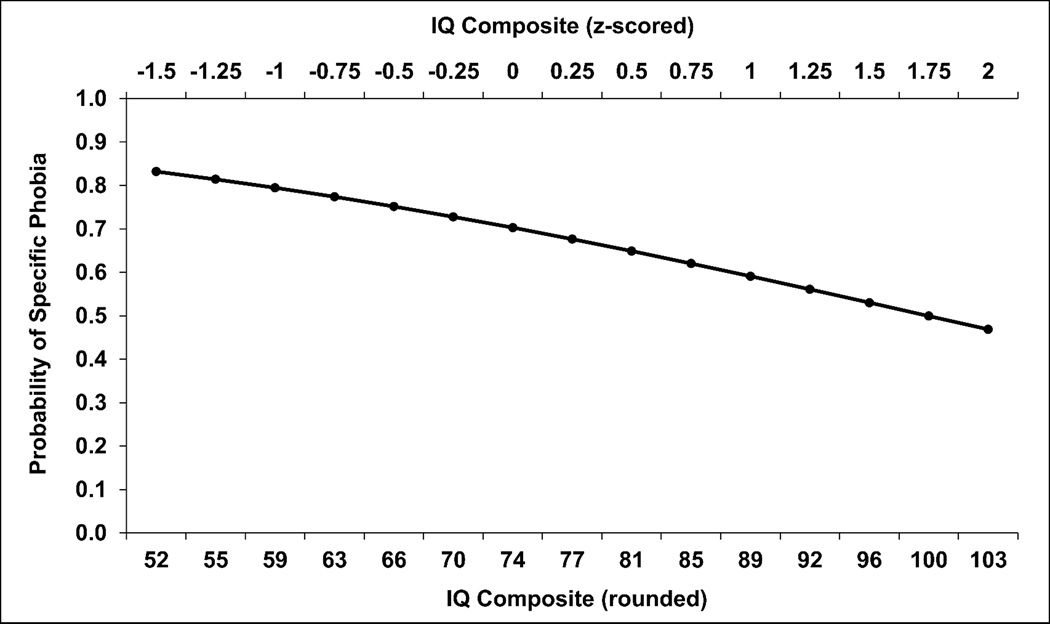
As indicated in Figure 2, as IQ Composite increased, the probability of receiving a SP diagnosis decreased. When converted to conditional probabilities, a child with an IQ of 52 (1.5 SD below the sample mean) had an 83% chance of receiving a SP diagnosis whereas a child with an IQ of 96 (1.5 SD above the sample mean) had a 53% chance, after controlling for BRI T-score, age, and gender.
Figure 2.
Predicted probability of receiving a diagnosis of specific phobia as a function of IQ Composite after controlling for Behavior Regulation Index (BRI) T-score, age, and gender. IQ Composite standard scores (SSs) are displayed on the bottom x-axis (rounded to the nearest whole number), and the corresponding z-scored IQ Composite SSs are displayed on the top x-axis. (Note: Logits were converted to conditional probabilities.)
As indicated in Figure 3, the probability of being diagnosed with SP gradually rose as BRI T-score moved toward the clinical range (behaviour regulation difficulties increased). When BRI T-scores reached the clinical range (T-score of 65), the likelihood of receiving a diagnosis of SP began to asymptote at a high level. A child with a BRI T-score of 50 (1.25 SD below the sample mean) had a 37% chance of receiving a SP diagnosis after controlling for gender, age, and IQ, whereas a child with a BRI T-score of 63 (sample mean and intercept) had a 70% chance and a child with a BRI T-score of 77 (1.25 SD above the sample mean) also had a 70% chance.4
Figure 3.
Predicted probability of receiving a diagnosis of specific phobia as a function of Behavior Regulation Index (BRI) T-score after controlling for IQ Composite, age, and gender. BRI T-scores are displayed on the bottom x-axis (rounded to the nearest whole number), and the corresponding z-scored BRI T-scores are displayed on the top x-axis. (Note: Logits were converted to conditional probabilities.
Discussion
The present study evaluated the relations of gender, age, intellectual abilities, and behaviour regulation difficulties to the probability of receiving a SP diagnosis for children and adolescents with WS. The sample size was considerably larger than that of previous studies of SP in individuals with WS. Results indicated that gender was not significantly related to the likelihood of receiving a diagnosis of SP. In contrast, even after controlling for the effects of each of the remaining independent variables, age, intellectual abilities, and behavioural regulation difficulties each had a significant effect on the probability of a diagnosis of SP. That is, after controlling for the effects of gender, IQ, and BRI, as age increased, the probability of SP diagnosis decreased significantly. Similarly, after holding all other variables constant, as intellectual abilities increased the probability of SP diagnosis decreased significantly. The strongest relation was found for BRI, after controlling for gender, age, and IQ. Importantly, our examination of curvilinear effects revealed that this relation was quadratic rather than linear: As behavioural regulation difficulties increased, the probability of SP diagnosis also increased until behavioural regulation difficulties approached the clinical level identified by the authors of the BRIEF (Gioia et al. 2000). At that point, the probability asymptoted at a high level. In the remainder of the Discussion we consider these findings in relation to prior literature and address the importance of evaluating for nonlinear effects. The implications of these patterns and the limitations of the study also are addressed.
Gender and Age
The prevalence of SP among the participants in the present study was quite high, with similar rates for girls and boys. This finding fits with those of previous studies that used DSM-based diagnostic parent interviews to assess SP in individuals with WS (Kennedy et al. 2006; Leyfer et al. 2006; Dodd & Porter 2009; Leyfer et al. 2009; Woodruff-Borden et al. 2010; Green et al. 2012; Zarchi et al. 2014). Our finding that the likelihood of a SP diagnosis decreased as age increased is consistent with the pattern observed in children in the general population (e.g., Last et al. 1996). It also is consistent with the nonsignificant trend observed in two prior studies of individuals with WS (Dodd & Porter 2006; Leyfer et al. 2006), suggesting that these studies likely were underpowered.
Intellectual Abilities
Our finding that as intellectual abilities increased, the probability of a SP diagnosis decreased fits with the results of prior epidemiological studies indicating that the prevalence of SP in children in the general population (Shaffer et al. 1996) is lower than that for children with ID of mixed etiology (Dekker & Koot 2003). This result also is consistent with Leyfer et al.’s (2006) finding that mean IQ was 5 points lower for children with WS who had a SP diagnosis than for those who did not, which did not reach significance, most likely due to inadequate power. Similarly, Cordeiro et al. (2011) found that individuals with fragile X syndrome and ID (IQ < 70) had a significantly higher rate of SP (71%) than those without ID (43%). Dekker and Koot (2003) suggest that the higher prevalence of SP among individuals with ID may be due to both difficulties in reality testing and lower self-confidence. These problems may increase the likelihood of development of an unreasonable or irrational fear of a specific situation or object.
Behavioural Regulation
In the present study, behavioural regulation difficulties (as measured by BRIEF BRI) were the strongest predictor of a positive diagnosis of SP, after taking into account gender, age, and intellectual abilities. The relation between BRI and diagnosis of SP was quadratic rather than linear, indicating that the probability of being diagnosed with SP gradually rose as behavioural regulation difficulties approached the clinical range. Once the clinical range of behavioural dysregulation was reached, the probability of receiving a SP diagnosis asymptoted at a high level. Overall, children with behavioural regulation difficulties at or above the clinical range of the BRIEF BRI T-score were at the greatest risk of developing a SP. This finding expands on that of Woodruff-Borden et al. (2010), who found that in a longitudinal sample of 33 children with WS, those who had a SP diagnosis had significantly higher (worse) BRI T-scores than those who did not. The current study replicated and further characterised the nature of the association between SP and BRI in a much larger cross-sectional sample, while accounting for gender, age, and IQ.
In line with theories of the development of SP (e.g., Thayler & Lane 2000; Thompson 2001; Amstadter 2008; Jacob et al. 2011), the present finding suggests that impairments in behavioural regulation make it difficult for individuals to self-regulate and shift attention when presented with a situation that is perceived as threatening. In turn, this difficulty increases the likelihood that an unreasonable or irrational fear of a specific situation or object may develop. There is evidence that behaviour regulation difficulties may contribute to poorer anxiety treatment outcomes (Halldorsdottir et al. 2015). Thus, alongside traditional exposure techniques for treating SP, it likely is critical to maintain an awareness of the underlying behavioural regulation challenges of many children with WS and to scaffold self-regulation to further develop these skills. Future research examining the effects of behavioural regulation interventions on the rates of fears and phobias in children with WS is warranted. Early identification and treatment of behaviour regulation difficulties also may be an important route to prevention or minimisation of fears and phobias.
Importance of Evaluating for Interactions and Curvilinear Effects
Examination of curvilinear effects allowed for a more accurate representation of the effect of behavioural regulation difficulties (BRIEF BRI) on SP diagnosis. Constraining BRI to follow a linear relation would have obscured this pattern, yielding predicted probabilities that would have been considerably less representative of the actual data. Often, researchers presume relations are linear without validating this assumption. However, if interactions or curvilinear effects are present but not modeled, the reported results are likely to be misleading and to violate assumptions. The findings from the current study support the importance of modeling curvilinear effects for accurate characterization of the data, yielding a better understanding of the relations between variables (Osborne 2015, 2017).
Limitations
Although the sample size for the present study was considerably larger than for any previous study of SP in individuals with WS, it still was relatively small for evaluating curvilinear effects and interactions. Complex terms tend to have lower power and are generally harder to detect (Osborne 2015, 2017). Accordingly, even larger sample sizes are likely needed to detect more subtle curvilinear effects and interactions among the dependent variables we considered. Although we did not detect curvilinear effects of age or IQ, it is likely that these effects on the probability of SP diagnosis are not as simple as a linear decline. These effects likely eventually stabilize, perhaps by early adulthood and among individuals with intellectual abilities at least in the low average range. Furthermore, although an interaction between BRI and IQ was not detected in the present sample, it is possible that the effect of IQ on SP diagnosis is moderately influenced by the effect of behaviour regulation difficulties. These limitations, along with our demonstration of the considerably more accurate understanding of the relation between behaviour regulation difficulties and the probability of a diagnosis of SP obtained by modeling the curvilinear effect, highlight both the need for replication of previous findings and the importance of large sample sizes to best characterize the phenotypes associated with WS and other syndromes. In order to evaluate the generalisability of the current findings to other syndromes that have elevated rates of SP (e.g., autism spectrum disorder, 7q11.23 duplication syndrome, fragile X syndrome), cross-syndrome comparisons of the predictors associated with SP should be conducted. These could further speak to possible mechanisms for SP across and within syndromes.
In conclusion, the present study demonstrated that for children with WS age, intellectual abilities, and behavioural regulation difficulties each has a significant effect on the likelihood of receiving a diagnosis of SP, even after controlling for the effects of the remaining independent variables. The largest effect was for behaviour regulation difficulties, and this effect was nonlinear (quadratic): After controlling for all other independent variables the likelihood of a SP diagnosis increased gradually until behavioural regulation difficulties approached the clinical range and then asymptoted at a very high level. These findings highlight the value of large samples and the importance of evaluating for nonlinear effects to provide accurate model specification when characterising relations among a dependent variable and possible predictors. They also support consideration of treatment of behavioural regulation difficulties as an approach to improving the adaptive behaviour of children with WS.
Acknowledgments
The authors would like to thank the many children and their parents who have participated in our research. This research was supported by grants from the National Institute of Child Health and Human Development (#R37 HD29957), the National Institute of Neurological Disorders and Stroke (#R01 NS35102), the Williams Syndrome Association (#WSA 0104), and the Center for Addiction and Behavioral Health at the University of Wisconsin – Milwaukee.
Footnotes
The strongest correlation was between IQ Composite and BRI T-score, r = −.17, p < .021.
The interaction between age and gender also was evaluated. No significant interaction was detected (b = 0.11, SEb = 0.30, p < .72).
The quadratic (curvilinear) effect of age also was evaluated. This effect was not significant (b = −0.07, SEb = 0.16, p < .68).
The possibility of an interaction between intellectual abilities and behaviour regulation difficulties on the probability of a child receiving a specific phobia diagnosis was evaluated in a separate preliminary analysis. Two cases were considered to have inappropriate levels of influence because standardised Cook’s Distance was greater than |3.5| standard deviations from the mean. These two cases were removed from the analysis. For block 1 and block 2, an identical pattern of results was observed. The interaction between IQ Composite and BRI T-score was entered in block 3. The interaction did not significantly improve model fit (χ2(1) = 3.35, p < .067). No significant interaction was detected (b = −0.31 SEb = 0.17, p < .075). Thus, the effect of IQ did not have a significant influence on the effect of behavioural regulation difficulties.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Arlington, VA: Author; 2000. text revision. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: Author; 2013. text revision. [Google Scholar]
- Amstadter A. Emotion regulation and anxiety disorders. Journal of Anxiety Disorders. 2008;22:211–221. doi: 10.1016/j.janxdis.2007.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordeiro L, Ballinger E, Hagerman R, Hessl D. Clinical assessment of DSM-IV anxiety disorders in fragile X syndrome: prevalence and characterization. Journal of Neurodevelopmental Disorders. 2011;3:57–67. doi: 10.1007/s11689-010-9067-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies M, Udwin O, Howlin P. Adults with Williams syndrome. Preliminary study of social, emotional and behavioural difficulties. The British Journal of Psychiatry. 1998;172:273–276. doi: 10.1192/bjp.172.3.273. [DOI] [PubMed] [Google Scholar]
- Dekker MC, Koot HM. DSM-IV disorders in children with borderline to moderate intellectual disability, I: Prevalence and impact. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:915–922. doi: 10.1097/01.CHI.0000046892.27264.1A. [DOI] [PubMed] [Google Scholar]
- Dodd HF, Porter MA. Psychopathology in Williams syndrome: The effect of individual differences across the life span. Journal of Mental Health Research in Intellectual Disabilities. 2009;2:89–109. [Google Scholar]
- Dykens EM. Anxiety, fears, and phobias in persons with Williams syndrome. Developmental Neuropsychology. 2003;23:291–316. doi: 10.1080/87565641.2003.9651896. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function: BRIEF. Odessa, FL: Psychological Assessment Resources; 2000. [Google Scholar]
- Grahame V, Rodgers J. Anxiety in neurodevelopmental disorders: Phenomenology, assessment, & intervention. In: Van Herwegen J, Riby D, editors. Neurodevelopmental disorders: Research challenges and solutions. New York, NY: Psychology Press; 2014. pp. 268–288. [Google Scholar]
- Green T, Avda S, Dotan I, Zarchi O, Basel-Vanagaite L, Zalsman G, et al. Phenotypic psychiatric characterization of children with Williams syndrome and response of those with ADHD to methylphenidate treatment. American Journal of Medical Genetics Part. B. Neuropsychiatric Genetics. 2012;159:13–20. doi: 10.1002/ajmg.b.31247. [DOI] [PubMed] [Google Scholar]
- Halldorsdottir T, Ollendick TH, Ginsburg G, Sherrill J, Kendall PC, Walkup J, et al. Treatment outcomes in anxious youth with and without comorbid ADHD in the CAMS. Journal of Clinical Child and Adolescent Psychology. 2015;44:985–991. doi: 10.1080/15374416.2014.952008. [DOI] [PubMed] [Google Scholar]
- Hillier LW, Fulton RS, Fulton LA, Graves TA, Pepin KH, Wagner-McPherson C, et al. The DNA sequence of chromosome 7. Nature. 2003;424:157–164. doi: 10.1038/nature01782. [DOI] [PubMed] [Google Scholar]
- Hocking DR, Reeve J, Porter MA. Characterising the profile of everyday executive functioning and relation to IQ in adults with Williams syndrome: Is the BRIEF Adult version a valid rating scale? PloS ONE. 2015;10:e0137628. doi: 10.1371/journal.pone.0137628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob ML, Thomassin K, Morelen D, Suveg C. Emotion regulation in childhood anxiety. In: McKat D, Storch E, editors. Handbook of Child and Adolescent Anxiety Disorders. New York, NY: Springer; 2011. pp. 171–185. [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test, second edition. Circle Pines, MN: American Guidance Services; 2004. [Google Scholar]
- Kennedy JC, Kaye DL, Sadler LS. Psychiatric diagnoses in patients with Williams syndrome and their families. Jefferson Journal of Psychiatry. 2006;20:22–31. [Google Scholar]
- Klein-Tasman BP, Lira EN, Li-Barber KT, Gallo FJ, Brei NG. Parent and teacher perspectives about problem behavior in children with Williams syndrome. American Journal on Intellectual and Developmental Disabilities. 2015;120:72–86. doi: 10.1352/1944-7558-120.1.72. [DOI] [PubMed] [Google Scholar]
- Last CG, Perrin S, Hersen M, Kazdin AE. A prospective study of childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1502–1510. doi: 10.1097/00004583-199611000-00019. [DOI] [PubMed] [Google Scholar]
- LeBeau RT, Glenn D, Liao B, Wittchen HU, Beesdo-Baum K, Ollendick T, et al. Specific phobia: a review of DSM-IV specific phobia and preliminary recommendations for DSM-V. Depression and Anxiety. 2010;27:148–167. doi: 10.1002/da.20655. [DOI] [PubMed] [Google Scholar]
- Leyfer OT, Woodruff-Borden J, Klein-Tasman BP, Fricke JS, Mervis CB. Prevalence of psychiatric disorders in 4 to 16-year-olds with Williams syndrome. American Journal of Medical Genetics Part B. 2006;141B:615–622. doi: 10.1002/ajmg.b.30344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyfer O, Woodruff-Borden J, Mervis CB. Anxiety disorders in children with Williams syndrome, their mothers, and their siblings: Implications for the etiology of anxiety disorders. Journal of Neurodevelopmental Disorders. 2009;1:4–14. doi: 10.1007/s11689-009-9003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervis CB, Morris CA. Williams syndrome. In: Mazzocco MMM, Ross JL, editors. Neurogenetic Developmental Disorders: Variation of Manifestation in Childhood. Cambridge, MA: MIT Press; 2007. pp. 199–262. [Google Scholar]
- Osborne JW. Best Practices in Logistic Regression. Thousand Oaks, CA: SAGE Publications; 2015. [Google Scholar]
- Osborne JW. Regression and Linear Modeling: Best Practices and Modern Methods. Thousand Oaks, CA: SAGE Publications; 2017. [Google Scholar]
- Pérez-García D, Brun-Gasca C, Pérez-Jurado L, Mervis C. Behavioral profiles of 6 – 14 year-old Children with Williams syndrome from Spain and the United States: Cross-cultural similarities and differences. American Journal on Intellectual and Developmental Disabilities. doi: 10.1352/1944-7558-122.2.156. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitts CH, Mervis CB. Performance on the Kaufman Brief Intelligence Test-2 by children with Williams syndrome. American Journal on Intellectual and Developmental Disabilities. 2016;121:33–47. doi: 10.1352/1944-7558-121.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davies M, Piacentini J, Schwab-Stone ME, et al. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:865–877. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV: Parent Interview Schedule. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Storch EA, Ehrenreich May J, Wood JJ, Jones AM, De Nadai AS, Lewin AB, Murphy TK. Multiple informant agreement on the Anxiety Disorders Interview Schedule in youth with autism spectrum disorders. Journal of Child and Adolescent Psychopharmacology. 2012;22:292–299. doi: 10.1089/cap.2011.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strømme P, Bjørnstad PG, Ramstad K. Prevalence estimation of Williams syndrome. Journal of Child Neurology. 2002;17:269–271. doi: 10.1177/088307380201700406. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders. 2000;61:201–216. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- Thompson RA. Childhood anxiety disorders from the perspective of emotion regulation and attachment. In: Vasey MW, Dadds MR, editors. The Developmental Psychopathology of Anxiety. New York, NY: Oxford University Press; 2001. pp. 160–182. [Google Scholar]
- Weiss DD, Last CG. Developmental variations in the prevalence and manifestation of anxiety disorders. In: Vasey MW, Dadds MR, editors. The Developmental Psychopathology of Anxiety. New York, NY: Oxford University Press; 2001. pp. 27–42. [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Clinical Child and Adolescent Psychology. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Woodruff-Borden J, Kistler DJ, Henderson DR, Crawford NA, Mervis CB. Longitudinal course of anxiety in children and adolescents with Williams syndrome. American Journal of Medical Genetics Part C. 2010;154:277–290. doi: 10.1002/ajmg.c.30259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarchi O, Diamond A, Weinberger R, Abbott D, Carmel M, Frisch A, et al. A comparative study of the neuropsychiatric and neurocognitive phenotype in two microdeletion syndromes: Velocardiofacial (22q11. 2 deletion) and Williams (7q11. 23 deletion) syndromes. European Psychiatry. 2014;29:203–210. doi: 10.1016/j.eurpsy.2013.07.001. [DOI] [PubMed] [Google Scholar]