Abstract
Objective
Reports on the finding from a six-year follow-up of a randomized trial of the Family Bereavement Program (FBP) on outcomes for spousally-bereaved parents.
Method
Spousally-bereaved parents (N=131) participated in the trial in which they were randomly assigned to receive the FBP (N = 72) or literature control (LC, N = 59). Parents were assessed at four time points, pre-test, post-test, 11-months, and six-year follow-up. Parents reported on mental health problems, grief and parenting at all four time periods. At the six-year follow-up parents reported on additional measures of persistent complex bereavement disorder, alcohol abuse problems, and coping efficacy.
Results
Bereaved parents in the FBP as compared to those in the LC had lower levels of symptoms of depression, general psychiatric distress, prolonged grief, alcohol problems, and higher coping efficacy at the six-year follow-up. Multiple characteristics of the parent (e.g., gender, age, baseline mental health problems) and of the spousal death (e.g., cause of death) were tested as moderators of program effects on each outcome. Latent-growth modeling found that the effects of the FBP on depression, psychiatric distress and grief occurred immediately following program participation and were maintained over six-years. Mediation analysis found that improvement in positive parenting partially mediated program effects to reduce depression and psychiatric distress, but had an indirect effect to higher levels of grief at the six years follow-up. Mediation analysis also found that improved parenting at the six year follow-up was partially mediated by program effects to reduce depression and that program effects to increase coping efficacy at the six-year follow-up was partially mediated through reduced depression and grief and improved parenting.
Conclusions
FBP reduced mental health problems, prolonged grief and alcohol abuse and increased coping efficacy of spousally-bereaved parents six years later. Mediation pathways for program effects differed across outcomes at the six-year follow-up.
Introduction
When families experience major family transitions such as parental death or divorce both children and their parents experience an increased risk for problem outcomes (e.g., Braver, Shapiro & Goodman, 2005; Melhem, Walker, Moritz & Brent, 2008). Prevention programs for these families have the opportunity to have a “double preventive effect” by improving outcomes for both parents and children. Randomized trials of parenting-focused preventive interventions with families who experienced divorce or separation have reported significant effects to reduce parents’ depressive symptoms, as well as to reduce children’s problem outcomes (e.g., DeGarmo, Patterson & Forgatch, 2004; Haine, Sandler, Wolchik, Tein & Dawson-McClure, 2003). The current paper reports on the effects of the Family Bereavement Program (FBP, Ayers et al., 2013–2014; Sandler, Wolchik, Ayers, Tein & Luecken, 2013) on multiple aspects of parental adjustment six years after program completion. The study addresses several questions. What aspects of bereaved parents’ adjustment are impacted by the FBP six years later? What factors moderate this impact? How does the FBP affect the trajectory of changes in parent adjustment over six years? The study also tests alternative pathways that account for FBP effects on parental adjustment over six years.
We first discuss the conceptual framework of the study as the examination of the cascading effects of the FBP over time to promote resilience of parents following the death of their spouse. We then present a description of the FBP and an overview of prior evidence of program effects. We then discuss how the current study advances evidence concerning the effects of the FBP on spousally-bereaved parents and contributes to the broader literature on the long-term effects of parenting interventions on the adjustment of parents.
Conceptual framework: Assessing the cascading effects of the experimental promotion of resilience of spousally-bereaved parents
A contextual resilience framework has previously been proposed to describe how the FBP promotes resilience (Sandler, Wolchik & Ayers, 2008). “From this perspective, the events surrounding the death disrupt the equilibrium of relations between individuals and their environment and threaten their well-being and performance of developmentally appropriate roles. Adaptation is seen as a process that occurs over time and is shaped by environmental and individual-level risk and protective factors. Multiple interrelated domains of outcomes are of interest, including levels of problems (including mental health problems, substance abuse, and physical illness), and positive well-being (including competent role performance and life satisfaction) and grief” (p.60). Resilience is defined to include higher levels of positive well-being and lower levels of problem outcomes for those who experienced this major life stress (Luthar, 2003). For bereaved parents, adaptation involves developing competent functioning in critical life tasks of middle adulthood that are disrupted by the death of their spouse as well as coping with grief. As described below, the FBP is designed to promote effective parenting, an adult life task (Levinson, 1978) that has been disrupted by the death of their spouse and one that has been found to be particularly stressful for single parents (Evenson & Simon, 2005). Prior research has found that programs that strengthen parenting have positive effects to reduce child and parent mental health problems (Barlow, Smailigie, Huband, Roloff & Bennett, 2012; Sandler, Ingram, Wolchik, Tein & Winslow, 2015). From a developmental perspective, there may be mutually reinforcing cascading effects in which improvements in parental mental health lead to increased positive parenting, and increases in positive parenting lead to decreased parent mental health problems over time.
The FBP is also designed to promote parent success in dealing with the tasks of coping with grief. Research on the course of grief has found little support for distinct, time-ordered stages of grief (Archer, 1999). Rather, research indicates that, although there are different trajectories of grief over time (Bonanno, Wortman, Lehman, Tweed, Haring, Sonnega et al. 2002), normatively, spousal grief gradually decreases over time before reaching an asymptote multiple decades following the death (Carnelley, Wortman, Bolger & Burke, 2006). The past decade has seen increasing interest in identifying pathological grief experiences which include experiences of prolonged yearning for the deceased and distress over the death that persist over time and impair healthy functioning (Bonanno, Neria, Mancini, Coifman, Litz & Insel, 2007). It is expected that the FBP’s effects to reduce grief in the short term will impact the trajectory of grief over time. The study will also examine cascading effects by which the FBP’s effects on other domains of functioning (e.g., parenting, depression) impact grief over time, and by which earlier effects on grief have cross-domain effects on parenting and mental health over time. Finally, the study of promotion of resilience includes increasing positive outcomes as well as reducing problem outcomes. From this perspective, it is hypothesized that positive effects of the FBP to promote effective coping with the stressors following spousal death will translate into an enhanced sense of efficacy that one can cope effectively with difficult situations.
Description and summary of effects of the FBP on children’s and parents’ outcomes
The FBP is a 12-session multi-component program for caregivers and children following the death of a parent. The program consisted of a parent1 group and a child/adolescent group that included several conjoint parent-youth activities. The program has been described in detail elsewhere (Ayers et al., 2013–2014; Sandler et al., 2013), so will only be briefly described here. Both the parent and youth groups focused on factors that have been found to relate to better outcomes for bereaved parents and youths. The parent group focused on building skills to strengthen positive parenting (i.e., positive parent-child relationship, listening skills, effective discipline), reducing parental depression and prolonged distressing grief (e.g., setting bereavement-related goals, positive reframing) and shielding children from exposure to other stressful events that often follow parental death. The child/adolescent group focused on teaching skills to strengthen adaptive coping and realistic control beliefs, reduce negative stress appraisals and inhibition of emotional expression and increase positive interactions and family relationships A randomized controlled trial of the FBP demonstrated that the program reduced child internalizing and externalizing problems, improved parenting and reduced depression and non-specific psychiatric symptoms for bereaved parents at the six-year follow-up (Sandler et al., 2010; Hagan, Tein, Sandler, Wolchik, Ayers & Luecken, 2012). The current study, which focuses only on spousally-bereaved parents, adds to prior reports by assessing the effects of the FBP on a broader range of outcomes than previously investigated, testing moderators of the program effects, assessing trajectories of change and testing pathways by which the FBP impacts parenting and parents’ adjustment.
What are the effects of the FBP on spousally-bereaved parents’ adjustment over six years?
A recent meta-analysis of 48 randomized trials of the effects of parenting programs found significant effects to reduce parent symptoms of anxiety, depression, stress, anger, guilt, confidence, and to increase parent satisfaction with partner relationships (Barlow, et al., 2012). The current study goes beyond the findings from this meta-analysis in three ways. First, the current study focuses on a group of parents who are at risk for multiple problem outcomes because of their experience of the death of their spouse, a major stressor that is most strongly associated with problem outcomes in younger widows, such as the bereaved parents in this study (Nolen-Hoeksema & Ahrens, 2002; Zisook, Schucter, Sledge & Mulvihill, 1993). Of the 48 trials reviewed in the Barlow et al. meta-analysis, only one focused on parents at risk because of a major family disruption (separation of parents), with the rest focusing on general population samples or parents of children with behavior problems. Spousal bereavement has been found to increase risk for multiple problem outcomes including depression, anxiety, prolonged grief and substance abuse (Keyes, Pratt, Galea, McLaughlin, Koenen, & Shear, 2014; Melhem, Walker, Moritz & Brent, 2008; Bruce, Kim, Leaf & Jacobs, 1990; Zisook & Schucter, 1991). A prior report of the effects of the FBP found that it reduced symptoms of mental health problems (depression and general mental health symptoms) and that it improved positive parenting at post-test and 11-month follow-up (Sandler et al., 2003). Because of these short-term effects, we expanded our assessment at the six-year follow-up to include a broader assessment of parental adjustment including measures of complicated grief, alcohol abuse, and coping efficacy. Prior literature has failed to find effects of preventive interventions on complicated grief (Wittouck, Van Autreve, De Jaegere, Portzky, & van Heeringen, 2011), however the effects of the FBP on depression and the comorbidity of depression, complicated grief and alcohol abuse (Hussong, Jones, Stein, Baucom & Bouding, 2011; Simon et al., 2007) led us to hypothesize long-term effects on multiple parent problem outcomes. Theoretically, the long-term effects might reflect the effects of the FBP to improve parental coping with the stress of bereavement which in turn leads to more effective regulation of negative affect, reduced symptoms of depression and mental health problems, and reduced use of alcohol as a strategy to regulate negative affect (Hussong et al., 2011). From a theoretical perspective, the effects of the program to improve parenting may also have positive cascading effects to reduce long-term parent problem outcomes. Positive parenting can be seen as effective functioning in a key role of middle adulthood (Simon, 1992), and as such may feedback to increase parents’ sense of competence and reduce a source of parenting stress and negative affect.
The second way in which the current study extends prior findings on the effects of parenting programs on parents’ adjustment is to extend the time frame for which effects were assessed. The current study assesses effects over a six year period following the intervention. Only one study in the meta-analysis reported effects at a follow-up longer than 12 months following the intervention. Although the meta-analysis found that positive effects on parents’ adjustment faded over one year follow-up, the effects may be more long-lasting in a sample of parents who are themselves experiencing a major stressor such as spousal death, which increases their risk for disorder.
A third way in which the current study extends prior literature on the effects of parenting programs on parents’ adjustment is by testing the trajectories of change by which effects manifest over time. At least three trajectories of change are theoretically plausible. Effects may occur directly following the program but fade over time. Findings in the Barlow et al. (2012) meta-analysis are consistent with a fading effects trajectory. They found that although there were significant effects of parenting programs at posttest, only the effects on stress and confidence were significant at the six-month follow-up and none of the effects were significant at the one-year follow-up. An alternative trajectory is that program effects occur immediately and are maintained over time because the use of program skills is reinforced by the social environment, barriers to use of program skills are reduced by the program, or both. Although the Barlow et al. (2012) meta-analysis reported no significant effects across trials at the one year follow-up, several of the randomized trials that were included in their meta-analysis did report significant effects at one year or longer follow-ups (e.g., Gardner, Burton & Klimes, 2006). A third possibility is that effects grow over time. Consistent with this model, DeGarmo, Patterson and Forgatch (2004) in their study of a parenting program for parents who experienced marital separation found a nonsignificant effect on parental depression at the six-, twelve- and eighteen-month assessments, but a small, significant effect at the 30-month assessment.
A fourth way in which the current study extends prior literature on the effects of a parenting program on parents’ adjustment is by studying potential moderators of such effects, including characteristics of the parents (i.e., baseline levels of mental health problems, gender, age) and characteristics of the bereavement (time since death, cause of death [illness vs. violent death (accident, suicide, homicide)]. These moderators were selected because prior literature has shown that they either moderate the effects of bereavement programs (e.g., baseline levels of problems; Currier, Neimeyer & Berman, 2008; Wittouck, et al., 2011), have been a special focus of research on the bereaved (e.g., sudden death, Keyes et al., 2014; Melhem et al., 2008), or have been found to moderate the effects of other preventive interventions (e.g., gender, age; Sandler, Wolchik, Cruden, Mahrer, Ahn & Brown, 2014).
What are the pathways that account for long-term FBP effects on bereaved parents’ adjustment and parenting?
Consistent with prior research on developmental cascades through which problems or competencies in one domain impact those in other domains over time (Masten & Cicchetti, 2010), alternative theoretical pathways are plausible to account for the long-term effects of the program on different aspects of parent adjustment. Reductions in depression or grief may have reciprocal long-term effects on each other and on long-term substance use, and improved earlier adjustment may impact later confidence in parents’ ability to deal with the stressors in their life. Also, it may be that program effects on parents’ adjustment (i.e., mental health problems or grief) mediate program effects on parenting. Research with bereaved parents as well as with other populations has found that parental depression or distress was associated with lower levels of effective parenting (e.g., Conger, Rueter & Conger, 2000; Kwok, Haine, Sandler, Ayers & Wolchik, 2005). Alternatively, it is plausible that improvements in parenting mediate program effects on parents’ adjustment. This may occur because parents gain a sense of efficacy through use of effective parenting skills or because improved parenting leads to decreases in family conflict and distress. A third alternative pathway is that reductions in child behavior problems lead to reductions in parental adjustment problems. In one of very few studies to test pathways by which a parenting program led to long-term changes in parental adjustment, DeGarmo et al. (2004) found that reductions in growth of boys’ externalizing problems over time led to reductions in growth of parental depression up to 30 months later. The current study investigates alternative pathways leading to improved parenting and reduced adjustment problems of bereaved parents over six years.
Methods
Participants
The procedures for recruitment, assessment, and random assignment to the intervention conditions have been presented in detail previously (Sandler, et al., 2003) and are briefly described here. Families that had experienced parental death and had one or more children between the ages of 8 and 16 were recruited through referrals from multiple community sources (e.g., schools, hospice). Caregivers and children were eligible if they met the following criteria: death occurred between 4 and 30 months prior to the start of the program; children were between 8 and 16 years of age; participants were not receiving mental health or bereavement services; children were not in a special class for the mentally handicapped; participants were willing to participate in either the group or self-study program and to participate in program evaluation interviews. Families were excluded and referred for clinical services if either the children or parent expressed suicidal ideation with a plan or met diagnostic criteria for a mental disorder that might interfere with their participation in the program (e.g. parental major depression).
The sample for the current study consisted of 131 spousally-bereaved parents and their 206 offspring who participated in the trial. These families represent a subsample of the 156 caregivers in the FBP which also included other relatives or friends who assumed a caregiving role following the parental death (Sandler et al., 2003). Families were randomly assigned to the intervention (72 parents and 108 children) or to the self-study group (59 parents and 98 children). Assignment was done after the pretest, using computer-generated randomization procedures. Of the bereaved parents, 77% were mothers and the mean age at program entry was 41.33 years (SD = 7.00, range = 27–57). Of the youths, 53% were males and the mean age at program entry was 11.98 years (SD = 2.56, range = 8–16). Ethnicity of the parents was 67.89% non-Hispanic White, 10% Hispanic, 6% African American, 1.5% Native American, 1.5% Asian American or Pacific Islanders, and 9% other or unknown. Median family income at pretest was in the range of $30,001 to $35,000. On average, parental death occurred 9.95 months (SD = 5.73, range = 4–30 months) prior to participation. Cause of death was 72% illness, 15% accident, and 12% homicide or suicide.
Intervention Programs
The intervention, which was fully described in a detailed manual (Ayers et al., 2008) consisted of separate groups for parents, children, and adolescents. The program for parents consisted of 12 two-hour group sessions and two individual sessions. The parent group focused on teaching skills and activities to promote positive parent-child relationships (e.g., one-on-one time, catch ‘em being good, active listening skill), strengthen effective discipline (e.g., clear expectations and rules, consistent and appropriate consequences), and protect children from exposure to post-bereavement stressors (e.g., reduce occurrence of stressful events in the family). The parent component also focused on reducing the parents’ depression and grief (e.g. normalizing grief experiences, positive reframing skills, seeking support from friends, increased involvement in positive activities, setting personal goals) (Sandler, Wolchik, Ayers, Tein, & Luecken, 2013). The child and adolescent programs targeted strengthening effective coping skills, adaptive control beliefs, expression of grief-related feelings and positive parent-child relationships and reducing negative esteem and threat appraisals. Four sessions included conjoint caregiver-youth activities. Parents and youth set personal goals for the program, and progress toward goal achievement was discussed throughout the program. The program emphasized applying skills learned in group at home and home practice was processed in each group session. In the self-study group, caregivers, children, and adolescents each received three books on dealing with grief along with a syllabus. Groups were led by two masters-level counselors who were extensively trained and supervised to deliver the program with high levels of fidelity. Fidelity of implementation was rated by objective reliable coders of session videos who rated the delivery of each action item described in the program manual. Leaders implemented 84% of the action items.
Procedures
Assessments were conducted at four time points: pretest (T1), posttest (T2), and 11 months (T3) and 6 years after posttest (T4). Data for T1 through T3 were collected across six cohorts of groups that were held between 1995 and 1998. Data collection for T4 occurred between 2001 and 2004. Retention of participants for the sub-sample of spousally-bereaved families is shown in Figure 1. Assessments were completed by trained interviewers. In response to a question at the end of the T4 interview 96.5% of the interviewers reported being unaware of interviewee’s program condition. Confidentiality was explained, and caregiver informed consent and child/adolescent assent were obtained prior to the interviews. All procedures were approved by the Arizona State University Institutional Review Board. At T1, T2, and T3, families that had one child in the study received $40 compensation for interviews involving one child, and an additional $30 for each addition child participating in the study. Caregivers and youths each received $175 at T4.
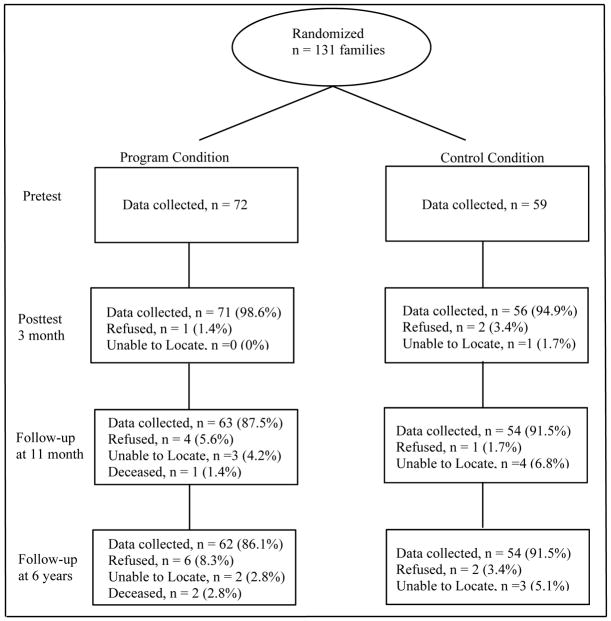
Figure 1.
Flow chart of data collection and attrition over six years
Note: This is a subsample of the Family Bereavement Project which include 156 families. Sandler, et al. (2010) presents the flowchart of recruitment, randomization, and assessments of the entire sample. It is not possible to present the recruitment information for this subsample because the information on whether the caregivers were the spousally-survived parents was unknown till pretest interview.
Measures
Mental Health Problems
The Psychiatric Epidemiology Research Interview (PERI; Dohrenwend, Shrout, Ergi, & Mendelsohn, 1980; a 27 item measures of general psychiatric symptoms; e.g., “How often have you felt confused and had trouble thinking?,” α = .93–.96 at T1–T4) and the Beck Depression Inventory (BDI; Beck & Steer, 1993; a 21 item measure of depression symptoms; e.g., “I cry all the time now,” α = .86–.90 at T1–T4) were administered to parents at all four assessments. Acceptable reliability and construct validity have been reported for the PERI (Dohrenwend et al., 1980) and the BDI (Beck & Steer, 1991). In addition, the Composite International Diagnostic Interview (Short Form) module for major depression (CIDI-SF; Walter, Kessler, Nelson & Broczek, 2002, α not applicable) was administered at the six-year follow-up (T4). Evidence of convergent validity for CIDI-SF in this sample is provided by significant relations with T4 BDI (r = .40) and T4 PERI (r = .54). In accord with the standard time frame for each scale, “past week” was used for the BDI (assessing the severity of depression), “past month” for the PERI (assessing non-specific psychiatric distress), and “past year” for the CIDI-SF. Two cutoff scores were used to indicate severity of depression on the BDI (Beck & Steer, 1993): scores of 10 or greater indicated mild or higher levels of depression and 19 or greater indicated moderate or severe levels of depression. Only one parent exceeded the cutoff for severe depression (scores of 30 or greater). At T1 53% of the parents had scores ≥10 and 15% ≥19. Major depression symptom and diagnosis were scored using CIDI-SF following the procedures outlined by Walter, et al., 2002.
Alcohol Problems
At T4 the 13-item parent report of Short Michigan Alcoholism Screening Test (SMAST) was administered to assess symptoms of alcoholism (Selzer, Vinolur & van Rooijen, 1975; e.g., “Have you been able to stop drinking when you wanted to?”; α = .89 at T4). The SMAST has adequate reliability and is effective in screening for alcoholism (Selzer et al., 1975). The response time frame was “in the last 6 years” to assess alcoholism symptoms following the program. We created two binary variables to indicate “possibly alcoholics” (score of 2 or above) and “alcoholics” (score of 3 or above) in accord with Selzer, Vinokur, and Rooijen (1975, p. 125)
General Coping Efficacy
At T4, an 8-item parent report of Coping Efficacy Scale (Sandler, Tein, Mehta, Wolchik & Ayers, 2000) was used to assess the parents’ beliefs about how effectively they deal with stressors in their lives (e.g., “Overall, how satisfied are you with the way you handled your problems”; α = .89). Evidence of construct validity is provided by a significant negative relation with parents’ depressive symptoms in the current study (r = −.53).
Grief
The 13-item Present Feelings subscale of the Texas Revised Inventory of Grief (TRIG; Faschingbauer, 1981) was used to assess current grief (e.g., “I can’t avoid thinking about my [deceased spouse]”) at all four assessment points (α = .89–.96 at T1–T4). The TRIG, one of the most commonly used measures of grief, has been demonstrated to have acceptable levels of reliability and validity (Neimeyer & Hogan, 2008). However, TRIG has been criticized for having little variation because most of the items represent normative aspects of grief (Neimeyer & Hogan, 2008). Therefore, at T4, we also administered the Inventory of Complicated Grief (ICG) which was adapted from the 38-item ICG2 developed by Prigerson and Jacobs (2001). The measure consisted of 26 items about their feeling (e.g., “Do you ever feel that a part of yourself died along with your [deceased]?”) and 12 items about the impact of their life (“Since {one month marker event}, did these feelings keep you from doing things or going places with other people your age?”). The items were selected in collaboration with one of the scale developers (Prigerson) to best represent problems associated with the proposed diagnosis of complicated grief disorder that was being considered for inclusion in the Diagnostic and Statistical Manual of Mental Disorders (Prigerson et al., 2009). Measures of grief disorder have been shown to predict impaired functioning, physical health problems, and suicidal ideation over and above the effects of other mental health problems (Bonanno, Neria, Mancini, Litz, Coifman & Insel, 2007; Prigerson, Vanderwerker & Maciejewski, 2008). The responses were scored so that higher values reflected greater levels of grief disorder. Based on findings from a prior factor analysis of children’s and adolescent’s responses to the ICG (Sandler et al., 2010) we tested a bi-factor model that specified a general factor that accounts for the commonality of all of the items and a specific factor over and above the general factor that included items related to lack of social trust, loneliness, and lack of control. The model fit the data adequately [χ2(df =159) = 228.78; CFI = 0.91; RMSEA = 0.06]. Using the factor scores of the latent general and specific factors from the bi-factor model, we created two measures – one for general prolonged grief and one for the specific prolong grief which we named prolonged social detachment and insecurity. In addition, items from the ICG and the TRIG at T4 were used to assess whether parents met the diagnostic criteria for Persistent Complex Bereavement Disorder (PCBD), identified as a condition for further study in the Diagnostic and Statistical Manual Version 5 (American Psychiatric Association, 2013). In addition to the death of a significant other (Criterion A), parents had to endorse one of the four symptoms described in Criterion B (persistent yearning, intense sorrow, preoccupation with the deceased, or circumstances of the death), six of the twelve symptoms in Criterion C (which included items assessing reactive distress to the death and social/identity disruption) and Criterion D (i.e. impairment of social, occupational or other important areas of functioning). Items on the ICG were coded as meeting criteria if they were reported to occur weekly or daily, and items on the TRIG were coded as meeting criteria if they were endorsed as being “mostly true” or “completely true”. Because it is a condition for further study rather than an established diagnosis two separate diagnostic criteria are reported in this paper, one that meets symptom criteria (A, B, C) and one that meets symptom plus impairment criteria (A,B,C & D).
Parental warmth
This construct, administered at all four assessment points, was measured as a composite of standardized scores on the following measures: parent and youth report of the 16-item Acceptance (e.g., “You saw [child]’s good points more than his/her faults.”) and 16-item Rejection subscales (“You were always getting after [child].”) of the Child Report of Parental Behavior Inventory (CRPBI; Schaefer, 1965; α’s at T1–T4 range .86–.94 across reporters); youth report of the 10-item Sharing of Feelings Scale (Ayers, Sandler, Twohey, & Haine, 1998; e.g., “When you tell your [parent] about a problem, [he/she] knows why you felt the way you did.”; α = .84–.90 at T1–T4), which assessed children’s perceptions that their caregiver understands their feelings; and parent report of the 6-item Talk With Reassurance subscale of the Caregiver Expression of Emotion Questionnaire which assessed how caregivers communicate with their children about stressful family events (Jones & Twohey, 1998; e.g., “Reassure child that you are dealing with your sadness,” α = .73–.85 at T1–T4). Acceptable internal consistency reliability and validity of youth and parent reports of the CRPBI have been reported (Schaefer, 1965). High scores on Sharing of Feelings Scale and Talk With Reassurance were associated with significantly lower mental health problems in bereaved youth (Jones & Twohey, 1998). The time frame of “past month” was used for all of these measures. Composite scores of these measures were computed at each wave on the basis of CFAs. After accounting for correlations between residuals of the measures from the same reporter, the fit of the one-dimension model was adequate for each wave: T1: χ2(4, N = 204) = 9.44; CFI = .98, RMSEA = .08; SRMR = .04; T2: χ2(4, N = 197) = 6.07; CFI = .99, RMSEA = .06; SRMR = .03; T3: χ2(4, N = 179) = 9.09; CFI = .98, RMSEA = .08; SRMR = .05; T4: χ2(4, N = 178) = 4.33; CFI = .99, RMSEA = .02; SRMR = .01.
Youth Externalizing Problems
At all four assessments, externalizing problems during the past month were assessed using the parent report of Child Behavior Checklist (CBCL) (Achenbach, 2001) for youth younger than 18 years and parent report of the Young Adult Behavior Checklist (YABCL) (Achenbach, 1997) for youth aged 18 years or older. Because the measures for youth and young adults were not identical, using a large data set obtained from Achenbach (Thomas M. Achenbach, PhD, unpublished raw data from the CBCL and YABCL, 2003), we applied item response theory to conduct an equating transformation that selected common items and put the scale scores of the items on a uniform metric across the four assessment points. The resulting items and metrics were applied to the current data to create scores for externalizing problems (α = .90–.93 at T1–T4).
Results
Data Analysis Overview
Multivariate outlier analyses were conducted, using hat matrix, DFFITS, DFBETAS, and Cook’s distance to identify influential data (Cook, 1977; Neter, Wasserman, & Kutner, 1989). Preliminary analyses compared baseline demographic and other variables across the experimental conditions and across attrition status at W4 assessment, using logistic regression for categorical measures or analysis of variance for continuous measures. Analysis for intervention effects were done under the intent-to-treat approach using MPlus (v. 7.0; Mutén & Mutén, 1998–2012) and full-information maximum likelihood estimation for handling missing data. Yuan and Bentler’s (2000) robust correction to standard errors (i.e., the T2* chi-square test statistics) was used for the binary outcomes and for the continuous variables that were highly skewed (≥2) or kurtotic (≥7) (West, Finch, & Curran, 1995).
To assess the effects of the FBP on parent outcomes six years after the intervention, analysis of covariance (ANCOVA) for continuous outcomes and logistic regression for binary outcomes were used. We controlled for the baseline scores for the measures that were assessed at all four time points; for variables that were only assessed at T4 we controlled for T1 mental health and grief measures of BDI, PERI, and TRIG. We examined differences between experimental groups and whether group difference was moderated by any of five variables -- the baseline measure, time since death, caregiver gender, caregiver age, and cause of death [illness vs. violent death (accident, suicide, homicide)]. We examined one moderator at a time by adding group x moderator interaction in the model for each of the nine outcome variables, for a total of 45 tests of moderation. For significant interactions, we conducted simple effect test to probe the region beyond which (for continuous moderator, e.g., baseline CDI) or the subsample (for categorical moderators, e.g., parent gender) the experimental groups differed significantly. If none of the moderation effects was significant, we examined the main effect without the interaction. To adjust for multiple tests, we also applied false discovery rate (FDR, Benjamini & Yekutieli, 2001), which controls for the expected proportion of false positives among all significant hypotheses, to examine the main and interaction effects separately.
For parent measures that were administered at all four time points (BDI, PERI, TRIG, and parental warmth), multi-group piecewise growth curve modeling (GCM) was used to examine whether the trajectory of change over four time points was equivalent across the FBP and self-study groups. Because significant effects at post-test were found for all variables that were assessed at all four time periods, we began by specifying this change. The maintenance, fading, and increasing effects models were tested using a piecewise model that included two growth factors: one for an upward or a downward shift immediately after the intervention (i.e., from T1 to T2) and one for an additional linear growth after (from T2 to T4). Using multi-group comparisons, we examined group differences as well as the assumption that the two groups might have different growth patterns. Groups differed on the first but not the second growth factor would support a maintenance model. A pattern in which the second growth factor also differed across groups would support either the increasing effects model or the fading effects model, depending on the shape of the growth trajectories in the two groups. Analysis for parental warmth controlled for the clustering effects that multiple children were nested within families (e.g., specifying cluster = family ID in Mplus).
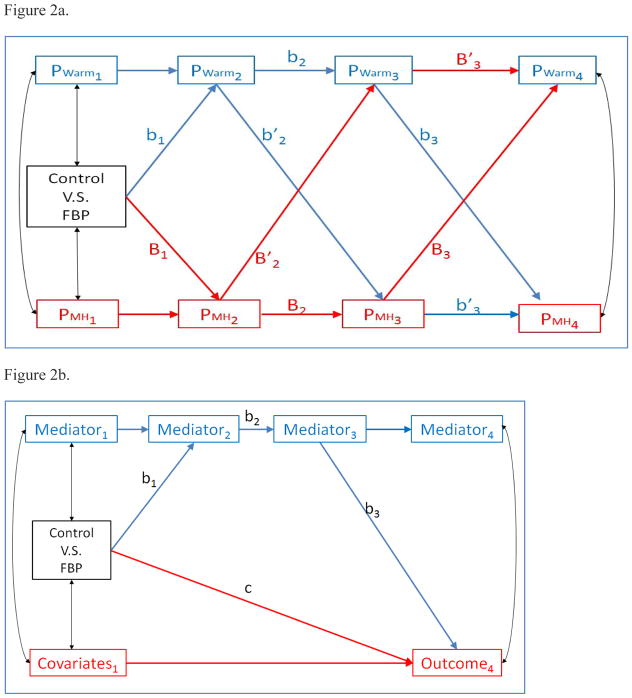
To examine the mediation pathways by which the FBP affected parenting or parental adjustment over time, we tested longitudinal mediation models (Cole & Maxwell, 2003). We examined one mediator variable and one outcome variable at a time. As illustrated in Figure 2a, the cross-lagged mediation model, where both the mediators and outcomes were assessed at all of the time points, allowed us to test two alternative direction of effects; that parents’ mental health adjustment (PMH; BDI, PERI, or TRIG) mediated FBP effects on parental warmth (PWarm) and alternatively that parental warmth mediated FBP effects on parents’ mental health. There are two prospective mediation pathways through two time lagged effects for each outcome, one leading from change from the mediator at T2 to the outcome at T3, then to the outcome at T4; and the other leading from the mediator at T2 to mediator at T3, then to the outcome at T4. For example, the mediation effects of parental warmth (mediator) on BDI (outcome) consisted of 1) FBP → T2 parental warmth → T3 parental warmth → T4 BDI (i.e., b1 * b2 * b3), and 2) FBP → T2 parental warmth → T3 BDI → T4 BDI (i.e., b1 * b′2 * b′3); the mediation effects of BDI (mediator) on parental warmth (outcome) consisted of 1) FBP → T2 BDI→ T3 BDI → T4 parental warmth (i.e., B1 * B2 * B3), and 2) FBP → T2 BDI → T3 parental warmth → T4 parental warmth (B1 * B′2 * B′3). Using similar cross-lagged mediation models, we also tested whether the program effects on youth externalizing problems mediated the program effects on parents’ adjustment.
Figure 2.
Figure 2a. Mediation model for mediators and outcomes assessed at all four time points
Figure 2b. Mediation model for mediators assessed at four time points and outcomes at T4 only
Note. Fig. 2a illustrates mediation models in which variables measured at four waves (e.g., parenting (PWarm) and parent adjustment (PMH, i.e., depression, grief and general mental health symptoms in separate models) mediate each others’ effects over six years.
Figure 2b illustrates the mediation model where the outcomes were only assessed at T4 (General Prolong Grief, Prolonged Social Detachment/Insecurity, Alcohol Problems, CIDI Depression, Coping Efficacy). Each variables assessed at T1, T2 and T3 were tested as potential mediators (i.e., BDI, PERI, TRIG, parental warmth, child externalizing problems) of the outcomes at T4. T1 BDI, PERI, and TRIG were treated as the control variables for each of the outcomes. The mediation pathway is FBP → T2 mediator → T3 mediator → T4 outcome (i.e., b1 * b2 * b3). As shown in Figure 2b the model was also applied to examine the mediation effects on the T4 binary outcomes (BDI Mild Diagnosis, CIDI-Depression Diagnosis, Persistent Complex Bereavement Disorder, and SMAST-Possible Alcoholism).
We applied multilevel mediation analysis for models that involved parental warmth and child externalizing problems, where there were multiple scores per family, for all other models where there was one score for each family (e.g., BDI, SMAST) we used single level models. We used the joint significant test to examine the three-path mediated effects, which include two mediators in a causal sequence. Taylor, MacKinnon, & Tein (2008) showed that the joint significance test for three-path mediation pathways is the preferred method of hypothesis testing of mediation effects than any other methods -- it has comparable power to the bias-corrected bootstrap method but has better control for Type I error; it has comparable Type I error to the percentile bootstrap method but has light better power. Similar conclusion also applies to two-path mediation pathways (MacKinnon, Lockwood, Hoffman, West, & Sheets (2002).
Preliminary Analyses
Table 1 shows the comparisons of the intervention and control groups on the demographic variables and baseline covariates. There was one significant difference – the FBP parents, on average, had higher levels of depression than the control parents at the program entry. As a result, T1 BDI was included as a control variable for all outcome evaluations, both for variables assessed at all four time points and those that were assessed only at T4. No influential cases were identified in the multivariate outlier analyses. No significant attrition or attrition x condition effects were found on the 12 baseline demographic and outcome measures indicating that differential attrition did not pose a threat to either internal or external validity of the findings.
Table 1.
Demographics and Outcome Variables at Baseline
| Control | FBP | Difference | |
|---|---|---|---|
| Demographics | |||
| Female caregiver, No. (%) | 41 (69.49%) | 60 (83.33%) | P = .06 |
| Caregiver mean age | 41.21 (6.71) | 41.42 (7.26) | P = .87 |
| Caregiver Ethnicity | P = .67 Χ2[5] = 3.20 |
||
| White, Non-Hispanic | 44 (74.58%) | 50 (69.44%) | |
| Hispanic | 6 (10.17%) | 7 (9.72%) | |
| Black | 2 (3.39%) | 6 (8.33%) | |
| Asian American/Pacific Islanders | 0 (0%) | 2 (2.78%) | |
| American Indian | 1 (1.69%) | 1 (1.39%) | |
| Other | 1 (1.69%) | 1 (1.39%) | |
| Missing | 5 (8.47%) | 5 (6.94%) | |
| Caregiver education | 4.74 (1.38) | 4.70 (1.26) | P = .87 |
| Family income | 7.88 (4.90) | 8.54 (4.78) | P = .47 |
| No. of youth living at home | 1.72 (.79) | 1.50 (.73) | P = .10 |
| Time since death (months) | 9.84 (5.38) | 10.04 (6.04) | P = .85 |
| Cause of death | P = .67 | ||
| Illness | 43 (74.14%) | 51 (70.83%) | |
| Violent | 15 (25.86%) | 21 (29.17%) | |
| Outcome Variables – Spousally-Bereaved Caregiver | |||
| Parental warmth | −.04 (.54) | .03 (.53) | P = .36 |
| Depression (BDI) | 9.38 (6.63) | 12.02 (8.00) | P = .05* |
| Anxiety (PERI) | 2.35 (.60) | 2.51 (.73) | P = .20 |
| Texas Revised Inventory of Grief (TRIG) | 3.36 (.79) | 3.32 (.89) | P = .79 |
FBP Effects at Six Years
With the exception of the T4 alcohol problems measure (SMAST) which was highly skewed (= 4.39) and kurtotic (= 21.03) all of the continuous outcome variables had skewness ≤1.5 and kurtosis ≤2.5. Thus, Yuan and Bentler (2000) robust correction to standard errors was used for analyses that included the SMAST as well as those that used binary outcomes. Table 2 shows the results of ANCOVA and Table 3 shows the results of logistic regression for examining the differences between the FBP and self-study conditions on T4 outcomes. There were six significant main effects on the continuous variables, based on the false discovery rate adjusted p-values, with effect sizes ranging from small to moderate. The parents in the FBP condition had significantly lower scores on measures of depression (BDI), non-specific psychiatric distress (PERI), normative grief problems (TRIG), general prolonged grief symptoms, and alcohol problems (SMAST) as well as higher scores on parental warmth than those in the self-study condition. Three of the 45 tests of moderation were also significant: a significant group x parent age interaction on BDI, a significant group x time since death interaction on parental warmth, and a significant group x parent gender effect on parent coping efficacy. Post-hoc analyses for these interactions found that: For parents who were 42 years old or younger (e.g., 57% of the parents) parents in the FBP had significantly lower BDI scores than those in the control condition; For the families who experienced death within 10 months prior to program entry (e.g., 69% of the families), parents in the FBP condition had significantly higher warmth than those in the control condition; Mothers but not fathers who participated in the FBP had significantly higher coping efficacy than those in the self-study group [adjust MFBP = 3.32, Mself-study = 2.89; b = 0.42, 95% CI = [0.25, 0.60], t = 4.77, p < 0.001] six years after the intervention.
Table 2.
ANCOVA Results for continuous outcomes
| 6-year Continuous Outcome | Adjusted Meana (FBP) | Adjusted Mean (Self-Study) | Unstandardized Program Effect [95% CI] e | t-statistics | False Discovery Rate—Adjusted p Value | Cohen’s d |
|---|---|---|---|---|---|---|
| BDIb - Depression | 5.74 | 8.35 | −2.62 [−4.89, −0.34] | −2.25* | .047* | .40 |
| PERI – Psychiatric Distress | 1.88 | 2.11 | −0.20 [−0.38, −0.02] | −2.12* | .047* | .38 |
| TRIG – Normative Grief | 2.53 | 2.83 | −0.30 [−0.56, −0.05] | −2.32* | .045* | .41 |
| CIDI-Depressive Symptoms | 0.83 | 1.42 | −0.59 [−1.31, 0.12] | −1.63† | .129 | .29 |
| General Prolonged Grief | 1.76 | 2.17 | −0.41 [−0.65, 0.17] | −3.32** | .009** | .59 |
| Prolonged Social Detachment/Insecurity | 0.17 | 0.23 | −0.06 [−0.13, 0.02] | −1.45 | .146 | |
| SMAST – Alcohol Problems | 0.05 | 0.71 | −0.66 [−.78, −0.33] | −2.57** | .030* | .45 |
| Coping Efficacyc | 2.95 | 3.30 | .14 [−.05, .34] | 1.46 | .146 | |
| Parental Warmthd | .27 | .01 | .26 [.08, .47] | 2.57** | .030* | .45 |
Abbreviations: BDI, Beck Depression Inventory; PERI, Psychiatric Epidemiology Research Interview; TRIG, Texas Revised Inventory of Grief; CIDI-SF, Composite International Diagnostic Interview (Short Form); SMAST, Short Michigan Alcoholism Screening Test; CI, confidence interval.
p < 0.10;
p < 0.05;
p < 0.01;
Adjust for the baseline measures, including baseline BDI.
The group x parent age interaction was significant (B = .38; t = 2.15; p =.03);
The group x parent gender interaction was significant (B = −.56; t = −2.80; p =.005);
The group x time since death interaction was significant (B = −.04; t = −2.38; p =.02).
Except for SMAST, all of the confidence intervals (CI) were computed with the bootstrap procedure by the Mplus. Boostrap procedure is not available for the Yuan-Bentler T2* chi-square test statistic (2001).
Table 3.
Logistic Regression Results for binary outcomes
| 6-year Binary Outcome (% endorsement, FBP vs. Self-study) | % FBP | % Self-study | Unstandardized Program Effect [95% CI] | Odds Ratio of Program Effect [95% CI] | False Discovery Rate— Adjusted p Value | Number Needed to Treat (NNT) |
|---|---|---|---|---|---|---|
| BDI Diagnosis – Mild Depression | 22.6% | 35.9% | −1.09* [−2.03, −0.14] | 0.34 [0.13, 0.87] | .045 | 7.54 |
| CIDI-Depression Diagnosis | 19.4% | 26.4% | −0.78† [−1.67, 0.10] | 0.46 [0.19, 1.11] | .084 | 14.16 |
| Persistent Complex Bereavement Disorder (symptom criteria) | 4.8% | 23.5% | −2.53** [−3.99, −1.07] | 0.08 [0.02, 0.34] | .040 | 5.35 |
| Persistent Complex Bereavement Disorder with Impairment | 0% | 11.8% | NA | NA | NA | 8.50 |
| SMAST-Possible Alcoholism | 1.6% | 15.1% | −2.40* [−4.65, −0.16] | 0.09 [0.01,0.63] | .045 | 7.41 |
Abbreviations: BDI, Beck Depression Inventory; CIDI-SF, Composite International Diagnostic Interview (Short Form); SMAST, Short Michigan Alcoholism Screening Test; CI, confidence interval.
p < 0.10,
p < 0.05,
p < 0.01
NA – not applicable because there was no parent in the FBP group that had the disorders and endorsed the impairment item.
There were three significant main effects on the binary outcomes. The analyses using cutoff scores on the T4 BDI, showed that parents in the FBP group were less likely than those in the self-study group to be above the cut point (BDI ≥10) for the mild or higher levels of depression 22.58% vs. 35.85%; odds ratio = .34 [95% CI = .13, .87]; NNT = 7.54). However for the moderate or higher levels of depression (BDI ≥19), the two group did not differ significantly (4.84% vs. 7.55%; odds ratio = .31 [95% CI = .07, 1.43]; p = .13). Parents in the FBP group were less likely than those in the self-study group to meet the symptom criteria (A,B and C) for persistent complex bereavement disorder (4.84% vs. 23.53%; odds ratio = .08 [95% CI = .02, .34]; NNT = 5.35) and to meet criteria for persistent complex bereavement disorder with moderate or higher level of impairment in social, occupational or other important areas of functioning [0% vs. 11.76%; NNT = 8.50; odds ratio could not be defined because no parents meet the criteria in the FBP group; Fisher’s Exact Test p = .007]. The analyses using the cutoff scores on the SMAST indicated that parents in the FBP group were less likely than those in the self-study group to have drinking problems (possible alcoholic: 1.61% vs. 15.09%; odds ratio = .09 [95% CI =.01, .77; NNT = 7.41]; alcoholic: 0% vs. 11.32%; NNT = 8.83; odds ratio could not be defined because no parents in FBP exceeded this cutoff; Fisher’s Exact Test p = .007].
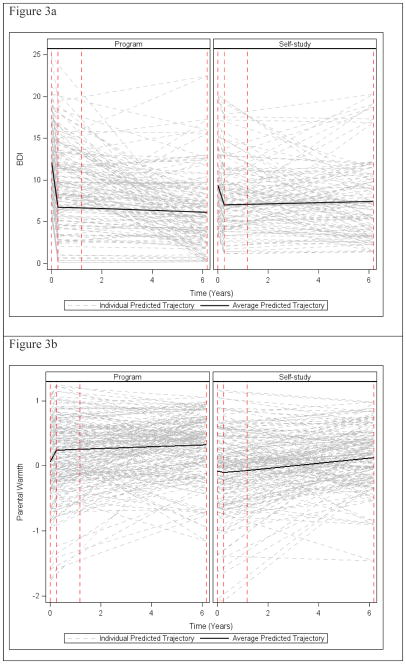
Trajectory of Program Effects
Table 4 shows the results of the multi-group comparisons of the growth factors (i.e., intercept, changes occurred immediately after the intervention, and linear growth after posttest). For illustration, Figures 3a and 3b present the piecewise growth model separately for the FBP and the self-study for BDI and parental warmth respectively. The improvement occurred mainly from pretest to posttest. The scores on BDI, PERI, Warmth and TRIG reduced significantly from pretest to posttest for both the FBP and self-study groups. However, the magnitude of reduction for the FBP parents was significantly larger than for that of the self-study parents. From the posttest to the 6-year follow-up, additional reductions also occurred for PERI and TRIG for both the FBP and self-study groups; however, the magnitude of reduction was not significantly different. These results indicate that the immediate effects of the FBP to decrease depression, non-specific psychiatric distress, parental warmth and grief were maintained over six years.
Table 4.
Piecewise Growth Curve Modeling Results
| Intercept | Slope 1 (Pretest-Posttest) | Slope 2 (Posttest-6-year) | ||
|---|---|---|---|---|
| BDI | FBP (N = 73) | 12.09(.78)** | −21.37(2.74)** | −0.10(.13) |
| Self-Study (N = 58) | 9.38(.87)** | −9.54(3.08)** | 0.08(.18) | |
| Difference [95% CI] | 2.72(1.17)* [0.43, 5.00] | −11.83(4.13)** [−19.92, −3.75] | −0.18(.22) [−0.62, 0.26] | |
|
| ||||
| PERI | FBP (N = 73) | 2.52(.07)** | −1.55(.23)** | −0.03(.01)** |
| Self-Study (N = 58) | 2.35(.08)** | −0.71(.26)** | −0.02(.01)† | |
| Difference [95% CI] | 0.16(.11) [−0.06, 0.38] | −0.84(.35)** [−1.52, −0.16] | −0.01(.02) [−0.05, 0.02] | |
|
| ||||
| TRIG | FBP (N = 73) | 3.32(.09)** | −1.74(.23)** | −0.06(.01)** |
| Self-Study (N = 58) | 3.36(.10)** | −1.17(.27)** | −0.05(.02)** | |
| Difference [95% CI] | −0.04(.14) [−0.31, 0.23] | −0.69(.35)* [−1.37, −0.001] | 0.001(.02) [−0.04, 0.04] | |
|
| ||||
| Warmth | FBP (N = 108) | 0.06(.08) | 0.77(.17)** | 0.01(01) |
| Self-Study (N = 98) | −0.08(.08) | −0.10(.18) | 0.04(.01)** | |
| Difference [95% CI] | 0.13(.11) [−0.09, 0.35] | 0.87(.25)** [0.38, 1.36] | −0.03(.02) [−0.06, 0.01] | |
p < 0.10,
p < 0.05,
p < 0.01.
Figure 3.
Figure 3a: Piecewise growth curve model of BDI
Figure 3b: Piecewise growth curve model on parental warmth
Mediation of Program Effects
For the tests of mediation for variables that were assessed at all four time points, the results show that warmth served as a mediator for BDI, PERI, and TRIG, through the same three linkage pathway; FBP → T2 warmth → T3 warmth → T4 BDI [b1 = .23 (.07), p < .001; b2 = .89 (.15), p < .001; b3 =− 5.20 (2.00), p = .009]; and similarly to T4 PERI [b1 = .23 (.06), p < .001; b2 = .89 (.13), p < .001; b3 = −.30 (.15), p = .05)] and TRIG [b1 = .21 (.06), p < .001; b2 = .95 (.13), p < .001; b3 = .30 (.14), p = .04)]. According to this model, program induced improvements in warmth at post-test, led to increased warmth at the 11-month follow-up which in turn lead to reduced parent symptoms of depression and non-specific psychiatric distress at the six-year follow-up. However the multi-linkage mediation models also showed a positive path from warmth at T3 to TRIG at the six-year follow-up, indicating that increased warmth at 11-months following the intervention led to increased grief six years following the intervention. BDI also served as a mediator for parental warmth through the FBP → T2 BDI → T3 BDI → T4 warmth pathway [B1 = −1.93 (.96), p=.05; B2 = .37 (.09), p < .001; B3 = −.02 (.01), p = .04]. According to this model, FBP effects on depression symptoms at posttest led to decreased depression symptoms 11 months later, which led to increased warmth six years following the intervention. Each of the two-path mediation models described above were significant using the joint significance test (Taylor, MacKinnon & Tein, 2008). The FBP effects on PERI did not mediate program effects on warmth. Neither PERI or TRIG were found to mediate program effects on warmth at the six-year follow-up. Youth externalizing problems was not a significant mediator of program effects on parental warmth or parental adjustment.
Mediation analyses were conducted for general prolonged grief, alcohol problems, and coping efficacy which were only assessed at the six-year follow-up and for which the intervention effects were significant. The intervention effect on general prolonged grief was mediated by program effects on BDI (b1 = −1.93 (.96), p=.05; b2 = .37 (.08), p < .001; b3 = .04 (.01), p = .008), TRIG (b1 = −.21 (SE=.09), p=.01; b2 = .76 (.04), p < .001; b3 = .50 (.11), p < .001), and parental warmth (b1 = .22 (.07), p=.001; b2 = .92 (.12), p < .001; b3 = .49 (.22), p = .03). According to these models, program effects to decreased depression and TRIG at post-test partially accounted for program effects to decrease prolonged grief six years following the intervention. Program effects to improve parental warmth, however, had an opposite effect to increase the level of prolonged grief at the six-years follow-up. The effects of the FBP on coping efficacy for mothers was mediated by BDI (b1 = −1.93 (.96), p=.05; b2 = .37 (.08), p < .001; b3 = −.02 (.01), p = .006), TRIG (b1 = −.21 (.09), p=.01; b2 = .76 (.04), p < .001; b3 = −.16 (.08), p = .04) and parental warmth (b1 = .23 (.08), p=.004; b2 = .88 (.14), p < .001; b3 = .51(.15), p = .001). No significant mediators were found to account for program effects on alcohol problems, alcoholism or persistent complex bereavement disorder. Mediation analyses were conducted for the T4 binary outcomes that had significant intervention effects, BDI – mild depression, persistent complex bereavement disorder (criteria A,B and C), and SMAST – possible alcoholism. No significant mediation effects were found on these variables.
The positive prospective relations between parental warmth at T3 and two different measures of grief at the 6-year follow-up were in the opposite direction from our expectations, and indicated a potential iatrogenic effect of increasing parental warmth to lead to an increase in prolonged grief. The effects of warmth on grief might be due to confounding variables such that the effects were contributed by shared variance between parental warmth and the other significant mediators. In order to test this possibility we tested a model which simultaneously included BDI, TRIG and warmth as mediators of program effects on the each of the measures of grief at the six-year follow-up. With the limited sample size, it is impossible to examine a full longitudinal mediation model similar to Figure 2a that included all of the mediators of all time points in the model. We thus examined only the effect of T3 parental warmth on T4 grief measures controlling other T3 mediators and direct intervention effect. We could not test such a model under the multilevel modeling framework either. The model would not converge, which was likely due to small cluster sizes (i.e., small number of children in each family) for a larger number of predictors. Positive parenting scores among the children within the same family were similar (e.g., intraclass correlations within family ranged from .42 to .66 for T1 to T2 measures of positive parenting), so we used the average of the parents’ rating of warmth across all children in the same family as the measure of warmth. We then conducted the analysis using the single-level analysis (family as the unit). The results show that, for both models, T3 warmth still had significant or marginal significant effects on TRIG [b = .14 (.08), p=.06] and General Prolonged Grief [b = .20 (.08), p=.01] at the six-year follow-up. However, the T3 BDI no longer had a significant effects on either TRIG or General Prolonged Grief at the six-year follow-up.
In addition, because the positive relations between parenting and grief represented potential iatrogenic effects of strengthening parenting to increase grief, further analyses were conducted to assess whether increased parenting led to the DSM V criteria of Persistent Complex Bereavement Disorder, with or without impairment. The results indicated that parental warmth at T3 was not a significant predictor of either of these measures of disordered grief. To further probe the potential iatrogenic effect of higher warmth to lead to higher grief we compared the level of grief at six years for parents with the highest (top 30%) and lowest (lowest 30%) scores on warmth at T3. We tested these effects on the two grief measures using 2 (FBP vs. control) x 2 (high vs. low warmth) analysis of covariance, controlling for T1 TRIG. The interaction was not significant. The main effects for warmth were significant for T4 general prolonged grief [F(1,60)=4.34, p = .04] and marginal significant for T4 TRIG [F(1,62)=3.14, p = .08]. The results indicated that those with higher warmth at T3 had higher grief than those with lower warmth as measured by both T4 TRIG (2.89 vs. 2.58) and general prolonged grief (2.21 vs. 1.81) at six years. The mean level of grief on T4 TRIG of the high warmth group was 2.79 (sd = .83), which corresponded to the midpoint on the 5 point scale, indicating that these symptoms were neither “true or false”. For T4 general prolonged grief, the mean level of symptoms of the high warmth group was 1.97 (sd = .84), which corresponds to a “slight sense of the grief symptom.”
Discussion
The current study demonstrated positive effects of the FBP on multiple domains of problem outcomes over six years including mental health (depression, general psychiatric distress), grief and alcohol abuse, as well as positive adjustment (parental warmth and coping efficacy). Significant main effects were found on six of the nine continuous parent adjustment and parenting variables and on three of five dichotomous measures of grief, mental health or alcohol abuse disorder assessed at the six-year follow-up. These findings extend prior findings on the effects of the FBP to domains of parent functioning at six-years that had not previously been tested (i.e., grief and alcohol use) including the prevalence of disorder in the domains of parental depression, grief and alcohol abuse. Although only three of 45 tests of moderated effects were significant, they indicate FBP effects on coping efficacy for females, an additional domain of functioning impacted by the FBP. The current paper also reported on the trajectory of program effects over six years and on mediating pathways that accounted for long-term program effects. Tests of mediating pathways provided evidence of multiple cascading effects of the program, by which change in one domain of functioning (e.g., positive parenting) impacted other domains of functioning (e.g., depression) over six years. The findings will be discussed in terms of their contribution to prior literature on the effects of parenting programs on parents’ adjustment and on the effects of interventions with bereaved adults. The implications of the findings for interventions with families who are bereaved from the death of a spouse/parent and the limitations of the study findings are also discussed.
The findings extend prior literature on the effects of parenting programs on parents’ own adjustment. In contrast to findings from the Barlow et al. (2012) meta-analysis which found that the effects of parenting programs on parents’ adjustment were significant at post-test and six-month follow-up but not at one year (Barlow et al., 2012), the current study found positive effects that lasted over six years after the program. One factor that may account for the long-term effects is that this trial focused on parents who themselves were at elevated risk for problem outcomes due to the experience of a major stressful event, the death of their spouse, in contrast to most of the trials in the Barlow et al. (2012) meta-analysis which included either parents of children being treated for behavior problems or samples of non-distressed parents. The only parenting program included in the Barlow et al. (2012) meta-analysis that focused on parents who experienced a major stressor (i.e., marital separation), was also the only one that reported significant long-term effects to reduce parental depression symptoms three years following the program (DeGarmo, Patterson & Forgatch, 2004). Younger bereaved spouses, such as those in the current study, are particularly at risk for the development of problem outcomes such as depression (Nolen-Hoeksema & Ahrens, 2002; Zisook, Shucter, Sledge & Mulvihill, 1993), and thus may be especially able to receive personal benefits from programs such as the FBP. A second factor that might account for the observed long-term effects is that although the program focused heavily on strengthening parenting skills, parents were also taught and practiced activities to improve their own adjustment including goal setting, support seeking and cognitive reframing skills to reduce negative thinking associated with depression. Schoenfelder, Sandler, Millsap, Wolchik, Berkel and Ayers (2013) found that different aspects of the FBP experience predicted improvements on different outcomes at post-test. Parents’ perception of group support and cohesion predicted decreases in depression, and parents’ reports of use of parenting skills predicted improvements in parenting. As described below, parenting and mental health problems have reciprocal influences on each other over time, so that the different outcomes promoted by different program components may have complimentary effects to maintain change on multiple domains of parent long-term adjustment.
The current findings advance the literature on interventions for the bereaved in several ways. First, this is the longest follow-up of a randomized trial to show an effect to improve grief, mental health problems, coping and alcohol abuse for bereaved adults (Currier et al., 2008; Wittouck, Van Autreve, De Jaegere, Portzky & van Heeringen, 2011). Second, the findings differ markedly from the conclusions from recent meta-analyses of the effects of programs for the bereaved (Currier et al., 2008; Wittouck, et al., 2011). Wittouck et al. (2011) reported positive effects for those who initially are experiencing high levels of distress or disordered grief, but not for preventive interventions with the general population of bereaved, and concluded that, “our results suggest that CG (complicated grief) can be treated but not prevented” (p. 77). However, the relatively small number of studies of preventive interventions (nine studies in Wittouck et al., 2011; 10 studies in Currier et al., 2008), which varied greatly on mode and length of the intervention and targeted very different bereaved populations suggest that the conclusions about the lack of effects of preventive interventions should be viewed with caution. For example, only one prevention study in the Wittouck et al., (2011) meta-analysis had a similar target population as the current study, young spousally-bereaved, and only three of the preventive interventions consisted of 10 or more sessions. In contrast to these conclusion, the current study found significant effects on multiple aspects of adjustment six years following the program for spousally-bereaved parents and the benefits were not greater for those with higher levels of problems at program entry (i.e., the baseline distress x program interactions were not significant). The medium effect sizes of the program effects at the six-year follow-up (range of d = .38 to .59) is comparable to the meta-analytic effects size at follow-up for bereavement programs for the indicated population in the Currier et al. (2008) meta-analysis.
Because spousally-bereaved are at risk for multiple problem outcomes (Keyes et al., 2014) it is important for an intervention that is designed to promote resilience to assess effects on multiple domains of functioning. Effects on several specific domains of functioning are particularly notable. This is the first finding of a significant effect of a preventive intervention to reduce the rates of bereaved people meeting DSM V proposed criteria for persistent complex bereavement disorder (PCBD), a condition identified for further study by the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders. This study adds to the findings of a treatment study (Shear, Wang, Skritskaya, Duan, Mauro & Ghesquiere, 2014) by showing that this condition is responsive to therapeutic interventions. The rate of the bereaved in the control group who meet criteria for PCBD with impairment (11.76%) is comparable to the expected rate of PCBD in the spousally-bereaved (Shear, 2015), indicating that although the sample was self-selected based on seeking help for their children’s bereavement adjustment, it is not an atypical sample in terms of the level of prolonged grief. The finding that the FBP lowered the rate of mild to moderate depression on the BDI, alcoholism on the SMAST and persistent complex bereavement disorder is evidence that the FBP reduces multiple domains of clinically significant problems. The numbers needed to treat in order to prevent one of these outcomes (7.54 for moderate depression; 8.50 for persistent complex bereavement disorder; 8.83 for alcoholism) indicates that a typical group of eight to ten parents (who are not selected for high levels of distress or grief) receiving the FBP would result in the prevention of at least one case of a serious disorder six years later. The maintenance of effects on parental warmth is important because of findings from this trial (Tein, Sandler, Ayers & Wolchik, 2006) as well as randomized trials of other parenting-focused prevention programs (Sandler, Schoenfelder, Wolchik & Mackinnon, 2011) that strengthening parenting leads to reductions in children’s mental health problems.
Three moderators of program effects at six years were found. The program effects to improve coping efficacy of mothers but not fathers may be due to the fact that the major focus of the program was on strengthening positive parenting, which may be more central to one’s sense of efficacy for mothers than fathers (Simon, 1992). The finding that the program was more effective in reducing depression for younger parents, and parental warmth for parents who were more recently bereaved indicates sub-populations that are most likely to receive benefits in terms of these specific outcomes. However, the fact that none of the variables examined moderated program effects across outcomes and the limited number of tests of moderation that were significant indicates that the program benefits were not constrained to a specific sub-group of spousally-bereaved. No significant moderation was found for several predicted moderators, such as cause of death and parents’ level of problems at baseline. These findings indicate that the FBP can have long-term benefits for the broad range of bereaved parents and stands in contrast to evidence from a prior meta-analytic study of 61 controlled studies of interventions with the bereaved that significant effects for those who had higher levels of problems at baseline, but not for lower risk bereaved (Currier, et al., 2008).
This is the first study to assess the trajectory of change in the bereaved following a preventive intervention. Bereaved parents in the FBP and those in the self-study condition reported reduced symptoms of depression, non-specific psychiatric distress and grief from pre to post-test, but the improvement was greater for the FBP than self-study group. Although grief and mental health problems decreased over the next six years in both groups, the rate of change did not differ between the groups and the differences between the FBP and self-study group were still found six years later. These findings are consistent with a maintenance of gains model. The current findings are the first to show maintenance of program effects for a preventive intervention for a bereaved population over a prolonged follow-up and extend the findings from several studies of treatment of complicated grief that have reported maintenance of gains in short-term follow-ups (Shear et al., 2014; Bryant et al., 2014; Boelen et al., 2007). The maintenance of gain model found in the current study differs from the increasing effects model found for parental depression by DeGarmo et al. (2004) in their 30-month follow-up of a parenting intervention with separated parents. In that study, there was no significant effect of the program on parental depression at post-test, but over thirty months, a multi-linkage effect was found in which reductions in children’s externalizing problems led to reductions in parents’ depressive symptoms. Unlike in the DeGarmo et al. (2004) study, improvements in youth externalizing problems did not mediate long-term program effects on any parent outcome variable.
The multi-path mediation models found reciprocal effects across domains of parent functioning, whereby improvements in warmth mediated long-term program effects to lower parental depression and general mental health problems and improvement in parental depression mediated long-term program effects on parental warmth. The finding that improved parental warmth mediated program effects on parents’ depression may be explained theoretically by considering the nature of the losses that occur following parental bereavement (e.g. Shear & Shair, 2005). One salient loss involves a supporter for the valued role of parent (Shapiro, 1994). The FBP’s emphasis on helping bereaved parents strengthen their relationship with their children may have led to enhanced sense of efficacy in the parental role which may be responsible for lower levels of depression over time. The finding that parents’ depressive symptoms partially mediated program effects on parental warmth is consistent with a large body of findings that parental depression and distress have a significant impact on parenting (e.g., Conger, et al., 2000). The effects of TRIG, BDI and parental warmth to mediate the program effect to increase coping efficacy can be viewed from the perspective of the dual process or two track model of adaptation to bereavement (Rubin & Malkinson, 2001; Stroebe & Schut, 1999). In these models the tasks of bereavement are to adapt to the grief over the loss of the deceased and to adapt to the demands of the post-death environment. It may be that successfully dealing with grief and depression (evidenced by lower TRIG and BDI at T3) and with the demands of parenting (evidenced by higher warmth at T3) increased bereaved parents’ general sense that they can handle the problems in their lives (evidenced by higher coping efficacy six years following the program).
The findings that increases in parental warmth were associated with an increase in both continuous measures of grief was not predicted. It may be that the closer relationship with the children which is evidenced by higher levels of warmth may increase occasions in which parents experience reminders of their loss of their spouse. There are two reasons why we do not consider the relationship between parental warmth and grief an iatrogenic effect of strengthening parenting. First, continuing to experience the loss many years later is increasingly recognized as a normative rather than a pathological aspect of grief (Carnelley, Wortman, Bolger, & Burke, 2006). However, when grief impairs functioning it can be considered pathological (Shear, 2015). The fact that there was no significant relation between parental warmth and the number of parents who met diagnostic criteria for prolonged complex bereavement disorder, either with or without impairment, reduces concern about the iatrogenic effect. Second, the low level of grief experiences at the six year follow-up, even among parents with high levels of parental warmth does not appear to exceed the experience of grief responses in the normative population (Carnelley et al., 2006).
Although depression was found to mediate program effects on grief when tested as a single mediator, it was no longer a significant mediator of either measure of grief at the six year follow-up when entered into a multiple mediator model in which the effects of grief and parental warmth at T3 were also included. This finding indicates that the program effects to reduce depression was not a pathway through which the program reduced long-term grief. In order to test the reciprocal pathway, we tested whether the effects of the FBP on TRIG at T3 mediated program effects on depression at the six-year follow-up. The results indicated that the prospective pathway from T3 TRIG to depression at the six-year follow-up was not significant. Prior literature has documented the distinctive nature of grief and depression in terms of different content of symptoms (e.g., Shear, 2015) and differences in the correlates of grief and depression (e.g. Boelen & Priggerson, 2007). Although the current prevention study (as well as prior treatment studies; Shear, 2005; 2014; Boelen et al., 2007; Bryant, et al., 2014) found significant effects on both depression and grief, these analyses are the first to find that the program impacted these two domains of symptoms through different pathways.
It may be that the multi-component nature of the current intervention as well as prior interventions (e.g. Shear, 2015; Boelen et al., 2007) account for the program effects on depression and grief, with some components impacting one outcome while other components impacting a different outcome. For example, a prior study found that parents’ perceptions of group support in the FBP predicted reductions in depression but not grief (Schoenfelder et al., 2013). One of the program components that may have been particularly responsible for the FBP effect on grief was the component on bereavement-related personal goals. Parents selected a bereavement-related personal goal in the first session and discussed their progress in accomplishing that goal over the course of the following 12 weeks. Goals that might have been particularly salient in terms of affecting the course of grief include planning and carrying out a special way of remembering the deceased and finding a special place to disperse ashes of the deceased (Sandler, Wolchik, Ayers, Tein & Luecken, 2013). Other components of the program, such as challenging negative thoughts and increasing positive activities were designed to reduce depression. Although the activities to strengthen parenting were not specifically designed to target depression they appear to have had that effect.
Although rigorously demonstrating the outcome-specific effects of differential program components would require experimentally testing their contribution (Bryant, et al., 2014), this may not be the most important goal for preventive interventions that are designed to promote resilience following major life stressors. A major stressor such as the death of one’s spouse increases the surviving spouse’s risk for developing problems across multiple domains of functioning as well as impairing positive functioning (Keyes et al., 2014). Resilience involves doing well in multiple domains of life; maintaining positive and satisfying developmentally appropriate roles as a parent and worker, effectively dealing with the stressors in one’s life as well as not experiencing mental health problems, substance abuse and prolonged disordered grief. Programs to promote resilience may want to include multiple components that allow participants to address the range of issues of most concern to them.
The current paper has significant implications for intervention programs with parentally bereaved families. The positive effects of the FBP on multiple domains of functioning of bereaved parents add to the findings of positive long-term effects for children on multiple domains of functioning that have been previously reported (e.g., internalizing and externalizing problems, Sandler et al., 2010; grief, Sandler, Ma et al., 2010), providing increased evidence of a “double prevention” effect of the FBP to improve outcomes for bereaved children and their parents. These findings support a contextual-resilience framework for programs with bereaved families (Sandler et al. 2008; Wyman, et al., 2001) that focuses on assisting people in adapting to the “changes that occur in the post-death environment and to the loss of the person who died” (Sandler et al., 2008, p. 2008). One implication of this framework is that because adaptation is seen as a normative process, interventions to promote healthy adaptation are appropriate for all who seek this assistance. In the current trial, the FBP was offered to all parents who sought out the program, with only those who were in need of more immediate clinical services excluded (Sandler et al., 2010). The finding that the FBP’s long-term benefits were not restricted to those who had higher levels of distress or grief at program entry supports the potential of such universally offered programs to have positive effects. A second implication is that programs for the bereaved include multiple components that address multiple potential pathways to resilience. Prior literature has supported the concept of multiple pathways to resilience in the bereaved (e.g., Bonanno et al., 2002). The design of the FBP was based on a multiple risk and protective factor model, in which each component was designed to address a different risk or protective factor identified in the empirical or theoretical literature (Sandler et al., 2013). The program structure individualized the program by having parents and children select their own goals and use the skills that were taught to help them accomplish these goals (Sandler et al., 2013). A third implication is that programs for bereaved children should include a component to strengthen parenting. Prior literature has strongly indicated that strengthening parenting mediates program effects to improve long-term outcomes in bereaved children (Tein et al., 2006), as well as other populations (Sandler et al., 2011; Sandler, Ingram, Wolchik, Tein & Winslow, 2015). The current results indicate that improved parenting has positive impacts on parents’ adjustment outcomes as well.
One limitation of the current study is that program effects on alcohol abuse, persistent complex bereavement disorder, and coping efficacy were only assessed at the six-year follow-up, so that the inferences concerning program effects on these outcomes need to be somewhat tentative. However, the fact that these effects were found in the context of a randomized experimental trial in which multiple baseline covariates were accounted for and attrition was not found to be differential across groups, provides support for attributing these effects to the FBP. A second limitation is that no significant mediators were found for alcoholism or alcohol problems. It may be that program effects on other aspects of parents’ lives may account for FBP on parents’ alcohol problems, such as other stressors or sources of social support that they encounter over time. A third limitation is that, although the sample included important sub-groups (e.g., 19% ethnic minorities,12% deaths from homicide or suicide and 15% accidents) the sample sizes were not large enough to assess effects within these high risk sub-groups. In addition, the fact that only people who agreed to participate in the experimental trial were included in this study limits the generalizability of the findings to the broader population who seek services but are not willing to be part of a research trial. A fourth limitation is that the effects of the FBP need to be replicated with a much larger and more heterogeneous sample of bereaved families. Future research, optimally conducted by an independent evaluator, is needed to replicate the effects found in this trial to increase confidence in the effectiveness of the FBP to improve outcomes for parents and children (Gottfredson et al., in press).
Acknowledgments
This research was funded by grants from the National Institute of Mental Health (3R01MH49155). The trial is registered at Clinicaltrials.gov identifier: NCT01008189
Footnotes
The program included people who were not biological or legal parents but who fulfilled a parenting role. As described below the sample studied in this paper was restricted to the parent who was a bereaved spouse of the parent who died.
We use the term ICG to refer to this measure throughout this paper for purposes of simplifying the presentation although the terms used to refer to the construct of disordered grief changed over time
Contributor Information
Irwin Sandler, Department of Psychology, REACH Institute, Arizona State University.
Jenn-Yun Tein, Department of Psychology, REACH Institute, Arizona State University.
Heining Cham, Department of Psychology, Fordham University.
Sharlene Wolchik, Department of Psychology, REACH Institute, Arizona State University.
Tim Ayers, Department of Psychology, REACH Institute, Arizona State University.
References
- Achenbach TM. Manual for the ASEBA School-age Forms and Profiles. Burlington: Research Center for Children, Youth & Families, University of Vermont; 2001. [Google Scholar]
- Achenbach TM. Manual for the Young Adult Self-report and Young Adult Behavior Checklist. Burlington: Dept. of Psychiatry, University of Vermont; 1997. [Google Scholar]
- Achenbach TM. Data from the CBCL and YABCL. 2003 Unpublished raw data. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Archer J. The nature of grief: The evolution and psychology of reactions to loss. Brunner-Routledge; New York: 1999. [Google Scholar]
- Ayers TS, Sandler IN, Twohey J. Conceptualization and measurement of coping in children and adolescents. In: Ollendick TH, Prinz RJ, editors. Advances in clinical child psychology. Vol. 20. New York: Plenum Press; 1998. pp. 243–301. [Google Scholar]
- Ayers TS, Wolchik SA, Sandler IN, Towhey JL, Lutzke Weyer JR, Jones S, Weiss L, Cole E, Kriege G. The Family Bereavement Program: Description of a theory-based prevention program for parentally-bereaved children and adolescent. Omega: Journal of Death and Dying. 2013–2014;68:293–314. doi: 10.2190/om.68.4.a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayers TS, Wolchik SA, Weiss L, Sandler IN, Jones S, Cole E, Barrow S. Family Bereavement Program: Group Leader Intervention Manual for Parent Program. Prevention Research Center, Arizona State University; 900 S. McAllister, Ave. Room 205, P.O. Box 876005, Tempe, AZ 85287-6005: 2008. [Google Scholar]
- Barlow J, Smailagic N, Huband N, Roloff, Bennett C. Group-based parent training programmes for improving parental psychosocial health. Campbell Systematic Reviews. 2012:15. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. The Annals Statistics. 2001;29:1165–1188. [Google Scholar]
- Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Annals of Statistics. 2001;29:1165–1188. [Google Scholar]
- Boelen PA, Prigerson HG. The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults: A prospective study. European Archives of Psychiatry and Clinical Neuroscience. 2007;257:444–452. doi: 10.1007/s00406-007-0744-0. [DOI] [PubMed] [Google Scholar]
- Boelen PA, de Keijser J, van den Hout MA, van den Bout J. Treatment of complicated grief: A comparison between cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology. 2007;75:277–284. doi: 10.1037/0022-006X.75.2.277. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Wortman CB, Lehman DR, Tweed RG, Haring M, Sonnega J, Carr D, Nesse RM. Resilience to loss and chronic grief: A prospective study from preloss to 18-months postloss. Journal of Personality and Social Psychology. 2002;83:1150–1162. doi: 10.1037//0022-3514.83.5.1150. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Neria Y, Mancini A, Litz B, Coifman &, Insel B. Is there more to complicated grief than depression and posttraumatic stress disorder? A test of incremental validity. Journal of Abnormal Psychology. 2007;116:342–351. doi: 10.1037/0021-843X.116.2.342. [DOI] [PubMed] [Google Scholar]
- Braver SL, Shapiro JR, Goodman MR. The consequences of divorce for parents. In: Fine MA, Harvey H, editors. Handbook of divorce and relationship dissolution. Mahwah, NJ: Erlbaum; 2005. pp. 313–337. [Google Scholar]
- Bruce ML, Kim K, Leaf PJ, Jacobs S. Depressive episodes and dysphoria resulting from conjugal bereavement in a prospective community sample. American Journal of Psychiatry. 1990;147(5):608–611. doi: 10.1176/ajp.147.5.608. (May 1990) [DOI] [PubMed] [Google Scholar]
- Bryant RA, Kenny L, Joscelyne A, Rawson N, Maccullum F, Cahill C, Hopwood S, Aderka I, Nickerson A. Treating prolonged grief disorder: A randomized clinical trial. JAMA Psychiatry. 2014;71:1332–1339. doi: 10.1001/jamapsychiatry.2014.1600. [DOI] [PubMed] [Google Scholar]
- Carnelley KB, Wortman CB, Bolger N, Burke CT. The time course of grief reactions to spousal loss: Evidence from a national probability sample. Journal of Personality and Social Psychology. 2006;91:476–492. doi: 10.1037/0022-3514.91.3.476. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Conger KJ, Rueter MA, Conger RD. The role of economic pressure in the lives of parents and their adolescents: The Family Stress Model. In: Crockett LJ, Silbereisen RK, editors. Negotiating adolescence in times of social change. New York: Cambridge University Press; 2000. pp. 201–223. [Google Scholar]
- Cook RD. Detection of influential observations in linear regression. Technometrics. 1977;19:15–18. [Google Scholar]
- Currier JM, Neimeyer RA, Berman JS. The effectiveness of psychotherapeutic interventions for bereaved persons: A comprehensive quantitative review. Psychology Bulletin. 2008;134:648–661. doi: 10.1037/0033-2909.134.5.648. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Shrout PE, Ergi G, Mendelsohn FS. Non-specific psychological distress and other dimensions of psychopathology. Archive of General Psychiatry. 1980;39:1229–1236. doi: 10.1001/archpsyc.1980.01780240027003. [DOI] [PubMed] [Google Scholar]
- DeGarmo DS, Patterson GR, Forgatch MS. How do outcomes in a specified parent training intervention maintain or wane over time? Prevention Science. 2004;5:73–89. doi: 10.1023/b:prev.0000023078.30191.e0. [DOI] [PubMed] [Google Scholar]
- Evenson RJ, Simon RW. Clarifying the relationship between parenthood and depression. Journal of Health and Social Behavior. 2005;46:341–358. doi: 10.1177/002214650504600403. [DOI] [PubMed] [Google Scholar]
- Faschingbauer TR. Texas Inventory of Grief-Revised manual. Houston, TX: Honeycomb; 1981. [Google Scholar]
- Gottfredson DC, Cook TD, Gardner FEM, Gorman-Smith D, Howe GW, Sandler IN, Zaff KM. Standards of evidence for efficacy, effectiveness, and scale-up research in prevention science: New generation. Prevention Science. doi: 10.1007/s11121-015-0555-x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner F, Burton J, Klimes I. Randomized controlled trial of a parenting intervention in the voluntary sector for reducing child conduct problems: Outcomes and mechanisms of change. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2006;47:1123–1132. doi: 10.1111/j.1469-7610.2006.01668.x. [DOI] [PubMed] [Google Scholar]
- Hagan MJ, Tein JY, Sandler IN, Wolchik SA, Ayers TS, Luecken LJ. Strengthening effective parenting practices over the long term: Effects of a preventive intervention for parentally bereaved families. Journal of Clinical Child & Adolescent Psychology. 2012;41:177–188. doi: 10.1080/15374416.2012.651996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haine RA, Sandler IN, Wolchik SA, Tein JY, Dawson-McClure SR. Changing the legacy of divorce: Evidence from prevention programs and future directions. Family Relations. 2003;52:397–405. [Google Scholar]
- Hofer MA. On the nature and consequences of early loss. Psychosomatic Medicine. 1996;58:570–581. doi: 10.1097/00006842-199611000-00005. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behavior. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S, Twohey JL. Parents’ Expression of Emotions Questionnaire: Psychometric properties. Paper presented at the 106th Annual Convention of the American Psychological Association; San Francisco. 1998. [Google Scholar]
- Keyes KM, Pratt C, Galea S, McLaughlin KA, Koenen KC, Shear MK. The burden of loss: Unexpected death of a loved one and psychiatric disorders across the life course in a national study. American Journal of Psychiatry. 2014;171:864–871. doi: 10.1176/appi.ajp.2014.13081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok O-M, Haine R, Sandler IN, Ayers TS, Wolchik SA. Positive parenting as a mediator of the relations between parental psychological distress and mental health problems of parentally-bereaved children. Journal of Clinical Child and Adolescent Psychology. 2005;34:261–272. doi: 10.1207/s15374424jccp3402_5. [DOI] [PubMed] [Google Scholar]
- Levinson D, Darrow CN, Klein EB, Levinson MH, McKee B. The seasons of a man’s life. Ballantine Books; New York: 1978. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test the significance of the mediated effect. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten A, Cicchetti D. Developmental cascades. Development and Psychopathology. 2010;22:491–495. doi: 10.1017/S0954579410000222. [DOI] [PubMed] [Google Scholar]
- Melhem NM, Walker M, Moritz G, Brent DA. Antecedents and sequalae of sudden parental death in offspring and surviving caregivers. Archives of Pediatric and Adolescent Medicine. 2008;162:403–410. doi: 10.1001/archpedi.162.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Múthen LK, Múthen BO. Mplus User’s Guide. 7. Los Angles: Múthen & Múthen; 1998–2012. [Google Scholar]
- Neimeyer RA, Hogan NS, Laurie A. The measurement of grief: Psychometric considerations in the assessment of reactions to bereavement. In: Stroebe MS, Hansson RO, Schut H, Stroebe W, Van den Blink E, editors. Handbook of bereavement research and practice: Advances in theory and intervention. Washington, DC: American Psychological Association; 2008. pp. 133–161. [Google Scholar]
- Neter J, Wasserman W, Kutner M. Applied linear regression analysis. Homewood, IL: Irwin; 1989. [Google Scholar]
- Nolen-Hoeksema S, Ahrens C. Age differences and similarities in the correlates of depressive symptoms. Psychology and Aging. 2002;17:116–124. doi: 10.1037//0882-7974.17.1.116. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychological Methods. 2010;15(3):209–233. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- Prigerson HO, Jacobs SC. Traumatic grief as a distinct disorder: A rationale, consensus criteria, and a preliminary empirical test. In: Stroebe MSH, Robert O, Stroebe Wolfgang, Schut Henk, editors. Handbook of bereavement research: Consequences, coping, and care. Washington, DC: American Psychological Association; 2001. pp. 613–645. [Google Scholar]
- Prigerson HG, Vanderwerker LC, Maciejewski PK. A case for inclusion of prolonged grief disorder in DSM-V. In: Stroebe MS, Hansson RO, Schut H, Stroebe W, Van den Blink E, editors. Handbook of bereavement research and practice: Advances in theory and intervention. Washington, DC: American Psychological Association; 2008. pp. 165–186. [Google Scholar]
- Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Asian M, Goodkin K, … Maciejewski PK. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Medicine. 2009;6(8):e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin S, Malkinson R. Parental response to child loss across the life cycle: Clinical and research perspectives. In: Stroebe MS, Hahnsson RO, Stroebe W, Schut H, editors. Handbook of bereavement research: Consequences, coping and care. Washington, DC: American Psychological Association; 2001. pp. 219–240. [Google Scholar]
- Sandler I, Ayers TS, Tein JY, Wolchik S, Millsap R, Khoo ST, Kaplan D, Ma Y, Luecken L, Schoenfelder E, Coxe S. Six-year follow-up of a preventive intervention for parentally-bereaved youth: A randomized controlled trial. Archives of Pediatrics and Adolescent Medicine. 2010;164:907–914. doi: 10.1001/archpediatrics.2010.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Ayers TS, Wolchik SA, Tein JY, Kwok OM, Haine RA, Twohey-Jacobs J, Suter J, Lin K, Padgett-Jones S, Weyer JL. Family Bereavement Program: Efficacy of a theory -based preventive intervention for parentally-bereaved children and adolescents. Journal of Consulting and Clinical Psychology. 2003;71:587–600. doi: 10.1037/0022-006x.71.3.587. [DOI] [PubMed] [Google Scholar]
- Sandler I, Ingram A, Wolchik S, Tein JY, Winslow E. Long-term effects of parenting-focused preventive interventions to promote resilience of children and adolescents. Child Development Perspectives. 2015;9:164–171. doi: 10.1111/cdep.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Ma Y, Tein JY, Ayers TS, Wolchik S, Kennedy C, Millsap R. Long-term effects of the Family Bereavement Program on multiple indicators of grief in parentally bereaved children and adolescents. Journal of Consulting and Clinical Psychology. 2010;78:131–144. doi: 10.1037/a0018393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Tein JY, Mehta P, Wolchik SA, Ayers TS. Coping efficacy and psychological problems of children of divorce. Child Development. 2000;71:1097–1118. doi: 10.1111/1467-8624.00212. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Schoenfelder EN, Wolchik SA, MacKinnon DP. Long-term impact of prevention programs to promote effective parenting: Lasting effects but uncertain processes. Annual Review of Psychology. 2011;62:299–329. doi: 10.1146/annurev.psych.121208.131619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Wolchik SA, Ayers TS, Tein JY, Luecken L. Family Bereavement Program (FBP) approach to promoting resilience following the death of a parent. Family Science. 2013;4:87–95. doi: 10.1080/19424620.2013.821763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Wolchik SA, Ayers TS. Resilience rather than recovery: A contextual framework on adaptation following bereavement. Death Studies. 2008;32:59–73. doi: 10.1080/07481180701741343. [DOI] [PubMed] [Google Scholar]
- Sandler I, Wolchik SA, Cruden G, Mahrer NE, Ahn S, Brincks A, Brown CH. Overview of meta-analyses of the prevention of mental health, substance use, and conduct problems. Annual Review of Clinical Psychology. 2014;10:243–273. doi: 10.1146/annurev-clinpsy-050212-185524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer ES. Children’s report of parental behavior: An inventory. Child Development. 1965;36:413–424. [PubMed] [Google Scholar]
- Schoenfelder EN, Sandler IN, Millsap RE, Wolchik SA, Berkel C, Ayers TS. Caregiver responsiveness to the Family Bereavement Program: What predicts responsiveness? What does responsiveness predict? Prevention Science. 2013;14:545–557. doi: 10.1007/s11121-012-0337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzer ML, Vinokur A, van Rooijen L. A self-administered Short Michigan Alcoholism Screening Test (SMAST) Journal of Studies on Alcohol. 1975;36(1):117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- Shapiro ER. Grief as a family process: A developmental approach to clinical practice. New York: Guilford Press; 1994. [Google Scholar]
- Shear MK. Complicated grief. New England Journal of Medicine. 2015;372:153–160. doi: 10.1056/NEJMcp1315618. [DOI] [PubMed] [Google Scholar]
- Shear MK, Wang Y, Skritskaya N, Duan N, Mauro C, Ghesquiere A. Treatment of complicated grief in elderly persons: A randomized clinical trial. JAMA Psychiatry. 2014;71:1287–1295. doi: 10.1001/jamapsychiatry.2014.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear K, Shair H. Attachment, loss and complicated grief. Developmental Psychobiology. 2005;47:253–267. doi: 10.1002/dev.20091. [DOI] [PubMed] [Google Scholar]
- Simon NM, Shear KM, Thompson EH, Zalta AK, Perlman C, Reynolds CF, Frank E, Melhem NM, Silowash R. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Comprehensive Psychiatry. 2007;48:395–399. doi: 10.1016/j.comppsych.2007.05.002. [DOI] [PubMed] [Google Scholar]
- Simon RW. Parental role strains, salience of parental identity and gender differences in psychological distress. Journal of Health and Social Behavior. 1992;33:25–35. [PubMed] [Google Scholar]
- Stroebe MS, Schut HAW. The Dual Process Model of coping with bereavement: Rationale and description. Death Studies. 1999;23:1–28. doi: 10.1080/074811899201046. [DOI] [PubMed] [Google Scholar]
- Taylor AB, MacKinnon D, Tein JY. Test of the three path mediated effect. Organization Research Methods. 2008;11:241–269. [Google Scholar]
- Tein JY, Sandler IN, Ayers TS, Wolchik SA. Mediation of the effects of the Family Bereavement Program on mental health problems of bereaved children and adolescents. Prevention Science. 2006;7:179–197. doi: 10.1007/s11121-006-0037-2. [DOI] [PubMed] [Google Scholar]
- Walters E, Kessler R, Nelson C, Mroczek D. Scoring the world health organization’s composite international diagnostic interview short form (CIDI-SF) 2002 Retrieved from http://www3.who.int/cidi/index.htm.
- West S, Finch J, Curran P. Structural equation models with nonnormal variables: Problems and remedies. In: Hoyle Rick H., editor. Structural equation modeling: Concepts, issues and applications. Thousand Oaks, CA: Sage; 1995. pp. 56–75. [Google Scholar]
- Wittouck C, Van Autreve S, De Jaegere E, Portzky G, van Heeringen K. The prevention and treatment of complicated grief: A meta-analysis. Clinical Psychology Review. 2011;31:69–78. doi: 10.1016/j.cpr.2010.09.005. [DOI] [PubMed] [Google Scholar]
- Wyman P, Sandler IN, Wolchik SA, Nelson K. Resilience theory and interventions: Cumulative developmental promotion and protection. In: Cichetti D, Rappaport J, Sandler IN, Weissberg R, editors. The promotion of wellness in children and adolescents. Washington, DC: CWLA Press; 2000. pp. 133–189. [Google Scholar]
- Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology. 2000;30:165–200. [Google Scholar]
- Zisook S, Schucter SR. Depression through the first year after the death of a spouse. American Journal of Psychiatry. 1991;148:1346–1352. doi: 10.1176/ajp.148.10.1346. [DOI] [PubMed] [Google Scholar]
- Zisook S, Shucter SR, Sledge P, Mulvihill M. Aging and bereavement. Journal of Geriatric Psychiatry and Neurology. 1993;6:137–143. doi: 10.1177/089198879300600302. [DOI] [PubMed] [Google Scholar]