Abstract
Background
Traditional intra-articular arthroscopic repair techniques for massive anterosuperior rotator cuff tears are technically demanding and necessitate sacrifice of the rotator interval to enable visualization. An interval slide allows mobilization through release of the medial aspect of the rotator interval, while leaving the lateral, bridging fibers intact.
Questions/Purposes
The purpose of this study was to report a novel, arthroscopic, open-equivalent technique using the subdeltoid space to address these tears along with early clinical results.
Methods
A retrospective review of prospectively collected data identified 11 consecutive arthroscopic massive anterosuperior rotator cuff repairs with a concomitant biceps tenodesis performed by the senior surgeon using a uniform technique. Outcome measures included range of motion, visual analog scale for pain, rotator cuff strength, American Shoulder and Elbow Surgeons (ASES) outcome scale, and Short Form-12 (SF-12).
Results
Average length of follow-up was 22.2 months (range 12.5–30.0 months). Visual analog scale (VAS) pain scores, ASES, and SF-12 all demonstrated significant improvement from pre-op to final follow-up from 6.2 to 0.9 (p < 0.05), 27.4 to 82.8 (p < 0.05), and 26.6 to 45.5 (p < 0.05) respectively. Average forward flexion improved from 145° to 160° (p < 0.05). Seven of the nine patients with a positive preoperative belly press had a negative test at final follow-up. Nine of the 10 patients with a positive lift off test demonstrated a negative test on final follow-up. Ninety-one percent reported they were satisfied with their outcome.
Conclusions
The described modified all-arthroscopic subdeltoid approach for anterosuperior cuff repairs enabled an open-equivalent interval slide technique that preserved the bridging lateral fibers of the rotator interval and demonstrated promising early-term clinical results.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9497-5) contains supplementary material, which is available to authorized users.
Keywords: massive anterosuperior rotator cuff tears, arthroscopic rotator cuff repair, subdeltoid space, rotator interval, interval slide
Introduction
Rotator cuff tears are a common cause of shoulder pain and disability. Several tear patterns have been described [16, 28, 35]. Large and massive rotator cuff tears, defined functionally as tears that involve two or more tendons, present two challenges—tissue mobilization and fixation [9, 14, 18, 38]. Improvements in advanced imaging techniques and arthroscopic acumen have led to an increased recognition of two-tendon anterosuperior rotator cuff tears, which involve the supraspinatus and at least the upper one third of the subscapularis tendon insertion [12]. Posterior propagation into the infraspinatus and concomitant involvement of the long head of the biceps are not uncommon as retraction of the subscapularis tendon causes medialization of the lateral rotator interval confluence, disrupting the bicipital sling [3, 18, 39, 41]. Traditionally, an open approach was used to address these tears due to limitations in visualization and tissue mobilization [2, 11, 21, 31]. More recently, several arthroscopic techniques have been described with favorable results [5, 7, 13, 20, 22, 33, 40]. A common theme among arthroscopic techniques designed to repair massive anterosuperior rotator cuff tears involves purposeful disruption of the rotator interval tissue to facilitate tendon excursion and mobilization [5, 7, 13, 20, 22, 33, 40].
Neer [32] described the rotator interval as the triangular area bound medially by the coracoid process, superiorly by the anterior edge of supraspinatus, and inferiorly by the superior edge of subscapularis. The rotator interval includes the coracohumeral ligament (CHL), the superior glenohumeral ligament (SGHL), and long head of the biceps tendon (LHBT) [3, 4, 8, 30]. These structures have widely been accepted as important biomechanical stabilizers of the shoulder based on the findings of several cadaver studies [36]. Most notable of these studies was a sectioning study conducted by Harryman et al. [17], which demonstrated that glenohumeral translation increases with rotator interval sectioning but decreases with imbrication [19, 30]. In addition, the CHL has been shown to envelope the supraspinatus and subscapularis tendons laterally, serving to stabilize the tendons [1]. Despite the reported biomechanical contributions of these structures, they are frequently sacrificed during anterosuperior tear mobilization and repair.
Lo and Burkhart [30, 31] described the interval slide, in which the anterosuperior rotator cuff is mobilized by releasing the medial aspect of the rotator interval while leaving the lateral “comma sign” intact. The “comma sign” bridges the leading edge of supraspinatus and subscapularis tendons [6, 24–26]. As of yet, no formal biomechanical studies have compared the strength of repair between this interval slide technique and those that sacrifice the bridging tissue laterally.
Traditional intra-articular arthroscopic techniques for subscapularis repair are technically demanding and necessitate sacrifice of the lateral “comma sign” portion of the rotator interval to enable visualization and instrumentation. To alleviate this issue, we developed a novel, all-arthroscopic rotator interval slide to repair large and massive anterosuperior rotator cuff tears using the subdeltoid space. The systematic, sequential, and safe exposure of the subdeltoid space described by O’Brien et al. [34] enables the surgeon to perform an open-equivalent procedure through the arthroscope with an extra-articular en fosse view of the anterior shoulder.
The purpose of this study was to report a novel, arthroscopic, open-equivalent, technique using the subdeltoid space to address massive anterosuperior rotator cuff tears along with early clinical results. We hypothesize that this novel technique will provide a safe and efficacious method for anterosuperior rotator cuff fixation, while providing unfettered access to the anterior shoulder.
Patients and Methods
Population
Our institutional review board approved this study. We identified 11 consecutive arthroscopic massive anterosuperior rotator cuff repairs performed by the senior surgeon (LVG) between May 2011 and December 2012. Diagnosis was based upon patient history, physical examination, and magnetic resonance imaging (MRI). Reverse total shoulder was not considered in this cohort as these patients, despite having massive rotator cuff tears, have reparable rotator cuff tears. Reverse shoulder replacement is only considered if the rotator cuff is deemed irreparable. All suspected anterosuperior cuff tears were confirmed at the time of diagnostic arthroscopy and subsequently repaired using the modified all-arthroscopic interval slide technique through a subdeltoid exposure described below.
Surgical Technique
Regional brachial plexus anesthesia and the beach chair position were used. The operative extremity was prepped and draped in the usual sterile fashion, and an examination under anesthesia was performed to assess range of motion and glenohumeral stability. The arthroscope was first introduced into the glenohumeral joint via a standard posterior portal. A 30° scope was routinely used. A second portal was then established anteriorly. Often, the rotator interval was not clearly identified since the subscapularis was torn and retracted. In these cases, the anterior portal was placed just lateral to the “comma sign.” An accessory anterolateral portal was also established over the biceps tendon. Spinal needle localization was used for accurate placement of each portal (Fig. 1). The LHBT was tenotomized for later tenodesis (Fig. 2).
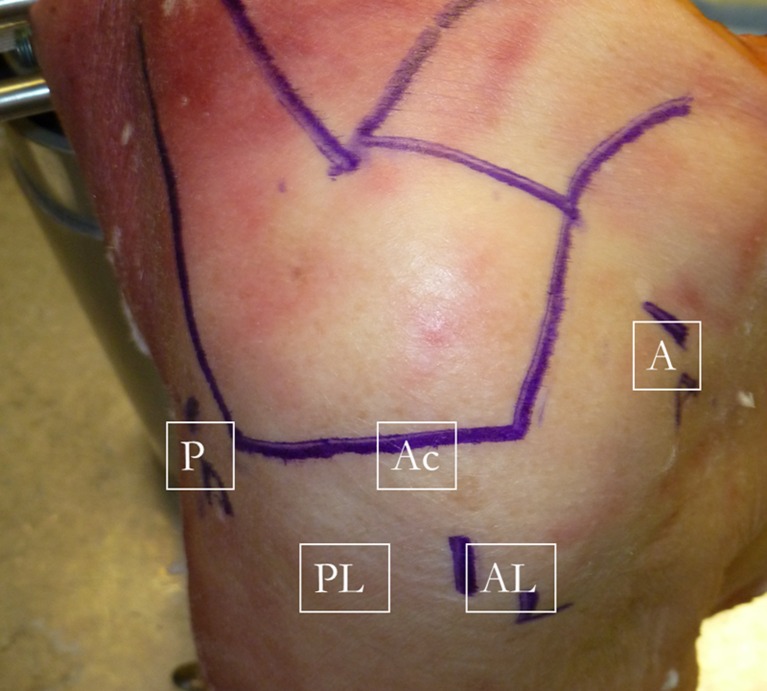
Fig. 1.
External view of the shoulder showing the standard portals used in repairing anterosuperior rotator cuff tears. For the working portion of the case, the arthroscope is placed in the posterolateral portal (PL). When working anteriorly either on the subscapularis or the LHBT, a penetrating device such as a “bird’s beak” can be placed through the anterior portal (A) while a grasper is placed through the anterolateral portal (AL) to aid in manipulating the tissue and feeding the sutures into the penetrator. As the repair progresses superiorly into the supraspinatus, anchors can be placed through a percutaneous portal on the lateral edge of the acromion (Ac). The scope is left in the PL portal, and an automatic suturing device is placed through the AL portal while sutures are retrieved through the A portal. The repair proceeds from anteroinferior to posterosuperior. The sutures are then tied from posterior to anterior.
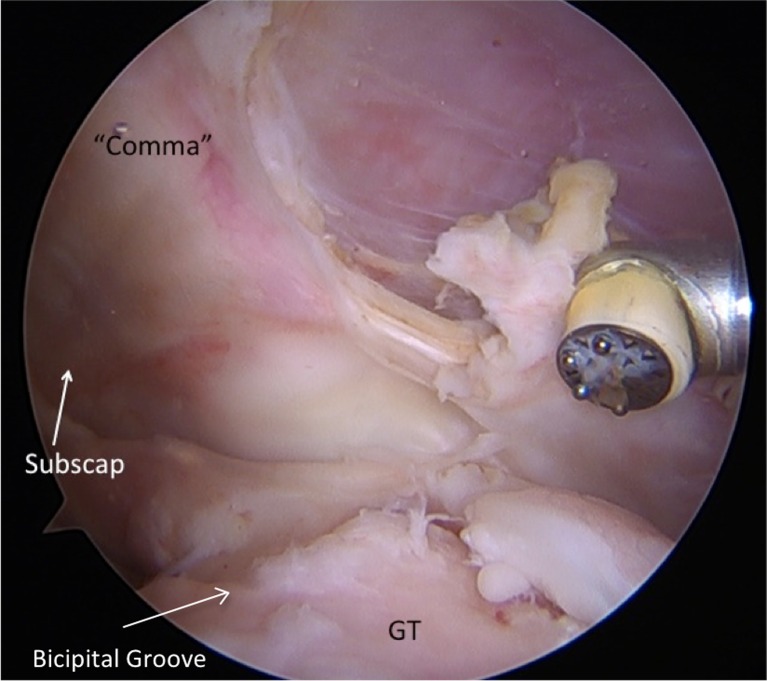
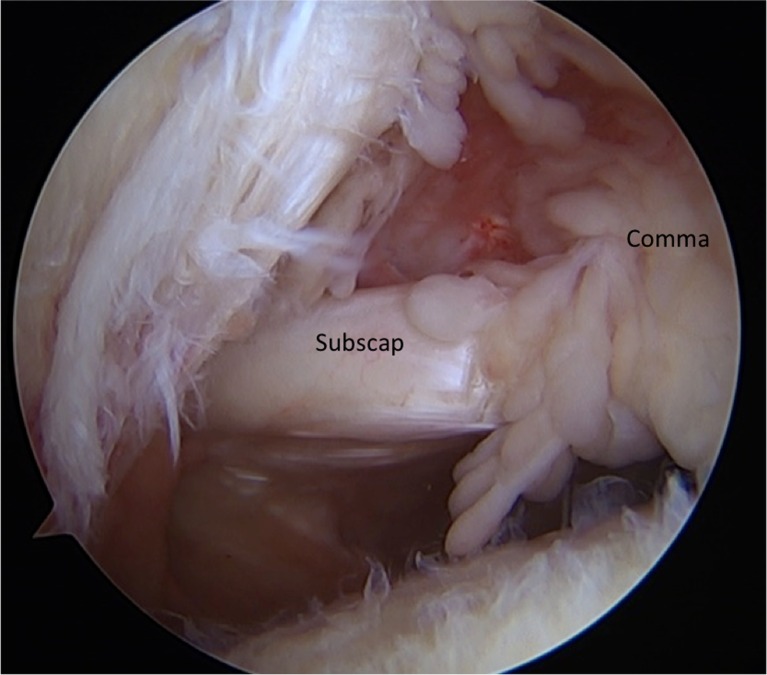
Fig. 2.
View from the posterior portal with the arthroscope in the joint showing the rotator cuff tear. The subscapularis tear is connected to the tear of the supraspinatus through the “comma sign.” (Subscap = subscapularis, GT = greater tuberosity).
The arthroscope was then repositioned into the subacromial space. A subacromial decompression and acromioplasty were performed to facilitate exposure and treat concomitant impingement. Step-wise exposure of the subdeltoid space was then undertaken, as previously described by O’Brien et al. [34]. The upper extremity was then repositioned in 90° of forward flexion, 90° of elbow flexion, 15–30° of arm abduction, and 45° of external rotation. The forward flexion allowed the humeral head to fall posterior opening the subdeltoid space anteriorly, and the external rotation brought the lesser tuberosity and the bicipital groove into view. The coracoacromial ligament, conjoint tendon, pectoralis major tendon, and humeral shaft were all exposed using radiofrequency ablation and a mechanical shaver. The extent of subdeltoid exposure was dictated by the necessity of exposure to address the pathology. Early in the subdeltoid work, the arthroscope was placed in the anterolateral portal, and the anterior portal was used as the working portal (Fig. 3). A traction suture was placed in the superior aspect of the subscapularis to aid in mobilization. This traction suture was then pulled through the posterior portal to facilitate dissection between the subscapularis and conjoint tendon. As the dissection progresses medially, care must be taken to identify and protect the axillary nerve. The superior border of the subscapularis was also freed from the base of the coracoid, and the medial aspect of the rotator interval is divided. Care was taken to preserve the lateral aspect of the rotator interval. The traction suture was then retrieved through the anterior portal to facilitate dissection between the subscapularis and the glenoid. The middle glenohumeral ligament was routinely divided. The axillary nerve must be protected as the dissection proceeds inferiorly since it will enter the field at the inferior aspect of the subscapularis muscle belly. A coracoplasty was not routinely performed.
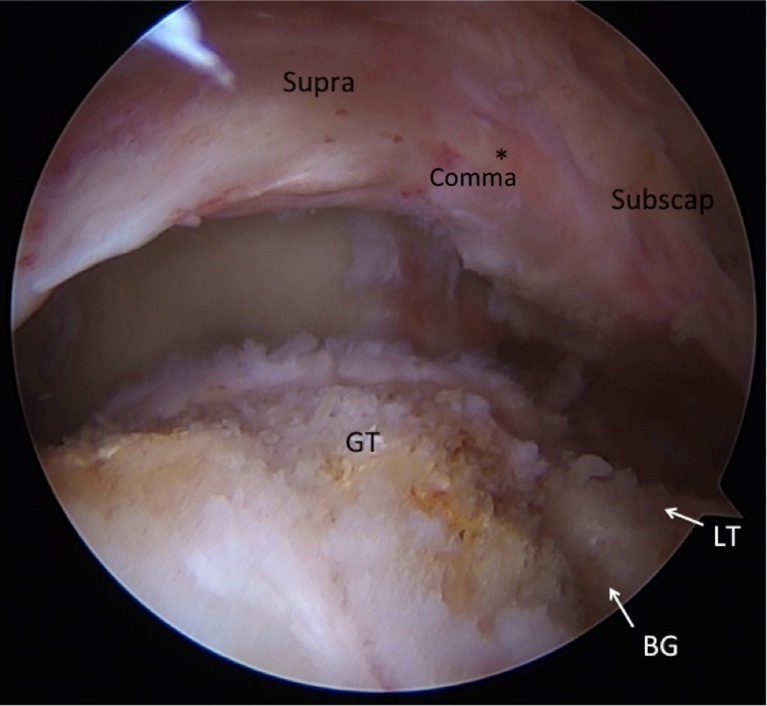
Fig. 3.
An anterosuperior rotator cuff tear as shown from the subacromial space while viewing from the anterolateral portal. There is a cuff of tissue that connects the subscapularis to the supraspinatus (asterisk). This tissue represents the “comma sign” and it is preserved throughout the repair. (Supra = supraspinatus, Subscap = subscapularis, GT = greater tuberosity, BG = bicipital groove, LT = lesser tuberosity).
The footprint locations for the supraspinatus and subscapularis on the greater and lesser tuberosities, respectively, were then abraded down to bleeding bone and suture anchors were placed as dictated by the tear. A posterolateral portal was then made where the arthroscope was placed for viewing. This left two portals, the anterior and the anterolateral, available for working portals while the posterolateral portal is used for visualization. Horizontal mattress sutures were used to secure the two tendons. For the subscapularis, the sutures were either passed with a suture device through the anterolateral portal or with a penetrator placed through the anterior portal aided with a grasper through the anterolateral portal. The repair proceeded from inferior to superior. Care was taken to avoid passing sutures through the conjoint tendon but still incorporating the tendinous portion of the subscapularis. Sutures were passed through the supraspinatus with a suture device. A transosseous equivalent repair was performed with two lateral row knotless anchors. After the medial row anchors were tied, the ones through the supraspinatus are passed through the posterior knotless anchor, and the ones through the subscapularis were passed through a knotless anchor placed in the bicipital groove. The free stay-suture from the bicipital groove knotless anchor was used to perform a biceps tenodesis with a lasso-loop stitch configuration in a similar fashion to that described by Levy [23] (Figs. 4 and 5) The bicipital tunnel was then released distally to the proximal margin of the pectoralis major to ensure decompression of the extra-articular segment of LHTB. When working anteriorly, either for placement of the anchors in the lesser tuberosity or bicipital groove, and for passing of the sutures through the subscapularis or LHBT, visualization was maximized with the shoulder in forward flexion and external rotation. When working superiorly, either for placement of the anchors in the greater tuberosity or for passage of the sutures through the supraspinatus and/or the infraspinatus, visualization was maximized with the shoulder adducted by the patient’s side and in neutral rotation.
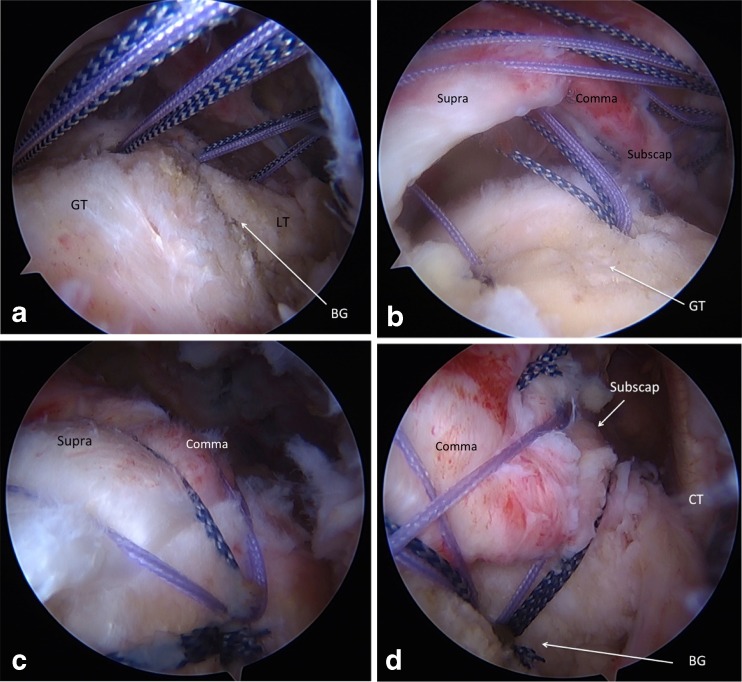
Fig. 4.
Anchors are placed from anterior to posterior. In this case, two anchors are placed into the lesser tuberosity, and two anchors are placed in the greater tuberosity (a). Anchors are placed at the articular margin as they will serve as a medial row. Sutures are then passed through the rotator cuff in a horizontal mattress fashion (b). The most anteroinferior sutures are typically passed through the subscapularis with a penetrating device (such as a bird’s beak penetrator), taking care to avoid the conjoint tendon. Sutures are passed through the “comma sign” tissue and into the supraspinatus maintaining its integrity as one cuff of tissue. Once the medial row sutures are tied, one limb from each knot is placed through a knotless, lateral row anchor. One anchor is then placed in the posterolateral aspect of the greater tuberosity footprint (c), and the other is placed in the bicipital groove (d). (BG = bicipital groove, GT = greater tuberosity, Supra = supraspinatus, Subscap = subscapularis, CT = conjoint tendon).
Fig. 5.
At the conclusion of the case, the arthroscope is placed back inside the glenohumeral joint where tensioning and repair of the subscapularis tendon can be adequately evaluated.
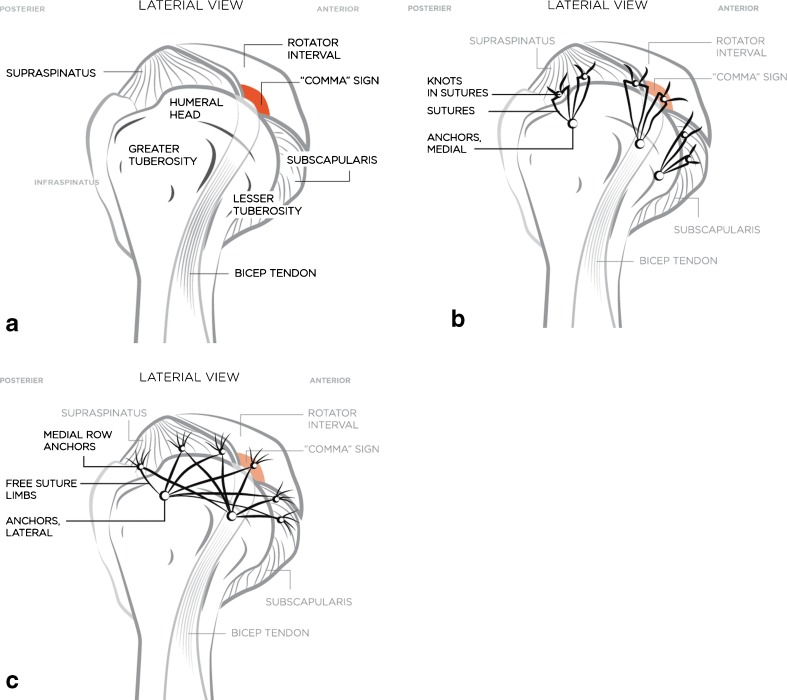
A schematic representation of the construct is provided (Fig. 6).
Fig. 6.
Schematic representation of the technique as seen from a lateral view. The bridging “comma sign” tissue between the supraspinatus and subscapularis is maintained (a). The supraspinatus, subscapularis, and bridging “comma sign” tissue are then brought over as a single cuff of tissue to a medial row of suture anchors with one anchor in the bicipital groove allowing for concomitant biceps tenodesis (b). The free suture limbs are then placed through knotless anchors forming a lateral row (c).
Postoperative Rehabilitation
All patients were managed with the standard post-operative rotator cuff rehabilitation protocol [27], which called for 6 weeks of sling immobilization, except for Codman and pendulum exercises. After 4 weeks, patients were allowed to come out of the sling for passive range of motion under the direction of a trained physical therapist. Given the subscapularis repair, external rotation was limited to 30° for the first 6 weeks. At 6 weeks, therapy was focused on regaining full range of motion by week 12. If at this point patients were able to achieve 90–95% of their range of motion, a strengthening program was initiated. The goal was for complete return to activity without limitation at 6 months post-operatively.
Outcome Measurements
Demographic data including age, sex, hand dominance, and time to surgery were collected. Objective clinical measurements were also gathered at each follow-up visit by the attending surgeon, including range of motion (forward flexion, external rotation, and internal rotation), visual analog scale (VAS) for pain, supraspinatus strength, infraspinatus strength, and subscapularis status as determined by the belly press test and lift off tests [15]. Subjective satisfaction was queried and outcome scores were also assessed pre-operatively and at latest follow-up using the American Shoulder and Elbow Surgeons (ASES) outcome scale (100-point scale) and Short Form-12 (SF-12) Physical and Mental Component Scores (100-point scale) [29, 37]. Required length of follow-up was set to 1 year.
Cohort Characteristics
Eleven consecutive patients with massive anterosuperior rotator cuff tears were repaired with the aforementioned arthroscopic subdeltoid technique. There were six males and five females. The average age was 62 (range 54–73). Six shoulders were right and five were left. The dominant shoulder was affected in five patients. All but one patient identified an acute injury. The most common mechanism was mechanical ground level fall (n = 6). Other reported mechanisms included tennis (n = 1), bocce ball (n = 1), bicycle accident (n = 1), shoveling snow (n = 1), and idiopathic atraumatic (n = 1). One patient received workers’ compensation.
Diagnostic arthroscopy confirmed preoperative assessment for all 11 patients. Three patients had two-tendon tears (supraspinatus and subscapularis) and eight patients had three-tendon tears (propagation into the infraspinatus). No tears extended into the teres minor tendon. Preoperative assessment suggested bicep involvement, which was confirmed, in all cases (tearing, inflammation, subluxation/instability, and complete tear). All patients underwent an arthroscopic biceps tenodesis as outlined in the surgical technique if the tendon was not otherwise torn. An average of five anchors (range 4–6) were used to perform each repair. Average time to surgery was 7 months (range 1–24 months). Average length of follow-up was 22.2 months (range 12.5–30.0 months) (Table 1).
Table 1.
Baseline cohort characteristics
| Number of patients | 11 |
| Mean time to surgery (range) in months | 7.0 (1–24) |
| Mean follow-up time (range) in months | 22.2 (12.5–30.0) |
| Mean age (range) in years | 62 (54–73) |
| Gender (male/female) | 6/5 |
| Side (right/left) | 6/5 |
| Side (dominant/nondominant) | 5/6 |
| Mean number of anchors used (range) | 5 (4–6) |
| Two-tendon tears (supraspinatus/subscapularis) | 3 |
| Three-tendon tears (subscapularis/supraspinatus/infraspinatus) | 8 |
| Biceps tenodesis | 11 |
| Workers’ compensation | 1 |
Data Analysis
Descriptive statistics were calculated according to standard methods when appropriate to determine mean, standard deviation, frequency, and ranges. Clinical outcome scores were analyzed by determining the mean value of each statistical measure at the pre-operative and post-operative time points. The pre-operative scores and post-operative scores were then compared against each other in a two-tailed t test to determine clinically significant changes. Statistical significance was set at p < 0.05. All statistics were generated using Microsoft Excel software.
Results
Full detailed results are outlined in Table 2. Briefly, VAS pain scores decreased from 6.2 pre-operatively to 0.8 (p < 0.001) at final follow-up. Mean ASES score increased from 27.4 pre-operatively to 82.8 at final follow-up (p < 0.001). Average SF-12 PCS also increased from 26.6 pre-operatively to 45.5 post-operatively (p < 0.001), while SF-12 MCS remained stable at 53.7 pre-operatively and 54.2 at final follow-up (p = 0.60).
Table 2.
Clinical outcome measures
| Mean ± SD (range) | ||||
|---|---|---|---|---|
| Outcome | Pre-operative | Post-operative | Improvement | P |
| ASES score | 27.42 ± 7.64 (13.35–34.99) | 82.82 ± 27.67 (21.7–100) | 55.4 | <0.001 |
| SF-12 PCS | 26.58 ± 3.49 (22.9–32.6) | 45.49 ± 13.4 (22.9–56.6) | 18.91 | <0.001 |
| SF-12 MCS | 53.74 ± 3.24 (48.5–58.4) | 54.17 ± 4.1 (48.5–60.8) | 0.43 | 0.6 |
| VAS pain | 6.18 ± 1.54 (4–9) | 0.82 ± 2.09 (0–7) | 5.36 | <0.001 |
| Forward flexion, deg | 145 ± 51.26 (30–180) | 160 ± 35.73 (90–180) | 15 | <0.05 |
| Lift-off test, positive | 10 | 1 | ||
| Belly press, positive | 9 | 2 | ||
| Patient satisfaction | 91% | |||
ASES American Shoulder and Elbow Society score, SF-12 PCS Short Form-12 Physical Component Score, SF-12 MCS Short Form-12 Mental Component Score, VAS visual analog scale, deg degrees, SD standard deviation
Active forward flexion and internal rotation improved from pre-operative evaluation to post-operative follow-up, both reaching statistical significance. Seven of the nine patients with a positive pre-operative belly press had a negative test at final follow-up. Nine of the 10 patients with a positive lift off test demonstrated a negative test on final follow-up. Ninety-one percent (10 of 11 patients) reported that they were satisfied with their outcome and would elect to have the procedure again. Additionally, these 10 patients all returned to activity without limitation.
The one patient who was dissatisfied required revision surgery for subscapularis re-tear sustained during a fall 2 weeks after the initial anterosuperior cuff repair. On retrospective analysis, this patient was the patient with the lower amount of pre-operative forward flexion (30) and highest pre-operative pain scores (9). She had persistent asymmetric strength and range of motion at most recent follow-up and had the largest limitation in forward flexion (90) and highest VAS pain score (7). Of note, this patient was not the patient who received workers’ compensation. No other patients in the cohort required reoperation. Additionally, none of the patients had evidence of transient or permanent neurovascular injury (Table 2).
Discussion
Arthroscopic management of massive anterosuperior rotator cuff tears presents unique operative challenges with regards to tissue mobilization and restoration of biomechanical stability. Traditional arthroscopic techniques call for the surgeon to sacrifice the rotator interval tissue, particularly the lateral fibers which coalesce to bridge the supraspinatus and subscapularis, to ensure adequate visualization and instrumentation. Using the described modified all-arthroscopic subdeltoid approach to the anterosuperior cuff repair, the surgeon is able to perform an open-equivalent interval slide technique and thus able to preserve the bridging lateral fibers. In our series of 11 patients, we demonstrated promising early results of this technique, with 91% of patients satisfied at average 2-year follow-up.
Previous reports of all-arthroscopic repairs of massive anterosuperior cuff tears are relatively limited in the literature. Ide et al. [18] published their results on 20 anterosuperior cuff tears treated with an intra-articular all-arthroscopic technique. All patients had a minimum follow-up of 2 years and were evaluated by both subjective measures and objective measures including MRI to assess the quality and durability of repair. Their cohort showed significant improvement in UCLA scores post-operatively. However, they also reported a re-tear rate of 35%. While the re-tear population still had improved functional scores compared to the pre-operative state, this population did have significantly worse outcomes when compared to the patients with intact repairs. Similar positive clinical outcomes were also seen in a prospective, multicenter study of 103 patients published by Toussaint et al. [40], with only an 8% re-tear rate at 1-year follow-up. Nho et al. [33] published a retrospective review of 17 patients who underwent arthroscopic anterosuperior cuff repair with an open biceps tenodesis. Again, significant improvement was seen post-operatively.
The first cohort study of arthroscopic anterosuperior cuff tears was published by Bennett [5] and evaluated a cohort of 35 patients with anterosuperior cuff tears treated with an all-arthroscopic technique involving attempted reconstruction of the bicipital sheath. The cohort showed significant improvements in both clinical and subjective outcome measures. The author suggests that the improvement in outcomes was in large part due to the recognition of hidden lesions within the lateral rotator interval and bicipital sheath, which were addressed in the repair. While most current literature tends to advocate LHBT tenodesis, the importance of the lateral rotator interval as a biomechanical structure remains evident.
The intra-articular interval slide technique described by Lo and Burkhart [25, 26] provided an alternative, allowing the surgeon to adequately mobilize massive tears for anatomic re-approximation without disruption of the lateral bridging fibers of the interval tissue. This technique involves performing the interval slide from an intra-articular position. The distinction in our proposed technique involves utilization of the subdeltoid space, which allows for an en face view of the anterior shoulder and visualization of the repair. In addition, technical challenges of the interval slide, such as suture management, are significantly decreased.
This technique demonstrates the versatility of the subdeltoid space. Drakos et al. [10] initially described using the subdeltoid space to perform a transfer of the long head of the biceps tendon to the conjoint tendon for cases of chronic refractory biceps tendonitis. O’Brien et al. [34] later described their systematic and sequential technique for exposure of the subdeltoid space, which begins by tracing the coracoacromial ligament medially to the coracoid, then tracing the conjoint tendon distally, followed by exposing the proximal margin of the pectoralis major tendon laterally to its insertion onto the humerus. By following their exposure recommendations, vital neurovascular structures are readily protected. Use of the subdeltoid space for repair of the anterosuperior cuff tears described in our series provided access to the anterior shoulder, allowing visualization of the repair.
Perhaps the most important technical pearl of this technique is to position the shoulder in forward flexion and external rotation. When viewing through the anterolateral portal, the bicipital groove is typically directly below the arthroscope with the lesser tuberosity anterior and the greater tuberosity posterior. This allows excellent visualization of the anterior aspect of the shoulder. With the lateral rotator interval tissue left intact, the subscapularis and supraspinatus are repaired as a single cuff of tissue. Approaching repair of the anterosuperior cuff in this manner is analogous to repairing posterosuperior tears of the supraspinatus and infraspinatus, with which most surgeons have more experience. The technique proposed in this report can be seen as the mirror image of a traditional posterosuperior rotator cuff repair. Again, position of the arm in the beachchair position makes accomplishing this intuitive.
Another aspect of our proposed surgical technique that is unique to the interval slide is the incorporation of the biceps tenodesis into the lateral row anchor in the bicipital groove. Although most current published techniques for arthroscopic fixation of the anterosuperior rotator cuff describe biceps tenotomy or tenodesis, no definitive consensus exists regarding proper management of the biceps, even though several articles have shown that subscapularis tears are associated with some amount of lateral rotator interval damage. This lateral interval damage often leads to biceps pulley pathology and subsequent biceps instability and pain [3, 41]. Our technique advocates for biceps tenodesis in every patient in which the LHBT is still present. We accomplish the fixation through utilization of the subdeltoid space, which allows an extra-articular view of the subscapularis footprint and bicipital groove. Because of the exposure gained through this approach, we are able to incorporate the tenodesis into the rotator cuff repair using the same suture anchors.
Our study has several limitations. Although prospectively collected, the data represents a retrospective review of limited clinical data of a small cohort over a relatively short follow-up period. All patients underwent surgery and post-operative follow-up examination by one surgeon, which is a potential source of bias. In addition, no post-operative imaging was collected to confirm healing of the repaired tendons. However, the goal of this project was not to formally test the outcomes of our proposed technique but to simply describe the technique and provide some supporting evidence that our patient population is achieving good outcomes as demonstrated by significant improvements in subjective outcome measures with improved strength and ROM on physical examination. Additionally, while several sectioning studies of the rotator interval have shown the biomechanical strength and stability imparted by this tissue, no formal biomechanical testing has been completed to evaluate the strength of the lateral bridging fibers of the rotator interval in the setting of massive anterosuperior rotator cuff tears. It follows that formal biomechanical studies must be undertaken in order to evaluate the strength of this repair as compared to traditional, intra-articular techniques which sacrifice the bridging, lateral fibers in favor of increased mobilization.
In conclusion, this novel all-arthroscopic modification of the rotator interval slide technique with utilization of the subdeltoid space is a safe and effective method for mobilization and fixation of massive anterosuperior rotator cuff tears that preserves the biomechanical integrity of the lateral rotator interval tissue that bridges the supraspinatus and subscapularis tendons.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(PDF 1225 kb)
Compliance with Ethical Standards
Conflict of Interest
Keith T. Corpus, MD, Samuel A. Taylor, MD, Stephen J. O’Brien, MD, MBA, and Lawrence V. Gulotta, MD have declared that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence
Case series, Level of evidence IV
References
- 1.Arai R, Nimura A, Yamaguchi K, et al. The anatomy of the coracohumeral ligament and its relation to the subscapularis muscle. J Shoulder Elb Surg. 2014 doi: 10.1016/j.jse.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Bartl C, Senftl M, Eichhorn S, et al. Combined tears of the subscapularis and supraspinatus tendon: clinical outcome, rotator cuff strength and structural integrity following open repair. Arch Orthop Trauma Surg. 2012;132(1):41–50. doi: 10.1007/s00402-011-1400-8. [DOI] [PubMed] [Google Scholar]
- 3.Bennett WF. Subscapularis, medial, and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of “hidden” rotator interval lesions. Arthroscopy. 2001;17(2):173–180. doi: 10.1053/jars.2001.21239. [DOI] [PubMed] [Google Scholar]
- 4.Bennett WF. Visualization of the anatomy of the rotator interval and bicipital sheath. Arthroscopy. 2001;17(1):107–111. doi: 10.1053/jars.2001.21024. [DOI] [PubMed] [Google Scholar]
- 5.Bennett WF. Arthroscopic repair of massive rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003;19(4):380–390. doi: 10.1053/jars.2003.50131. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder’s “suspension bridge”. Arthroscopy. 1993;9(6):611–616. doi: 10.1016/S0749-8063(05)80496-7. [DOI] [PubMed] [Google Scholar]
- 7.Chalmers PN, Frank RM, Gupta AK, et al. All-arthroscopic patch augmentation of a massive rotator cuff tear: surgical technique. Arthrosc Tech. 2013;2(4):e447–51. doi: 10.1016/j.eats.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cole BJ, Rodeo SA, O'Brien SJ, et al. The anatomy and histology of the rotator interval capsule of the shoulder. Clin Orthop Relat Res. 2001;390:129–137. doi: 10.1097/00003086-200109000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Denard PJ, Burkhart SS. Medialization of the subscapularis footprint does not affect functional outcome of arthroscopic repair. Arthroscopy. 2012;28(11):1608–1614. doi: 10.1016/j.arthro.2012.02.030. [DOI] [PubMed] [Google Scholar]
- 10.Drakos MC, Verma NN, Gulotta LV, et al. Arthroscopic transfer of the long head of the biceps tendon: functional outcome and clinical results. Arthroscopy. 2008;24(2):217–223. doi: 10.1016/j.arthro.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 11.Flury MP, John M, Goldhahn J, et al. Rupture of the subscapularis tendon (isolated or in combination with supraspinatus tear): when is a repair indicated? J Shoulder Elb Surg. 2006;15(6):659–664. doi: 10.1016/j.jse.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 12.Foad A, Wijdicks CA. The accuracy of magnetic resonance imaging and magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy. 2012;28(5):636–641. doi: 10.1016/j.arthro.2011.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Galatz LM, Ball CM, Teefey SA, et al. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996;78(7):1015–1023. doi: 10.2106/00004623-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Han Y, Shin JH, Seok CW, et al. Is posterior delamination in arthroscopic rotator cuff repair hidden to the posterior viewing portal? Arthroscopy. 2013;29(11):1740–1747. doi: 10.1016/j.arthro.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 17.Harryman DT 2nd, Sidles JA, Harris SL, et al. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992; 74(1): 53-66. [PubMed]
- 18.Ide J, Tokiyoshi A, Hirose J, et al. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg Am. 2007;89(11):2378–2388. doi: 10.2106/JBJS.G.00082. [DOI] [PubMed] [Google Scholar]
- 19.Itoi E, Berglund LJ, Grabowski JJ, et al. Superior-inferior stability of the shoulder: role of the coracohumeral ligament and the rotator interval capsule. Mayo Clin Proc. 1998;73(6):508–515. doi: 10.4065/73.6.508. [DOI] [PubMed] [Google Scholar]
- 20.Kim DY, Yoo YS, Lee SS, et al. Arthroscopic percutaneous repair of anterosuperior rotator cuff tear including biceps long head: a 2-year follow-up. Clin Orthop Surg. 2012;4(4):284–292. doi: 10.4055/cios.2012.4.4.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kreuz PC, Remiger A, Erggelet C, et al. Isolated and combined tears of the subscapularis tendon. Am J Sports Med. 2005;33(12):1831–1837. doi: 10.1177/0363546505277118. [DOI] [PubMed] [Google Scholar]
- 22.Lafosse L, Jost B, Reiland Y, et al. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89(6):1184–1193. doi: 10.2106/JBJS.F.00007. [DOI] [PubMed] [Google Scholar]
- 23.Levy JC. Simultaneous rotator cuff repair and arthroscopic biceps tenodesis using lateral row anchor. Arthrosc Tech. 2012;1(1):e1–4. doi: 10.1016/j.eats.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lo IK, Burkhart SS. The comma sign: an arthroscopic guide to the torn subscapularis tendon. Arthroscopy. 2003;19(3):334–337. doi: 10.1053/jars.2003.50080. [DOI] [PubMed] [Google Scholar]
- 25.Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004;20(1):22–33. doi: 10.1016/j.arthro.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 26.Lo IK, Burkhart SS. The interval slide in continuity: a method of mobilizing the anterosuperior rotator cuff without disrupting the tear margins. Arthroscopy. 2004;20(4):435–441. doi: 10.1016/j.arthro.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 27.Maschi R, Fives G. Rotator cuff repair: arthroscopic and open. In: Cioppa-Mosca J, Cahill J, Young Tucker C, editors. Postsurgical rehabilitation guidelines for the orthopedic clinician; 2006.
- 28.Mesiha MM, Derwin KA, Sibole SC, et al. The biomechanical relevance of anterior rotator cuff cable tears in a cadaveric shoulder model. J Bone Joint Surg Am. 2013;95(20):1817–1824. doi: 10.2106/JBJS.L.00784. [DOI] [PubMed] [Google Scholar]
- 29.Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elb Surg. 2002;11(6):587–594. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 30.Morag Y, Bedi A, Jamadar DA. The rotator interval and long head biceps tendon: anatomy, function, pathology, and magnetic resonance imaging. Magn Reson Imaging Clin N Am. 2012;20(2):229–59, x. doi: 10.1016/j.mric.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 31.Namdari S, 3rd Henn RF, Green A. Traumatic anterosuperior rotator cuff tears: the outcome of open surgical repair. J Bone Joint Surg Am. 2008;90(9):1906–1913. doi: 10.2106/JBJS.F.01446. [DOI] [PubMed] [Google Scholar]
- 32.Neer CS 2nd. Displaced proximal humeral fractures: part I. Classification and evaluation. 1970. Clin Orthop Relat Res. 2006; 442: 77-82. doi:00003086-200601000-00014. [DOI] [PubMed]
- 33.Nho SJ, Frank RM, Reiff SN, et al. Arthroscopic repair of anterosuperior rotator cuff tears combined with open biceps tenodesis. Arthroscopy. 2010;26(12):1667–1674. doi: 10.1016/j.arthro.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 34.O'Brien SJ, Taylor SA, DiPietro JR, et al. The arthroscopic “subdeltoid approach” to the anterior shoulder. J Shoulder Elb Surg. 2013;22(4):e6–10. doi: 10.1016/j.jse.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 35.Park JY, Jung SW, Jeon SH, et al. Arthroscopic repair of large U-shaped rotator cuff tears without margin convergence versus repair of crescent- or L-shaped tears. Am J Sports Med. 2014;42(1):103–111. doi: 10.1177/0363546513505425. [DOI] [PubMed] [Google Scholar]
- 36.Plancher KD, Johnston JC, Peterson RK, et al. The dimensions of the rotator interval. J Shoulder Elb Surg. 2005;14(6):620–625. doi: 10.1016/j.jse.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 37.Resnick B, Parker R. Simplified scoring and psychometrics of the revised 12-item Short-Form Health Survey. Outcomes Manag Nurs Pract. 2001;5(4):161–166. [PubMed] [Google Scholar]
- 38.Richards DP, Burkhart SS, Tehrany AM, et al. The subscapularis footprint: an anatomic description of its insertion site. Arthroscopy. 2007;23(3):251–254. doi: 10.1016/j.arthro.2006.11.023. [DOI] [PubMed] [Google Scholar]
- 39.Schnaser E, Toussaint B, Gillespie R, et al. Arthroscopic treatment of anterosuperior rotator cuff tears. Orthopedics. 2013;36(11):e1394–400. doi: 10.3928/01477447-20131021-20. [DOI] [PubMed] [Google Scholar]
- 40.Toussaint B, Audebert S, Barth J, et al. Arthroscopic repair of subscapularis tears: preliminary data from a prospective multicentre study. Orthop Traumatol Surg Res. 2012;98(8 Suppl):S193–200. doi: 10.1016/j.otsr.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 41.Walch G, Nove-Josserand L, Levigne C, et al. Tears of the supraspinatus tendon associated with “hidden” lesions of the rotator interval. J Shoulder Elb Surg. 1994;3(6):353–360. doi: 10.1016/S1058-2746(09)80020-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1225 kb)