Abstract
Adolescents have special sexual and reproductive health needs (whether or not they are sexually active or married). This review assesses the impact of interventions to improve adolescent sexual and reproductive health (including the interventions to prevent female genital mutilation/cutting [FGM/C]) and to prevent intimate violence. Our review findings suggest that sexual and reproductive health education, counseling, and contraceptive provision are effective in increasing sexual knowledge, contraceptive use, and decreasing adolescent pregnancy. Among interventions to prevent FGM/C, community mobilization and female empowerment strategies have the potential to raise awareness of the adverse health consequences of FGM/C and reduce its prevalence; however, there is a need to conduct methodologically rigorous intervention evaluations. There was limited and inconclusive evidence for the effectiveness of interventions to prevent intimate partner violence. Further studies with rigorous designs, longer term follow-up, and standardized and validated measurement instruments are required to maximize comparability of results. Future efforts should be directed toward scaling-up evidence-based interventions to improve adolescent sexual and reproductive health in low- and middle-income countries, sustain the impacts over time, and ensure equitable outcomes.
Keywords: Adolescent sexual health, Reproductive health, Genital mutilation, Sexual health education, Teenage pregnancy, Contraception
A significant number of adolescents around the globe are sexually active, and this proportion increases steadily from mid- to late adolescence [1]. Sexual activity of adolescents varies markedly by gender and region; more girls compared with boys are sexually active in sub-Saharan Africa, Asia, and central Asia while in Latin America and Caribbean, more boys are sexually active than girls [1]. About 3 in 10 unmarried adolescent women in sub-Saharan Africa and nearly one in four in South America have ever had sex [2]. Early sexual debut increases the risk of sexually transmitted infections (STIs), including HIV, and can result in unintended pregnancy and early childbearing. Adolescents have limited and, in some places, no access to sexual and reproductive health education and contraception, making adolescent girls more prone to early and unintended pregnancies [3].
Nearly a quarter of girls aged 15–19 years are married with an estimated 16 million adolescents giving birth each year globally, of whom, 95% are from low- and middle-income countries (LMICs) [4]. Almost half of the women aged 20–24 years in Asia and Africa are married by age 18 years, putting them at a higher risk for early pregnancy, repeated pregnancies, maternal disability, and death [3], [5]. Adolescent birth rate in LMICs is more than double that of high-income countries (HICs) and often within a formal marital relationship, especially in Asia, Middle East, and North African regions [6]. Although rates of births among adolescent girls have declined in all regions since 1990, they are still high in Africa, Asia, Latin America, and Caribbean. Among females aged 15–19 years, pregnancy-related death is the second leading cause of death after self-harm [7]. Younger mothers are at an increased risk of obstetric fistula, anemia, eclampsia, postpartum hemorrhage, and puerperal endometritis [7], [8], [9]. Girls younger than 19 years have a 50% increased risk of stillbirths and neonatal deaths, as well as an increased risk for preterm birth, low birth weight, and asphyxia [8]. In addition to affecting the health of the mother, early marriage and/or childbearing also often prevent girls from attending school and perpetuate the cycle of poverty [9], [10], [11]. In LMICs, adolescent pregnancy is a severe impediment to development and can lead to a number of challenges including abandonment by their partners, school dropout, and lost productivity, which ultimately limits their future social and economic opportunities leading to intergenerational transmission of poverty [12], [13].
Female genital mutilation/cutting (FGM/C) is a hazardous traditional practice on prepubescent girls that involves partial or total removal of the external female genitalia or other injury to the female genital organs for nonmedical reasons [14]. It is practiced in about 28 countries of Africa, and recent figures suggest a prevalence of more than 70% in Burkina Faso, Djibouti, Egypt, Eritrea, Ethiopia, Guinea, Mali, Mauritania, Northern Sudan, Sierra Leone, and Somalia [15], [16]. It is also practiced by immigrant communities in a number of other countries, including Australia, Canada, France, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the U.S. [17]. However, there is considerable variation in prevalence between and within countries, reflecting ethnicity and tradition. Girls exposed to FGM/C are at risk of immediate physical consequences, such as severe pain, bleeding, shock, difficulty in passing urine and feces, and infections. Long-term consequences can include chronic pain, sexual/orgasmic dysfunction, infections, and mental trauma [18], [19].
In 2011, the World Health Organization (WHO) issued guidelines on preventing early pregnancy and poor reproductive outcomes in adolescents from LMICs focusing on four major pregnancy prevention outcomes: (1) increasing access to and use of contraception; (2) preventing marriage before 18 years; (3) increasing knowledge and understanding of the importance of early pregnancy prevention; and (4) preventing coerced sex [20].
Adolescents have special sexual and reproductive health needs that remain unmet, mainly due to lack of knowledge, social stigma, laws and policies preventing provision of contraception and abortion to unmarried (or any) adolescents, and judgmental attitudes among service providers [21]. To maintain sexual and reproductive health, adolescents need access to accurate information and to the safe, effective, affordable, and acceptable contraception method of their choice. They must be informed and empowered to protect themselves from STIs. All sexually active adolescents, regardless of marital status, deserve to have their contraceptive needs acknowledged and responded to. This article is part of a series of reviews conducted to evaluate the effectiveness of potential interventions for adolescent health and well-being. A detailed framework, methodology, and other potential interventions have been discussed in separate articles [22], [23], [24], [25], [26], [27], [28]. This article aims to assess the impact of interventions to improve sexual and reproductive health, prevent adolescent pregnancy; FGM/C; and intimate partner violence.
Methods
We systematically reviewed all published literature up to December 2014 on interventions to improve sexual health in adolescent population focusing on sex education, preventing unintended adolescent pregnancy, intimate partner violence, and FGM/C. We took a systematic approach to consolidate the existing evidence through the following three methodologies in order to include all the recent evidence:
-
1.
Overview of systematic reviews: We conducted an overview of systematic reviews for interventions where recent systematic reviews existed;
-
2.
Updating existing reviews: We updated the existing systematic reviews if the existing review only included evidence prior to 2011; and
-
3.
De novo review: For interventions where no reviews existed, we conducted a de novo review.
For the purpose of this review, the adolescent population was defined as aged 11–19 years; however, since many studies targeted youth (aged 15–24 years) along with adolescents, exceptions were made to include studies targeting adolescents and youth. Studies were excluded if they targeted age groups other than adolescents and youth or did not report segregated data for the age group of interest. The search was conducted till December 2014, and we did not apply any limitations on the start search date or geographical settings and have attempted to carry out subgroup analysis for various interventions and settings, where data permitted.
Methodology for de novo review
For de novo reviews, our priority was to select existing randomized, quasi-randomized, and before/after studies, in which the intervention was directed toward adolescents and related to sexual and reproductive health outcomes. A separate search strategy was developed for each aspect using appropriate keywords, medical subject heading, and free text terms. The following principal sources of electronic reference libraries were searched to access the available data: The Cochrane Library, Medline, PubMed, Popline, LILACS, CINAHL, EMBASE, World Bank's JOLIS search engine, CAB Abstracts, British Library for Development Studies BLDS at Institute of Development Studies, the WHO regional databases, Google, and Google Scholar. The titles and abstracts of all studies identified were screened independently by two reviewers for relevance and matched. Any disagreements on selection of studies between these two primary abstractors were resolved by the third reviewer. After retrieval of the full texts of all the studies that met the inclusion/exclusion criteria, data from each review or study were abstracted independently and in duplicate into a standardized form. Quality assessment of the included randomized controlled trials (RCTs) was done according to the Cochrane risk of bias assessment tool. We conducted a meta-analysis for individual studies using the software Review Manager, version 5.3 (Cochrane Collaboration, London, United Kingdom). Pooled statistics were reported as the relative risk (RR) for categorical variables and standard mean difference (SMD) for continuous variables between the experimental and control groups with 95% confidence intervals (CIs). A grade of “high,” “moderate,” “low,” and “very low” was used for grading the overall evidence indicating the strength of an effect on specific health outcome according to the Grading of Recommendations Assessment, Development and Evaluation criteria [29].
Methodology for existing systematic review
We considered all available published systematic reviews on the interventions to improve adolescent sexual health. Our priority was to select existing Cochrane and non-Cochrane systematic reviews of randomized or non-RCTs, which fully or partly addressed the interventions. A broad search strategy was used that included a combination of appropriate keywords, medical subject heading, and free text terms, and search was conducted in The Cochrane Library, Medline, and PubMed. The abstracts (and the full sources where abstracts are not available) were screened by two abstractors to identify systematic reviews adhering to our objectives. Any disagreements on selection of reviews between these two primary abstractors were resolved by the third reviewer. After retrieval of the full texts of all the reviews that met the inclusion/exclusion criteria, data from each review were abstracted independently and in duplicate into a standardized form. Information was extracted on (1) the characteristics of included studies; (2) description of methods, participants, interventions, and outcomes; (3) measurement of treatment effects; (4) methodological issues; and (5) risk of bias tool. We extracted pooled effect size for the outcomes of interest with 95% CIs. We assessed and reported the quality of included reviews using the 11-point assessment of the methodological quality of systematic reviews (AMSTAR) criteria [30].
Methodology for updated review
We updated the existing systematic reviews only if the most recent review on a specific intervention was conducted before December 2011. For updating the existing reviews, we adopted the same methodology and search strategy mentioned in the existing review to update the search and find all the relevant studies after the last search date of the existing review. After retrieval of the full texts of all the articles that met the inclusion/exclusion criteria, data from each study were abstracted independently and in duplicate into a standardized form. Information was extracted on study design, geographical setting, intervention type and description, mode of delivery, and outcomes assessed. We then updated the estimates of reported outcomes by pooling the evidence from the new studies identified in the updated search and reported new effect size for the outcomes of interest with 95% CIs. We then assessed and reported the quality of included reviews using the 11-point AMSTAR criteria [30].
Results
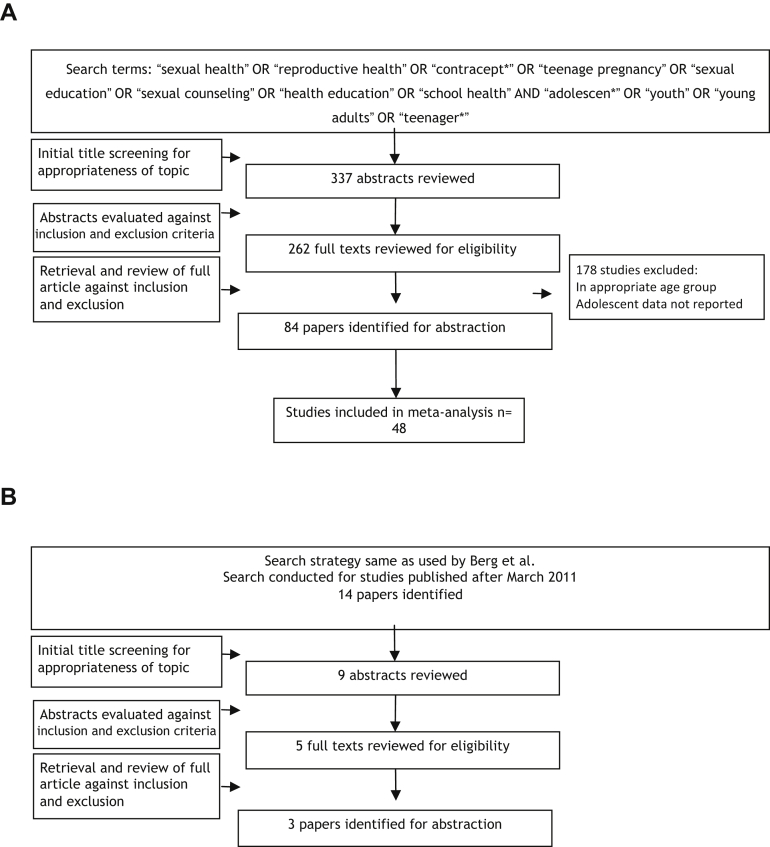
We found existing systematic reviews on interventions for improving adolescent sexual and reproductive health; however, they were limited in their scope to a particular strategy such as school-based interventions [31], [32], peer-led interventions [33], mass media [34], [35], and youth centers [36]; geographic settings [37], [38]; or limited to trial data only [13], [39]. Hence, we conducted a de novo review for the effectiveness of sexual and reproductive health education and contraceptive availability. We found a recent existing Cochrane review by Fellmeth et al. [40] on interventions to prevent intimate partner violence and reported the relevant findings. For interventions to prevent FGM/C, we updated the review by Berg and Denison [14] and also broadened its scope to include studies outside of Africa. Figure 1 depicts the search flow diagrams while Table 1 describes in detail the characteristics of the included studies for the de novo review.
Figure 1.
(A) Search flow for interventions to improve sexual and reproductive health and prevent adolescent pregnancy (de novo review). (B) Search flow for interventions to prevent FGM/C (update).
Table 1.
Characteristics of included studies for sexual health education
| Author, year | Design | Country | Setting | Intervention | Target population | Outcomes |
|---|---|---|---|---|---|---|
| Aarons et al., 2000 [41] | RCT | U.S.A. | School based | Reproductive health classes, the Postponing Sexual Involvement curriculum, health risk screening, and “booster” educational activities during the following (eighth grade) school year. | Eighth-grade students | Use of contraception |
| Agha and Van Rossem, 2004 [42] | Quasi | Zambia | Community based | Peer-led education projects focusing on promoting abstinence and condom use among male and female school children. Peer educators consisted of people aged 18–22 years who were trained by a professional peer education trainer to convey their messages through a mixture of techniques. | Males and females aged 14–23 years | Abstinence, multiple sexual partners, condom use |
| Baptiste et al., 2006 [43] | RCT | South Africa and Trinidad and Tobago | Community based | Community participatory research framework to adapt and deliver family-based prevention. | Youth | Communication, HIV knowledge and prevalence |
| Barnet et al., 2007 [44] | RCT | U.S.A. | Home based | Home visiting or routine care. They delivered a parenting curriculum, encouraged contraceptive use, connected the teen with primary care, and promoted school continuation. | Pregnant females aged 12–18 years | Birth control after index child, repeat pregnancy |
| Berenson and Rahman, 2012 [45] | RCT | U.S.A. | Clinic | Face-to-face behavioral counseling and education at their baseline clinic visit or this same intervention followed by monthly phone calls for 6 months or standard care. | Females aged 16–24 years | Consistent contraceptive use, hormonal contraceptive use, condom use, dual usage, no contraception |
| Morrison-Beedy et al., 2012 [94] | RCT | U.S.A. | Community based | Peer education groups. Theory-based sexual risk reduction intervention or a structurally equivalent health promotion control group. | Females aged 15–19 years | Multiple sexual partners, intercourse |
| Black et al., 2006 [46] | RCT | U.S.A. | Home based | Home visiting or routine care. Home-based intervention curriculum was based on social cognitive theory and focused on interpersonal negotiation skills, adolescent development, and parenting. | Postpartum females 13.5–17.9 years | Repeat pregnancy |
| Blake et al., 2003 [47] | Quasi | U.S.A. | School based | Condom availability in high school | High-school adolescents | Condom use |
| Bonell et al., 2013 [48] | RCT | England | Community based | “Teens and toddlers” intervention: 18–20 weekly sessions in preschool nurseries | Teens | Contraception use |
| Brieger et al., 2001 [49] | Quasi | West Africa: Nigeria and Gambia | Community based | Peer education groups. Peer educators provided information and counseling through one-on-one sessions, group talks and presentations, and distribution of print materials. | Male and female adolescents | Knowledge |
| Bull et al., 2012 [50] | RCT | U.S.A. | Community social media | Exposure to Just/Us, a Facebook page developed with youth input, or to control content on 18–24 News, a Facebook page with current events for 2 months. | Youth | Condom use |
| Chen et al., 2010 [51] | RCT | U.S.A. | Community and school based | “Focus on Youth in the Caribbean” (FOYC) is based on the Protection Motivation Theory (PMT), consists of 10 primary sessions (delivered weekly after a baseline survey) and two annual boosters (delivered after 12 and 24 months postintervention assessment). The sessions are designed to augment decision-making skills, including the development of a lifelong perspective in decision-making, communication and listening skills, and protective knowledge and skills regarding safer sexual behavior. GFI and CImPACT are parenting interventions. GFI includes a 20-minute video filmed in the USA, which addresses decision-making regarding future planning for the parent and child; the video is followed by a structured discussion among the participants. CImPACT includes a 20-minute video filmed in the Bahamas addressing parent–child communication about sexual decision-making, followed by role-playing and a condom demonstration. | Males and females aged 10–12 years | Knowledge, condom use |
| Clark et al., 2005 [52] | RCT | U.S.A. | School based | The AIM is a 10-session curriculum based on the theory of possible selves. Class exercises encourage students to articulate a possible future self-identity and to develop self-promotion skills. | Seventh-grade African-Americans | Abstinence, sex initiation |
| Cornelius et al., 2013 [53] | Pre–post | U.S.A. | Community social media | Becoming a Responsible Teen (BART) is a community-based HIV prevention curriculum, which consists of interactive group discussions and role plays that allow participants to practice behavioral skills for safer sex. BART was followed by the delivery of daily multimedia messages for 3 months | African-American adolescents | Knowledge, condom use, HIV prevention scores |
| Coyle et al., 2001 [54] | RCT | U.S.A. | School based | Safer Choices, a theory-based, multicomponent educational program designed to reduce sexual risk behaviors and increase protective behaviors in preventing HIV, other STDs, and pregnancy among high-school students. | Ninth-grade students | Condom use |
| Coyle et al., 2004 [56] | RCT | U.S.A. | School based | Draw the Line/Respect the Line, a theoretically based curriculum designed to reduce sexual risk behaviors among middle-school adolescents. | Sixth graders | Sex initiation, knowledge |
| Coyle et al., 2013 [55] | RCT | U.S.A. | School based | (1) HIV/STI/pregnancy prevention curriculum only; (2) service learning only; (3) HIV/STI/pregnancy prevention curriculum plus service learning; or (4) an attention control curriculum | High-school adolescents | Mean sexual intercourse, mean use of condom |
| Daniel 2008 [124] | Quasi | India | Community based | Orientation and training of reproductive health teams of community leaders and influential residents, and through group meetings with young couples' parents and in-laws; messages were disseminated through street theater performances and wall paintings, and formal and informal rural health service providers were trained on reproductive health issues and contraception. | Young couples aged <25 years | Contraceptive use, knowledge and attitude |
| Danielson et al., 1990 [57] | RCT | U.S.A. | Clinic | A reproductive health intervention combining a highly explicit half-hour slide-tape program with a personal health consultation was provided. | Males aged 15–18 years | Consistent contraceptive use, hormonal contraceptive use, condom use, dual usage, no contraception |
| DiClemente et al., 2004 [58] | RCT | U.S.A. | Community based | Peer education groups. All participants received four 4-hour group sessions. The intervention emphasized ethnic and gender pride, HIV knowledge, communication, condom use skills, and healthy relationships. The comparison condition emphasized exercise and nutrition. | Females aged 14–18 years | Condom use |
| DiClemente et al., 2009 [59] | RCT | U.S.A. | Clinic | Intervention participants received two 4-hour group sessions and four telephone contacts over a 12-month period, targeting personal, relational, sociocultural, and structural factors associated with adolescents' STD/HIV risk and were given vouchers facilitating male partners' STD testing/treatment. | Females aged 15–21 year | Condom use |
| Dilorio et al., 2007 [60] | RCT | U.S.A. | Community based | HIV education, communication skills, take-home activities for fathers and adolescents. | Males aged 11–14 years | Condom use |
| Downs et al., 2004 [61] | RCT | U.S.A. | Community based | Video-based sessions versus book-based information | Urban adolescent girls | Abstinence, condom use, STI |
| Elliott et al., 2012 [62] | Quasi | Scotland | School based | Healthy Respect 2 (HR2) combined sex education with youth-friendly sexual health services, media campaigns and branding, and encouraged joint working between health services, local government and the voluntary sector. | 15- to 16-year-old adolescents | Knowledge, condom acceptability, having sex, condom use |
| Erulkar et al., 2004 [121] | Quasi | Kenya | Community based | The Nyeri Youth Health Project, a community-based project for young people. Adult counselors worked in their own communities to educate both adolescents and parents on reproductive health and to encourage dialogue between them. The counselors were trained for 1 month and used a life skills curriculum entitled “Life Planning Skills for Adolescents in Kenya,” which includes sessions on community, family and individual values, adolescent development, sexuality, gender roles, relationships, pregnancy, STIs, HIV/AIDS, harmful traditional practices, substance abuse, planning for the future, children's rights, and advocacy. | 10–24 years of age | Sexual initiation, secondary abstinence, condom use, sex partners, communication with parents |
| Ferguson, 1998 [63] | RCT | U.S.A. | Community based | Peer education groups. Peer counseling in a culturally specific adolescent pregnancy prevention program. | Females aged 12–16 years | Condom use |
| Forehand et al., 2007 [64] | RCT | U.S.A. | Community | Enhanced communication intervention (five sessions), single-session communication intervention(one session) | African-American parent–preadolescent dyads (child, aged 9–12 years) | Mean change in knowledge |
| Garcia et al., 2012 [65] | RCT | Peru | Community based | The intervention comprised four modalities: strengthened STI syndromic management by pharmacy workers and clinicians; mobile-team outreach for STI screening and pathogen-specific treatment; periodic presumptive treatment of FSWs for trichomoniasis; and condom promotion. | Urban young men (aged 18–29 years) and female sex workers | Sexual intercourse, STI prevalence |
| Gold et al., 2004 [66] | RCT | U.S.A. | Clinic based | The intervention group received information about EC and was told how to access EC and in addition received one complete course of EC for future use. Participants in the AEC group were informed that they could obtain up to two additional courses of advance EC during the 6 months of the study and were told that they could obtain these subsequent courses from the study office whenever they requested them. Participants in the control group received written and verbal information about EC and were told how to access EC on request from the adolescent clinic. | Urban adolescent females aged 15–20 years | EC use |
| Hall et al., 2012 [67] | RCT | U.S.A. | Community text messaging | The intervention group received 180 daily text messages, including 47 individual messages (which were repeated up to four times over the study). | Young women aged 13–25 years | OC knowledge |
| Harper et al., 2009 [68] | Quasi | U.S.A. | Community based | Peer education groups. Nine-session SHERO's (a female-gendered version of the word hero) intervention or a single-session information-only HIV prevention intervention. | Females aged 12–21 years | Intercourse, knowledge |
| Herceg-Baron et al., 1986 [69] | Quasi | U.S.A. | Clinic | Increase family + teenager or teenager + clinic staff contact | Adolescent aged 12–17 years | Contraceptive use, unintended pregnancy |
| Howard and McCabe, 1990 [70] | Quasi | U.S.A. | Community based | Peer education. The program is led by older teenagers and focuses on helping students resist peer and social pressures to initiate sexual activity. | Males and females aged 14–16 years | Intercourse |
| Hughes et al., 1995 [71] | RCT | U.S.A. | Clinic | Increase in family planning clinic for education counseling and access compared with no clinic. | Females aged 14–18 years | Unintended pregnancy, intercourse |
| Jemmott III et al., 1998 [72] | RCT | U.S.A. | School based | HIV and abstinence education: intervention involved eight 1-hour modules implemented by adult facilitators or peer cofacilitators. Abstinence education enforced delaying sexual intercourse or reducing its frequency; safer sex intervention stressed condom use; control intervention concerned health issues unrelated to sexual behaviors. | African-American adolescents | Having sex, condom use, knowledge, self-efficacy |
| Jemmott et al., 2005 [73] | RCT | U.S.A. | Clinic | Counseling, skills building, and case management services | Females aged 12–19 years | Knowledge, number of sex partners, unprotected intercourse |
| Jemmott et al., 2010 [74] | RCT | South Africa | School based | Two 6-session interventions based on behavior-change theories and qualitative research. The HIV/STD risk-reduction intervention targeted sexual risk behaviors; the attention-matched health promotion control intervention targeted health issues unrelated to sexual behavior. | Sixth-grade students | Having sex, multiple sex partners, condom use |
| Mason-Jones et al., 2011 [89] | Quasi | U.S.A. | Community based | Peer-led education sessions. Peer educators were recruited and trained to provide information and support to their fellow students. | Males and females aged 15–16 years | Abstinence, condom use |
| Key et al., 2008 [75] | Quasi | U.S.A. | School based | School-based social work services coordinated with comprehensive health care. | Teen mothers | Contraception, pregnancy |
| Kiene and Barta, 2006 [76] | RCT | U.S.A. | Community computer based | Custom computerized intervention. Content and delivery were based on the Information–Motivation–Behavioral Skills model of health behavior change and used Motivational Interviewing techniques. | College students | Knowledge, condom availability and use, sexual risk behavior |
| Kim et al., 2001 [123] | Quasi | Zimbabwe | Community-based mass media | Multimedia campaign promoted sexual responsibility among young people in Zimbabwe, while strengthening their access to reproductive health services by training providers. | 10–24 years of age | Contraceptive knowledge, contraceptive use |
| Kinsler et al., 2004 [77] | Quasi | U.S.A. | School based | HIV prevention education: Project Light uses a cognitive-behavioral approach to motivate the program participants to change their risk behaviors and adopt safer behaviors. | Primary and secondary school students | Knowledge, efficacy, communication |
| Kirby et al., 2004 [79] | RCT | U.S.A. | School based | Safer Choices was designed to reduce unprotected sex by delaying initiation of sex, reducing its frequency, or increasing condom use. Its five components included: school organization, an intensive curriculum with staff development, peer resources and school environment, parent education, and school-community linkages. | Ninth-grade adolescents | Sexual risk-taking |
| Kirby et al., 2010 [78] | RCT | U.S.A. | Clinic- and telephone-based follow-ups | Regular clinic services or regular clinic services plus nine follow-up phone calls over 12 months to improve sexual risk behaviors. | Females aged 14–18 years | Use of contraception |
| Kisker et al., 1996 [80] | Quasi | U.S.A. | School based | School-Based Adolescent Health Care Program, which provided comprehensive health-related services. | Youth | Health care access, knowledge, sexual risk behaviors |
| Klepp et al., 1997 [81] | RCT | Tanzania | School based | Sexual and HIV risk reduction and awareness | Sixth graders | Knowledge, sexual initiation |
| Kogan et al., 2012 [82] | RCT | U.S.A. | Community based | The Strong African American Families–Teen (SAAF–T) program, a family-centered preventive intervention that included an optional condom skills unit. | 16-year-old African-American and their caregivers | Unprotected intercourse and condom use efficacy |
| Koo et al., 2011 [83] | RCT | U.S.A. | School based | 10–13 classroom sessions related to delaying sexual initiation | Fifth-grade students | Knowledge, communication, having sex, abstinence |
| Larkey et al., 2010 [84] | RCT | Tanzania | Community and school based | Provision of youth-friendly health services, as part of a package of interventions including reproductive health education in primary school; the provision of youth-friendly sexual and reproductive health services; community-based condom promotion and distribution; and community-wide activities. | Adolescents 15 years onward and community people | Prevalence of STI, clinic visit and condom distribution |
| Lewis et al., 2010 [85] | Quasi | Australia | Clinic | Contraceptive education and use of Implanon or depot medroxyprogesterone acetate (DMPA) or nothing | Postpartum females (12–18 years old) | Unintended pregnancy |
| Lim et al., 2012 [86] | Quasi | Australia, New Zealand | Community text messaging | The 12-month intervention included SMS (catchy sexually transmissible infections prevention slogans) and e-mails. | Youth aged 16–29 years | Having sex, condom use, STI test |
| Lou et al., 2004 [122] | Quasi | China | Community based | The intervention intended to build awareness and offer counseling and services related to sexuality and reproduction among unmarried youths, in addition to the routine program activities, which were exclusively provided in the control site. | 15–24 years of age | Contraceptive use, condom use |
| Marcell et al., 2013 [87] | Quasi | U.S.A. | Community based | Peer education. Participants received three 1-hour curriculum sessions on consecutive days. | Males aged 16–24 years | Multiple sexual partners, intercourse, condom use, knowledge |
| Markham et al., 2012 [88] | RCT | U.S.A. | School based | Group and individualized computer-based activities addressing psychosocial variables. The risk avoidance (RA) program met federal abstinence education guidelines; the risk reduction (RR) program emphasized abstinence and included computer-based condom skills training. | African-American and Hispanic seventh- to ninth-grade students | Having sex, unprotected sex, sexual initiation, number of sex partners |
| McBride et al., 2007 [90] | Quasi | U.S.A. | Community based | The Collaborative HIV/AIDS Adolescent Mental Health Project (CHAMP): the program involves having youth participate with parents and/or other adult caregivers who can steer them through pubertal changes, increases in romantic thoughts and feelings, and social pressure to engage in risky behavior, which may involve sexual activity. | Males and females aged 9–11 years | Parent–adolescent communication |
| Meekers, 2000 [91] | Quasi | South Africa | Community based | Targeted social marketing program on reproductive health beliefs and behavior | Young females | Knowledge and awareness |
| Meekers et al., 2005 [92] | Pre–post | Cameroon | Community based | “100% Jeune” social marketing campaign | Youth 15–24 years old | Perceived condom attributes and access, self-efficacy, and perceived social support |
| Merakou and Kourea-Kremastinou, 2006 [93] | Quasi | U.S.A. | School based | Peer education. Recruitment and training of the peer educators, implementation of HIV prevention activities in schools on behalf of the peer educators and evaluation. | 13- to 17-year-old adolescents | Sexual encounter, condom use |
| Munodawafa et al., 1995 [95] | Quasi | Zimbabwe | School based | Student nurses to provide health instruction among rural school-age populations. | School-based adolescents | Knowledge |
| O-Donnell et al., 2005 [96] | RCT | U.S.A. | Community based | “Saving sex for later”—a parent and youth education program | Females and males aged 10–11 years | Communication |
| Ozcebe et al., 2004 [97] | Pre–post | Turkey | Community based | Peer education groups. An education program was scheduled every week and included the following discussion subjects: male and female anatomy–physiology of the reproductive system; types of STIs; etiopathology, progress and treatment of HIV/AIDS; preventive precautions against sexually transmitted diseases and HIV/AIDS; family planning methods; and communication skills. | Male and female adolescents | Knowledge |
| Pearlman et al., 2002 [98] | Quasi | U.S.A. | Community based | Peer education program. Short course and ongoing group work to plan HIV/AIDS outreach activities supervised by an adult. | Youth | Knowledge, perception, risk raking behaviors |
| Peltzer et al., 2011 [99] | RCT | U.S.A. | Clinic | Counseling, skills building: 18-minute information–education segment used a tabletop flip chart and visual materials to illustrate key concepts and interactive activities to dispute HIV myths, stigmas, and misinformation. The information component focused on HIV destigmatization as well as providing accurate risk information including risks related to male circumcision. | Males aged 18–35 years | Knowledge, number of sex partner, unprotected intercourse |
| Petersen et al., 2007 [100] | RCT | U.S.A. | PHC | Contraceptive counseling with optional advance EC prescription | Women aged 16–44 years | EC acceptance (only for 16- to 25-year age group) |
| Pinkleton et al., 2008 [101] | Quasi | U.S.A. | Community and school | Teen-led, media literacy curriculum focused on sexual portrayals in the media. | Primary- to middle-school students | Knowledge, efficacy, abstinence |
| Prado et al., 2012 [102] | RCT | U.S.A. | Community based | Family-specific interventions designed to reduce HIV risk behaviors | Hispanic males and females aged 12–17 years | Parent–adolescent communication, intercourse |
| Raymond et al., 2006 [103] | RCT | U.S.A. | Clinic based | Two methods of access to emergency contraceptive pills: increased access (two packages of pills dispensed in advance with unlimited resupply at no charge) or standard access (pills dispensed when needed at usual charges) | Females aged 14–24 years | Pregnancy, having sex, use of contraception, STI |
| Rickert et al., 2006 [104] | RCT | U.S.A. | Clinic | Contraceptive education and Depo Now compared to initiating with a bridge method (pills, transdermal patch, or vaginal ring) | Female aged 14–26 years | Consistent contraceptive use, hormonal contraceptive use, condom use, dual usage, no contraception, unintended pregnancy |
| Rocca et al., 2007 [105] | RCT | U.S.A. | Clinic based | Access to EC through advance provision, pharmacies, or clinics | Females aged 15–24 years | EC use |
| Rosenbaum, 2009 [106] | Quasi | U.S.A. | Community based | Virginity pledgers | >15 years of age virginity pledgers | Premarital sex, sexually transmitted diseases, and anal and oral sex variables |
| Ross et al., 2007 [107] | RCT | Tanzania | Community based | Community activities; teacher-led, peer-assisted sexual health education in Years 5–7 of primary school; training and supervision of health workers to provide “youth-friendly” sexual health services; and peer condom social marketing. | Adolescents | Knowledge, attitude, HIV, HSV |
| Rotheram-borus et al., 1998 [108] | RCT | U.S.A. | Community based | (1) Seven sessions of 1.5 hours each (10.5 hours); (2) three sessions of 3.5 hours each (10.5 hours); or (3) a no-intervention condition. | Adolescent aged 13–24 years | Self-efficacy, condom use. |
| Schreiber et al., 2010 [109] | RCT | U.S.A. | Clinic based | Routine postpartum contraceptive care and advanced supply of one pack of EC pills with unlimited supply thereafter upon request. | Postpartum teenage females | Sexual encounter, any contraception, condom use, EC use, pregnancy |
| Shrier et al., 2001 [110] | RCT | U.S.A. | Clinic based | Counseling and education. Standard STD education or to watch a videotape and have an individualized intervention session. | Female adolescents diagnosed with STI | Condom use, knowledge |
| Sieving et al., 2012 [111] | RCT | U.S.A. | Clinic | Counseling, skills building, and case management services. | Females aged 13–17 years | Number of sex partner |
| Suffoletto et al., 2013 [112] | RCT | U.S.A. | Community text messaging | Intervention participants received a sequence of text messages that assessed risky encounters over the past week, were provided personalized feedback on risk behavior, and were prompted collaborative goal setting to not have a risky encounter for the coming week. | Females aged 18–25 years | Condom use |
| Tocce et al., 2012 [113] | Quasi | U.S.A. | Clinic | Contraceptive education and etonogestrel implant (IPI) | Females aged 13–23 years | Consistent contraceptive use, hormonal contraceptive use, condom use, no contraception, unintended pregnancy |
| Villarruel et al., 2006 [115] | RCT | U.S.A. | School based | The HIV and health-promotion control interventions consisted of six 50-minute modules delivered by adult facilitators to small, mixed-gender groups in English or Spanish. | Latino adolescents aged 13–18 years | Self-reported sexual behavior |
| Villarruel et al., 2008 [114] | RCT | Mexico | Community | Parent education for adolescent sexual risk reduction | Parents of adolescents | Communication |
| Walker et al., 2004 [116] | RCT | Mexico | School based | An HIV prevention course that promoted condom use, the same course with emergency contraception as backup, or the existing sex education course. | High-school students | Knowledge, condom use |
| Weed et al., 2008 [117] | Quasi | U.S.A. | School based | Abstinence education program; the core of the program was a nine-unit abstinence curriculum taught consecutively over 20 class periods, called Reasonable Reasons to Wait: Keys to Character. | Seventh-grade adolescents | Sexual initiation |
| Wiggins et al., 2009 [118] | Quasi | England | Community based | Intensive, multicomponent youth development program including sex and drugs education (Young People's Development Program) versus standard youth provision. | 13- to 15-year-old adolescents | Pregnancy, weekly cannabis use, and monthly drunkenness |
| Winter and Breckenmaker, 1990 [119] | Quasi | U.S.A. | Clinic | In-depth counseling and education in an adolescent friendly environment | Teenagers | Contraceptive use, pregnancy |
| Zimmer-Gembeck, 2001 [120] | Pre–post | U.S.A. | School based | Family planning care visits and contraceptive availability | Female adolescents | Use of contraception |
AEC = advance emergency contraceptive; AIM = Adult Identity Mentoring; CImpact = Caribbean Informed Parents and Children Together; EC = emergency contraceptive; FSW = female sex workers; GFI = goal for information technology; HSV = herpes simplex virus; IPI = immediate postpartum transplant; OC = oral contraceptive; PHC = primary health care; RCT = randomized controlled trial; SMS = short messaging service; STD = sexually transmitted disease; STI = sexually transmitted infection.
Sexual and reproductive health interventions to prevent adolescent pregnancy
Studies were included if any form of sexual and reproductive health education, counseling, and access to contraception was delivered to adolescents compared to no intervention or general health education. We identified 1,123 titles from the search conducted in all databases. After screening the titles and abstracts, 84 studies were identified that met the inclusion criteria [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83] [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109] [110], [111], [112], [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124]; 51 studies were RCTs while 29 were quasi-experimental design and four were pre–post studies. Fifty four of 84 studies focused on adolescent age group alone (11–19 years) while the rest had overlapping age groups. Meta-analysis could be conducted for 48 studies as other studies did not report data that could be pooled. Most of these studies were conducted in HICs in North America and Europe except 10 studies that were conducted in LMICs including Zambia, Zimbabwe, Cameroon, Tanzania, Gambia, Kenya, China, and Peru. Interventions mainly included (1) education and counseling through peer groups, parent education, community members, telephone calls, Web-based content, and home visitation; (2) youth-friendly health services; (3) improving access to contraceptives through pharmacy, clinic, and advance provision of contraceptives; (4) condom distribution; (5) abstinence-focused education; (6) emergency contraceptive promotion; (7) skills development; and (8) multicomponent interventions.
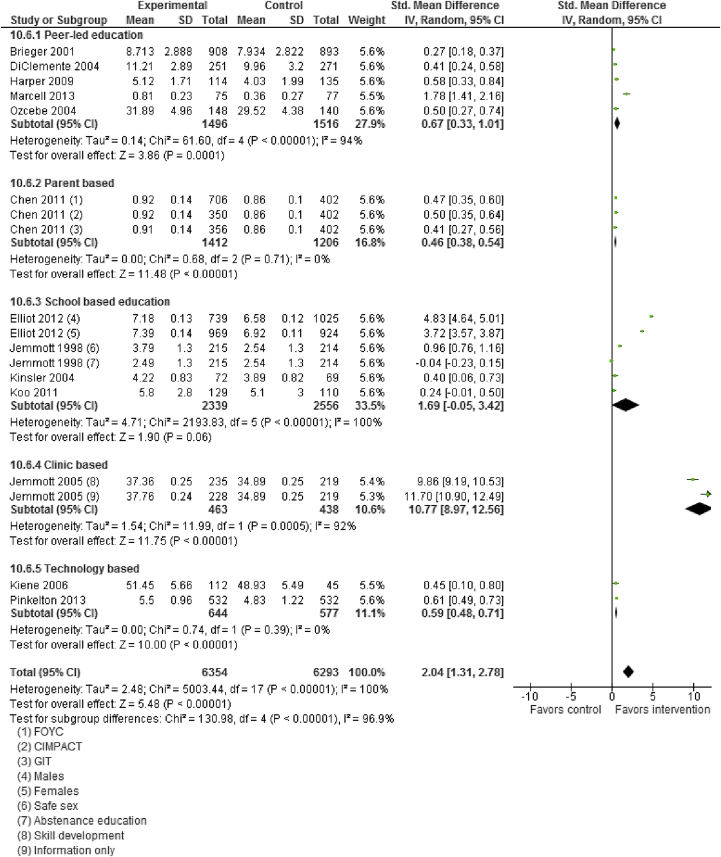
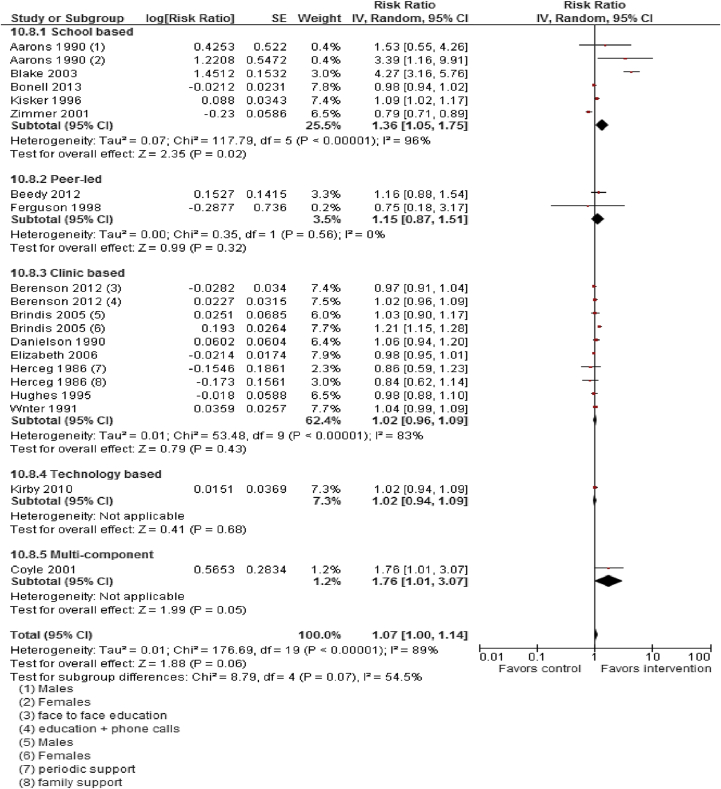
Moderate quality data suggest that sexual and reproductive health education, counseling, and contraceptive availability increased “mean knowledge score about sexual health and contraception” (SMD: 2.04; 95% CI: 1.31–2.78), “mean condom use self-efficacy score” (SMD: .76; 95% CI: .22–1.30), use of any contraception (RR: 1.07; 95% CI: 1.00–1.14), and condom use (RR: 1.11; 95% CI: 1.04–1.20; Figures 2 and 3). Sexual health education did not significantly impact risk of having sex (RR: 1.00; 95% CI: .93–1.07) or STIs (RR: 1.08; 95% CI: .79–1.46). Pooled analysis from moderate quality evidence showed a 15% decrease (RR: .85; 95% CI: .74–.98) in incidence of adolescent pregnancies and a 37% decrease (RR: .63; 95% CI: .49–.82) in the rate of repeat adolescent pregnancies.
Figure 2.
Impact of sexual health education/counseling on mean knowledge score. CI = confidence interval; FOYC = Focus on Youth in the Caribbean; GIT = Goal for IT; IV = inverse variance; SD = standard deviation.
Figure 3.
Impact of sexual health education/counseling on use of any contraception. CI = confidence interval; IV = inverse variance; SE = standard error.
Subgroup analysis according to the type of interventions suggests that peer-led counseling significantly improved mean knowledge score however did not significantly impact use of contraception. Peer-led counseling comprised peer educators providing information and counseling through one-on-one sessions, group talks and presentations, and distribution of print materials. Number of group sessions varied from study to study, ranging from three sessions to nine sessions. The intervention mainly emphasized male and female anatomy–physiology of the reproductive system, preventive precautions against sexually transmitted diseases and HIV/AIDS, family planning methods, communication skills, ethnic and gender pride, condom use skills, and healthy relationships. Parent-directed interventions were also effective in improving sexual knowledge, and the interventions included a 20-minute video filmed, which addressed decision-making regarding future planning for the parent and child, parent–child communication about sexual decision-making, followed by role-playing and a condom demonstration. The video was followed by a structured discussion among the participants. Clinic-based interventions comprising counseling, skills building, and case management services improved mean knowledge. These findings are limited to a single study only. Clinic-based face-to-face behavioral counseling and education followed by monthly phone calls for 6 months and reproductive health intervention combining a highly explicit half-hour slide-tape program with a personal health consultation did not have any impact on contraceptive use. Technology-based interventions including custom-computerized intervention in which content and delivery were based on the Information–Motivation–Behavioral Skills model of health behavior change and teen-led, media literacy curriculum focused on sexual portrayals in the media were effective in improving sexual knowledge but did not have any impact on contraceptive use. School-based interventions including combined sex education with youth-friendly sexual health services, curriculum modules implemented by adult facilitators or peer cofacilitators (including abstinence education, delaying sexual intercourse or reducing its frequency, safer sex intervention, condom use), and HIV prevention education were effective in improving contraceptive use but did not impact mean knowledge scores. Subgroup analysis for HICs and LMICs could not be conducted due to limited number of studies in LMIC settings (Table 2). Data quality was rated to be “moderate” since the study designs were not robust (included RCTs, quasi and pre–post studies), substantial statistical heterogeneity, and limited generalizability.
Table 2.
Summary of findings for the effect of sexual and reproductive health interventions
| Quality assessment |
Summary of findings |
|||||||
|---|---|---|---|---|---|---|---|---|
| Number of studies | Design | Limitations | Consistency | Directness |
Number of participants |
RR/SMD (95% CI) | ||
| Generalizability to population of interest | Generalizability to intervention of interest | Intervention | Control | |||||
| Mean knowledge score: moderate outcome-specific quality of evidence | ||||||||
| 13 | RCT and pre–post | Study design is not robust | Twelve studies suggest benefit Substantial heterogeneity, I2 = 100% | All studies targeted adolescents | Multicomponent interventions | 6,206 | 6,293 | 2.04 (1.31–2.78) |
| Mean efficacy score: moderate outcome-specific quality of evidence | ||||||||
| 5 | RCT and pre–post | Study design is not robust | Four studies suggest benefit Substantial heterogeneity, I2 = 99% | All studies targeted adolescents | Multicomponent intervention | 2,699 | 2,508 | .76 (.22–1.30) |
| Use of any contraception: moderate outcome-specific quality of evidence | ||||||||
| 16 | RCT and pre–post | Study design is not robust | Five studies suggest benefit Substantial heterogeneity, I2 = 89% | All studies targeted adolescents | Multicomponent intervention | 9,269 | 9,364 | 1.07 (1.00–1.14) |
| Condom use: moderate outcome-specific quality of evidence | ||||||||
| 23 | RCT and pre–post | Study design is not robust | Seven studies suggest benefit Considerable heterogeneity, I2 = 72% | All studies targeted adolescents | Multicomponent intervention | 9,659 | 9,842 | 1.11 (1.04–1.20) |
| Sexual encounter: moderate outcome-specific quality of evidence | ||||||||
| 23 | RCT and pre–post | Study design is not robust | Only two studies suggest reduced sex Substantial heterogeneity, I2 = 88% | All studies targeted adolescents | Multicomponent intervention | 16,845 | 16,746 | 1.00 (.93–1.07) |
| Adolescent pregnancies: moderate outcome-specific quality of evidence | ||||||||
| 18 | RCT | Four studies showed significant improvement Some heterogeneity, I2 = 54% | All studies targeted adolescents | Comprehensive interventions addressing communities, sexual and reproductive health services, contraceptive provision and school-based education, and youth development | 1,572 | 1,868 | .85 (.74–.98) | |
| Repeat adolescent pregnancies: moderate outcome-specific quality of evidence | ||||||||
| 16 | RCT | Six studies showed significant improvement Considerable heterogeneity, I2 = 74% | All studies targeted adolescents | Parental skills training and encouraging young mothers to finish school, as well as comprehensive medical care | 1,572 | 1,868 | .63 (.49–.82) [I2: 74%] | |
| STI: moderate outcome-specific quality of evidence | ||||||||
| Six | RCT and pre–post | Study design is not robust | Only one study suggests reduced sex Considerable heterogeneity, I2 = 78% | All studies targeted adolescents | Multicomponent intervention | 298 | 367 | 1.8 (.79–1.46) [I2: 78%] |
CI = confidence interval; RCT = randomized controlled trial; RR = relative risk; SMD = standard mean difference; STI = sexually transmitted infection.
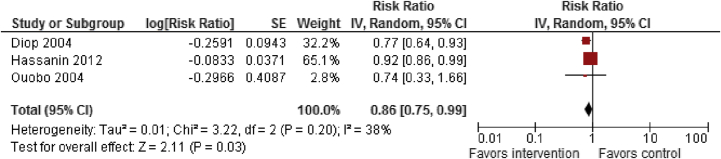
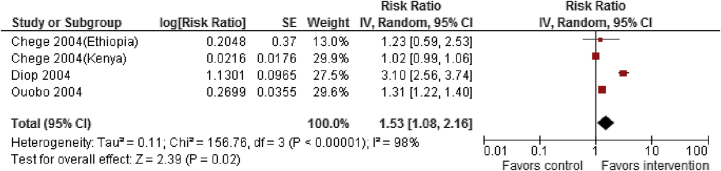
Female genital mutilation
A search was conducted for literature published after March 2011 following the same methodology as Berg et al. A total of 11 studies [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135] (eight included in existing review + three new studies) were included, mostly from Africa. All studies were pre–post studies. For female genital mutilation prevention, studies focused on interventions, including: (1) legislation against FGM/C; (2) education about health risks associated with FGM/C; (3) training health workers as change agents; (4) training and converting circumcisers; (5) alternative rites; (6) positive deviance; and (7) comprehensive social development including outreach and advocacy. Findings from low-quality evidence suggest that interventions to prevent FGM/C did not have any significant impact on belief that FGM/C compromises human rights of women, though there was significant statistical heterogeneity in the two included studies (RR: 1.30; 95% CI: .47–3.64). However, these interventions significantly reduced the prevalence of FGM/C (RR: .86; 95% CI: .75–.99) and improved knowledge of harmful consequences of FGM/C (RR: 1.53; 95% CI: 1.08–2.16; Figures 4 and 5), though there was significant heterogeneity in the interventions (Table 3). Subgroup analysis suggests that these interventions significantly improved knowledge of harmful consequences in both men and women. These studies suggest that the factors related to the continuance and discontinuance of FGM/C varied across contexts, but the main factors that supported FGM/C were tradition, religion, and reduction of women's sexual desire.
Figure 4.
Impact of interventions to prevent FGM on FGM prevalence. CI = confidence interval; FGM = female genital mutilation; IV = inverse variance; SE = standard error.
Figure 5.
Impact of interventions to prevent FGM on knowledge of harmful consequences. CI = confidence interval; FGM = female genital mutilation; IV = inverse variance; SE = standard error.
Table 3.
Summary of findings for the effect of interventions to prevent female genital mutilation
| Quality assessment |
Summary of findings |
|||||||
|---|---|---|---|---|---|---|---|---|
| Number of studies | Design | Limitations | Consistency | Directness |
Number of participants |
SMD/RR (95% CI) | ||
| Generalizability to population of interest | Generalizability to intervention of interest | Intervention | Control | |||||
| Belief that FGM/C compromise human rights of women: low outcome-specific quality of evidence | ||||||||
| One | Pre–post | Study design is not robust | Only one study | All studies targeted adolescents | Multicomponent intervention | 1,120 | 1,120 | 1.30 (.47–3.64) |
| Prevalence of FGM/C: low outcome-specific quality of evidence | ||||||||
| Three | Pre–post | Study design is not robust | Two studies showed reduced prevalence. Low heterogeneity, I2 = 38% | All studies targeted adolescents | Multicomponent intervention | 1,377 | 916 | .63 (.49–.82) |
| Knowledge of harmful consequences of FGM/C: low outcome-specific quality of evidence | ||||||||
| Three | Pre–post | Study design is not robust | Two studies showed benefit Substantial heterogeneity, I2 = 98% | All studies targeted adolescents | Multicomponent intervention | 2,368 | 1,987 | 1.53 (1.08–2.16) |
CI = confidence interval; FGM/C = Female Genital Mutilation/Cutting; RR = relative risk; SMD = standard mean difference.
Intimate partner violence
We report the findings from a Cochrane review by Fellmeth et al. [40] focusing on educational and skills-based interventions targeted at young people aged 12–25 years for preventing intimate partner violence with an AMSTAR rating of 11 . A total of 38 studies were included, 33 of which were included in the meta-analysis. All the included studies were conducted in HICs. There was an increase in knowledge related to relationship violence in favor of the intervention (SMD: .44; 95% CI: .28–.60). However, moderate-quality evidence suggests no significant impact of such interventions on episodes of relationship violence (RR: .77; 95% CI: .53–1.13), behavior scores related to relationship violence (SMD: −.07; 95% CI: −.31 to .16), and a skills score related to relationship violence (to communicate effectively; SMD: .03; 95% CI: −.11 to .17). Subgroup analyses showed no statistically significant differences by intervention setting or type of participants.
Discussion
Our review suggests that sexual and reproductive health education, counseling, and contraceptive availability are effective in increasing adolescent knowledge related to sexual health, contraceptive use, and decreasing adolescent pregnancy. We could not conduct subgroup analysis for the effectiveness of these interventions in HICs and LMICs since there were limited studies from LMIC settings. Among interventions to prevent FGM/C, community mobilization and female empowerment have the potential to raise awareness of the adverse health consequences of FGM/C and decrease its prevalence; however, there is a need to conduct methodologically rigorous intervention evaluations. Overall, there was limited and inconclusive evidence for the effectiveness of interventions to prevent intimate partner violence.
Our findings are in concordance with existing reviews evaluating the effectiveness of various interventions for improving adolescent sexual and reproductive health and also collate various interventions under a broader umbrella to evaluate the combined effectiveness of these interventions. An existing Cochrane review on primary prevention interventions (school based, community or home based, clinic based, and faith based) on unintended pregnancies among adolescents also suggests that combination of educational and contraceptive interventions can lower the rate of unintended pregnancy among adolescents with nonconclusive evidence on secondary outcomes, including initiation of sexual intercourse, use of birth control methods, abortion, childbirth, and STIs [13]. Group-based comprehensive risk reduction has been reported as an effective strategy to reduce adolescent pregnancy, HIV, and STIs while effectiveness of group-based abstinence education was inconclusive [136]. Another review on adolescent fertility in LMICs suggests improved knowledge-based indicators in the intervention groups of almost all interventions evaluated; however, it is not clear that such interventions necessarily lead to short- or long-term behavior change [137], [138].
The United Nations Fund for Population Activities (UNFPA) and United Nations International Children's Emergency Fund (UNICEF) joint program, developed in 2007 to protect girls and women by accelerating abandonment of FGM/C and providing care for its consequences, has accelerated existing changes toward FGM/C abandonment by legal frameworks, coordination mechanisms, and access to services at both community and national level. But, further efforts are needed, especially at the national and community levels, to bring changes in behaviors and practices [139]. A recent report by WHO on preventing intimate partner and sexual violence suggests that evidence is still in its infancy and much remains to be accomplished [140].
This existing evidence on adolescent sexual reproductive health has several limitations. Most trials failed to utilize allocation concealment, blinding, and randomization to optimize their outcomes. Hence, most of the outcomes were rated as low or moderate in methodological quality. There was a lack of rigorous study design for the interventions to prevent FGM/C with most studies utilizing before and after designs without comparable controls, although individual or cluster RCTs to address FGM/C would pose huge ethical challenges. Nevertheless, many of the trials focused on nonstandardized and self-reported outcomes with short follow-up periods that might have been insufficient to detect any meaningful behavioral changes to establish or to wash out the effect of intervention. Most studies on intimate partner violence analyzed outcomes such as attitude and knowledge rather than episodes of violence and behavioral change. Furthermore, we found a dearth of evidence on interventions for improving sexual health of adolescents living in LMICs where the majority of the adolescent population of the world resides. This might lead to limited external validity for many of these interventions. Most of the studies did not report data segregated by gender which is essential since males and females might respond differently to behavioral interventions. The wide variability in study constructs, nonuniformity in subgroup population, lack of subgroup analysis of gender, socioeconomic status, and nonstandardized outcomes all preclude the external validity and effectiveness of the present interventions in LMICs.
Our review suggests that a range of comprehensive interventions targeting sexual health education, counseling, consistent birth control methods promotion, and provision have the potential to prevent and control the adverse outcomes related to risky sexual behavior. However, much more is needed to increase awareness and prevent FGM and intimate partner violence.
Acknowledgments
All authors contributed to finalizing the manuscript.
Footnotes
Conflicts of Interest: The authors do not have any financial or nonfinancial competing interests for this review.
Disclaimer: Publication of this article was supported by the Bill and Melinda Gates Foundation. The opinions or views expressed in this supplement are those of the authors and do not necessarily represent the official position of the funder.
Funding Sources
The preparation and publication of these papers was made possible through an unrestricted grant from the Bill & Melinda Gates Foundation (BMGF).
References
- 1.Chandra-Mouli V., McCarraher D.R., Phillips S.J., Williamson N.E., Hainsworth G. Contraception for adolescents in low and middle income countries: Needs, barriers, and access. Reprod Health. 2014;11:1. doi: 10.1186/1742-4755-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd C.B., editor. Growing up global: The changing transitions to adulthood in developing countries. National Academies Press; Washington, DC: 2005. [Google Scholar]
- 3.Williamson N. Facing the challenge of adolescent pregnancy. United Nations Population Fund; New York, NY: 2013. State of world population 2013. Motherhood in childhood; p. 132. [Google Scholar]
- 4.United Nations: We can end poverty: Millennium development goals and beyond 2015. Available at: http://www.un.org/millenniumgoals/childhealth.shtml. Accessed November 16, 2015.
- 5.World Health Organization . 2012. Adolescent pregnancy. [Google Scholar]
- 6.United Nations Fund for Population Activities . 2013. Adolescent and youth demographics: A brief overview. [Google Scholar]
- 7.World Health Organization: Health for the world's adolescents: A second chance in the second decade. Available at: http://public.tableausoftware.com/profile/digitalteam#!/vizhome/shared/3JW3RBSZ3. Accessed November 16, 2015.
- 8.Haldre K., Rahu K., Karro H., Rahu M. Is a poor pregnancy outcome related to young maternal age? A study of teenagers in Estonia during the period of major socio-economic changes (from 1992 to 2002) Eur J Obstetrics Gynecol Reprod Biol. 2007;131:45–51. doi: 10.1016/j.ejogrb.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Michaud P.A., Ambresin A.E. The health of adolescents around a world in transition. Georgian Med News. 2014;5:54–59. http://www.geomednews.org/shared/issues/med230.pdf#page=59 Available at: [PubMed] [Google Scholar]
- 10.United Nations International Children's Emergency Fund (UNICEF) 2012. Progress for children: A report card on adolescents. (No. 10)http://www.unicef.org/publications/files/Progress_for_Children_-_No._10_EN_04272012.pdf New York, NY: U.S. Available at: Accessed November 16, 2015. [Google Scholar]
- 11.United Nations Population Fund . 2013. Motherhood in childhood: Facing the challenge of adolescent pregnancy.http://www.unfpa.org/webdav/site/global/shared/swp2013/EN-SWOP2013-final.pdf Available at: Accessed November 16, 2015. [Google Scholar]
- 12.World Health Organization (WHO) WHO; Geneva: 2007. Adolescent pregnancy—unmet needs and undone deeds: A review of the literature and programmes; pp. 55–56. [Google Scholar]
- 13.Oringanje C., Meremikwu M.M., Eko H. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database Syst Rev. 2009:CD005215. doi: 10.1002/14651858.CD005215.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Berg R.C., Denison E. Interventions to reduce the prevalence of female genital mutilation/cutting in African countries. Campbell Systematic Reviews. 2012:9. [Google Scholar]
- 15.Yoder S., Abderrahim N., Zhuzhuni A. ORC Macro; Calverton, Maryland, USA: 2004. Female genital cutting in the demographic and health surveys: A critical and comparative analysis. DHS comparative reports no. 7. [Google Scholar]
- 16.Yoder S., Kahn S. United States Agency for International Development; USA: 2008. Numbers of women circumcised in Africa: The production of a total. DHS working papers. [Google Scholar]
- 17.World Health Organization; Geneva: 2006. HRP (the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction). Progress in sexual and reproductive health, Newsletter 72. [Google Scholar]
- 18.Berg R.C., Denison E. Does female genital mutilation/cutting (FGM/C) affect women's sexual functioning? A systematic review of the sexual consequences of FGM/C. Sex Res Soc Pol. 2012;9:41–56. [Google Scholar]
- 19.WHO study group on female genital mutilation and obstetric outcome. Banks E., Meirik O. Female genital mutilation and obstetric outcome: WHO collaborative prospective study in six African countries. Lancet. 2006;367:1835–1841. doi: 10.1016/S0140-6736(06)68805-3. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization . WHO; Geneva: 2011. WHO guidelines on preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. [PubMed] [Google Scholar]
- 21.United Nations Fund for Population Activities . 2014. Adding it up: The cost and benefit of investing in sexual and reproductive health.http://www.unfpa.org/sites/default/files/pub-pdf/Adding%20It%20Up-Final-11.18.14.pdf Available at: Accessed November 16, 2015. [Google Scholar]
- 22.Salam R.A., Das J.K., Lassi Z.S., Bhutta Z.A. Adolescent health and well-being: Background and methodology for review of potential interventions. J Adolesc Health. 2016;59(Suppl. 4):S4–S10. doi: 10.1016/j.jadohealth.2016.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salam R.A., Hooda M., Das J.K. Interventions to improve adolescent nutrition: A systematic review and meta-analysis. J Adolesc Health. 2016;59(Suppl. 4):S29–S39. doi: 10.1016/j.jadohealth.2016.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Das J.K., Salam R.A., Arshad A. Systematic review and meta-analysis of interventions to improve access and coverage of adolescent immunizations. J Adolesc Health. 2016;59(Suppl. 4):S40–S48. doi: 10.1016/j.jadohealth.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Das J.K., Salam R.A., Arshad A. Interventions for adolescent substance abuse: An overview of systematic reviews. J Adolesc Health. 2016;59(Suppl. 4):S61–S75. doi: 10.1016/j.jadohealth.2016.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Das J.K., Salam R.A., Lassi Z.S. Interventions for adolescent mental health: an overview of systematic reviews. J Adolesc Health. 2016;59(Suppl. 4):S49–S60. doi: 10.1016/j.jadohealth.2016.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salam R.A., Arshad A., Das J.K. Interventions to prevent unintentional injuries among adolescents: A systematic review and meta-analysis. J Adolesc Health. 2016;59(Suppl. 4):S76–S87. doi: 10.1016/j.jadohealth.2016.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salam R.A., Das J.K., Lassi Z.S., Bhutta Z.A. Adolescent health interventions: Conclusions, evidence gaps, and research priorities. J Adolesc Health. 2016;59(Suppl. 4):S88–S92. doi: 10.1016/j.jadohealth.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walker N., Fischer-Walker C., Bryce J. Standards for CHERG reviews of intervention effects on child survival. Int J Epidemiol. 2010;39(Suppl.1):i21–i31. doi: 10.1093/ije/dyq036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shea B.J., Grimshaw J.M., Wells G.A. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mason-Jones A.J., Crisp C., Momberg M. A systematic review of the role of school-based healthcare in adolescent sexual, reproductive, and mental health. Syst Rev. 2012;1:1–13. doi: 10.1186/2046-4053-1-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bennett S.E., Assefi N.P. School-based teenage pregnancy prevention programs: A systematic review of randomized controlled trials. J Adolesc Health. 2005;36:72–81. doi: 10.1016/j.jadohealth.2003.11.097. [DOI] [PubMed] [Google Scholar]
- 33.Kim C.R., Free C. Recent evaluations of the peer-led approach in adolescent sexual health education: A systematic review. Perspect Sex Reprod Health. 2008;40:144–151. doi: 10.1363/4014408. [DOI] [PubMed] [Google Scholar]
- 34.Guse K., Levine D., Martins S. Interventions using new digital media to improve adolescent sexual health: A systematic review. J Adolesc Health. 2012;51:535–543. doi: 10.1016/j.jadohealth.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 35.Jones K., Eathington P., Baldwin K., Sipsma H. The impact of health education transmitted via social media or text messaging on adolescent and young adult risky sexual behavior: A systematic review of the literature. Sex Transm Dis. 2014;41:413–419. doi: 10.1097/OLQ.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 36.Zuurmond M.A., Geary R.S., Ross D.A. The effectiveness of youth centers in increasing use of sexual and reproductive health services: A systematic review. Stud Fam Plann. 2012;43:239–254. doi: 10.1111/j.1728-4465.2012.00324.x. [DOI] [PubMed] [Google Scholar]
- 37.Wamoyi J., Mshana G., Mongi A. A review of interventions addressing structural drivers of adolescents' sexual and reproductive health vulnerability in sub-Saharan Africa: Implications for sexual health programming. Reprod Health. 2014;11:88. doi: 10.1186/1742-4755-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Speizer I.S., Magnani R.J., Colvin C.E. The effectiveness of adolescent reproductive health interventions in developing countries: A review of the evidence. J Adolesc Health. 2003;33:324–348. doi: 10.1016/s1054-139x(02)00535-9. [DOI] [PubMed] [Google Scholar]
- 39.DiCenso A., Guyatt G., Willan A., Griffith L. Interventions to reduce unintended pregnancies among adolescents: Systematic review of randomised controlled trials. BMJ. 2002;324:1426. doi: 10.1136/bmj.324.7351.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fellmeth G.L., Heffernan C., Nurse J. Educational and skills-based interventions for preventing relationship and dating violence in adolescents and young adults. Cochrane Database Syst Rev. 2013:CD004534. doi: 10.1002/14651858.CD004534.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aarons S.J., Jenkins R.R., Raine T.R. Postponing sexual intercourse among urban junior high school students-a randomized controlled evaluation. J Adolesc Health. 2000;27:236–247. doi: 10.1016/s1054-139x(00)00102-6. [DOI] [PubMed] [Google Scholar]
- 42.Agha S., Van Rossem R. Impact of a school-based peer sexual health intervention on normative beliefs, risk perceptions, and sexual behavior of Zambian adolescents. J Adolesc Health. 2004;34:441–452. doi: 10.1016/j.jadohealth.2003.07.016. [DOI] [PubMed] [Google Scholar]
- 43.Baptiste D.R., Bhana A., Petersen I. Community collaborative youth-focused HIV/AIDS prevention in South Africa and Trinidad: Preliminary findings. J Pediatr Psychol. 2006;31:905–916. doi: 10.1093/jpepsy/jsj100. [DOI] [PubMed] [Google Scholar]
- 44.Barnet B., Liu J., DeVoe M. Home visiting for adolescent mothers: Effects on parenting, maternal life course, and primary care linkage. Ann Fam Med. 2007;5:224–232. doi: 10.1370/afm.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berenson A.B., Rahman M. A randomized controlled study of two educational interventions on adherence with oral contraceptives and condoms. Contraception. 2012;86:716–724. doi: 10.1016/j.contraception.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Black M.M., Bentley M.E., Papas M.A. Delaying second births among adolescent mothers: A randomized, controlled trial of a home-based mentoring program. Pediatrics. 2006;118:e1087–e1099. doi: 10.1542/peds.2005-2318. [DOI] [PubMed] [Google Scholar]
- 47.Blake S.M., Ledsky R., Goodenow C. Condom availability programs in Massachusetts high schools: Relationships with condom use and sexual behavior. Am J Public Health. 2003;93:955–962. doi: 10.2105/ajph.93.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bonell C., Maisey R., Speight S. Randomized controlled trial of 'teens and toddlers': A teenage pregnancy prevention intervention combining youth development and voluntary service in a nursery. J adolescence. 2013;36:859–870. doi: 10.1016/j.adolescence.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 49.Brieger W.R., Delano G.E., Lane C.G. West African youth initiative: Outcome of a reproductive health education program. J Adolesc Health. 2001;29:436–446. doi: 10.1016/s1054-139x(01)00264-6. [DOI] [PubMed] [Google Scholar]
- 50.Bull S.S., Levine D.K., Black S.R. Social media delivered sexual health intervention: A cluster randomized controlled trial. Am J Prev Med. 2012;43:467–474. doi: 10.1016/j.amepre.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen X., Stanton B., Gomez P. Effects on condom use of an HIV prevention programme 36 months postintervention: A cluster randomized controlled trial among Bahamian youth. Int J STD AIDS. 2010;21:622–630. doi: 10.1258/ijsa.2010.010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Clark L.F., Miller K.S., Nagy S.S. Adult identity mentoring: Reducing sexual risk for African-American seventh grade students. J Adolesc Health. 2005;37:337. doi: 10.1016/j.jadohealth.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 53.Cornelius J.B., Dmochowski J., Boyer C. Text-messaging-enhanced HIV intervention for African American adolescents: A feasibility study. J Assoc Nurses AIDS Care. 2013;24:256–267. doi: 10.1016/j.jana.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coyle K., Basen-Engquist K., Kirby D. Safer choices: Reducing teen pregnancy, HIV, and STDs. Public Health Rep. 2001;116(Suppl. 1):82. doi: 10.1093/phr/116.S1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coyle K.K., Glassman J.R., Franks H.M. Interventions to reduce sexual risk behaviors among youth in alternative schools: A randomized controlled trial. J Adolesc Health. 2013;53:68–78. doi: 10.1016/j.jadohealth.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coyle K.K., Kirby D.B., MarÃn B.V. Draw the line/respect the line: A randomized trial of a middle school intervention to reduce sexual risk behaviors. Am J Public Health. 2004;94:843–851. doi: 10.2105/ajph.94.5.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Danielson R., Marcy S., Plunkett A. Reproductive health counseling for young men: What does it do? Fam Plann Perspect. 1990;22:115–121. [PubMed] [Google Scholar]
- 58.DiClemente R.J., Wingood G.M., Harrington K.F. Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. JAMA. 2004;292:171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- 59.DiClemente R.J., Wingood G.M., Rose E.S. Efficacy of sexually transmitted disease/human immunodeficiency virus sexual risk-reduction intervention for African American adolescent females seeking sexual health services: A randomized controlled trial. Arch Pediatr Adolesc Med. 2009;163:1112–1121. doi: 10.1001/archpediatrics.2009.205. [DOI] [PubMed] [Google Scholar]
- 60.DiIorio C., McCarty F., Resnicow K. Real men: A group-randomized trial of an HIV prevention intervention for adolescent boys. Am J Public Health. 2007;97:1084–1089. doi: 10.2105/AJPH.2005.073411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Downs J.S., Murray P.J., Bruine de Bruin Wn. Interactive video behavioral intervention to reduce adolescent females' STD risk: A randomized controlled trial. Soc Sci Med. 2004;59:1561–1572. doi: 10.1016/j.socscimed.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 62.Elliott L., Henderson M., Nixon C., Wight D. Has untargeted sexual health promotion for young people reached its limit? A quasi-experimental study. J Epidemiol Community Health. 2013;67:398–404. doi: 10.1136/jech-2012-201034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ferguson S.L. Peer counseling in a culturally specific adolescent pregnancy prevention program. J Health Care Poor Underserved. 1998;9:322–340. doi: 10.1353/hpu.2010.0291. [DOI] [PubMed] [Google Scholar]
- 64.Forehand R., Armistead L., Long N. Efficacy of a parent-based sexual-risk prevention program for African American preadolescents: A randomized controlled trial. Arch Pediatr Adolesc Med. 2007;161:1123–1129. doi: 10.1001/archpedi.161.12.1123. [DOI] [PubMed] [Google Scholar]
- 65.Garcia P.J., Holmes K.K., Carcamo C.P. Prevention of sexually transmitted infections in urban communities (Peru PREVEN): A multicomponent community-randomised controlled trial. Lancet. 2012;379:1120–1128. doi: 10.1016/S0140-6736(11)61846-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gold M.A., Wolford J.E., Smith K.A., Parker A.M. The effects of advance provision of emergency contraception on adolescent women's sexual and contraceptive behaviors. J Pediatr Adolesc Gynecol. 2004;17:87–96. doi: 10.1016/j.jpag.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 67.Hall K.S., Westhoff C.L., Castano P.M. The impact of an educational text message intervention on young urban women's knowledge of oral contraception. Contraception. 2013;87:449–454. doi: 10.1016/j.contraception.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Harper G.W., Bangi A.K., Sanchez B. A quasi-experimental evaluation of a community-based HIV prevention intervention for Mexican American female adolescents: The SHERO's program. AIDS Educ Prev. 2009;21(5 Suppl.):109–123. doi: 10.1521/aeap.2009.21.5_supp.109. [DOI] [PubMed] [Google Scholar]
- 69.Herceg-Baron R., Furstenberg F.F., Jr., Shea J., Harris K.M. Supporting teenagers' use of contraceptives: A comparison of clinic services. Fam Plann Perspect. 1986;18:61–66. [PubMed] [Google Scholar]
- 70.Howard M., McCabe J.B. Helping teenagers postpone sexual involvement. Fam Plann Perspect. 1990;22:21–26. [PubMed] [Google Scholar]
- 71.Hughes M.E., Furstenberg F.F., Jr., Teitler J.O. The impact of an increase in family planning services on the teenage population of Philadelphia. Fam Plann Perspect. 1995;27:60–65. [PubMed] [Google Scholar]
- 72.Jemmott J.B., III, Jemmott L.S., Fong G.T. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: A randomized controlled trial. JAMA. 1998;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- 73.Jemmott J.B., Jemmott L.S., Braverman P.K., Fong G.T. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: A randomized controlled trial. Arch Pediatr Adolesc Med. 2005;159:440–449. doi: 10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]
- 74.Jemmott J.B., Jemmott L.S., O'Leary A. School-based randomized controlled trial of an HIV/STD risk-reduction intervention for South African adolescents. Arch Pediatr Adolesc Med. 2010;164:923–929. doi: 10.1001/archpediatrics.2010.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Key J.D., Gebregziabher M.G., Marsh L.D., O'Rourke K.M. Effectiveness of an intensive, school-based intervention for teen mothers. J Adolesc Health. 2008;42:394–400. doi: 10.1016/j.jadohealth.2007.09.027. [DOI] [PubMed] [Google Scholar]
- 76.Kiene S.M., Barta W.D. A brief individualized computer-delivered sexual risk reduction intervention increases HIV/AIDS preventive behavior. J Adolesc Health. 2006;39:404–410. doi: 10.1016/j.jadohealth.2005.12.029. [DOI] [PubMed] [Google Scholar]
- 77.Kinsler J., Sneed C.D., Morisky D.E., Ang A. Evaluation of a school-based intervention for HIV/AIDS prevention among Belizean adolescents. Health Educ Res. 2004;19:730–738. doi: 10.1093/her/cyg091. [DOI] [PubMed] [Google Scholar]
- 78.Kirby D., Raine T., Thrush G. Impact of an intervention to improve contraceptive use through follow-up phone calls to female adolescent clinic patients. Perspect Sex Reprod Health. 2010;42:251–257. doi: 10.1363/4225110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kirby D.B., Baumler E., Coyle K.K. The “safer choices” intervention: Its impact on the sexual behaviors of different subgroups of high school students. J Adolesc Health. 2004;35:442–452. doi: 10.1016/j.jadohealth.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 80.Kisker E.E., Brown R.S. Do school-based health centers improve adolescents' access to health care, health status, and risk-taking behavior? J Adolesc Health. 1996;18:335–343. doi: 10.1016/1054-139X(95)00236-L. [DOI] [PubMed] [Google Scholar]
- 81.Klepp K.-I., Ndeki S.S., Leshabari M.T. AIDS education in Tanzania: Promoting risk reduction among primary school children. Am J Public Health. 1997;87:1931–1936. doi: 10.2105/ajph.87.12.1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kogan S.M., Yu T., Brody G.H. Integrating condom skills into family-centered prevention: Efficacy of the strong African American families' teen program. J Adolesc Health. 2012;51:164–170. doi: 10.1016/j.jadohealth.2011.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Koo H.P., Rose A., El-Khorazaty M.N. Evaluation of a randomized intervention to delay sexual initiation among fifth-graders followed through the sixth grade. Sex Educ. 2011;11:27–46. doi: 10.1080/14681811.2011.538146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Larke N., Cleophas-Mazige B., Plummer M.L. Impact of the MEMA kwa Vijana adolescent sexual and reproductive health interventions on use of health services by young people in rural Mwanza, Tanzania: Results of a cluster randomized trial. J Adolesc Health. 2010;47:512–522. doi: 10.1016/j.jadohealth.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 85.Lewis L.N., Doherty D.A., Hickey M., Skinner S.R. Implanon as a contraceptive choice for teenage mothers: A comparison of contraceptive choices, acceptability and repeat pregnancy. Contraception. 2010;81:421–426. doi: 10.1016/j.contraception.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 86.Lim M.S.C., Hocking J.S., Aitken C.K. Impact of text and email messaging on the sexual health of young people: A randomised controlled trial. J Epidemiol Community Health. 2012;66:69–74. doi: 10.1136/jech.2009.100396. [DOI] [PubMed] [Google Scholar]
- 87.Marcell A.V., Allan E., Clay E.A. Effectiveness of a brief curriculum to promote condom and health care use among out-of-school young adult males. Perspect Sex Reprod Health. 2013;45:33–40. doi: 10.1363/4503313. [DOI] [PubMed] [Google Scholar]
- 88.Markham C.M., Tortolero S.R., Peskin M.F. Sexual risk avoidance and sexual risk reduction interventions for middle school youth: A randomized controlled trial. J Adolesc Health. 2012;50:279–288. doi: 10.1016/j.jadohealth.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mason-Jones A.J., Mathews C., Flisher A.J. Can peer education make a difference? Evaluation of a South African adolescent peer education program to promote sexual and reproductive health. AIDS Behav. 2011;15:1605–1611. doi: 10.1007/s10461-011-0012-1. [DOI] [PubMed] [Google Scholar]
- 90.McBride C.K., Baptiste D., Traube D. Family-based HIV preventive intervention: Child level results from the CHAMP family program. Social work Ment Health. 2007;5:203–220. doi: 10.1300/J200v05n01_10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Meekers D. The effectiveness of targeted social marketing to promote adolescent reproductive health: The case of Soweto, South Africa. J HIV/AIDS Prev Educ Adolesc Child. 2000;3:73–92. [PubMed] [Google Scholar]
- 92.Meekers D., Agha S., Klein M. The impact on condom use of the “100% Jeune” social marketing program in Cameroon. J Adolesc Health. 2005;36:530. doi: 10.1016/j.jadohealth.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 93.Merakou K., Kourea-Kremastinou J. Peer education in HIV prevention: An evaluation in schools. Eur J Public Health. 2006;16:128–132. doi: 10.1093/eurpub/cki162. [DOI] [PubMed] [Google Scholar]
- 94.Morrison-Beedy D., Jones S.H., Xia Y. Reducing sexual risk behavior in adolescent girls: Results from a randomized controlled trial. J Adolesc Health. 2013;52:314–321. doi: 10.1016/j.jadohealth.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Munodawafa D., Marty P.J., Gwede C. Effectiveness of health instruction provided by student nurses in rural secondary schools of Zimbabwe: A feasibility study. Int J Nurs Stud. 1995;32:27–38. doi: 10.1016/0020-7489(94)00029-j. [DOI] [PubMed] [Google Scholar]
- 96.O-Donnell L., Stueve A., O'Donnell C. Long-term reductions in sexual initiation and sexual activity among urban middle schoolers in the reach for health service learning program. J Adolesc Health. 2002;31:93–100. doi: 10.1016/s1054-139x(01)00389-5. [DOI] [PubMed] [Google Scholar]
- 97.Ozcebe H., Akin L., Aslan D. A peer education example on HIV/AIDS at a high school in Ankara. Turk J Pediatr. 2004;46:54–59. [PubMed] [Google Scholar]
- 98.Pearlman D.N., Camberg L., Wallace L.J. Tapping youth as agents for change: Evaluation of a peer leadership HIV/AIDS intervention. J Adolesc Health. 2002;31:31–39. doi: 10.1016/s1054-139x(02)00379-8. [DOI] [PubMed] [Google Scholar]
- 99.Peltzer K., Simbayi L., Banyini M., Kekana Q. HIV risk reduction intervention among traditionally circumcised young men in South Africa: A cluster randomized control trial. J Assoc Nurses AIDS Care. 2011;22:397–406. doi: 10.1016/j.jana.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 100.Petersen R., Albright J.B., Garrett J.M., Curtis K.M. Acceptance and use of emergency contraception with standardized counseling intervention: Results of a randomized controlled trial. Contraception. 2007;75:119–125. doi: 10.1016/j.contraception.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 101.Pinkleton B.E., Austin E.W., Cohen M. Effects of a peer-led media literacy curriculum on adolescents' knowledge and attitudes toward sexual behavior and media portrayals of sex. Health Commun. 2008;23:462–472. doi: 10.1080/10410230802342135. [DOI] [PubMed] [Google Scholar]
- 102.Prado G., Pantin H., Huang S. Effects of a family intervention in reducing HIV risk behaviors among high-risk Hispanic adolescents: A randomized controlled trial. Arch Pediatr Adolesc Med. 2012;166:127–133. doi: 10.1001/archpediatrics.2011.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Raymond E.G., Stewart F., Weaver M. Impact of increased access to emergency contraceptive pills: A randomized controlled trial. Obstet Gynecol. 2006;108:1098–1106. doi: 10.1097/01.AOG.0000235708.91572.db. [DOI] [PubMed] [Google Scholar]
- 104.Rickert V.I., Tiezzi L., Lipshutz J. Depo Now: Preventing unintended pregnancies among adolescents and young adults. J Adolesc Health. 2007;40:22–28. doi: 10.1016/j.jadohealth.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 105.Rocca C.H., Schwarz E.B., Stewart F.H. Beyond access: Acceptability, use and nonuse of emergency contraception among young women. Am J obstet Gynecol. 2007;196:29.e1–29.e6. doi: 10.1016/j.ajog.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 106.Rosenbaum J.E. Patient teenagers? A comparison of the sexual behavior of virginity pledgers and matched nonpledgers. Pediatrics. 2009;123:e110–e120. doi: 10.1542/peds.2008-0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ross D.A., Changalucha J., Obasi A.I.N. Biological and behavioural impact of an adolescent sexual health intervention in Tanzania: A community-randomized trial. AIDS. 2007;21:1943–1955. doi: 10.1097/QAD.0b013e3282ed3cf5. [DOI] [PubMed] [Google Scholar]
- 108.Rotheram-Borus M.J., Gwadz M., Fernandez M.I., Srinivasan S. Timing of HIV interventions on reductions in sexual risk among adolescents. Am J Community Psychol. 1998;26:73–96. doi: 10.1023/a:1021834224454. [DOI] [PubMed] [Google Scholar]
- 109.Schreiber C.A., Ratcliffe S.J., Barnhart K.T. A randomized controlled trial of the effect of advanced supply of emergency contraception in postpartum teens: A feasibility study. Contraception. 2010;81:435–440. doi: 10.1016/j.contraception.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 110.Shrier L.A., Ancheta R., Goodman E. Randomized controlled trial of a safer sex intervention for high-risk adolescent girls. Arch Pediatr Adolesc Med. 2001;155:73–79. doi: 10.1001/archpedi.155.1.73. [DOI] [PubMed] [Google Scholar]
- 111.Sieving R.E., Bernat D.H., Resnick M.D. A clinic-based youth development program to reduce sexual risk behaviors among adolescent girls prime time pilot study. Health Promot Pract. 2012;13:462–471. doi: 10.1177/1524839910386011. [DOI] [PubMed] [Google Scholar]
- 112.Suffoletto B., Akers A., McGinnis K.A. A sex risk reduction text-message program for young adult females discharged from the emergency department. J Adolesc Health. 2013;53:387–393. doi: 10.1016/j.jadohealth.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 113.Tocce K.M., Sheeder J.L., Teal S.B. Rapid repeat pregnancy in adolescents: Do immediate postpartum contraceptive implants make a difference? Am J obstet Gynecol. 2012;206:481.e1–481.e7. doi: 10.1016/j.ajog.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 114.Villarruel A.M., Cherry C.L., Cabriales E.G. A parent-adolescent intervention to increase sexual risk communication: Results of a randomized controlled trial. AIDS Educ Prev. 2008;20:371–383. doi: 10.1521/aeap.2008.20.5.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Villarruel A.M., Jemmott J.B., Jemmott L.S. A randomized controlled trial testing an HIV prevention intervention for Latino youth. Arch Pediatr Adolesc Med. 2006;160:772–777. doi: 10.1001/archpedi.160.8.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Walker D., Gutierrez J.P., Torres P., Bertozzi S.M. HIV prevention in Mexican schools: Prospective randomised evaluation of intervention. BMJ. 2006;332:1189–1194. doi: 10.1136/bmj.38796.457407.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Weed S.E., Ericksen I.H., Lewis A. An abstinence program's impact on cognitive mediators and sexual initiation. Am J Health Behav. 2008;32:60–73. doi: 10.5555/ajhb.2008.32.1.60. [DOI] [PubMed] [Google Scholar]
- 118.Wiggins M., Bonell C., Sawtell M. Health outcomes of youth development programme in England: Prospective matched comparison study. BMJ. 2009;339:b2534. doi: 10.1136/bmj.b2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Winter L., Breckenmaker L.C. Tailoring family planning services to the special needs of adolescents. Fam Plann Perspect. 1991;23:24–30. [PubMed] [Google Scholar]
- 120.Zimmer-Gembeck M.J., Doyle L.S., Daniels J.A. Contraceptive dispensing and selection in school-based health centers. J Adolesc Health. 2001;29:177–185. doi: 10.1016/s1054-139x(01)00220-8. [DOI] [PubMed] [Google Scholar]
- 121.Erulkar A.S., Ettyang L.I., Onoka C. Behavior change evaluation of a culturally consistent reproductive health program for young Kenyans. Int Fam Plann Perspect. 2004;30:58–67. doi: 10.1363/3005804. [DOI] [PubMed] [Google Scholar]
- 122.Lou C.H., Wang B., Shen Y., Gao E.S. Effects of a community-based sex education and reproductive health service program on contraceptive use of unmarried youths in Shanghai. J Adolesc Health. 2004;34:433–440. doi: 10.1016/j.jadohealth.2003.07.020. [DOI] [PubMed] [Google Scholar]
- 123.Kim Y.M., Kols A., Nyakauru R. Promoting sexual responsibility among young people in Zimbabwe. Int Fam Plan Perspect. 2001;27:11–19. [Google Scholar]
- 124.Daniel E.E., Masilamani R., Rahman M. The effect of community-based reproductive health communication interventions on contraceptive use among young married couples in Bihar, India. Int Fam Plan Perspect. 2008;34:189–197. doi: 10.1363/ifpp.34.189.08. [DOI] [PubMed] [Google Scholar]
- 125.Diop N., Sangaré M., Tandia F., Touré K. Population Council; Bamako, Mali: 1998. Study of the effectiveness of training Malian social and health agents in female genital cutting issues and in educating their clients. [Google Scholar]
- 126.Diop N.J., Faye M.M., Moreau A. Population Council; Washington: 2004. The TOSTAN program: Evaluation of a community based education program in Senegal. [Google Scholar]
- 127.Mounir G.M., Mahdy N.H., Fatohy I.M. Impact of health education program about reproductive health on knowledge and attitude of female Alexandria University students. J Egypt Public Health Assoc. 2002;78:433–466. [PubMed] [Google Scholar]
- 128.Babalola S., Brasington A., Agbasimalo A. Impact of a communication programme on female genital cutting in eastern Nigeria. Trop Med Int Health. 2006;11:1594–1603. doi: 10.1111/j.1365-3156.2006.01701.x. [DOI] [PubMed] [Google Scholar]
- 129.Chege J., Askew I., Igras S., Mutesh J.K. Testing the effectiveness of integrating community-based approaches for encouraging abandonment of female genital cutting into CARE's reproductive health programs in Ethiopia and Kenya. Front Reprod Health Popul Counc. 2004 [Google Scholar]
- 130.Easton P., Miles R., Monkman K. Florida State University; Tallahassee, Florida: 2002. Final report on the evaluation of the Tostan/IEP village empowerment program pilot project in the Republic of Mali. [Google Scholar]
- 131.Ouoba D., Congo Z., Diop N.J. Population Council, Frontiers in Reproductive Health; Washington, DC: 2004. Experience from a community based education program in Burkina Faso the Tostan Program; p. 62. [Google Scholar]
- 132.Monkman K., Miles R., Easton P. The transformatory potential of a village empowerment program: The Tostan replication in Mali. Womens Studies International Forum. 2007;30:451–464. [Google Scholar]
- 133.Asekun-Olarinmoye E.O., Amusan O.A. The impact of health education on attitudes towards female genital mutilation (FGM) in a rural Nigerian community. Eur J Contracept Reprod Health Care. 2008;13:289–297. doi: 10.1080/13625180802075174. [DOI] [PubMed] [Google Scholar]
- 134.Ekwueme O.C., Ezegwui H.U., Ezeoke U. Dispelling the myths and beliefs toward female genital cutting of woman assessing general outpatient services at a tertiary health institution in Enugu State, Nigeria. East Afr J Public Health. 2010;7:64–67. doi: 10.4314/eajph.v7i1.64684. [DOI] [PubMed] [Google Scholar]
- 135.Hassanin I.M., Shaaban O.M. Impact of the complete ban on female genital cutting on the attitude of educated women from Upper Egypt toward the practice. Int J Gynaecol Obstet. 2013;120:275–278. doi: 10.1016/j.ijgo.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 136.Chin H.B., Sipe T.A., Elder R. The effectiveness of group-based comprehensive risk-reduction and abstinence education interventions to prevent or reduce the risk of adolescent pregnancy, human immunodeficiency virus, and sexually transmitted infections: Two systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;42:272–294. doi: 10.1016/j.amepre.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 137.McQueston K., Silverman R., Glassman A. Center for Global Development Working Paper; Washington, DC: 2012. Adolescent fertility in low-and middle-income countries: Effects and solutions; p. 295. [Google Scholar]
- 138.Widman L., Choukas-Bradley S., Noar S.M. Parent-adolescent sexual communication and adolescent safer sex behavior: A meta-analysis. JAMA Pediatr. 2015;170:52–61. doi: 10.1001/jamapediatrics.2015.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.United Nations Fund for Population Activities. United Nations International Children's Emergency Fund . 2013. UNFPA-UNICEF joint programme on female genital mutilation cutting: Accelerating change.http://www.unfpa.org/sites/default/files/pub-pdf/Joint%20Programme%20on%20FGMC%20Summary%20Report.pdf Available at: Accessed November 16, 2015. [Google Scholar]
- 140.World Health Organization/London School of Hygiene and Tropical Medicine . World Health Organization; Geneva: 2010. Preventing intimate partner and sexual violence against women: Taking action and generating evidence. [Google Scholar]