Abstract
Objective
To assess trends in injecting and non-injecting drug use after implementation of large-scale syringe exchange in New York City. The belief that implementation of syringe exchange will lead to increased drug injecting has been a persistent argument against syringe exchange.
Methods
Administrative data on route of administration for primary drug of abuse among patients entering the Beth Israel methadone maintenance program from 1995 – 2007. Approximately 2000 patients enter the program each year.
Results
During and after the period of large scale implementation of syringe exchange, the numbers of methadone program entrants reporting injecting drug use decreased while the numbers of entrants reporting intranasal drug use increased (p < .001).
Conclusion
While assessing possible effects of syringe exchange on trends in injecting drug use is inherently difficult, this may be the strongest data collected to date showing a lack of increase in drug injecting following implementation of syringe exchange.
Keywords: Syringe exchange, injecting drug use, intranasal drug use
Introduction
HIV is spreading rapidly among injecting drug users (IDUs) in many parts of Eastern Europe and Asia [1]. Syringe exchange programs are considered to be one of the most effective methods of reducing HIV transmission among IDUs [2], but remain controversial in many countries. The argument that implementing syringe exchange programs will reduce the threat of HIV/AIDS and then lead to increases in injecting drug use has been one of the most persistent and powerful rationales for opposing syringe exchange [3, 4]. While we know of no evidence that supports this potential causal chain of events, it is certainly difficult to study these potential relationships with any methodological rigor. It is particularly difficult to study this potential chain in areas where syringe exchange was implemented when HIV prevalence was quite low among injecting drug users (IDUs). In such areas, HIV prevalence typically stays low among IDUs [5], and the threat of widespread HIV/AIDS is at least partly hypothetical. Determining the consequences of the removal of a threat that is partly hypothetical would be extremely difficult. This would require making assumptions about the effects of the HIV/AIDS threat if it were to actually develop, and then further assumptions about the effects of reducing the threat through implementation of syringe exchange programs.
There have been several previous studies showing no increase in drug injecting following implementation of syringe exchange in areas with moderate to high HIV prevalence (and thus a very real threat of widespread HIV/AIDS), e.g., [6, 7, 8]. These studies were conducted relatively soon (several years) after implementation of syringe exchange, however, so that it is not clear whether the exchanges had been implemented for a sufficient time to have an effect on the frequency of drug injecting. One would not expect an instantaneous effect, rather potential injectors would need to be convinced that the exchange is operating on a sufficiently large scale that they would have very easy access to sterile syringes, and thus could inject drugs without fear of HIV/AIDS. Thus, long time periods after implementation of syringe exchange need to be considered to examine whether an increase in injecting might occur.
In this brief report, we examine the temporal associations of 1. Large-scale implementation of syringe exchange programs for IDUs in New York City, 2. Reduction in the threat of HIV/AIDS, and 3. Patterns of injecting and non-injecting heroin use among persons entering methadone maintenance treatment. We believe that this data provides the strongest test to date of whether implementation of syringe exchange leads to an increase in injecting drug use.
HIV and AIDS among IDUs in New York City
With over 63,000 cases of AIDS among IDUs [9], New York City has experienced the world’s largest IDU HIV epidemic. HIV entered the IDU population in the mid-1970s, spread rapidly during the late 1970s, and then stabilized at over 50% prevalence during the 1980s [5]. IDUs were well aware of the threat of HIV/AIDS and were increasing their use of clean needles by the early 1980s [10]. One particularly interesting response to the threat of HIV/AIDS was the emergence of intranasal heroin use as a partial replacement for injecting heroin [11, 12]. Intranasal users including both persons who had never injected heroin and persons who had transitioned from injecting to intranasal use.
Large-scale syringe exchange for IDUs in New York
During the late 1980s and early 1990s, there was a pilot syringe exchange operated by the Department of Health and a number of modest-scale “underground” exchanges in the city. Large-scale implementation of syringe exchange programs began in late 1992, when the State Health Department formally approved and funded large-scale syringe exchange programming. From 1992 to 2002, the annual number of syringes exchanged increased from 250,000 to 3,000,000 [13] and possession of needles and syringes obtained from an exchange was no longer a criminal offense.
Large-scale syringe exchange and HIV among IDUs
The large-scale implementation of syringe exchange was followed by a substantial reduction in HIV incidence among IDUs in the city, from 4/100 person-years in 1990–93 to 1/100 person-years in 1998–2002 [13]. The relationship between the number of syringes exchanged per year and HIV incidence among IDUs was highly significant, r = .99, p < .001.
Methods
Beginning in 1994, the Beth Israel methadone maintenance program implemented a new computerized intake data system that captured the current (past 30 days) “usual” route of administration for the primary drug of abuse among entrants to the program. The methadone maintenance program is quite large, with an average of approximately 7000 patients at any point over this time period and an average of approximately 2000 new admissions per year. Addiction to an opioid drug is an eligibility requirement for program entry. These admissions include both persons who are new to methadone treatment and persons with previous experience in methadone treatment.
Results
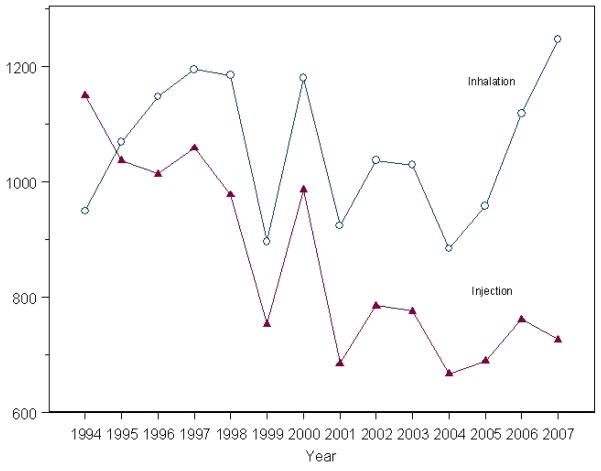
Figure 1 shows the numbers of new methadone program entrants reporting injecting and intranasal use as their route of drug administration. After 1995, the numbers of new admissions with inhalation as their primary route of drug administration was greater than the number with injecting as their primary route of drug administration. The difference in entrants reporting intranasal versus injecting administration actually increased over time (p<0.001 by Cochran-Armitage test). Approximately half of the intranasal heroin users are persons who have never injected and half are persons who previously injected but have transitioned to intranasal use [14].
Figure 1.
Number of MMTP admissions over time by route of administration (inhalation vs. injection)
Discussion
The data reported here are observational, so that care is needed in making causal (or lack of causation) inferences. There are undoubtedly multiple factors related to the large numbers of non-injecting heroin users in New York during this timey. As noted below, we believe that the most important factor was the relative high quality/low cost of street heroin during this time period. The data are from entrants to a methadone maintenance program, however, they are consistent with data from entrants to a large detoxification program and from respondent driven sampling of community IDUs in New York [14, 15].
The data in Figure 1 are clearly inconsistent with the hypothesis that implementation of large-scale syringe exchange and reduction in the threat of HIV/AIDS will lead to a substantial increase in drug injecting. During the same period in which syringe exchange programs were expanding greatly—from 250,000 syringes exchanged per year in 1993 to 3,000,000 syringes exchanged per year in 2002—the ratio of injecting to intransal heroin decreased. If removal of the threat of HIV/AIDS causes increased drug injecting, then one would have expected the percentage of injectors to have increased.
The data also raise the more interesting question of why intranasal heroin use persisted despite syringe exchange and the reduction in the threat of HIV/AIDS. First, the quality of street heroin in the city is sufficient that intranasal use will produce potent drug effects. Interviews with former injectors (persons who previously injected heroin but transitioned to intranasal use) suggest multiple reasons for preferring intranasal use, including not only avoiding AIDS, but avoiding other health problems, maintaining positive social relationships, maintaining a positive self-image as a non-injector, and preferring the more “mellow” high associated with intranasal use [14].
A final implication of the data in Figure 1 is a caution against making public policy based on simplified stereotypes of psychoactive drug users: that they are interested in only the most intense drug highs (from injecting), that a fear of AIDS alone determines their choice of the route of drug administration, and that they are not at all concerned about multiple health issues or their social relationships. If public policy is going to successfully address the many individual and social problems associated with psychoactive drug use, then it will be necessary to base policy on the best available scientific evidence, rather than upon common stereotypes of drug users.
Acknowledgments
This research was supported by grants DA 03574 from the US National Institutes of Health.
Footnotes
There are no conflicts of interest.
References
- 1.Mathers B, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 2.Wodak A, McLeod L. The role of harm reduction in controlling HIV among injecting drug users. AIDS. 2008;22:S81–S92. doi: 10.1097/01.aids.0000327439.20914.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Committee on the Prevention of HIV Infection among Injecting Drug Users in High Risk Countries. Preventing HIV Infection among Injecting Drug Users in High Risk Countries: an Assessment of the Evidence. Washington: Institute of Medicine; 2006. [Google Scholar]
- 4.Normand J, Vlahov D, Moses LE. Preventing HIV Transmission: The Role of Sterile Needles and Bleach. Washington, D.C: National Academy Press/National Research Council/Institute of Medicine; 1995. [PubMed] [Google Scholar]
- 5.Des Jarlais DC, Hagan H, Friedman SR, et al. Maintaining low HIV seroprevalence in populations of injecting drug users. JAMA. 1995;274:1226–1231. doi: 10.1001/jama.274.15.1226. [DOI] [PubMed] [Google Scholar]
- 6.Des Jarlais DC, Friedman SR, Sotheran JL, et al. Continuity and Change Within an HIV Epidemic: Injecting Drug Users in New York City, 1984 Through 1992. JAMA. 1994;271:121–127. [PubMed] [Google Scholar]
- 7.Guydish J, Bucardo J, Young M, et al. Evaluating Needle Exchange: Are There Negative Effects? AIDS. 1993;7:871–876. [PubMed] [Google Scholar]
- 8.Watters JK, Estilo MJ, Clark GL, Lorvick J. Syringe and needle exchange as HIV/AIDS prevention for injection drug users. JAMA. 1994;271:115–120. [PubMed] [Google Scholar]
- 9.Li W, Kennedy J, Kelley D, et al. Summary of Vital Statistics 2007: The City of New York. New York: New York City Department of Health and Mental Hygiene, Statistical Analysis and Reporting Unit and Research and Surveillance Unit of the Bureau of Vital Statistics; 2008. pp. 1–94. [Google Scholar]
- 10.Des Jarlais DC, Hopkins W. “Free” needles for intravenous drug users at risk for AIDS: current developments in New York City. N Engl J Med. 1985;313:1476. doi: 10.1056/NEJM198512053132311. [DOI] [PubMed] [Google Scholar]
- 11.Casriel C, Des Jarlais DC, Rodriguez R, et al. Working with heroin sniffers: Clinical issues in preventing drug injection. J Subst Abuse Treat. 1990;7:1–10. doi: 10.1016/0740-5472(90)90031-k. [DOI] [PubMed] [Google Scholar]
- 12.Casriel C, Rockwell R, Stepherson B. Heroin sniffers: between two worlds. J Psychoactive Drugs. 1988;20:437–440. doi: 10.1080/02791072.1988.10472513. [DOI] [PubMed] [Google Scholar]
- 13.Des Jarlais DC, Perlis T, Arasteh K, et al. HIV incidence among injection drug users in New York City, 1990 to 2002: use of serologic test algorithm to assess expansion of HIV prevention services. Am J Public Health. 2005;95:1439–1444. doi: 10.2105/AJPH.2003.036517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Des Jarlais DC, Perlis T, Arasteh K, et al. The transition from injection to non-injection drug use: long-term outcomes among heroin and cocaine users in New York City. Addiction. 2007;10:778–785. doi: 10.1111/j.1360-0443.2007.01764.x. [DOI] [PubMed] [Google Scholar]
- 15.Des Jarlais DC, Perlis T, Arasteh K, et al. Convergence of HIV seroprevalence among injecting and non-injecting drug users in New York City: A new stage in a very large HIV epidemic. AIDS. 2008;21:231–235. doi: 10.1097/QAD.0b013e3280114a15. [DOI] [PubMed] [Google Scholar]