Abstract
Though researchers have attended to disorganized attachment in infants and children, they have infrequently focused on the character of disorganized attachment in adults. In this study, we aimed to identify clusters of participants based on attachment levels and styles, seeking to better delineate severity and stylistic differences in disorganized attachment than has been previously articulated. We used a new assessment approach focused on a hierarchy of attachment organization, including secure, insecure (dismissive and preoccupied), rigid-controlling (hostile control and compulsive caregiving) and disorganized (contradictory, impoverished and unresolved) levels of attachment. Clinical evaluators used information from diagnostic and attachment-based interviews to rate participants on each of these aspects of attachment. Latent class analysis revealed a 4-class solution, including a secure (n = 33), insecure (n = 110) and two disorganized classes. One disorganized class (disorganized-oscillating) was characterized by elevations on contradictory and preoccupied styles (n = 77) and another (disorganized-impoverished) showed elevations on impoverished and dismissive styles (n = 53). The disorganized-oscillating class exhibited elevated PD severity and general symptom severity, BPD, histrionic and antisocial dimensional scores, and the most severe identity disturbance compared to the other classes. The impoverished-dismissive class exhibited the highest avoidant and schizoid PD dimensional scores of the classes, and higher PD severity compared to the insecure and secure classes. These results highlight the possibility of identifying distinct classes of attachment organization, differentiated both by aspects of severity and interpersonal style. They also shed light on the manifestation of attachment disorganization in adults.
Keywords: disorganized attachment, latent profile analysis, borderline personality disorder, social cognition, interpersonal functioning
In adults, attachment disorganization is believed to represent a severe disturbance in threat responding (Cassidy & Mohr, 2001), social cognition and identity development (Fonagy, Gergely, Jurist, & Target, 2002), and likely confers risk for personality disorders (Nakash-Eisikovits, Dutra, & Westen, 2002). However, the construct of disorganized attachment has remained amorphous in adults, and as a consequence is lacking somewhat in utility. Though disorganized attachment is clearly a designation of severity of attachment problems, the construct tends not to indicate style of difficulties. We sought to delineate whether, in addition to an indicator of severity of attachment disturbance, attachment disorganization may also cluster around elements of attachment style. We hypothesized that using latent class analysis (LCA)1 with continuous, clinician rated measures, we would find evidence for a predominantly preoccupied style of disorganized attachment, as well as a dismissive style of disorganization. In addition, we sought to provide empirical evidence that attachment disorganization is linked to greater mental health severity, social cognitive difficulties, poorer interpersonal functioning and increased incidence of hostility. These latter aspects of disorganized attachment have been frequently hypothesized, but have not been well-studied empirically. A finer-grained understanding of attachment disorganization is needed because differences in styles of disorganization are likely to be associated with specific sets of difficulties with regard to self and others, and, therefore different approaches to treatment.
Disorganized Attachment in Children
Attaining attachment security with a sensitive, responsive caregiver is optimal for mental health (Mikulincer & Shaver, 2007). However, in the face of insensitive parenting, toddlers can adopt insecure attachment styles: less-than-ideal, but still coherent strategies for maintaining proximity. For instance, anxious-avoidant children are thought to deactivate the attachment system, resulting in decreased expression of needs and distress in response to a parent who is overwhelmed by, or rejecting of attachment bids. Anxious-ambivalent children, on the other hand, are thought to hyperactivate the attachment system in response to an unpredictable, negligent caregiver, in a bid to maintain the caregiver's attention and help. Such children are likely to present as needy, readily express distress and wishes to be habitually close to caregivers. Though such secondary strategies have effects on later social functioning and mental health (Waters, Merrick, Treboux, Crowell, & Albersheim, 1978), they are believed to be coherent strategies, as they reflect an adaptive response within the infant-caregiver context, and allow maintenance of proximity in response to stress (Main, Kaplan, & Cassidy, 1985). Among children coded as disorganized, such coherence is not evident (Lyons-Ruth & Jacobvitz, 1999). The defining feature of disorganized attachment is the absence of a coherent strategy for interacting with and responding to a caregiver in times of stress (Main & Solomon, 1990). Within Ainsworth's classification system, these children were originally coded as “unclassifiable”; they exhibited bizarre, contradictory approach/withdrawal behaviors, confusion, and/or disorientation and fear regarding their parent.
Although the expression of disorganized attachment in infants and toddlers may be idiosyncratic by definition, the literature contains two major themes of disorganization: highly affective states-of-mind coupled with difficult to understand and contradictory behaviors, and low affective/disengaged states-of-mind coupled with extreme inhibited or dissociated behavior (Lyons-Ruth & Jacobvitz, 1999; Lyons-Ruth, Yellin, Melnick, & Atwood, 2005; Main & Solomon, 1986; Solomon & George, 2011; van Ijzendoorn, Schuengel, & Bakermans-Kranenburg, 1999). More affective, contradictory behaviors include simultaneous or rapidly oscillating approach and withdrawal behaviors, out-of-context anger, or aggression with no apparent trigger (Lyons-Ruth & Jacobvitz, 1999; Obsuth, Hennighausen, Brumariu, & Lyons-Ruth, 2014; Solomon & George, 2011). In terms of more low-affect/disengaged behaviors, Main and Solomon (1986, 1990) noted that some children responded to maternal reunion with inhibited activity, stilling, freezing, “disorganized” wandering, or apparent “falling asleep”, yet interacted with strangers or other family members with casual, friendly behavior.
While some toddlers classified as disorganized remain disorganized through childhood, others will develop extreme, rigid attachment patterns (what we refer to as excessively rigid structure) characterized by control and role reversal with parents (Obsuth et al., 2014). Lyons-Ruth and colleagues (Lyons-Ruth & Jacobvitz, 1999; Obsuth et al., 2014) have described controlling-punitive and controlling-caregiving behaviors, and documented these patterns in both children and adolescents. Controlling-punitive behavior is manifest by children who seek to control their parent through mean, defiant, or humiliating behavior. Controlling-caregiving behavior is manifest by children who attempt to “parent” their caregiver by guiding the caregiver, giving emotional support or providing encouragement. Both types have been linked to poor mental health outcomes (Greenberg, Speltz, & Deklyen, 1993; Lyons-Ruth, 1996).
Disorganized attachment in adulthood
Most of the research on attachment disorganization in adults has focused on discerning the prevalence of attachment disorganization in healthy and clinical populations (Levy, 2005), or characterizing disorganized caregiving in infant-caregiver dyads (Lyons-Ruth, Alpern, & Repacholi, 1993). The most commonly used indicator of disorganized attachment in adults is the Adult Attachment Interview code “Unresolved state of mind with respect to loss or trauma”, or “U”. This classification, based on narratives regarding specific loss or trauma experiences, is thought to capture a lack of full integration of a trauma or loss into consciousness. A number of studies have found a relationship between disorganized attachment in childhood and adult U (see van Ijzendoorn et al., 1999 for review). However, researchers (Lyons-Ruth, et al., 2005) have criticized the U classification on methodological grounds. It is only coded if participants report a trauma and evidence lapses in communication during discussion of trauma or loss. This coding rule likely explains the low rate of U classifications in populations with severe attachment disturbances (Holtzworth-Munroe, Stuart, & Hutchinson, 1997; van IJzendoorn et al., 1997).
Disorganized attachment and personality disorders
Increasingly, personality disorders (PDs) have been defined as severe difficulties related to self and other (Skodol et al., 2011). Attachment insecurity and disorganized attachment are thought to provide a diathesis to such problems (Drew Westen, Nakash, Thomas, & Bradley, 2006). Main and Hesse (1990) proposed that disorganized attachment would be associated with severe psychopathology in adulthood. Research has often shown that PDs are associated with disorganized attachment, though they are also strongly related to additional insecure attachment styles (Brennan & Shaver, 1998; Nakash-Eisikovits et al., 2002; D Westen et al., 1992). Many theorists have observed the similarities between the contradictory and disoriented behaviors of disorganized infants and the severe attachment disturbances evidenced by individuals with personality disorders (PDs), and particularly borderline personality disorder (Fonagy et al., 1996; Gunderson, 1996; Melges & Swartz, 1989; Meyer & Pilkonis, 2005). A large research base suggests individuals with BPD are more likely to exhibit preoccupied or unresolved attachment (see Levy, 2005 for review). Preoccupied attachment captures some of the features of the disorder, particularly concerns about rejection, needs to keep close others proximal, and desires for intense intimacy, coupled with frequent dissatisfaction in relationships. However, the extreme severity of attachment disturbance evident in BPD is not fully captured by preoccupied attachment (Choi-Kain, Fitzmaurice, Zanarini, Laverdière, & Gunderson, 2009). In addition, other attachment-related features of BPD, such as extreme oscillation in representations of self and others and identity diffusion, are not part of the preoccupied attachment construct. Another social cognitive disturbance not captured by typical preoccupied attachment, but indicated by disorganized attachment are problems with mentalization (Cassidy & Mohr, 2001), which refers to the ability to understand the behavior of others in terms of intentional mental states (Fonagy et al., 2002). Insecure attachment styles, including preoccupied attachment, are part of a description of normal development (Ainsworth, Blehar, Waters, & Wall, 1978). This limits the utility of a connection between preoccupied attachment and BPD, for instance, because this same attachment style is often used to characterize healthy individuals.
Levy and Blatt (1999) offered an approach to capture differences in severity of attachment disturbance within insecure attachment styles. They suggested that even people with severe personality pathology tend to struggle with either problems of interpersonal relatedness (preoccupied attachment) and/or problems related to self-definition (dismissive attachment). However, they argued, people exhibit more or less adaptive forms of preoccupied and dismissive attachment, depending on the content and structure (e.g., differentiation between self and other; integration of positive and negative aspects of self and others) of internal working models of self and others. Within this system, a more severe preoccupied attachment disturbance, for instance, would exhibit a character resembling a preoccupied style of disorganization. Individuals with this style would exhibit unintegrated working models and poor differentiation between self and others. Likewise, individuals with more severe dismissive attachment disturbance would resemble others with problems related to self-definition (e.g., needing to see oneself as superior, self-sufficient, and seeing dependency needs as weak). However, more severe expressions of dismissive attachment would be marked by impaired sense of self, more negative representations of others, and difficulty integrating positive and negative aspects of close others.
Similarly, Gunderson & Lyons-Ruth (2008) have argued that individuals with BPD evidence a disorganized-ambivalent attachment style, characterized by extreme need for relational closeness, intense fear of rejection and contradictory mental states and behaviors. Lyons-Ruth and colleagues (2005) have described a hostile-helpless attachment style, characterized by pervasively contradictory or unintegrated emotional evaluations of a caregiver, often also exhibiting unexamined identification with a hostile caregiver. Both of these descriptions of disorganized attachment in adults are promising, yet only one study has examined the presence of the hostile-helpless (H-H) style. Lyons-Ruth and colleagues (2007) found that all 12 participants diagnosed with BPD were also classified as (H-H), though 6 of 11 dysthymic participants also evidenced this attachment style. The study utilized too small a sample size to make firm conclusions, however. Moreover, no study has examined the similar concept of disorganized-ambivalent attachment.
Current Study
For the present study, we derived descriptions of a number of features of attachment disorganization (contradictory, impoverished, unresolved, controlling-caregiver, hostile-control) from the literature and asked evaluators to rate participants on these and more organized styles of attachment (See Table 1). Using a person-centered analytic approach, LCA for continuous predictors, we sought to identify classes of individuals based on patterns of attachment styles derived from clinician ratings of attachment. Raters were based on the participant's narrative regarding current and past attachment relationships. From theory, we expected to find evidence for differing levels of attachment organization. Drawing from Levy and Blatt's (1999) descriptions and others (e.g., Gunderson & Lyons-Ruth, 2008), we hypothesized more severe/less organized presentations of preoccupied and dismissive attachment would emerge from our latent class analysis, as well as more organized classes. We planned to evaluate differences among classes in PD symptoms, severity of psychopathology, interpersonal and work functioning, and identity and social cognitive functioning. These variables were evaluated as external variables, estimated outside of LCA. Informed by previous theory and research on disorganized attachment, we expected disorganized classes would be differentiated by greater PD symptoms, greater psychopathology, more difficulties in interpersonal and work functioning, as well greater difficulties with identity and mentalization. Identity disturbance and mentalization were included because attachment disorganization is thought to inhibit development of a stable sense of self and disturb social cognition (Beeney et al., 2015; Fonagy et al., 2002).
Table 1.
Levels of Attachment Organization.
| Flexible and balanced structure | |
| Secure attachment | Participant has meaningful relationships with perceived risk to autonomy; can be with and apart from others; enjoys being part of close relationships; is able to depend on others when appropriate and have others depend on her/him. |
| Functional but not optimal structure | |
| Preoccupied attachment | Participant demonstrates elevated concern regarding close relationships; emphasizes distress, vulnerability and helplessness with close others; requires reassurance from others; is chronically dissatisfied with care in relationships; often engages in voluminous discussion of attachment relationships and issues. |
| Dismissive attachment | Participant focuses on personal definition, self-reliance, and/or superiority; has idealized representations of attachment figures without supporting examples and/or dismisses attachment relationships as unimportant; persistent inability to recall details of attachment relationships. |
| Excessively rigid structure | |
| Hostile, controlling patterns of relationships | Participant evidences consistent pattern of controlling behavior usually accompanied with anger; emotion is often constricted except for anger; takes perfectionistic attitude toward self and others. |
| Compulsive care-giving | Participant persistently ignores own needs in favor of focusing on needs of others; becomes involved with romantic partners who are needy and vulnerable; may express resentment about unequal care in relationships with others. |
| Disorganization and lack of structure | |
| Generalized incoherence (type 1) | High intensity/high affect with multiple, shifting, mood-dependent states-of-mind; narrative contains multiple, unmonitored contradictions; may show evidence of oscillating between extremes of attachment styles; may oscillate between hostility and helplessness in describing caregivers. |
| Generalized incoherence (type 2) | Low intensity/low affect with diffuse, vague, confusing or inadequate states-of-mind; has not struggled with or has prematurely foreclosed on career, romantic relationships, and/or social relationships; lack of concern about impoverished ideas of self or others; has not pondered minds of self or others. |
| Unresolved states-of-mind regarding specific trauma, loss, of other events | Has experienced specific traumatic event (including physical or sexual abuse) or loss and demonstrates lapses in narrative including long pauses, intrusions in speech, or extreme tension and avoidance when discussing loss or trauma. |
Method
Participants and Recruitment Procedures
The study sample (N = 272) was comprised of individuals from psychiatric outpatient clinics and the community across two different research protocols. In the first sample, participants were selected from one of three groups: individuals with BPD, those with another PD, or those without a PD. In the second, we recruited participants according to 3 strata: 0-2, 3-4, and 5 or more symptoms, based on the McLean Screening Instrument (MSI; Zanarini et al., 2003). For simplicity, hereafter, we treat these two samples as one. Psychiatric patients (n = 197; 72.4%) were solicited from general adult outpatient psychiatric clinics and were active in treatment at the time of participation in this study. The community sample (n = 75; 27.6%) was recruited by telephone through the use of a random digit dialing (RDD) method coordinated by the University Center for Social and Urban Research at the University of Pittsburgh. Participants with psychotic disorders, organic mental disorders, severe developmental disability, and major medical illnesses that influence the central nervous system were excluded. Overall, recruitment resulted in a sample in which 81% of participants had a current Axis I disorder, and 66% of the sample was diagnosed with an Axis II disorder.
Participants were between the ages of 21 and 61 (M = 41.5; SD = 11.04) and 187 were female (69.0%). One-hundred eighty participants (66.2%) identified as White, 82 (30.1%) as Black, 8 (2.9%) as more than one race, and 2 (0.7%) as Asian. Seven participants (2.6%) identified their ethnicity as Hispanic. A large majority of the sample obtained education beyond high school (n = 207; 76.1% with at least some vocational or college training), but the majority of the sample was unemployed/receiving disability (n = 163, 59.9%).
Assessment Procedures
All participants were interviewed by trained research staff with a minimum of a master's degree in social work or clinical psychology and at least five years of assessment/clinical experience. Diagnostic assessments consisted of three or more sessions, which included assessment of Axis I and II disorders using the Structured Clinical Interview for DSM Disorders (First, Spitzer, & Williams, 1997) and the Structured Interview for DSM-IV Personality (Pfohl, Blum, & Zimmerman, 1997). In a subsequent interview session, a detailed social and development history was taken using the Interpersonal Relations Assessment (IRA; Heape, Pilkonis, Lambert, & Proietti, 1989). Our research team conducts case conferences for each study participant, including at least two judges, in addition to the primary clinical evaluator. The primary evaluator presents all information gathered in interview, and information gathered from clinical records and other sources. Having gathered all available information, judges will discuss the case and make consensus ratings for diagnoses and attachment (see Pilkonis, Heape, Ruddy, & Serrao, 1991, for a more thorough description of the LEAD standard approach). The University of Pittsburgh Institutional Review Board approved all study procedures, and participants provided informed, voluntary, written consent. Fifteen total cases were rated by 5 or more raters to assess reliability. Reliability was calculated for BPD and OPD diagnoses. Our group evidenced high reliability coding BPD (.80), and other personality disorders (.78).
Measures
Attachment assessment procedures
Clinical evaluators rated participants on 4 different levels of attachment, describing a hierarchy of attachment organization. Each level of attachment had 1-3 styles, totaling 8 styles as described in Table 1. Evaluators were allotted 100 points to distribute across these 8 styles in any manner they felt best captured the participant's attachment organization and style. The most organized attachment level was named “flexible and balanced structure”, with the single style of secure attachment. The next level was characterized as “functional but not optimal structure”, and consisted of typical insecure attachment styles: preoccupied and dismissive. The subsequent level was described as “excessively rigid structure” and consisted of hostile, controlling patterns of relationships and compulsive care-giving styles. “Excessively rigid structure” refers to the lack of flexibility and limited behavioral repertoire among individuals at this level, particularly in responding to stressful interpersonal situations. Individuals with elevations at this level are likely to respond to most interpersonal situations with hostile control, or compulsive caregiving, regardless of what the situation calls for. The lowest level of organization was dubbed “disorganization and lack of structure” specified by three styles: “high intensity and highly affective incoherence”, “low intensity and low affective incoherence”, and “unresolved”. Neither disorganized types, nor levels of attachment organization were mutually exclusive; evaluators could give points to all categories that were characteristic of the person.
Personality disorder symptoms
Within LEAD standard meetings, interviewers and additional judges came to agreement on consensus scores for each of the SID-P criteria. These consensus scores for SID-P criteria were used to evaluate personality disorder symptoms. Dimensional scores for each PD were calculated by summing ratings (ranging from 0 absent to 2 strongly present) of the individual criteria for each PD from the SID-P.
Work and social functioning
Evaluators also measured interpersonal functioning using the Revised Adult Personality Functioning Assessment (Hill, Harrington, Fudge, Rutter, & Pickles, 1989). The RAPFA focuses on interpersonal functioning over the previous 5 years in the domains of work, romantic relationships, and friendships. Interviewers were trained to rate each domain on a nine-point scale according to severity and pervasiveness of dysfunction. In a second consensus conference, a minimum of three judges who were different from judges in the diagnostic case conference and unaware of diagnostic status, decided on consensus ratings for each domain. The intraclass correlation coefficient (ICC) for the total RAPFA score was .84.
Violence and hostility
The Conflict Tactics Scale (CTS; Straus, Hamby, Boney-Mccoy, & Sugarman, 1996) is a measure of relationship hostility and violence. Participants were asked to report hostility and aggression over the 12-months prior to completing the measure. Participants were also asked to report separately on instances in which they were the victim or perpetrator.
Measuring aspects of social cognition
Social cognitive scales, including impoverished identity, self-other differentiation, and mentalization were derived from a previous study first using an exploratory factor and analysis followed by a confirmatory factor analysis on a large battery of measures to isolate these social cognitive dimensions (Beeney et al., 2015). Both of the identity scales were measured using self-report items, whereas the mentalization scale was derived from all clinician-rated items. Factor scores for each latent variable were extracted from the measurement model.
Analytic Approach
The first goal of the present study was to identify naturally occurring profiles of attachment among participants, using latent class analysis (LCA) with continuous observed variabless (sometimes called Latent Profile Analysis). LCA is a person-centered approach, used to cluster participants rather than variables (Hallquist & Wright, 2014). In this way, it allows us to identify latent subgroups within the data. A number of statistical indicators are used in LCA as to select between models with different numbers of classes. The Bayesian Information Criterion (BIC), and sample-size adjusted BIC have been shown to be among the most reliable indices for selecting the true model based on simulation studies (Nylund, Asparouhov, & Muthén, 2007). Identifying the correct number of classes based on the BIC is similar to examining a scree plot within factor analysis. Researchers are advised to look for breaks in the incremental improvement in fit, which along with use of theory can be used to guide decisions on the correct number of classes to model. The Lo-Mendel-Rubin (LMR) likelihood difference test is also frequently used in order to test the fit between two nested models that differ by one class. A significant LMR p-value suggests that a model fits the data significantly better than a model with one less class. When this value is non-significant for n classes, researchers are advised to return to the n-minus-1 class. Classification precision is summarized by the entropy measure, with a value closer to 1 indicating better classification.
To test class mean differences on variables purportedly related to disorganized attachment (PD symptoms, work and interpersonal functioning, hostility and social cognitive difficulties), we evaluated differences in class-specific means by running a Wald test, using the auxiliary variable (e) function in Mplus (Muthén & Muthén, 2013). This approach provides a test of the equality of means of each criterion across the total number of latent groups. In addition, the approach allows for these auxiliary variables to be omitted from the LCA model, meaning measurement of the LCA is independent of the external variables. We chose this, rather than the 3-Step approach, which uses multinomial logistic regression, for ease in interpretability (Marsh, Lüdtke, Trautwein, & Morin, 2009). Multinomial logistic regression uses a reference group for comparison to other groups on each variable, meaning interpretation is relative to whichever reference group is selected. In addition, variables included in the model in addition to the clustering variables in the 3-step process impact measurement of the clusters themselves. Because our major aims were to define natural clusters of attachment profiles, and to compare group-differences on additional variables, we found the above approach most appropriate.
Results
Correlations between attachment styles, PD severity and interpersonal functioning are presented in table 2. Prior to running the LCA, we chose to omit the compulsive caregiving attachment style, given this variable had an extremely low base rate and excessive skew (of 272 participants only 80 were scored higher than 0, with majority of these participants scoring 20 or fewer points out of 100), and appeared to capture something more akin to altruism or empathy, rather than a rigid personality style (e.g., positive associations with attachment security and negative associations with PD severity). Therefore, this variable was excluded from further analyses. We ran the LCA in Mplus (Muthén & Muthén, 2013) on the 7 remaining attachment categories. One- through six-class models were fitted to the data (See table 3). Although both the BIC and adjusted BIC continued to improve with the addition of each class up to 6, the LMR was non-significant when comparing the 5-class solution with the 4-class solution, suggesting that a 4-class solution may be optimal. The 5-class solution was also less interpretable than the 4-class solution, simply breaking up the secure class into two largely similar and insufficiently small classes (n=8 and 25). The high entropy value (.93) suggested a high degree of class differentiation, as did the average posterior latent class assignment probabilities for the 4-class model, which ranged between .93 and .98 for most likely class membership and .00 to .04 for off-diagonal probabilities. Class counts for profiles ranged from 33-110 participants.
Table 2.
Correlations Between Evaluator Ratings of Attachment, PD Severity and Interpersonal Domains
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Type 1 | – | |||||||||||
| 2. Type 2 | −.22** | – | ||||||||||
| 3. Unresolved | .09 | −.02 | – | |||||||||
| 4. Hostile Control | .08 | −.30** | −.19* | – | ||||||||
| 5. Preoccupied | .13* | −.24** | −.01 | −.12 | – | |||||||
| 6. Dismissive | −.27** | .10 | −.17* | .02 | −.44** | – | ||||||
| 7. Secure | −.40** | −.28** | −.28** | −.15* | −.17* | −.18* | – | |||||
| 8. PD Severity | .50** | .25** | .25** | .14* | .16* | .10 | −.86** | – | ||||
| 9. RAPFA Work | .32** | .32** | .20* | .00 | .00 | .08 | −.55** | .65** | – | |||
| 10. RAPFA Relationships | .20** | .24** | .19* | .01 | .04 | .11 | −.59** | .62** | .50** | – | ||
| 11. RAPFA Family | .25** | .20** | .18* | .01 | .07 | .06 | −.52** | .58** | .50** | .55** | – | |
| Mean | 9.94 | 10.75 | 9.89 | 12.35 | 16.62 | 21.34 | 12.37 | 63.13 | 6.02 | 7.05 | 5.79 | |
| SD | 14.63 | 17.57 | 13.06 | 13.74 | 17.09 | 18.32 | 19.62 | 13.05 | 1.99 | 1.79 | 1.90 | |
Note:
p < .05
p < .001.
Measures 1-9 are evaluator ratings of attachment styles. PD severity is evaluator rating of axis II severity score. RAPFA = Revised adult personality functioning assessment.
Table 3.
Model Fit Indices for 1- to 6-Class Solutions.
| Model | K | LL | BIC | Adj. BIC | LMR p | Entropy |
|---|---|---|---|---|---|---|
| 1 Class | 14 | −7999.23 | 16062.84 | 16118.55 | -- | 0.94 |
| 2 Class | 22 | −7868.15 | 15859.25 | 15789.88 | 0.003 | 0.93 |
| 3 Class | 30 | −7758.85 | 15677.79 | 15582.67 | 0.002 | 0.93 |
| 4 Class | 32 | −7658.85 | 15530.71 | 15410.22 | <.001 | 0.93 |
| 5 Class | 46 | −7587.88 | 15453.63 | 15307.78 | 0.054 | 0.93 |
| 6 Class | 54 | −7555.57 | 15413.84 | 15242.63 | 0.51 | 0.93 |
Note: K = number of free parameters; LL = Loglikelihood; BIC = Bayesian Information Criteria; Adj. BIC = Adjusted BIC; LMR p = p-value of the Lo-Mendell-Rubin ratio test.
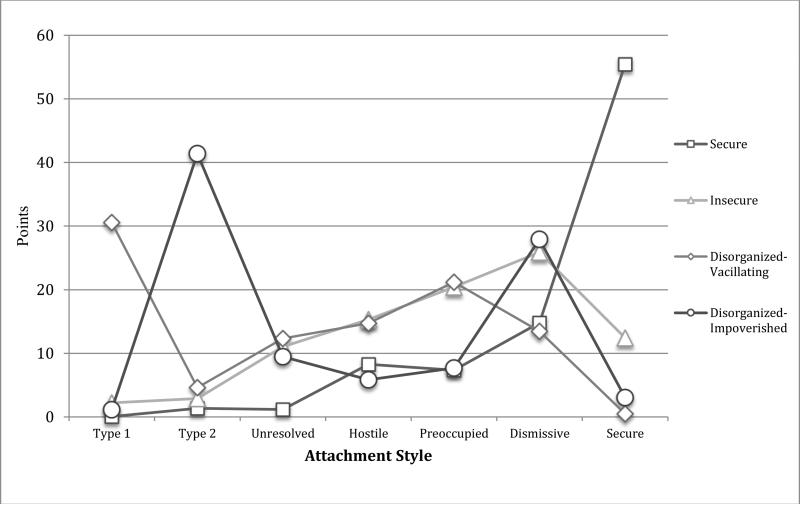
We summarize the identified latent classes in Figure 1. The Secure (12%; n= 33) class had a high elevation on attachment security and a mild elevation on dismissive attachment within an otherwise flat profile. The Insecure (40%; n=110) class had elevations on dismissive and preoccupied attachment, low attachment disorganization, and mild elevations on unresolved, hostile-controlling and secure attachment styles. Two distinct disorganized profiles were identified. The disorganized-oscillating (28%; n=77) class had a peak for Type 1 (mood dependent) disorganization and a smaller preoccupied elevation, no elevations for Type 2 (impoverished) or secure attachment, and mild elevations for other attachment styles. The Disorganized-Impoverished (19%; n=52) class exhibited a peak on Type 2 disorganization, an elevation on dismissive attachment and low scores on all other attachment styles. These results supported our hypothesis that we would identify two types of disorganized attachment and generally supported our hypothesis that we would identify classes at differing levels of attachment organization, though we did not identify a class differentiated by a greater rigid-controlling organization.
Figure 1.
Latent attachment profiles.
Analyses of mean differences on variables external to the LCA supported the hypothesis that disorganized classes would be characterized by greater impairment in a number of domains (See table 4). The disorganized-oscillating class evidenced the greatest PD severity, followed by the disorganized-impoverished group. Both of these classes evidenced poorer work, relationship and family functioning compared to the organized classes. In addition, the disorganized-oscillating class evidenced the most severe identity disturbance, showing the most impoverished identity of the classes and the poorest differentiation between self and others. Both disorganized classes evidenced poorer mentalization compared to the organized classes. When examining specific PD symptoms, the disorganized-oscillating class had significantly higher borderline, antisocial, and histrionic dimensional scores than all other classes. The disorganized-impoverished class had significantly higher avoidant and schizoid dimensional scores compared to all other classes. The disorganized-oscillating class showed evidence of higher levels of hostility and violence compared to all other classes.
Table 4.
Class Differences on Attachment-relevant Variables.
| Class 1 | Class 2 | Class 3 | Class 4 | Chi-Squared | |
|---|---|---|---|---|---|
|
Domain Functioning
| |||||
| PD Severity | 39.46bcd | 61.08acd | 72.96abd | 67.78abc | 292.056* |
| RAPFA Work | 3.97bcd | 5.36acd | 6.94ab | 6.97ab | 64.60* |
| RAPFA Relationships | 4.85bcd | 6.65acd | 7.89ab | 7.76ab | 55.25* |
| RAPFA Family | 3.66bcd | 5.54acd | 6.58ab | 6.44ab | 63.52* |
|
Personality Disorder Symptoms | |||||
| Borderline | 0.18bcd | 2.5ac | 8.29abd | 2.2ac | 288.74* |
| Antisocial | 0.13bcd | 0.83ac | 2.72abd | 1.13ac | 56.13* |
| Avoidant | 0.44bcd | 2.8ac | 2.3abd | 4.79abc | 41.16* |
| Paranoid | 0.13bcd | 1.05ac | 1.53ad | .86ac | 44.02* |
| Schizoid | 0.10d | 0.22d | 0.18d | 1.53abc | 18.92* |
| Schizotypal | 0.10cd | 0.14cd | 0.54ab | 0.85ab | 11.19* |
| Histrionic | 0.52bc | 1.04acd | 2.82abd | 0.57bc | 41.80* |
| Narcissistic | 0.64bc | 2.20a | 2.79ad | 1.42c | 28.21* |
| Dependent | 0.30bcd | 1.58ac | 2.33ab | 1.59a | 49.28* |
| Obsessive | 1.32b | 2.55ac | 1.50b | 2.05 | 15.92* |
|
Violence and Hostility | |||||
| CTS Hostility – Victim | 19.53bcd | 30.67ac | 45.79ab | 38.72a | 17.18* |
| CTS Hostility - Aggressor | 20.37cd | 25.52c | 44.96ab | 35.99a | 15.10* |
| CTS Assault – Victim | 1.38bd | 3.12c | 7.91ab | 6.72a | 18.12* |
| CTS Assault - Aggressor | 1.91c | 2.64c | 8.40abd | 3.91c | 11.72* |
|
Social Cognition | |||||
| Impoverished Identity | −0.61bcd | −0.112acd | 0.41abd | 0.15abc | 79.87* |
| Self-Other Differentiation | −0.57bcd | −0.16ac | 0.53abd | 0.02a | 45.07* |
| Mentalization | 1.57bcd | 0.32acd | −0.72ab | −0.80ab | 50.97* |
Note:
significantly different from Class 1
significantly different from Class 2
significantly different from class 3
significantly different from class 4
RAPFA = Revised Adult Personality Functioning Assessment; CTS = Conflict Tactics Scale.
Discussion
We sought to characterize attachment disorganization among adults by investigating patterns of attachment styles in a predominantly clinical population with high psychopathology. We found evidence for differing levels of attachment organization, separated by PD severity, work and social functioning, and identity and mentalization. At the same time, we identified two distinct classes characterized by attachment disorganization, which differed in personality difficulties and other stylistic elements. One of these classes, disorganized-oscillating, appeared to be a disorganized version of preoccupied attachment: highly affective with difficulty tracking self and others, more angry and violent, and high on cluster B symptoms, particularly BPD. The other disorganized class, disorganized-impoverished, had characteristics of a disorganized variant of dismissive attachment: low affect and impoverished identity, with poor mentalization, more avoidant PD symptoms and a significant elevation for schizoid PD symptoms. These results suggest that while attachment disorganization is related to greater psychopathology, these classes also showed evidence of stylistic differences that bear some resemblance to classic organized-insecure styles.
Our results were partially supportive of differing levels of attachment organization, yielding four distinct attachment classes, covering secure, insecure and disorganized levels of organization (See Figure 1). The disorganized-oscillating class (n = 77) exhibited a major theme of high-affect, contradictory disorganization, with a strong trait of preoccupied attachment, but also significant hostile-controlling and dismissive behavior. The disorganized-impoverished class (n = 52) was characterized by a major theme of vague, impoverished disorganization, in which dismissive attachment represented the only other significant elevation. The insecure group, the largest class (n = 110), showed almost no elevation on disorganized attachment, but was also somewhat undifferentiated in terms of a particular insecure style. Among these individuals, dismissive, preoccupied and hostile controlling, and even a mild elevation for secure attachment were the most relevant styles. Finally, the secure class was strongly secure. Contrary to hypotheses, we did not find a class predominated by a rigid-controlling level of attachment organization. One possibility is that this pattern, which has been found in children and adolescents, may diminish in adulthood. A more likely possibility is that the absence of this level of organization is sample specific. In samples concentrated with participants with narcissistic or antisocial PD, a hostile-controlling style may be more likely to emerge. In addition, we omitted controlling-caregiving from our LCA due to a low base rate. However, in a sample characterized by dependent or passive-aggressive features, this style would likely predominate.
The resemblance of these two disorganized classes to Ainsworth's insecure-organized styles suggests they may represent extreme presentations of preoccupied and dismissive attachment. In this way, our results are supportive of Levy and Blatt's (1999) proposal of different levels of severity within classic insecure styles. Related to this theoretical proposal, recent research has focused on whether PDs can be differentiated from non-PDs (through consideration of severity) and whether one PD can meaningfully be differentiated from another (through consideration of style). Hopwood and colleagues (Hopwood et al., 2011) offered data to suggest that a consideration of both severity and style are vital to PD diagnosis. The current results suggest a similar narrative, but using attachment style and severity of attachment difficulties as a starting point. Authors (Hopwood, Wright, Ansell, & Pincus, 2013; Luyten & Blatt, 2013) have argued that healthy personality development critically involves a dialectic between relatedness and self-definition, and personality dysfunction can typically be characterized by extreme difficulties within either of these realms. In the current study, individuals comprising the disorganized-oscillating class appear to primarily struggle and fixate on issues of relatedness, given elevations on preoccupied attachment, as well as difficulties differentiating between self and others. Individuals in the disorganized-impoverished class appear to struggle with a disorganized version of dismissive attachment, showing elevations on dismissive attachment, and a seemingly avoidant style of disorganization. Our data suggest that individual attachment styles, even when disorganized, tend more towards problems with self-definition or problems with interpersonal connection.
Levy and Blatt (1999) predicted that severe presentations of preoccupied or dismissive attachment would involve more global, diffuse, fragmentary and inflexible representations of self and other. Interpersonal theorists make similar predictions regarding extreme difficulties in relatedness or self-definition (Hopwood et al., 2013). They suggest extreme interpersonal problems are likely to involve dysregulation in social cognition and feelings related to self and others, as well as disorganized behavior in interpersonal situations. In addition, Bateman and Fonagy (2004) have argued that the parenting behaviors that promote insecure and disorganized attachment impede the development of identity and mentalization. Both disorganized classes evidenced greater identity and social cognitive disturbance compared to organized classes. Disorganized classes showed different patterns of disturbance in these domains. The disorganized-oscillating group reported greater impoverished identity and poorer self-other differentiation, whereas the disorganized-impoverished group reported greater impoverishment than the organized classes, and did not report poorer self-other boundaries compared to the insecure class. Greater difficulty with self-other differentiation has frequently been linked to preoccupied attachment, and has been shown to be elevated in BPD (Beeney et al., 2015). Consistent with our hypothesis, the disorganized classes exhibited less ability to understand the behavior of oneself and others in terms of intentional mental states compared to the other classes. That the disorganized-impoverished class would report less identity impoverishment compared to the disorganized-oscillating was unexpected, however. This finding may underline the severe identity disturbance experienced by those who develop a disorganized-oscillating attachment. Alternatively, it could represent a response style among each class, with the oscillating class tending to endorse high scores, and the impoverished class potentially both muting scores, and/or lacking the self-knowledge to make an accurate judgment on identity. In total, our results support attachment disorganization as signifying impairment in cognition regarding self and other.
The disorganized-oscillating class we identified clearly bears resemblance to BPD-attachment types articulated in the literature, such as Lyons-Ruth's hostile-helpless disorganization (Lyons-Ruth et al., 2005), or Gunderson and Lyons-Ruth's (2008) related construct of disorganized-ambivalence. Each of these descriptions of attachment states of mind and behavior characterize individuals who evidence rapid, unmonitored fluctuations in mental states particularly related to self and others, intense affect with regards to relationships, and high distress and misery. Thus, our results provide support for a style of disorganization associated with BPD that has been previously voiced in the literature.
The disorganized-impoverished class found in our LCA has not been as clearly articulated. Bateman & Fonagy (2004) formerly characterized individuals with BPD as having impoverished mentalization and identity. The disorganized-impoverished class, however, with a scattered profile of avoidant, BPD, obsessive and schizoid symptoms, presents a more mixed diagnostic picture. In addition, this group evidenced severe impairment in multiple domains, but with less affective intensity, anger and hostility. Rather than excessive, volatile mental states, this class evidenced extreme avoidance. Specifically, many of the participants in this class were not active in work or stable social relationships. Members of this class had difficulty describing themselves or others, even with significant encouragement. In addition to this, anecdotal reports from clinicians who interviewed disorganized-impoverished participants revealed that individuals in this class often appeared surprised by questions asking for reflection or puzzled about questions regarding themselves or others. Rather than defensive separation, idealization, or devaluation, these participants convinced the evaluator of having little curiosity about themselves or others. For many of these participants, life appeared to be organized around avoiding stress and anxiety, resulting in a strictly limited range of experience in both a physical and mental sense.
Attachment disorganization in adults was expected to be associated with significant impairment in personality functioning, and the major domains of life: work, romantic and social functioning. Both disorganized classes exhibited significantly more dysfunction in each of these domains. In fact, the disorganized-vacillating class had a mean PD severity close to the poorest quadrant of functioning, signifying profound personality dysfunction. Both disorganized classes also evidenced severe problems in work, family, and relationships. The more organized classes exhibited both statistically and clinically higher scores in each of these domains. The results underline the serious impairments associated with severe attachment disturbance.
Though unresolved attachment has been the most researched construct of adult disorganized attachment, none of our groups was differentiated by an elevation in unresolved attachment. This was unexpected, given that the sample was selected for a range of PD pathology. Our operationalization of unresolved attachment was similar to the AAI protocol, in that we considered the code only when a trauma or loss was reported, and only when participants evidenced lapses, while discussing the loss or trauma. The absence of any class in which unresolved attachment was elevated suggests that disorganized attachment commonly occurs outside of an identified trauma or loss. Though unexpected, this finding is also consistent with previous research, which failed to find high rates of unresolved attachment among apparently disorganized samples (Holtzworth-Munroe et al., 1997; van IJzendoorn et al., 1997).
From a clinical standpoint, the differentiation we found both in levels of attachment organization and stylistic differences in disorganized clusters is consequential. Clarity in terms of the level of attachment organization of a client will likely inform treatment – in the length of treatment needed, nature of difficulties and obstacles to recovery. In addition, stylistic differences among individuals with disorganized attachment will likely require different treatment approaches. Whereas the disorganized-oscillating type may respond best to the structured, containing approach that is common across most early-treatment phases for BPD, the disorganized-impoverished group may benefit most from an early focus on social integration.
Strengths and Limitations
This study included a number of strengths, including a large clinical sample, participants who were well characterized using diagnostic interviews and various attachment ratings, as well as multiple methods in the design. Using a person-centered approach also allowed us to examine patterns of attachment that cluster within people, providing a more complete characterization of within-person attachment profiles. However, it should also be noted that the approach, both in attachment assessment and examining mean differences was exploratory in nature, and should be replicated in additional samples. Though a strength of this study is the use of a thorough interview battery and case conference for making consensus-based clinical decisions, this approach also meant that clinicians made both diagnoses and attachment ratings, and consensus judges were aware of diagnosis in informing attachment ratings. Thus, knowledge of diagnosis and general severity may have biased attachment ratings. Future work could improve on the current research by having different evaluators and consensus judges for diagnostic and attachment interviews and ratings.
Conclusion
We identified three levels of attachment organization within a sample high in psychopathology. Participants clustered into a disorganized-oscillating style similar to that proposed previously in the literature, as well as less frequently discussed disorganized-impoverished class. Disorganized classes were differentiated from organized classes by PD severity, work, social and romantic functioning, identity and mentalization. These classes were also distinct from one another, particularly in terms of personality disorder symptom profiles and specific style of identity impairment reported. The study is a first attempt to more fully characterize disorganized attachment in adults, and suggests that disorganized attachment styles are related to serious functional impairment across multiple domains.
Acknowledgments
This research was supported by grants from the National Institute of Health (F32 MH102895, PI: Joseph E. Beeney, L30 MH101760, PI: Aidan G.C. Wright, and R01 MH05688, PI: Paul A. Pilkonis).
Footnotes
The authors declare no competing financial interests.
LCA with continuous indicators is sometimes referred to as latent profile analysis.
References
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Lawrence Erlbaum; Oxford, England: 1978. [Google Scholar]
- Bateman A, Fonagy P. Psychotherapy for borderline personality disorder: Mentalization-based treatment. Oxford University Press; USA: 2004. [Google Scholar]
- Beeney JE, Stepp SD, Hallquist MN, Scott LN, Wright AGC, Ellison WD, Pilkonis PA. Attachment and social cognition in borderline personality disorder: Specificity in relation to antisocial and avoidant personality disorders. Personality Disorders: Theory, Research, and Treatment. 2015;6(3):207–215. doi: 10.1037/per0000110. doi:10.1037/per0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeney J, Stepp SD, Hallquist MN, Scott LN, Wright AGC, Ellison WD, Pilkonis PA. Attachment and Social Cognition in Borderline Personality Disorder: Specificity in Relation to Antisocial and Avoidant Personality Disorders. Personality Disorders: Theory, Research, and Treatment. 2015;6(3) doi: 10.1037/per0000110. doi:10.1037/per0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan K. a, Shaver PR. Attachment styles and personality disorders: their connections to each other and to parental divorce, parental death, and perceptions of parental caregiving. Journal of Personality. 1998;66(5):835–78. doi: 10.1111/1467-6494.00034. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9802235. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Mohr JJ. Unsolvable Fear, Trauma, and Psychopathology: Theory, Research, and Clinical Considerations Related to Disorganized Attachment Across the Life Span. Clinical Psychology: Science and Practice. 2001;8(3):275–298. doi:10.1093/clipsy/8.3.275. [Google Scholar]
- Choi-Kain LW, Fitzmaurice GM, Zanarini MC, Laverdière O, Gunderson JG. The relationship between self-reported attachment styles, interpersonal dysfunction, and borderline personality disorder. The Journal of Nervous and Mental Disease. 2009;197(11):816–821. doi: 10.1097/NMD.0b013e3181bea56e. doi:10.1097/NMD.0b013e3181bea56e. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Williams JB. Structured clinical interview for DSM-IV axis I disorders SCID-I: clinician version, administration booklet. American Psychiatric Pub; 1997. [Google Scholar]
- Fonagy P, Gergely G, Jurist EL, Target M. Affect regulation, mentalization, and the development of the self. Other Press; New York: 2002. [Google Scholar]
- Fonagy P, Leigh T, Steele M, Steele H, Kennedy R, Mattoon G, Gerber A. The relation of attachment status, psychiatric classification, and response to psychotherapy. J Consult Clin Psychol. 1996;64(1):22–31. doi: 10.1037//0022-006x.64.1.22. [DOI] [PubMed] [Google Scholar]
- Greenberg MT, Speltz ML, Deklyen M. The role of attachment in the early development of disruptive behavior problems. Development and Psychopathology. 1993 doi:10.1017/S095457940000434X. [Google Scholar]
- Gunderson JG. The borderline patient's intolerance of aloneness: insecure attachments and therapist availability. Am J Psychiatry. 1996;153(6):752–758. doi: 10.1176/ajp.153.6.752. [DOI] [PubMed] [Google Scholar]
- Hallquist MN, Wright AGC. Mixture Modeling Methods for the Assessment of Normal and Abnormal Personality, Part I: Cross-Sectional Models. Journal of Personality Assessment. 2014;96(3):256–268. doi: 10.1080/00223891.2013.845201. doi:10.1080/00223891.2013.845201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heape CL, Pilkonis PA, Lambert J, Proietti J. Interpersonal Relations Assessment. 1989 Unpublished Manuscript. [Google Scholar]
- Hill J, Harrington R, Fudge H, Rutter M, Pickles A. Adult personality functioning assessment (APFA). An investigator-based standardised interview. The British Journal of Psychiatry : The Journal of Mental Science. 1989;155:24–35. doi: 10.1192/bjp.155.1.24. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2605429. [DOI] [PubMed] [Google Scholar]
- Holtzworth-Munroe A, Stuart GL, Hutchinson G. Violent versus nonviolent husbands: Differences in attachment patterns, dependency, and jealousy. Journal of Family Psychology. 1997 doi:10.1037/0893-3200.11.3.314. [Google Scholar]
- Hopwood CJ, Malone JC, Ansell EB, Sanislow CA, Grilo CM, McGlashan TH, Morey LC. Personality assessment in DSM-5: empirical support for rating severity, style, and traits. J Pers Disord. 2011;25(3):305–320. doi: 10.1521/pedi.2011.25.3.305. doi:10.1521/pedi.2011.25.3.305. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Wright AGC, Ansell EB, Pincus AL. The Interpersonal Core of Personality Pathology. Journal of Personality Disorders. 2013;27(3):270–295. doi: 10.1521/pedi.2013.27.3.270. doi:10.1521/pedi.2013.27.3.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy KN. The implications of attachment theory and research for understanding borderline personality disorder. Dev Psychopathol. 2005;17(4):959–986. doi: 10.1017/s0954579405050455. [DOI] [PubMed] [Google Scholar]
- Levy KN, Blatt SJ. Attachment theory and psychoanalysis: Further differentiation within insecure attachment patterns. Psychoanalytic Inquiry. 1999;19(4):541–575. doi:10.1080/07351699909534266. [Google Scholar]
- Luyten P, Blatt SJ. Interpersonal relatedness and self-definition in normal and disrupted personality development: Retrospect and prospect. American Psychologist. 2013;68(3):172–83. doi: 10.1037/a0032243. doi:10.1037/a0032243. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K. Attachment relationships among children with aggressive behavior problems: the role of disorganized early attachment patterns. Journal of Consulting and Clinical Psychology. 1996;64(1):64–73. doi: 10.1037//0022-006x.64.1.64. doi:10.1037/0022-006X.64.1.64. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Alpern L, Repacholi B. Disorganized infant attachment classification and maternal psychosocial problems as predictors of hostile-aggressive behavior in the preschool classroom. Child Development. 1993;64(2):572–585. doi: 10.1111/j.1467-8624.1993.tb02929.x. doi:10.2307/1131270. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Jacobvitz D. Attachment disorganization: Unresolved loss, relational violence, and lapses in behavioral and attentional strategies. Handbook of Attachment: Theory, Research, and Clinical Applications. 1999:520–554. [Google Scholar]
- Lyons-Ruth K, Yellin C, Melnick S, Atwood G. Expanding the concept of unresolved mental states: hostile/helpless states of mind on the Adult Attachment Interview are associated with disrupted mother-infant communication and infant disorganization. Development and Psychopathology. 2005;17(1):1–23. doi: 10.1017/s0954579405050017. doi:10.1017/S0954579405050017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main M, Hesse E. Parents’ unresolved traumatic experiences are related to infant disorganized attachment status: Is frightened and/or frightening parental behavior the linking mechanism? Attachment in the Preschool Years: Theory, Research, and Intervention. 1990 [Google Scholar]
- Main M, Kaplan N, Cassidy J. Security in infancy, childhood and adulthood: a move to the level of representation. 1985;50(1):66–104. doi:128.147.28.1. [Google Scholar]
- Main M, Solomon J. Discovery of an insecure-disorganized/disoriented attachment pattern. In Affective development in infancy. 1986:95–124. doi:10.1023/A. [Google Scholar]
- Main M, Solomon J. Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation. Attachment in the preschool years: Theory, research, and intervention. 1990:121–160. [Google Scholar]
- Marsh HW, Lüdtke O, Trautwein U, Morin AJS. Classical Latent Profile Analysis of Academic Self-Concept Dimensions: Synergy of Person- and Variable-Centered Approaches to Theoretical Models of Self-Concept. Structural Equation Modeling: A Multidisciplinary Journal. 2009;16(2):191–225. doi:10.1080/10705510902751010. [Google Scholar]
- Melges FT, Swartz MS. Oscillations of attachment in borderline personality disorder. Am J Psychiatry. 1989;146(9):1115–1120. doi: 10.1176/ajp.146.9.1115. [DOI] [PubMed] [Google Scholar]
- Meyer B, Pilkonis PA. An attachment model of personality disorders. Major Theories of Personality Disorder. 2005;2:231–281. [Google Scholar]
- Mikulincer M, Shaver PR. Attachment in Adulthood: Structure, Dynamics, and Change. Guilford Press; 2007. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Seventh Ed Muthén & Muthén; Los Angeles, CA: 2013. [Google Scholar]
- Nakash-Eisikovits O, Dutra L, Westen D. Relationship between attachment patterns and personality pathology in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(9):1111–23. doi: 10.1097/00004583-200209000-00012. doi:10.1097/00004583-200209000-00012. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):535–569. doi:10.1080/10705510701575396. [Google Scholar]
- Obsuth I, Hennighausen K, Brumariu LE, Lyons-Ruth K. Disorganized behavior in adolescent-parent interaction: relations to attachment state of mind, partner abuse, and psychopathology. Child Development. 2014;85(1):370–87. doi: 10.1111/cdev.12113. doi:10.1111/cdev.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality: SIDP-IV. American Psychiatric Pub; 1997. [Google Scholar]
- Pilkonis PA, Heape CL, Ruddy J, Serrao P. Validity in the diagnosis of personality disorders: The use of the LEAD standard. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(1):46. [Google Scholar]
- Skodol AE, Clark LA, Bender DS, Krueger RF, Morey LC, Verheul R, Oldham JM. Proposed changes in personality and personality disorder assessment and diagnosis for DSM-5 Part I: Description and rationale. Personal Disord. 2011;2(1):4–22. doi: 10.1037/a0021891. doi:10.1037/a0021891. [DOI] [PubMed] [Google Scholar]
- Solomon J, George C. The Disorganized Attachment-Caregiving System: The Origins of Caregiver Helplessness. In: Solomon J, George C, editors. Disorganized attachment and caregiving. Guilford Press; New York: 2011. p. 427. [Google Scholar]
- Straus MA, Hamby SL, Boney-Mccoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and Preliminary Psychometric Data. Journal of Family Issues. 1996 doi:10.1177/019251396017003001. [Google Scholar]
- van IJzendoorn MH, Feldbrugge JT, Derks FC, de Ruiter C, Verhagen MF, Philipse MW, Riksen-Walraven JM. Attachment representations of personality-disordered criminal offenders. The American Journal of Orthopsychiatry. 1997;67(3):449–459. doi: 10.1037/h0080246. doi:10.1037/h0080246. [DOI] [PubMed] [Google Scholar]
- van Ijzendoorn MH, Schuengel C, Bakermans-Kranenburg MJ. Disorganized attachment in early childhood: meta-analysis of precursors, concomitants, and sequelae. Development and Psychopathology. 1999;11(2):225–249. doi: 10.1017/s0954579499002035. doi:10.1017/S0954579499002035. [DOI] [PubMed] [Google Scholar]
- Waters E, Merrick S, Treboux D, Crowell J, Albersheim L. Attachment security in infancy and early adulthood: a twenty-year longitudinal study. Child Development. 1978;71:684–9. doi: 10.1111/1467-8624.00176. [DOI] [PubMed] [Google Scholar]
- Westen D, Moses MJ, Silk KR, Lohr NE, Cohen R, Segal H. Quality of depressive experience in borderline personality disorder and major depression: When depression is not just depression. Journal of Personality Disorders. 1992;6(4):382–393. [Google Scholar]
- Westen D, Nakash O, Thomas C, Bradley R. Clinical assessment of attachment patterns and personality disorder in adolescents and adults. Journal of Consulting and Clinical Psychology. 2006;74(6):1065–85. doi: 10.1037/0022-006X.74.6.1065. doi:10.1037/0022-006X.74.6.1065. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD). Journal of Personality Disorders. 2003;17(6):568–73. doi: 10.1521/pedi.17.6.568.25355. [DOI] [PubMed] [Google Scholar]