Abstract
Promoting physical activity is essential for addressing elevated cardiovascular risk and high obesity rates affecting people with serious mental illness. Numerous challenges interfere with exercise participation in this high-risk group including mental health symptoms, low motivation, and limited access to safe and affordable options for physical activity. Wearable devices and mobile health technologies may afford new opportunities for promoting physical activity and supporting behavioral weight loss efforts. This exploratory study examined whether daily step count measured using Fitbit wearable devices was associated with weight loss and improved fitness among individuals with serious mental illness enrolled in a 6-month lifestyle program. Participants (n=34) had a schizophrenia spectrum disorder (23.5%), major depression (50.0%), or bipolar disorder (26.5%), and wore Fitbits most of the days (M=86.2%; SD=18.4%) they were enrolled in the study. At 6-months, higher average daily step count was associated with greater weight loss (F=5.07; df=1,32; p=0.0314), but not improved fitness (F=1.92; df=1,31; p=0.176). These findings demonstrate that encouraging participants with serious mental illness enrolled in lifestyle interventions to collect more steps may contribute to greater weight loss. This suggests that wearable devices may offer a feasible and potentially effective strategy for supporting behavioral weight loss in community mental health settings.
Keywords: serious mental illness, mHealth, wearable devices, weight loss, fitness, physical activity
1. Introduction
Rates of obesity are nearly twice as high among people with serious mental illness, including schizophrenia spectrum and mood disorders, compared to the general population (Allison et al., 2009). This dramatic disparity in obesity prevalence is largely due to the combination of unhealthy lifestyle behaviors such as physical inactivity and poor diet, metabolic effects of psychoactive medications, poverty, and the impact of mental health symptoms on motivation and functioning (Allison et al., 2009). As a result, people with serious mental illness experience elevated risk of cardiovascular disease and significantly reduced life expectancy (Walker et al., 2015). Efforts are urgently needed to address the early mortality health disparity affecting these individuals.
Recent randomized controlled trials have demonstrated that promoting physical activity as part of lifestyle interventions for weight loss can contribute to clinically significant reduction in cardiovascular risk in as many as half of participants with serious mental illness (Bartels et al., 2013; Bartels et al., 2015; Daumit et al., 2013; Green et al., 2015). A robust body of evidence supports the numerous benefits of physical activity participation for people with serious mental illness. A systematic review of 39 trials found that engaging in regular physical activity resulted in fewer depressive symptoms, greater aerobic capacity, and improved quality of life among people with mental illnesses including schizophrenia and bipolar disorder (Rosenbaum et al., 2014). Recent meta-analyses have also demonstrated that physical activity contributes to reduction in mental health symptom severity among people with serious mental illness (Dauwan et al., 2015; Firth et al., 2015a).
Despite well-documented benefits of physical activity for people with serious mental illness, there are numerous challenges to effectively promoting more active lifestyles in this high-risk group. Compared to the general population, people with serious mental illness are less likely to participate in exercise (Daumit et al., 2005) and more frequently engage in sedentary behaviors (Stubbs et al., 2016). Among individuals with schizophrenia, fewer than one in five report engaging in moderate exercise at least once per week, and nearly 40% are physically inactive (Brown et al., 1999). People with serious mental illness report many barriers to physical activity including low confidence and low motivation due to symptoms of depression, stress, fatigue and anxiety, as well as fears of discrimination, limitations due to physical health conditions, and concerns about neighborhood safety (Browne et al., 2015; Johnstone et al., 2009; McDevitt et al., 2006; Ussher et al., 2007). Consistent with other low-income groups (Powell et al., 2006), inadequate access to safe and affordable options for exercise such as local parks or recreation facilities is a likely contributor to physical inactivity among people with serious mental illness. In addition, few public sector mental health facilities offer supported opportunities for people with serious mental illness to participate in physical activity programs (Dixon et al., 1999; Jeste et al., 1996; Richardson et al., 2005). Finally, the effects of debilitating mental health symptoms, impaired information processing capabilities, and low-motivation likely create challenges for planning ahead to meet weekly activity goals, prioritizing exercise over competing demands, and adhering to a set exercise regimen over time (Richardson et al., 2005).
Feasible and effective strategies are needed to overcome these diverse challenges and to promote physical activity participation among people with serious mental illness. Mobile health technologies and wearable devices are particularly promising for supporting physical activity as part of lifestyle interventions for these individuals. In a series of pilot studies, we demonstrated the feasibility and acceptability of using popular wearable devices among people with serious mental illness (Naslund et al., 2015a; Naslund et al., 2016b). These devices offer a user-friendly platform and interface that includes several features that are motivating and make being physically active enjoyable such as reminders, goal setting, rewards for achieving milestones, social connection and competition with peers, and ability to track individual performance over time (Patel et al., 2015). As mobile technologies become increasingly affordable and more widely available among people with serious mental illness (Firth et al., 2015b), there are opportunities to use wearable devices to support broader health promotion efforts targeting weight loss and cardiovascular risk factors in this vulnerable group. However, it is not clear whether these devices can support a lifestyle intervention targeting weight loss and fitness, and whether data captured using wearable devices is associated with improved outcomes.
In this exploratory study, participants with serious mental illness who were enrolled in a community-based group behavioral weight loss program were given Fitbit wearable devices to support their physical activity and weight loss goals. We examined whether average daily step count measured using the wearable devices over the 6-month study duration was associated with weight loss and improved fitness. We hypothesized that higher average daily step count would be associated with greater weight loss and improved fitness at 6-months. We then explored whether changes in step count over time (such as increasing or decreasing steps) was associated with weight loss or improved fitness (i.e., a time-varying relationship). We did not have a specific hypothesis regarding timing of steps and associated changes in weight and fitness, but we hypothesized that increased steps at any time during the course of the study would be associated with greater weight loss and improved fitness.
2. Methods
2.1 Participants and Setting
Participants in this study were enrolled in a 6-month group behavioral weight loss program targeting fitness and healthy eating through an urban community mental health center in southern New Hampshire. Participants were age 21 or older; had serious mental illness defined by an axis I diagnosis of schizophrenia, schizoaffective disorder, major depressive disorder, or bipolar disorder; spoke English; were on stable pharmacological treatment defined as receiving the same psychiatric medications over the prior 2 months; and had obesity defined as body mass index (BMI) ≥30. Participants were excluded if they had any medical contraindication to weight loss; were pregnant or planning to become pregnant within the next 6 months; or had a current diagnosis of an active alcohol-use or substance-use disorder. Participants received medical clearance from a primary care provider prior to starting the program and had to be able to walk at least one city block. Committees for the Protection of Human Subjects at Dartmouth College and the New Hampshire Department of Health and Human Services approved all study procedures.
2.2 Wearable Devices
Participants were given Fitbit Zip wearable devices and smartphones to use for the 6-month study duration. The Fitbit Zip is a compact wearable accelerometer that clips onto participants’ clothing. It tracks number of steps and it synchs wirelessly with a free companion smartphone application. The Fitbit rewards milestones such as reaching daily step goals with colorful trophies, and it allows users to compare steps and progress with others through the smartphone application. We elected to use Fitbit Zip wearable devices because in our previous work we found that these devices were both feasible and acceptable for use among people with serious mental illness (Naslund et al., 2015a; Naslund et al., 2016b). Participants attended two brief 30- minute training sessions with a member of the research staff for instruction in using the Fitbit wearable devices and synching the Fitbit with the companion smartphone application. Technical support for using the Fitbit or companion mobile application was provided to participants on an as needed basis by a member of the research team over the study duration.
2.3 Group-based Lifestyle Program
The group-based lifestyle program focused on achieving weight loss through healthy eating and increasing physical activity. The program was modeled after the evidence-based Diabetes Prevention Program, and included weekly group sessions led by lifestyle coaches. Full descriptions of the program are available elsewhere (Aschbrenner et al., 2016; Aschbrenner et al., 2015). Participants shared an activity goal of reaching 150 minutes of exercise each week. As part of the program, participants received 3-5 text messages from research staff each week as reminders to attend optional exercise classes, to be more active as part of their daily routines, to provide encouragement for finding new ways to be more active, and to support participants in reaching the program’s weekly physical activity goal. Additionally, participants were encouraged to set daily step goals on their Fitbits, and they were given the opportunity to review and revise these goals each week. Participants had varying capabilities to engage in physical activity, and some participants had mobility issues. As a result, the goal-setting component of the program was personalized to meet participants’ physical abilities, whereby participants set individual daily step goals that they felt that they could reach.
2.4 Measures
Step Count
Daily step count data for the 6-month study duration was exported from participants’ personal Fitbit accounts into an Excel spreadsheet. Days where participants recorded no steps were coded as ‘missing’. If participants wore the device and the device was functioning properly then it would be highly unlikely to obtain zero steps in a day. Missing step data typically occurred due to technical malfunctions with the Fitbit device or dead battery, or in cases where participants forgot to wear the device or temporarily lost the device. The reliability of the Fitbit wearable device for measuring steps has been previously demonstrated (Case et al., 2015).
Weight
Weight was measured in pounds and reported as the change in body weight from baseline to 6- months.
Fitness
Fitness was measured using the 6-Minute Walk Test (6-MWT), which measures the distance in feet that an individual can walk in six minutes. The 6-MWT is considered a reliable and valid measure of fitness (Beriault et al., 2009; Larsson and Reynisdottir, 2008) and has demonstrated reproducibility in people with serious mental illness (Vancampfort et al., 2011). Change in fitness was calculated as the change in feet on the 6-MWT from baseline to 6-months.
2.5 Statistical Analysis
To test our first hypothesis (average daily step count would be associated with weight loss and improved fitness), we used linear regression models to evaluate the association between average daily step count over the 6-month study duration and the pre-post changes in participants’ weight and fitness. To test our second hypothesis (increased steps at any time would be associated with greater weight loss and improved fitness), we used penalized functional regression (Goldsmith et al., 2011) models to evaluate the time-varying association between daily step count collected using the wearable devices (intensive repeated-measure variable) and the pre-post changes in participants’ weight and fitness (individual-level outcome measures). This analysis allowed for observation of patterns in increased steps over the course of the study and tested whether there are certain patterns that confer greater weight loss or an increase in fitness. For example, with this analysis, we could test whether earlier increases in step count were more predictive of weight loss than later increases in step count. Change in weight and fitness were calculated as the post-intervention measure minus the baseline measure. Significance of the functional predictor (steps) was evaluated using a permutation test (Ramsay et al., 2009). A p-value of 0.05 was considered statistically significant.
3. Results
The current analysis included 34 participants who completed the 6-month post-intervention assessments and for whom step data were collected over the entire study duration. Participants' baseline characteristics are presented in Table 1. Initially, a total of 43 participants enrolled in the 6-month group lifestyle intervention were given Fitbit Zip wearable devices to support their physical activity goals as part of the program. Nine participants were lost to follow-up or stopped participation due to various concerns including serious medical issues (n = 2), mental health concerns (n = 3), pregnancy (n = 1), work commitments (n = 2), and other behavioral issues (n = 1). The 34 participants included in this analysis did not differ on any baseline characteristics from the 9 participants who were lost to follow-up or who stopped participation.
Table 1.
Baseline demographic and clinical characteristics of participants
| Characteristic | Total Sample (N=34) |
|---|---|
| Demographic Characteristics | |
| Mean Age (SD) | 50.2 (11.0) |
| Female (%) | 21 (61.8%) |
| Non-Hispanic white (%) | 34 (100%) |
| Education | |
| Less than high school | 2 (5.9%) |
| High school | 11 (32.4%) |
| Some college | 13 (38.2%) |
| College degree | 8 (23.5%) |
| Living situation | |
| Living independently | 27 (79.4%) |
| Living with family | 6 (17.7%) |
| Assisted or supported housing | 1 (2.9%) |
| Marital status | |
| Never married | 11 (32.4%) |
| Currently married | 3 (8.8%) |
| Previously married | 20 (58.8%) |
| Currently Employed (part or full-time) | 7 (20.6%) |
| Enrolled in Medicaid only | 8 (23.5%) |
| Enrolled in Medicare only | 8 (23.5%) |
| Dual Eligible (enrolled in Medicaid and Medicare) | 18 (52.9%) |
| Clinical Characteristics | |
| Mental illness diagnosis (%) | |
| Schizophrenia spectrum disorders | 8 (23.5%) |
| Major depressive disorder | 17 (50.0%) |
| Bipolar disorder | 9 (26.5%) |
| BMI (kg/m2) (SD) | 38.5 (9.3) |
| Weight (lbs) | 231.9 (46.7) |
| Fitness | 1303.8 (323.2) |
| Current smoker | 6 (17.7%) |
3.1 Wearable Device Use
Participants had their Fitbits to use for an average of 181.7 days (SD = 34.7), with a median of 181.5 days (interquartile range = 169 to 196). This variation in length of time with the Fitbit occurred due to rolling enrollment at the start of the study. Participants wore their Fitbits for a mean of 86.2% (SD = 18.4%) of the days that they had the Fitbit to use (median = 94.0% of the days, interquartile range = 82.0% to 97.0%).
3.2 Average Daily Step Count and Weight Loss and Improved Fitness
Participants achieved an average of 4453.5 (SD = 2707.4) steps each day, with average daily step counts ranging from 1037.6 (SD = 767.9) steps to 11,366.3 (SD = 3416.9) steps. In total, 21 (61.8%) participants achieved 10,000 steps or more on at least one day during the study. These 21 participants achieved 10,000 daily steps or more for a mean of 16.1% (SD = 21.0%) of the days that they had the Fitbit to use (median = 25.7% of the days, interquartile range = 0.9% to 25.7%). Three (8.8%) participants achieved 10,000 daily steps or more on at least half of the days that they were enrolled in the study.
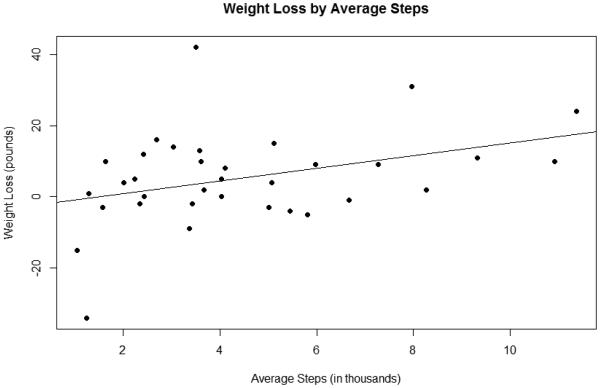
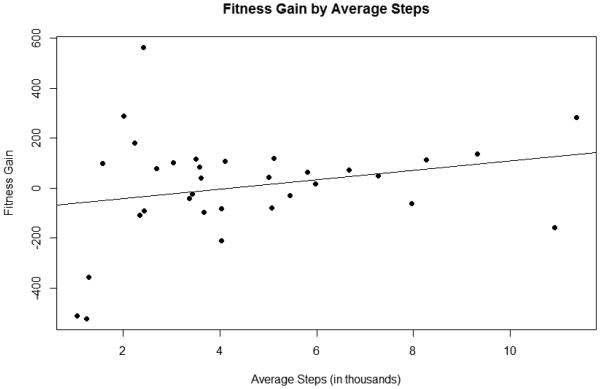
There was a significant association between participants’ average daily step count and weight loss. Figure 1 shows that for every 1000 step increase in participants’ daily average step count, they experienced a decrease in weight of 1.78 pounds (F = 5.07; df = 1, 32; p = 0.0314). The relationship between average daily step count and change in fitness was not significant. However, as illustrated in Figure 2 the direction of the relationship is consistent with our hypothesis. If participants average daily step count increased by 1000 steps, it corresponded to an increase of 18.79 feet on the 6-Minute Walk Test (F = 1.92; df = 1, 31; p = 0.176).
Figure 1. Association between average daily steps and weight lossa.
a The association between participants’ average daily step count and weight loss (measured in pounds) was statistically significant (F = 5.07; df = 1, 32; p = 0.0314).
Figure 2. Association between average daily steps and gain in fitnessa.
a The relationship between participants’ average daily step count and change in fitness (measured in feet using the 6-Minute Walk Test) was not significant (F = 1.92; df = 1, 31; p = 0.176); however, the direction of the relationship is consistent with our hypothesis.
3.3 Time-Varying Relationship Between Step Count and Weight Loss and Improved Fitness
In the penalized functional regression models, it was observed that the time-varying relationship between daily step count and weight loss (permutation test statistic = 0.180; p = 0.264) and improved fitness (permutation test statistic = 0.076; p = 0.574) were not significant. This suggests that there was no specific period of time for which an increase in steps was significantly associated with either weight loss or improved fitness.
4. Discussion
The findings from our exploratory study suggest that wearable devices and their companion smartphone applications may serve as valuable tools for supporting community-based weight loss efforts for people with serious mental illness. Importantly, we observed that a higher average daily step count over the 6-month program duration was associated with greater weight loss. Therefore, it appears that providing participants with serious mental illness the recommendation to collect more steps each day and maintain a high average daily step count throughout participation in a lifestyle intervention may contribute to greater weight loss. These are preliminary findings and should be interpreted with caution, but they offer promise regarding the potential benefits of using wearable devices to support lifestyle interventions delivered through community mental health settings.
While we did not observe a significant relationship between average daily step count and improved fitness, the direction of the association was positive suggesting that with a larger sample size this relationship could have been significant. Also, we found that there was no time- varying association between steps and changes in weight or fitness. That is, it was not particularly important for an increase in steps to happen at a specific time during the intervention (at the beginning, for example). This finding is indicative of the wide variety of patterns of steps over the course of the study, and no specific pattern appeared predictive of changes in weight or fitness as long as the overall average step count was higher over the course of the study.
Research in the general population has demonstrated that devices such as pedometers can help support weight loss efforts. Prior systematic reviews have highlighted that using pedometers to track daily steps can contribute to modest weight loss when used over long durations (Richardson et al., 2008) and when individuals set daily step goals (Bravata et al., 2007). A cross-sectional study of sedentary adults also found that number of steps per day was associated with lower rates of hypertension and better overall cardiovascular health (Lee et al., 2013).
However, a recent review of studies in the general population demonstrated that technology appears most effective for supporting weight loss efforts when combined with other evidence- based practices (Levine et al., 2015). For example, technology can serve an important role to facilitate strategies that are known to contribute to successful weight loss such as self-monitoring, feedback, or encouragement and lifestyle coaching (Levine et al., 2015). This notion was supported in a study of adults with serious mental illness who received pedometers combined with established motivational interviewing strategies that resulted in greater physical activity and weight loss after 12-weeks (Methapatara and Srisurapanont, 2011). In our study, the Fitbit wearable devices were integrated as part of the behavioral weight loss program, and were used as a way to support self-monitoring, goal setting, and tracking progress over time.
Our study contributes to a small number of preliminary studies that have explored the use of wearable sensors among people with serious mental illness (Ben-Zeev et al., 2016; Naslund et al., 2015b), and to our knowledge is the first study to highlight an association between data collected using wearable devices and weight loss in this high-risk group. As Patel and colleagues (2015) caution, there remains a considerable gap between recording individual-level information using wearable devices and contributing to meaningful and lasting health behavior change (Patel et al., 2015). While it is possible that the wearable devices in our study helped participants monitor their activity over time and may have provided them with additional encouragement, we also know that participants were highly engaged in the lifestyle program and had access to social and informational support from other participants as well as the lifestyle coaches who led the weekly group sessions (Aschbrenner et al., 2016; Aschbrenner et al., 2015). Therefore, the success of the wearable devices in contributing to weight loss may have been largely driven by the theoretically based components of the group lifestyle intervention that supported changes in participants’ physical activity and dietary behaviors. Wearable devices alone are unlikely to contribute to behavior change, especially given surveys that have found that many people are quick to stop using these devices (Ledger, 2014). The success of wearable devices likely relies on whether they can leverage key principles of behavior theories including self-monitoring, self-efficacy, or social competition, and whether there are strategies to sustain user engagement (Patel et al., 2015).
In our study, we observed that the recommendation to collect more steps each day was acceptable and easily understood by participants. Wearable devices may be useful for simplifying physical activity recommendations for high-risk and low-health literacy groups such as people with serious mental illness. Encouraging people to get more steps over the course of their daily routines is an easier and more straight forward message that avoids the executive function demands to plan and schedule ahead to meet the 150 minute weekly physical activity guidelines. This may also be beneficial for sedentary individuals with chronic health conditions who may be overwhelmed with the prospect of exercising for 150 minutes each week. For example, walking is a preferred type of activity among people with serious mental illness (Ussher et al., 2007), and it is important for low-income individuals because it does not require access to a gym, expensive equipment, or a costly fitness trainer. Walking is especially appropriate for individuals who were previously sedentary or who experience mobility difficulties (Siegel et al., 1995) and appears to contribute to improved cardiorespiratory fitness among people with serious mental illness (Strassnig et al., 2012). Wearable devices may help to reinforce the benefits of walking by offering a tangible reward in the form of steps that can be tracked over time, and that connects with individuals’ mobile devices.
It is promising that an increasing number of people with serious mental illness have smartphones that can connect to the companion mobile applications for popular wearable devices (Firth et al., 2016; Naslund et al., 2016a). However, the costs of the actual wearable devices remain a significant barrier that cannot be overlooked. In this study, the Fitbit devices cost about $60 each, which may be a barrier for low-income individuals with serious mental illness to purchase these devices on their own. To date, use of wearable devices has largely been among more affluent individuals who are living healthy lifestyles and who are interested in tracking their progress (Piwek et al., 2016). The sustainability and potential for widespread health benefits of using wearable devices will only be realized if the individuals who stand to benefit the most from these devices, such as low-income individuals with poor overall health and with chronic health conditions, are able to easily obtain access to these devices (Patel et al., 2015).
4.1 Limitations
There are several limitations that should be considered when interpreting these findings. First, this study had a small sample size that lacked racial or ethnic diversity, and therefore these findings may not generalize to other community mental health settings. Second, the analyses presented here were based on the program participants who received the Fitbit wearable devices, remained engaged in the research study, and used the devices over the 6-month study duration. Participation in a concurrent 6-month lifestyle intervention may limit the generalizability of these findings. Third, we were unable able to determine if participants who dropped out of the study may have experienced difficulty participating in physical activity or using the Fitbit to measure their daily steps, though participants who dropped out did not differ from completers on any characteristics at baseline. Lastly, all participants in this study were receiving services through community mental health settings, indicating that these findings are likely not representative of individuals with serious mental illness not currently receiving services.
5. Conclusions
This exploratory study highlights the potential to use wearable devices to help people with serious mental illness enrolled in lifestyle programs track their physical activity and achieve greater weight loss. Wearable devices can potentially simplify how physical activity recommendations are targeted at high-risk groups such as people with serious mental illness, and may be effective for supporting walking programs and other lifestyle interventions delivered through community mental health settings. Further research is necessary to investigate whether wearable devices and companion smartphone applications can serve as effective tools for helping people with serious mental illness to reach the weekly physical activity guidelines. Future large scale studies using randomized controlled designs are also needed to determine whether use of wearable devices as part of lifestyle interventions delivered through community mental health settings can contribute to reduction in cardiovascular risk and sustained benefits over time for individuals with serious mental illness.
Highlights.
People with serious mental illness used wearable devices to support weight loss.
Participants wore Fitbit devices for most of the days enrolled in the study.
Higher average daily step count was associated with greater weight loss.
Wearable devices could simplify efforts promoting physical activity in this group.
Wearable devices appear effective for supporting behavioral weight loss programs.
Acknowledgements
This study was supported by the National Institute of Mental Health (R01 MH089811-01) and the United States Centers for Disease Control and Prevention Health Promotion and Disease Prevention Research Center (Cooperative Agreement Number U48DP005018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors report no conflicting interests.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allison DB, Newcomer JW, Dunn AL, Blumenthal JA, Fabricatore AN, Daumit GL, Cope MB, Riley WT, Vreeland B, Hibbeln JR. Obesity among those with mental disorders: a National Institute of Mental Health meeting report. American journal of preventive medicine. 2009;36(4):341–350. doi: 10.1016/j.amepre.2008.11.020. [DOI] [PubMed] [Google Scholar]
- Aschbrenner KA, Naslund JA, Shevenell M, Kinney EC, Bartels SJ. A pilot study of a peer-group lifestyle intervention enhanced with mHealth technology and social media for adults with serious mental illness. Journal of Nervous and Mental Disease. 2016;204(6):483–486. doi: 10.1097/NMD.0000000000000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbrenner KA, Naslund JA, Shevenell M, Mueser KT, Bartels SJ. Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness. Psychiatric Quarterly. 2015:1–15. doi: 10.1007/s11126-015-9395-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Jue K, Wolfe RS, Xie H, McHugo G, Santos M, Williams GE, Naslund JA, Mueser KT. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatric Services. 2013;64(8):729–736. doi: 10.1176/appi.ps.003622012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Naslund JA, Wolfe RS, Xie H, McHugo G, Jimenez D, Jue K, Feldman J, Bird B. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. American Journal of Psychiatry. 2015;172(4):344–352. doi: 10.1176/appi.ajp.2014.14030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Wang R, Abdullah S, Brian R, Scherer EA, Mistler LA, Hauser M, Kane JM, Campbell A, Choudhury T. Mobile behavioral sensing for outpatients and inpatients with schizophrenia. Psychiatric Services. 2016;67(5):558–561. doi: 10.1176/appi.ps.201500130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beriault K, Carpentier AC, Gagnon C, Menard J, Baillargeon JP, Ardilouze JL, Langlois MF. Reproducibility of the 6-minute walk test in obese adults. Int J Sports Med. 2009;30(10):725–727. doi: 10.1055/s-0029-1231043. [DOI] [PubMed] [Google Scholar]
- Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, Stave CD, Olkin I, Sirard JR. Using pedometers to increase physical activity and improve health: a systematic review. Jama. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychological medicine. 1999;29(03):697–701. doi: 10.1017/s0033291798008186. [DOI] [PubMed] [Google Scholar]
- Browne J, Mihas P, Penn DL. Focus on exercise: client and clinician perspectives on exercise in individuals with serious mental illness. Community Mental Health Journal. 2015;52(4):387–394. doi: 10.1007/s10597-015-9896-y. [DOI] [PubMed] [Google Scholar]
- Case MA, Burwick HA, Volpp KG, Patel MS. Accuracy of smartphone applications and wearable devices for tracking physical activity data. Jama. 2015;313(6):625–626. doi: 10.1001/jama.2014.17841. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, Young DR, Frick KD, Yu A, Gennusa JV, 3rd, Oefinger M, Crum RM, Charleston J, Casagrande SS, Guallar E, Goldberg RW, Campbell LM, Appel LJ. A behavioral weight-loss intervention in persons with serious mental illness. The New England journal of medicine. 2013;368(17):1594–1602. doi: 10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daumit GL, Goldberg RW, Anthony C, Dickerson F, Brown CH, Kreyenbuhl J, Wohlheiter K, Dixon LB. Physical activity patterns in adults with severe mental illness. The Journal of nervous and mental disease. 2005;193(10):641–646. doi: 10.1097/01.nmd.0000180737.85895.60. [DOI] [PubMed] [Google Scholar]
- Dauwan M, Begemann MJ, Heringa SM, Sommer IE. Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: a systematic review and meta-analysis. Schizophrenia Bulletin. 2015 doi: 10.1093/schbul/sbv164. sbv164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon L, Postrado L, Delahanty J, Fischer PJ, Lehman A. The association of medical comorbidity in schizophrenia with poor physical and mental health. The Journal of nervous and mental disease. 1999;187(8):496–502. doi: 10.1097/00005053-199908000-00006. [DOI] [PubMed] [Google Scholar]
- Firth J, Cotter J, Elliott R, French P, Yung A. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychological medicine. 2015a;45(07):1343–1361. doi: 10.1017/S0033291714003110. [DOI] [PubMed] [Google Scholar]
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophrenia Bulletin. 2015b doi: 10.1093/schbul/sbv132. sbv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophrenia Bulletin. 2016;42(2):448–455. doi: 10.1093/schbul/sbv132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith J, Bobb J, Crainiceanu CM, Caffo B, Reich D. Penalized functional regression. Journal of Computational and Graphical Statistics. 2011;20(4):830–851. doi: 10.1198/jcgs.2010.10007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CA, Yarborough BJH, Leo MC, Yarborough MT, Stumbo SP, Janoff SL, Perrin NA, Nichols GA, Stevens VJ. The STRIDE weight loss and lifestyle intervention for individals taking antipsychotic medications: a randomized trial. The American journal of psychiatry. 2015;172(1):71–81. doi: 10.1176/appi.ajp.2014.14020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP. Medical comorbidity in schizophrenia. Schizophrenia Bulletin. 1996;22(3):413–430. doi: 10.1093/schbul/22.3.413. [DOI] [PubMed] [Google Scholar]
- Johnstone R, Nicol K, Donaghy M, Lawrie S. Barriers to uptake of physical activity in community-based patients with schizophrenia. Journal of Mental Health. 2009;18(6):523–532. [Google Scholar]
- Larsson UE, Reynisdottir S. The six-minute walk test in outpatients with obesity: reproducibility and known group validity. Physiotherapy Res Int. 2008;13(2):84–93. doi: 10.1002/pri.398. [DOI] [PubMed] [Google Scholar]
- Ledger D. Inside wearables - part 2: a look at the uncertain future of smart wearable devices, and five industry developments that will be necessary for meaningful mass market adoption and sustained engagement. Endeavour Partners. 2014 http://endeavourpartners.net/assets/Endeavour-Partners-Inside-Wearables-Part-2-July-2014.pdf. [Google Scholar]
- Lee PH, Nan H, Yu Y-Y, McDowell I, Leung GM, Lam T. For non-exercising people, the number of steps walked is more strongly associated with health than time spent walking. Journal of Science and Medicine in Sport. 2013;16(3):227–230. doi: 10.1016/j.jsams.2012.10.005. [DOI] [PubMed] [Google Scholar]
- Levine DM, Savarimuthu S, Squires A, Nicholson J, Jay M. Technology-assisted weight loss interventions in primary care: a systematic review. Journal of general internal medicine. 2015;30(1):107–117. doi: 10.1007/s11606-014-2987-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt J, Snyder M, Miller A, Wilbur J. Perceptions of barriers and benefits to physical activity among outpatients in psychiatric rehabilitation. Journal of Nursing Scholarship. 2006;38(1):50–55. doi: 10.1111/j.1547-5069.2006.00077.x. [DOI] [PubMed] [Google Scholar]
- Methapatara W, Srisurapanont M. Pedometer walking plus motivational interviewing program for Thai schizophrenic patients with obesity or overweight: a 12-week, randomized, controlled trial. Psychiatry and clinical neurosciences. 2011;65(4):374–380. doi: 10.1111/j.1440-1819.2011.02225.x. [DOI] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular m-Health technologies for activity tracking among individuals with serious mental illness. Telemedicine and e-Health. 2015a;21(3):213–216. doi: 10.1089/tmj.2014.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Bartels SJ. How people living with serious mental illness use smartphones, mobile apps, and social media. Psychiatric rehabilitation journal. 2016a:1–4. doi: 10.1037/prj0000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Aschbrenner KA, Bartels SJ. Wearable devices and smartphones for activity tracking among people with serious mental illness. Mental Health and Physical Activity. 2016b;10:10–17. doi: 10.1016/j.mhpa.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund JA, Marsch LA, McHugo GJ, Bartels SJ. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health. 2015b;24(5):321–332. doi: 10.3109/09638237.2015.1019054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. Jama. 2015;313(5):459–460. doi: 10.1001/jama.2014.14781. [DOI] [PubMed] [Google Scholar]
- Piwek L, Ellis DA, Andrews S, Joinson A. The rise of consumer health wearables: promises and barriers. PLoS Medicine. 2016;13(2):e1001953. doi: 10.1371/journal.pmed.1001953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: a national study. American journal of public health. 2006;96(9):1676–1680. doi: 10.2105/AJPH.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsay JO, Hooker G, Graves S. Functional data analysis with R and MATLAB. Springer Science & Business Media; New York, NY: 2009. [Google Scholar]
- Richardson CR, Faulkner G, McDevitt J, Skrinar GS, Hutchinson DS, Piette JD. Integrating physical activity into mental health services for persons with serious mental illness. Psychiatric Services. 2005;56(3):324–331. doi: 10.1176/appi.ps.56.3.324. [DOI] [PubMed] [Google Scholar]
- Richardson CR, Newton TL, Abraham JJ, Sen A, Jimbo M, Swartz AM. A meta-analysis of pedometer-based walking interventions and weight loss. The Annals of Family Medicine. 2008;6(1):69–77. doi: 10.1370/afm.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. The Journal of clinical psychiatry. 2014;75(9):964–974. doi: 10.4088/JCP.13r08765. [DOI] [PubMed] [Google Scholar]
- Siegel PZ, Brackbill RM, Heath GW. The epidemiology of walking for exercise: implications for promoting activity among sedentary groups. American journal of public health. 1995;85(5):706–710. doi: 10.2105/ajph.85.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strassnig MT, Newcomer JW, Harvey PD. Exercise improves physical capacity in obese patients with schizophrenia: pilot study. Schizophrenia research. 2012;141(2):284–285. doi: 10.1016/j.schres.2012.08.011. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Williams J, Gaughran F, Craig T. How sedentary are people with psychosis? A systematic review and meta-analysis. Schizophrenia Research. 2016;171(1-3):103–109. doi: 10.1016/j.schres.2016.01.034. [DOI] [PubMed] [Google Scholar]
- Ussher M, Stanbury L, Cheeseman V, Faulkner G. Physical activity preferences and perceived barriers to activity among persons with severe mental illness in the United Kingdom. Psychiatric services. 2007;58(3):405–408. doi: 10.1176/ps.2007.58.3.405. [DOI] [PubMed] [Google Scholar]
- Vancampfort D, Probst M, Sweers K, Maurissen K, Knapen J, De Hert M. Reliability, minimal detectable changes, practice effects and correlates of the 6-min walk test in patients with schizophrenia. Psychiatry research. 2011;187(1):62–67. doi: 10.1016/j.psychres.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]