Abstract
Casting is a routine procedure used for fracture care in the pediatric population. The purpose of this review is to provide pearls and pitfalls that our institution has learned from previous literature. When applying the cast, we recommend using cotton padding for the liner and fiberglass or plaster depending on how much swelling is expected. A well-molded cast must be applied in order to prevent further fracture displacement. Cast valving is a valuable technique that allows a decrease in pressure which prevents discomfort and complications like compartment syndrome. Preventing thermal injuries, skin complications, and a wet cast are other important considerations when caring for casts. Appropriate use of a cast saw, avoiding pressure spots, and properly covering the cast are ways to respectively prevent those complications. Lastly, patient education remains one of the most valuable tools in ensuring proper cast maintenance.
Keywords: Cast care, Fracture cast, Pediatric casting, Pediatric fractures, Casting, Cast complications
Core tip: Casting is a routine procedure used for fracture care in the adult and pediatric population. The pediatric population present a unique set of attributes that often making casting difficult. In this article we will review different pearls and pitfalls seen while treating fractures in children which includes cast application, maintenance, and removal.
INTRODUCTION
Casting is a routine procedure used for fracture care in the pediatric population. Casting may be performed to immobilize non-displaced fractures, maintain reduction of displaced fractures and protect operatively treated fractures. As commonly as casting is performed, the art of this technique appears to be less emphasized in many orthopaedic training programs, especially with the advancement in methods of surgical fixation of children’s fractures. However, their use remains as a mainstay in orthopedics. Orthopaedic providers with a wide range of training background (i.e., physician assistants, nurse practitioners, cast technicians) often are the primary applicators of a cast. Despite casting being performed by a wide range of providers, it should not be viewed as a procedure without risks.
Numerous studies, historical and recent, have looked at common complications of casting[1-11]. Many of these have focused on hip spica casts and forearm fractures treated with short or long arm casts[12-16]. These complications can range from skin excoriations to compartment syndrome.
Complications and improper application of casts have contributed a burden of non-emergent patients seen in emergency departments[17]. Sawyer et al[17] investigated patients that are seen in emergency departments for problems relative to their cast and found that approximately 29% of the visits were because of a wet cast; 10%, were secondary to a damaged cast; 23%, a tight cast; 13%, a loose cast; and 10%, new or different pain. When casting has been applied correctly, it has the potential to save a significant amount of money when compared to surgical alternatives[17]. According to Newton and Mubarak, the total charges for a hip spica were $494 while the surgical alternative was approximately $21000[18].
The purpose of this article is to review the current literature pertinent to casting and share our own pearls and pitfalls that we have learned while caring for children’s fractures with a cast. We also aim to provide various recommendations to safely and effectively place, maintain, and remove casts.
CAST MATERIAL
One of the primary decisions the provider has to make when applying a cast is what material to use. The two types that are traditionally used are plaster and fiberglass. Each of which have benefits and drawbacks that must be considered when choosing one over the other.
Plaster-impregnated cloth’s major advantage includes its ability to mold more easily than it’s counterpart. This allows the provider to apply a custom mold to a reduced fracture and maintain reduction during the healing process. The drawbacks of plaster is it has a poor resistance to water and low strength-to-weight ratio which make it noticeably heavier than fiberglass[19].
When treating fractures in children primarily with a cast, fiberglass is usually our preferred choice. Since the child on average will wear the cast for 4-6 wk, the lighter and less bulky fit often makes it more comfortable for the child.
CAST APPLICATION
Cast application entails many elements which include the type and amount of material used, type of soft roll, presence or absence of stockinet and the method of rolling the cast as well as the final cast shape and position. The importance of a well-molded cast cannot be over emphasized[12,20]. One of the main tenets of the cast application is to apply a mold based on the fracture pattern to, when applicable, maintain reduction and/or prevent displacement from occurring or at least worsening (Figure 1).
Figure 1.
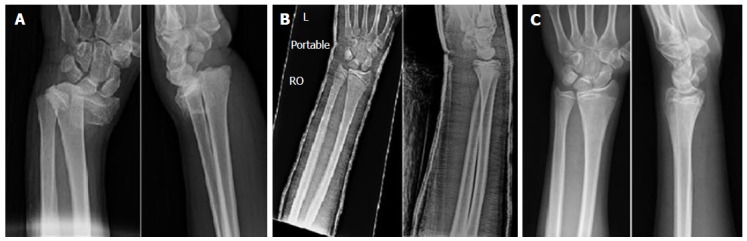
Well-molded cast. A: Pre-reduction X-rays of pediatric forearm demonstrating a completely displaced distal both bone forearm fracture. Immediate post-reduction X-rays; B: Immediate post-reduction X-rays demonstrating adequate reduction with a flexion mold to prevent fracture from dorsal displacement; C: Three-months follow-up X-rays demonstrating completely healed fracture with near-anatomic alignment.
Excessive focused pressure over a small surface area of the cast can lead to decreased areas of perfusion and cause pressure sores. The practitioner should be constantly aware of their hand position in addition to the assistants’ so they do not stay in one location for too long. Avoiding wrinkles and uneven ridges throughout the cast are details that will cause even pressure distribution throughout the extremity.
When treating distal radial and ulna fractures calculating the cast index on post application radiographs has been demonstrated to predict fracture displacement after cast application[14,20-22] (Figure 2). The measure is performed at the level of the fracture. The goal is to create a ratio of sagittal width to coronal width to be equal or less than 0.8. If the ratio is equal or less than 0.8 the fracture has approximately 5% of displacement as opposed to 26% chance for an index greater than 0.8. Another radiographic measurement that can be used when treating fractures of the distal radius and ulna is an angle measured by the index finger or second-metacarpal and distal radius[23]. To oppose the pull of the brachioradialis, which is often a deforming force in distal one-third radial fractures, molding a cast in ulnar deviation is recommended. If molded with ulnar deviation (second metacarpal-radius angle > 0 degrees), the outcome was considered to be ideal in 86.7% of cases compared to only 74.4% when it was < 0 degrees[23].
Figure 2.
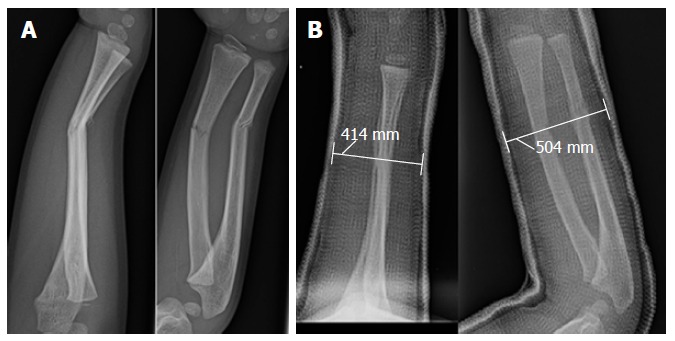
Cast index. A: Initial X-rays of a pediatric forearm fracture with angulation; B: Immediate post-reduction X-rays demonstrating an appropriate cast application based on the cast index (< 0.8). Cast index = Saggital width/coronal width = 41.4 mm/54.4 mm = 0.76.
Applying the index layer of fiberglass is crucial to ensuring a proper fit to the child’s extremity. It is also important when needing a mold. If the index layer is applied too loosely, the cast will slide on the extremity when applying the mold and ultimately cause displacement of where the mold was originally intended for (Figure 3). However, if the index layer is applied too tightly, the obvious concern is soft tissue and vascular compromise. Our recommendation is that the material, whether plaster or fiberglass, be “un-rolled” onto the extremity to be casted and not pulled onto or wrapped in a fashion that can be constricting.
Figure 3.

Loose cast. Pediatric cast that was applied too loosely. The physician’s hand (right) was able to pull the cast off the child easily.
CAST VALVING AND PADDING
Cast valving and spreading is a technique that is employed in an attempt to alleviate pressure within a cast[9,10,19,24]. A cast valve is performed using a cast saw to create a longitudinal linear cut parallel to the long axis of the limb. The cut is either left open with or without a space holder and may be secured by tape. This technique is commonly used after an acute injury, closed reduction, or immediately after surgical fixation all scenarios where the treated limb is at risk for further swelling.
Roberts et al[6] performed a biomechanical study that evaluated the amount of pressure reduction after valving a cast in relation to different casting material. They compared effects of cotton, synthetic, and waterproof padding in addition to the effects of overwrapping a valved cast with an elastic bandage. They concluded that valving a cast with cotton padding beneath resulted in the greatest amount pressure reduction when compared to synthetic and waterproof padding and concluded that cotton padding demonstrated the greatest change in pressure within a long-arm cast after undergoing a bivalve. They stated that synthetic and waterproof cast padding should not be used in the setting of an acute fracture to accommodate swelling. Our custom and practice has been to use cotton padding in all instances because of its ease of use, ability to mold and trim in addition to better pressure reduction after valving as shown by Roberts et al[6].
In warm climates especially during warmer months waterproof material is also an acceptable option especially when caring for sub-acute or non-displaced fractures. Robert et al[25] designed a study that compared casts lined with cotton vs water-proof liners and their effectiveness on maintaining pediatric distal forearm fractures. The results showed that there was no significant difference in amount of displacement and angulation at final follow-up between the two groups and that waterproof liners were equally as effective in maintaining reduction.
When considering univalving vs bivalving, this decision is based on how much swelling the practitioner expects from the injury. Most low-to-medium energy trauma can be treated with a univalve, however children that have undergone a high-energy mechanism trauma, bivalving should be strongly considered in cases where casting is preferred over splinting. Zaino et al[24] performed a study comparing the most effective method in decreasing method in reducing cast pressure in fiberglass casts. Their study concluded that the triple cut method which included bivalving, spreading, and cutting the cotton padding was the most effective in reducing clinically relevant skin pressure[24].
Another useful tool that can be used when valving a cast are commercially available cast spacers (Figure 4). These cast spacers are inserted in the valved area and are taped circumferentially around the cast. The purpose of the spacer is to maintain a constant spread in the cast material and diminish underlying pressure. The commercially available spacer we typically use has four different inserts that differ in size (3, 6, 9 or 12 mm) in which the provider can adjust the size of the space. Kleis et al[26] recently presented their experimental findings after investigating the utility of spacer placement after cast valving. In their study model they reported reduction or pressure by 34% to 95% depending on the setting of the spacer. They recommended using Position #2 for most scenarios as it reduces pressure by an average of 78% but does not weaken the cast. For high energy traumas, Position #3 would be a safer option to prevent excessive compartment pressures.
Figure 4.
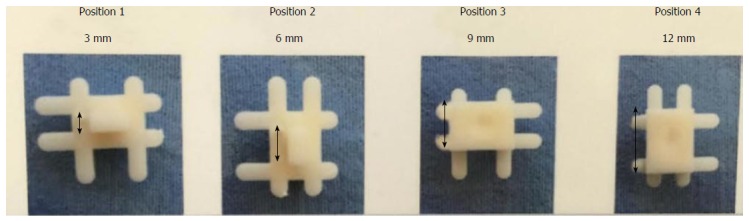
Cast spacers. Cast spacers with four different size settings (3, 6, 9 and 12 mm).
It is customary for us to use cast spacers in every valved cast most often in the 6 mm position.
THERMAL INJURY
Burns caused after cast application have been studied in recent reports[27,28]. The curing of the cast material itself is exothermic and heat producing. Although the occurrence is not a commonly encountered complication, an unnecessary heat exposure to the child can be uncomfortable and stressful. The risk of thermal injuries may be increased when the temperature of the dip water for the cast material exceeds > 50 °C or when the cast is too thick > 24-ply[27,28].
Accurately measuring the dip water immediately prior to each cast application is possible but not highly feasible in most clinical scenarios. Dip water temperature should be warm to the touch similar to the temperature customary when bathing an infant. Although using warmer temperatures will allow the cast to harden at a faster rate, practitioners need to be aware that higher water temperature will increase the risk of thermal injury.
Cast thickness greater than 24-ply is difficult to achieve on most standard casts however the areas that are of concern are located on the concavities and flexion creases of the extremity. A natural surface area discrepancy is present when a cast is placed across a joint that is not in pure extension. These locations include the dorsal aspect of the ankle joint, posterior knee joint, and antecubital fossa of the elbow joint. In these locations a 1:2, concave: Convex ratio is recommended when applying material in these areas. This will prevent excess layers in the areas that are prone to thermal injury.
Another important aspect of preventing thermal injury during casting is to ensure the cast is completely hardened before supporting the extremity on a pillow or soft blanket[27]. If the un-hardened cast is placed on a pillow, the heat generated from the exothermic reaction in the material will be smothered, heat escape limited and the potential for thermal injury is increased.
PREVENTING A WET CAST
When a cast becomes wet, numerous complications can occur, which include skin maceration, infection, and disruption of the structural integrity of the cast[29]. Although educating the patient and family regarding the importance of protecting their cast and keeping it dry is paramount the incidence of a wet cast still continues to be problematic[17]. Currently, there are various methods and products whose purpose is to help prevent casts from becoming wet. These methods include commercially available cast protectors, waterproof liners, and a combination of household products.
McDowell et al[30] compared these various methods on their effectiveness in preventing water absorption when applied to a cast. In addition, they also evaluated the most cost effective method. They found that all of the methods provided some level of protection when the cast in their experimental model was exposed to water. They concluded that although abstaining from contact with water is the most prudent approach, if a cast cover is to be used, double plastic bags with duct tape (100% prevention, $10) and the store bought cast protector (100% prevention, $13) were their preferred contemporary methods to prevent a wet cast.
Waterproof padding or cast liners are another option for children to allow bathing or water based activities while in a cast. We have often found that the adding cost of these materials are not covered by most commercial insurers in the United State and often the cost of these materials are transferred to the patient and family.
It is the utmost importance to remind patients and guardians to prevent the cast from becoming wet. Many times the complications from a wet padding can be unnoticed and will not be discovered until the final follow-up when the cast is removed. In order to prevent further skin complications that can lead to significant infection and injury, educating the parents on signs of wound infection such as deterioration of the fiberglass or a strong malodor from the cast must be performed.
SKIN COMPLICATIONS
Skin complications from cast application is a common occurrence that can range from minor skin excoriations to severe pressure ulcers that can eventually require surgical debridement and coverage[31]. There are only several studies published that focused solely on pediatric skin complications associated with casting[12,31].
Many of the skin complications we have encountered in the clinic or emergency department were likely due to poor cast padding. In order to prevent pressure ulcers, it is important to be aware of the locations of the extremity that have notable protuberances (i.e., fibular head, heel, femoral epicondyles, etc.). At these areas, more padding needs to be placed to prevent excessive pressure. Difazio et al[31] published a recent study on reducing the incidence of casted-related skin complications, more specifically heel pad ulcers. Through adding extra padding at the heel area in addition to respective provider education, they decreased the incidence of casted-related skin complications from 17.1 per 1000 lower extremity casts to 6.8.
CAST REMOVAL
The use of cast saws have brought much attention in the orthopedic literature[1-4,7,24,32,33]. These studies have focused mainly on the complications that come with using the saw. Although they are routinely advertised to patients and their families that it is only intended to cut the fiberglass and not the child’s skin, cast saws can still result in thermal injuries and abrasions.
Shuler et al[4] recently evaluated factors that prevented excessive increase in temperatures when using a cast saw blade. What they found was significant was the amount of cast padding and the relationship with temperature. They recommended four layers, as opposed to two, when applying the padding. This adjustment helped decrease the temperature by 8.0 °C.
Killian et al[3] provided another study that evaluated multiple factors that contribute to thermal injuries from cast saw use. In this study they compared thickness of casts, dullness of blades, and experience of cast saw users. What they concluded was that frequent changes to cast blades, cast thickness to be less than 3/8 inch, and a heightened sense of awareness on the temperature of the blade during cast saw use were important clinical factors that can prevent thermal injuries. They included a tip on how to gauge cast-saw blade temperature which was that if the user is unable to hold the blade with two fingers for longer than 5 s the blade is too hot.
Several articles on cast saw complications have emphasized the importance of the user’s experience[2,3,7,32]. Just like any new procedure, it has been studied that an inexperienced user can cause significant harm to the child if not done correctly. Brubacher et al[32] developed a cast removal training simulation using a fracture model and experimenting it with various levels of orthopedic attendings and residents. As expected, the more experience surgeons resulted in lower mean peak temperatures after cast removal. What they also discovered was that the beginner and intermediate groups were able to achieve progressively decreasing mean temperatures after they experienced more trials with the simulator. In addition, the study displayed the potential benefits of using a simulation workshop to allow providers of all skill levels to develop experience and comfort when using a cast saw.
At our institution, we strictly emphasize the importance of cast saw use. Our cast-saw blades are routinely checked on a weekly basis and a “blade status/change log” is maintained by our orthopedic technicians.
Using a Saw Stop© protective strip (Figure 5) is another way to further protect the limb from the cast saw during removal. The strip is placed directly over the webril layer on the side that the cast saw will cut. The fiberglass is then layered on top of the protective strip and the cast saw user is now able to cut through the fiber glass without risk of contacting the skin because of the added protection layer. They are crucial to use if the person removing the cast is unsure of the quality integrity or even the presence of soft roll beneath the cast material. Having a dedicated formal teaching session(s) in place and a practical exam is recommended prior to allowing practitioner in any medical setting use a cast saw to remove a cast in any patient.
Figure 5.
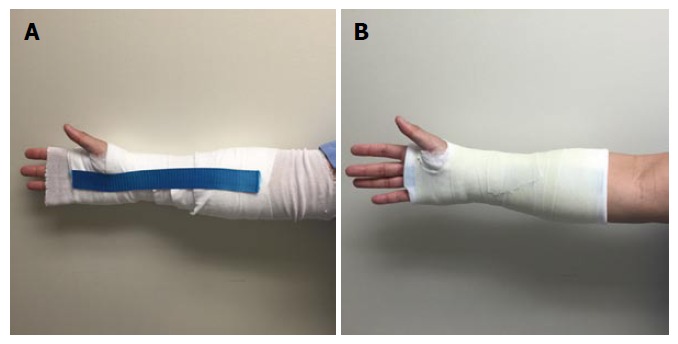
Saw Stop© protective strip (A and B). This protective strip is placed on top of the webril layer before applying the fiberglass cast roll. The strip provides a durable protective layer for the cast saw to cut over.
PATIENT EDUCATION
Equally as important as all the factors above when applying a cast, is the detailed patient education on how patients and patient’s family can maintain this cast. As common as cast application and maintenance is for orthopedic surgeons, it is easily forgotten on how novel this treatment is for the patient and their families. Thus, emphasizing the “do’s and don’ts” of cast care is imperative on preventing complications.
DiPaola et al[34] designed a prospective study on documenting the incidence and etiology related to unplanned cast changes. What they discovered was that the major reason for unplanned cast changes wasn’t because of the technique of the cast application but rather patient non-adherence to instructions or lack of education on maintaining it.
The importance of patient education must be emphasized. After each cast application, the practitioner should have a discussion with the child and family that touches on numerous factors on cast care maintenance that should include how to prevent cast from becoming wet, avoiding inserting objects into the cast and how to handle certain irritating symptoms such as itchiness. Patients are provided with an educational handout on how to best care for their cast and it is translated into their native language when necessary.
CONCLUSION
Casting was one of the first methods of fracture treatment and remains as one of the most common modes of treatment. Perfecting the art of casting remains crucial in ensuring optimal patient outcomes and preventing significant healthcare expenses related to complications.
The ideal cast has a long list of factors that need to be considered to ensure a high quality of patient care. A good cast should immobilize the extremity, remain comfortable, and not cause complications. These factors include the type of cast material and how much padding to apply at certain areas of the extremity. Afterwards, educating the patient and family on how to prevent the cast from getting wet will assist in maintenance, comfort and anxiety. Finally, learning how to properly use a cast saw to prevent thermal injury are just a few notable aspects of providing an optimal cast experience.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
Conflict-of-interest statement: Authors declare no conflict of interests for this article.
Peer-review started: April 29, 2016
First decision: June 17, 2016
Article in press: July 22, 2016
P- Reviewer: Emara K, Matuszewski LS, Vulcano E S- Editor: Ji FF L- Editor: A E- Editor: Li D
References
- 1.Shore BJ, Hutchinson S, Harris M, Bae DS, Kalish LA, Maxwell W, Waters P. Epidemiology and prevention of cast saw injuries: results of a quality improvement program at a single institution. J Bone Joint Surg Am. 2014;96:e31. doi: 10.2106/JBJS.L.01372. [DOI] [PubMed] [Google Scholar]
- 2.Puddy AC, Sunkin JA, Aden JK, Walick KS, Hsu JR. Cast saw burns: evaluation of simple techniques for reducing the risk of thermal injury. J Pediatr Orthop. 2014;34:e63–e66. doi: 10.1097/BPO.0000000000000274. [DOI] [PubMed] [Google Scholar]
- 3.Killian JT, White S, Lenning L. Cast-saw burns: comparison of technique versus material versus saws. J Pediatr Orthop. 1999;19:683–687. [PubMed] [Google Scholar]
- 4.Shuler FD, Grisafi FN. Cast-saw burns: evaluation of skin, cast, and blade temperatures generated during cast removal. J Bone Joint Surg Am. 2008;90:2626–2630. doi: 10.2106/JBJS.H.00119. [DOI] [PubMed] [Google Scholar]
- 5.Large TM, Frick SL. Compartment syndrome of the leg after treatment of a femoral fracture with an early sitting spica cast. A report of two cases. J Bone Joint Surg Am. 2003;85-A:2207–2210. doi: 10.2106/00004623-200311000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Roberts A, Shaw KA, Boomsma SE, Cameron CD. Effect of Casting Material on the Cast Pressure After Sequential Cast Splitting. J Pediatr Orthop. 2015 doi: 10.1097/BPO.0000000000000574. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Ansari MZ, Swarup S, Ghani R, Tovey P. Oscillating saw injuries during removal of plaster. Eur J Emerg Med. 1998;5:37–39. [PubMed] [Google Scholar]
- 8.Weiss AP, Schenck RC, Sponseller PD, Thompson JD. Peroneal nerve palsy after early cast application for femoral fractures in children. J Pediatr Orthop. 1992;12:25–28. [PubMed] [Google Scholar]
- 9.Mohler LR, Pedowitz RA, Byrne TP, Gershuni DH. Pressure generation beneath a new thermoplastic cast. Clin Orthop Relat Res. 1996;(322):262–267. [PubMed] [Google Scholar]
- 10.Garfin SR, Mubarak SJ, Evans KL, Hargens AR, Akeson WH. Quantification of intracompartmental pressure and volume under plaster casts. J Bone Joint Surg Am. 1981;63:449–453. [PubMed] [Google Scholar]
- 11.Mubarak SJ, Frick S, Sink E, Rathjen K, Noonan KJ. Volkmann contracture and compartment syndromes after femur fractures in children treated with 90/90 spica casts. J Pediatr Orthop. 2006;26:567–572. doi: 10.1097/01.bpo.0000230329.06460.f7. [DOI] [PubMed] [Google Scholar]
- 12.Wolff CR, James P. The prevention of skin excoriation under children’s hip spica casts using the goretex pantaloon. J Pediatr Orthop. 1995;15:386–388. doi: 10.1097/01241398-199505000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez DL. Closed manipulation and casting of distal radius fractures. Hand Clin. 2005;21:307–316. doi: 10.1016/j.hcl.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Webb GR, Galpin RD, Armstrong DG. Comparison of short and long arm plaster casts for displaced fractures in the distal third of the forearm in children. J Bone Joint Surg Am. 2006;88:9–17. doi: 10.2106/JBJS.E.00131. [DOI] [PubMed] [Google Scholar]
- 15.Ferguson J, Nicol RO. Early spica treatment of pediatric femoral shaft fractures. J Pediatr Orthop. 2000;20:189–192. [PubMed] [Google Scholar]
- 16.Illgen R, Rodgers WB, Hresko MT, Waters PM, Zurakowski D, Kasser JR. Femur fractures in children: treatment with early sitting spica casting. J Pediatr Orthop. 1998;18:481–487. [PubMed] [Google Scholar]
- 17.Sawyer JR, Ivie CB, Huff AL, Wheeler C, Kelly DM, Beaty JH, Canale ST. Emergency room visits by pediatric fracture patients treated with cast immobilization. J Pediatr Orthop. 2010;30:248–252. doi: 10.1097/BPO.0b013e3181d213bc. [DOI] [PubMed] [Google Scholar]
- 18.Newton PO, Mubarak SJ. Financial aspects of femoral shaft fracture treatment in children and adolescents. J Pediatr Orthop. 1994;14:508–512. doi: 10.1097/01241398-199407000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Halanski M, Noonan KJ. Cast and splint immobilization: complications. J Am Acad Orthop Surg. 2008;16:30–40. doi: 10.5435/00124635-200801000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Iltar S, Alemdaroğlu KB, Say F, Aydoğan NH. The value of the three-point index in predicting redisplacement of diaphyseal fractures of the forearm in children. Bone Joint J. 2013;95-B:563–567. doi: 10.1302/0301-620X.95B4.31143. [DOI] [PubMed] [Google Scholar]
- 21.Kamat AS, Pierse N, Devane P, Mutimer J, Horne G. Redefining the cast index: the optimum technique to reduce redisplacement in pediatric distal forearm fractures. J Pediatr Orthop. 2012;32:787–791. doi: 10.1097/BPO.0b013e318272474d. [DOI] [PubMed] [Google Scholar]
- 22.Chess DG, Hyndman JC, Leahey JL, Brown DC, Sinclair AM. Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop. 1994;14:211–213. doi: 10.1097/01241398-199403000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Edmonds EW, Capelo RM, Stearns P, Bastrom TP, Wallace CD, Newton PO. Predicting initial treatment failure of fiberglass casts in pediatric distal radius fractures: utility of the second metacarpal-radius angle. J Child Orthop. 2009;3:375–381. doi: 10.1007/s11832-009-0198-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zaino CJ, Patel MR, Arief MS, Pivec R. The effectiveness of bivalving, cast spreading, and webril cutting to reduce cast pressure in a fiberglass short arm cast. J Bone Joint Surg Am. 2015;97:374–380. doi: 10.2106/JBJS.N.00579. [DOI] [PubMed] [Google Scholar]
- 25.Robert CE, Jiang JJ, Khoury JG. A prospective study on the effectiveness of cotton versus waterproof cast padding in maintaining the reduction of pediatric distal forearm fractures. J Pediatr Orthop. 2011;31:144–149. doi: 10.1097/BPO.0b013e318209d83a. [DOI] [PubMed] [Google Scholar]
- 26.Kleis K, Schlechter JA, Doan A, Farnsworth CL, Edmonds EW. Under Pressure: The Utility of Splitting Fiberglass Casts. Orthopedic Trauma Association, 2015. doi: 10.1097/BPO.0000000000000961. [DOI] [PubMed] [Google Scholar]
- 27.Gannaway JK, Hunter JR. Thermal effects of casting materials. Clin Orthop Relat Res. 1983;(181):191–195. [PubMed] [Google Scholar]
- 28.Lavalette R, Pope MH, Dickstein H. Setting temperatures of plaster casts. The influence of technical variables. J Bone Joint Surg Am. 1982;64:907–911. [PubMed] [Google Scholar]
- 29.Berman AT, Parks BG. A comparison of the mechanical properties of fiberglass cast materials and their clinical relevance. J Orthop Trauma. 1990;4:85–92. doi: 10.1097/00005131-199003000-00015. [DOI] [PubMed] [Google Scholar]
- 30.McDowell M, Nguyen S, Schlechter J. A Comparison of Various Contemporary Methods to Prevent a Wet Cast. J Bone Joint Surg Am. 2014;96:e99. doi: 10.2106/JBJS.M.00203. [DOI] [PubMed] [Google Scholar]
- 31.Difazio RL, Harris M, Feldman L, Mahan ST. Reducing the Incidence of Cast-related Skin Complications in Children Treated With Cast Immobilization. J Pediatr Orthop. 2015 doi: 10.1097/BPO.0000000000000713. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 32.Brubacher JW, Karg J, Weinstock P, Bae DS. A Novel Cast Removal Training Simulation to Improve Patient Safety. J Surg Educ. 2016;73:7–11. doi: 10.1016/j.jsurg.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 33.Nielsen DM, Ricketts DM. Where to split plaster casts. Injury. 2005;36:588–589. doi: 10.1016/j.injury.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 34.DiPaola MJ, Abzug JM, Pizzutillo PD, Herman MJ. Incidence and etiology of unplanned cast changes for fractures in the pediatric population. J Pediatr Orthop. 2014;34:643–646. doi: 10.1097/BPO.0000000000000191. [DOI] [PubMed] [Google Scholar]


