Abstract
Background
With the movement towards bundled payments, stakeholders should know the true cost of the care they deliver. Time-driven activity-based costing (TDABC) can be used to estimate costs for each episode of care. In this analysis, TDABC is used to both estimate the costs of anesthesia care and identify the primary drivers of those costs of 11 common oncologic outpatient surgical procedures.
Methods
Personnel cost were calculated by determining the hourly cost of each provider and the associated process time of the 11 surgical procedures. Using the anesthesia record, drugs, supplies and equipment costs were identified and calculated. The current staffing model was used to determine baseline personnel costs for each procedure. Using the costs identified through TDABC analysis, the effect of different staffing ratios on anesthesia costs could be predicted.
Results
Costs for each of the procedures were determined. Process time and costs are linearly related. Personnel represented 79% of overall cost while drugs, supplies and equipment represented the remaining 21%. Changing staffing ratios shows potential savings between 13-28% across the 11 procedures.
Conclusions
TDABC can be used to estimate the costs of anesthesia care. This costing information is critical to assessing the anesthesiology component in a bundled payment. It can also be used to identify areas of cost savings and model costs of anesthesia care. CRNA to anesthesiologist staffing ratios profoundly influence the cost of care. This methodology could be applied to other medical specialties to help determine costs in the setting of bundled payments.
Introduction
As our nation moves to redesign healthcare delivery and reimbursement the concept of value is gaining ever increasing attention. Michael Porter defines value in healthcare as the balance between outcomes that matter to patients and the cost to achieve those outcomes1 Alternative payment models include bundled-payment arrangements where health care providers are accountable for the outcomes and cost of the care they deliver to patients2. As we transition away from our current model of reimbursement health care organizations need to have a better understanding of their outcomes and their costs of care.
Most healthcare costing systems are based upon charges yet cost shifting has made most charge-based systems unreliable when used to measure costs3. In 2004, Kaplan and Anderson introduced a new approach to activity based costing called time-driven activity based costing (TDABC) which uses estimates of resource consumption during business activities to measure costs of services4. Recently, TDABC has been applied to healthcare to develop more accurate estimates of healthcare costs5,6.
Anesthesia is one of the most costly aspects of healthcare delivery. In a 2011 report, the Healthcare Cost Institute found that anesthesia care had the highest average price per service for a professional procedure7. Previously, anesthesia cost assessments have been tied to coding systems for reimbursement, such as the American Society of Anesthesiologists (ASA) classification or American Society of Anesthesiologists' Relative Value Scale system 8. Anesthesia cost assessments focused on differences in anesthesia technique, personnel costs, staffing models, and budgets related to physician salaries, equipment, drugs and service contracts 9,10. Other studies have described anesthesia cost drivers and proposed alternative costing methodologies to assess hospitals' costs of anesthesia care9,11. A study from Serbia reported the use of activity-based costing to quantify anesthesia costs. It found 40% of direct costs related to personnel salaries, 32% to drugs and supplies, and 28% on other costs such as analyses and equipment 12.
The current method for billing anesthesia services includes a time component; however, this is combined with two other procedure and patient related factors that may or may not correlate to the actual cost of anesthesia. Anesthesia professional billing is unique because it is the only professional service that uses time as a component of its billing methodology. All other professional services (e.g. surgery) bill for visits and procedures.
Currently, the anesthesia charge results from the creation of two separate charges – professional charge and facility charge. Anesthesia charge covers pre-operative anesthesia assessment, delivery of anesthesia and immediate postoperative care. Professional charges comprise three units: Base Unit, Time Unit, and Special Units. Assigned by the ASA, Base Unit relates to surgery procedure type and difficulty level to deliver anesthesia. The Time Unit is the time anesthesia care starts to the end of the surgical case. Most insurance carriers and Centers for Medicare & Medicaid Services (CMS) assign 15 minutes to each Time Unit. Special Units may be added for several complicating conditions. Examples include patients of extreme age (e.g. less than one year old) or anesthesia complicated by patient acuity (e.g. ASA status). The final professional charge is determined by adding Base, Time, and Special Units together. Professional practices determine the charge per unit. The total professional charge is the Total Units multiplied by per unit charge.
The facility charge for anesthesia services is related to supplies, equipment, time of technical personnel used to support the service and overhead. Its calculation methodology is less proscriptive than the professional charge. At this institution, the facility charge is determined by two factors: location of anesthesia service and anesthesia time associated with the case. All related, allowed expenses are bundled into this charge.
For a bundled payment, costs of anesthesia care will be built into the reimbursement for a specific surgical procedure or a longer episode of care and paid in the form of a lump sum to the healthcare provider and/or provider organization. Most anesthesiologists and anesthesia provider organizations have independent billing relationships with insurance companies and CMS. In a bundled payment model, the internal allocation of the single payment will most likely reflect the proportional costs of the care delivered by all services. Therefore, anesthesiologists and all stakeholders need costing systems that accurately define costs of the care as internal negotiations for their portion of the bundled payment begin.
Our institution has used a form of activity-based costing known as time-driven activity-based costing (TDABC)4 to assess the costs of patient care cycles within the head and neck center and preoperative assessment center5,6. In this study, TDABC estimates the cost of the entire episode of anesthesia care for 11most commonly performed outpatient oncologic surgical procedures. The objective was to quantify the anesthesia costs for each outpatient oncologic surgical procedure, define the distribution of those costs and identify cost drivers. Once the predominant cost driver was defined, different staffing ratios were modeled to better understand how these scenarios affected anesthesia costs. The overall goal was to estimate the costs of anesthesia care using the TDABC methodology for a proposed bundled payment system.
Methods
Process maps of anesthesia care for 11 most commonly performed outpatient oncologic surgical procedures were created as seen in Figure A. Process times were either estimated or measured directly. Anesthesia providers and staff estimated clinical process time directly associated with the patient for the first of the three phases shown in the process map - the Pre-Procedure Phase. The other two phases, Operating Room and Post-Anesthesia Care Unit, times were derived from the anesthesia record.
Figure A. Process Map for Outpatient Oncologic Surgical Procedures- Overview.
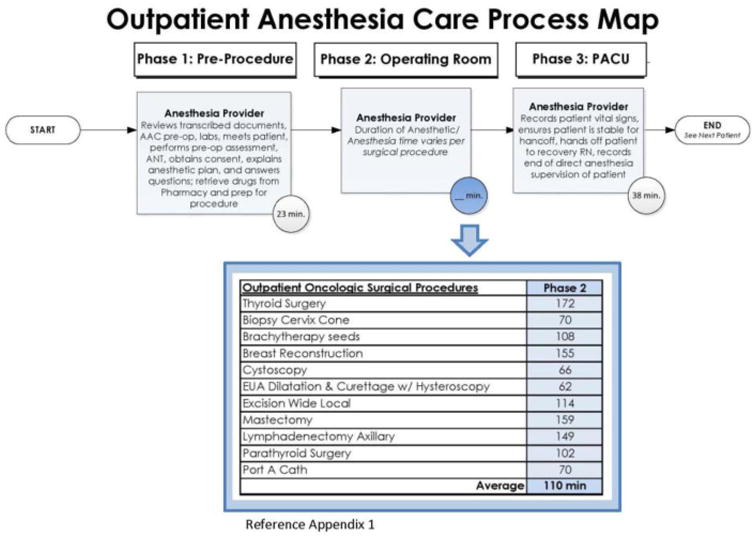
Time-driven activity based costing process maps of anesthesia patient care were created for each of the 11 most commonly performed outpatient oncologic surgical procedures.
Preliminary data was extracted from the institution's perioperative electronic health record1, billing database2, financial database3, and the pharmacy database4. We evaluated 5,357 outpatient anesthesia cases across 261 procedure codes. At the discretion of anesthesia providers, procedures were grouped by common procedure terminology codes (Appendix 1). The resulting 11 procedure groups were generated: thyroid surgery (n=221), mastectomy (n=1242), breast reconstruction (n=567), lymphadenectomy axillary (n=100), excision wide local (n=443), parathyroid surgery (n=93), brachytherapy seeds (n=88), biopsy cervix cone (n=172), cystoscopy (n=953), port-a-cath (n=1348) and exam under anesthesia (EUA) dilatation and curettage with hysteroscopy (n=130) (Table 1). Anesthesia providers and administrators defined the following cost drivers for analysis: anesthesia personnel, drug, supplies and equipment depreciation. Indirect costs were excluded.
Table 1. Distribution of Defined Cost Drivers by Outpatient Oncologic Surgical Procedure Groups.
The distribution of costs by defined cost drivers are shown below for each outpatient oncologic surgical procedure group.
| Outpatient Oncologic Surgical Procedures | N | % Personnel | % Drugs | %Supplies | %Equipment |
|---|---|---|---|---|---|
| Thyroid Surgery | 221 | 79% | 16% | 3% | 1% |
| Mastectomy | 124 2 | 83% | 13% | 3% | 1% |
| Breast Reconstruction | 567 | 80% | 15% | 4% | 1% |
| Lymphadenectomy Axillary | 100 | 83% | 12% | 4% | 1% |
| Excision Wide Local | 443 | 83% | 11% | 4% | 2% |
| Parathyroid Surgery | 93 | 81% | 13% | 5% | 2% |
| Brachytherapy seeds | 88 | 81% | 12% | 5% | 2% |
| Biopsy Cervix Cone | 172 | 77% | 15% | 6% | 2% |
| Cystoscopy | 953 | 71% | 21% | 6% | 2% |
| Port A Cath | 134 8 | 78% | 14% | 6% | 2% |
| EUA Dilatation & Curettage w/ Hysteroscopy | 130 | 75% | 16% | 6% | 2% |
| 5357 | 79% | 15% | 4% | 2% |
Personnel Costs
To determine the per-minute cost for each anesthesia team member, a model of the current staffing ratio was created that identified the total full-time evaluates (FTE) required to staff the outpatient operating room (OR). For analysis, the average length of a workday in the OR was defined as the time between scheduled start and average maximum anesthesia end time plus and additional to account for patient and discharge. This was determined to be 10 hours and 44 minutes. The staffing model was based on an anesthesia-staffing ratio of one anesthesiologist providing medical direction to two CRNA's. The total FTE's needed to staff the OR also included non-productive time (e.g. Sick Leave). Non-productive time was derived from the average of the group over the period of a year. Using average length of day Non-productive time and staffing ratios the total number of FTE's required for anesthesia services is determined. From the general ledger, total annual personnel costs were divided by total FTE's to calculate the cost/FTE/year. To calculate cost per minute for each resource the cost/FTE/year was divided by the product of average total minutes for a length of day (644 minutes) and the number of workdays (250 days). The result was the cost rate/minute/FTE. Cost rates were derived for all anesthesia providers involved in direct patient care: anesthesiologist, CRNA's, anesthesia and supply technicians. Using a process map (Figure A), personnel costs were derived for each outpatient oncologic surgical procedure. The total anesthesia process time included three phases: Phase 1: Pre-Procedure, average duration of 23 minutes; Phase 2, Operating Room, average durations 62-172 minutes; and Phase 3, Post-Anesthesia Care Unit, average duration of 38 minutes.
Drug Cost
Patient pharmacy data was matched with institutional drug acquisition costs to determine the per-case cost of all drugs, fluids and inhalation agents delivered. These costs varied by case type and provider.
Supply & Equipment Depreciation Costs
Average annual supply cost per case rate was derived from the general ledger then applied to each procedure. Total anesthesia equipment depreciation for the study period was identified from the general ledger and allocated equally to each case.
Average Estimated Total Anesthesia Patient Care Costs
The estimated total costs for each of the 11 surgical procedure groups were calculated by adding the weighted averages of each case within each procedure group. Costs include personnel, drug, supply and equipment. Average total cost for each of the common oncologic surgical procedures is depicted with standard deviations in Figure B. All costs are reported as normalized ratios to the lowest total TDABC in all three proposed staffing models to allow for relative cost comparisons (Table 2).
Figure B. Cost of Anesthesia Patient Care for Outpatient Oncologic Surgical Procedures.
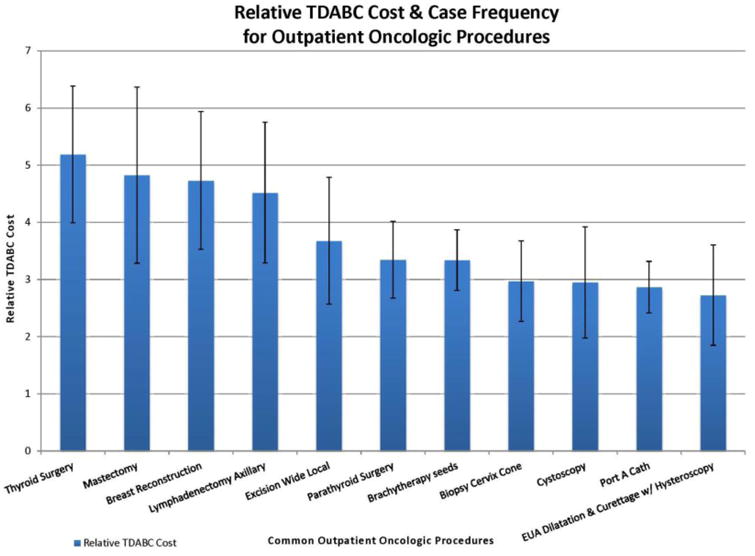
The graph displays the average total cost for the 11 common outpatient oncologic surgical procedures; total costs include personnel, drug, and supply and equipment costs. The average cost for each of the common oncologic surgical procedures is depicted with standard deviations. Costs are reported as normalized ratios.
Table 2. Current and Projected Anesthesia Patient Care Costs.
The current and projected relative cost per procedure for each staffing model are shown with projected change in cost.
| Outpatient Oncologic Surgical Procedure | 2 CRNA : 1MD | 3 CRNA : 1MD | 6 CRNA : 1MD | ||
|---|---|---|---|---|---|
| Relative Cost per Procedure (baseline) | Relative Cost per Procedure | % Change (from baseline) | Relative Cost per Procedure | % Change (from baseline) | |
| Thyroid Surgery | 5.19 | 4.46 | -14.0% | 3.74 | -28.0% |
| Mastectomy | 4.83 | 4.12 | -14.6% | 3.42 | -29.2% |
| Breast Reconstruction | 4.73 | 4.06 | -14.2% | 3.39 | -28.3% |
| Lymphadenectomy Axillary | 4.52 | 3.86 | -14.7% | 3.20 | -29.3% |
| Excision Wide Local | 3.68 | 3.14 | -14.6% | 2.60 | -29.2% |
| Parathyroid Surgery | 3.35 | 2.87 | -14.2% | 2.40 | -28.4% |
| Brachytherapy seeds | 3.34 | 2.86 | -14.4% | 2.38 | -28.7% |
| Biopsy Cervix Cone | 2.97 | 2.56 | -13.7% | 2.16 | -27.3% |
| Cystoscopy | 2.95 | 2.58 | -12.6% | 2.21 | -25.1% |
| Port A Cath | 2.87 | 2.47 | -13.8% | 2.08 | -27.5% |
| EUA Dilatation & Curettage w/ Hysteroscopy | 2.73 | 2.36 | -13.3% | 2.00 | -26.6% |
Projected Anesthesia Patient Care Costs
Projected costs were calculated by changing the ratio of CRNA-to-anesthesiologist, from the current model of 2:1 to models of both 3:1 and 6:1. Each of these models change the per-minute cost of the personnel variable in the total cost of anesthesia patient care. The two resulting personnel cost per minute values were then inserted into the existing TDABC based process map to determine and quantify the change in costs.
Statistical Analysis
Eleven of the most common outpatient oncological procedure categories were developed with multiple procedure codes within each group (Appendix 1). Descriptive and quantitative statistical analyses were used to describe the nature of cost data and illustrate the quantitative measure of correlation between time and costs. Mean of relative TDABC cost was calculated for each procedure category for comparison. Standard deviation was calculated for each procedure category to evaluate variability of costs due to case difference within one category. Correlation coefficient was tested to evaluate potential relationships between relative costs and total process time for all cases in the 11 most common outpatient oncologic procedures categories5. This analysis help to illustrate the portion distribution of costs across four predominant cost drivers.
Results
Relative TDABC mean and standard deviation were compared for eleven common outpatient oncologic surgical procedure categories in Figure B. Estimated cost for thyroid surgery procedures topped the list with a relative cost mean of 5.19. EUA sDilation/Curettage/Hysteroscopy was estimated least costly with a relative cost mean of 2.73. The standard deviation showed variation of costs within each procedure group was relatively small, largest value of 1.54 for mastectomy procedures. The case frequency distribution was unbalanced among the 11procedure groups with a maximum 1348 Port-A-Cath procedures and minimum 88 cases of brachytherapy seeds.
The correlation coefficient was computed between the cost mean and process time mean among eleven procedure groups in Figure C. A strong correlation is seen between the total relative cost and total process time for each procedure with an R2 value of 0.9461 and p-value of less than 0.05.
Figure C. Relationship between Anesthesia Patient Care Cost and Process Time.
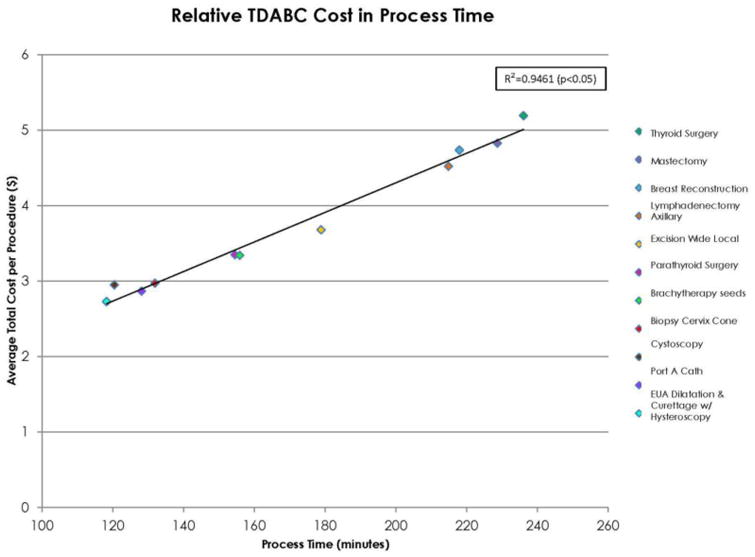
There is a positive correlation between the relative cost and total process time for all cases in the 11 common outpatient oncologic surgical procedure groups. Costs are reported as normalized ratios.
Table 1 showed cost distribution of four predominant cost drivers for each of the eleven outpatient oncologic surgical procedure categories. The dominant cost driver was personnel, which accounted for 79% of the total costs, followed by drugs (15%), supplies (4%) and equipment (2%).
Modeling changes to personnel, by substituting different CRNA to anesthesiologist staffing ratios; Table 2, shows current and projected anesthesia patient care relative costs. These changes show projected cost decreases between 13-28%.
Discussion
While there is generalized assumption that personnel is the most costly area of anesthesia care, this study provides new insight into the cost breakdown by quantifying the very large component of personnel costs(79%)compared to the small contribution of all other anesthesia related costs (21%). It provides a costing framework that can be applied to other specialties that supervise midlevel providers, such as advanced practice nurses, physician's assistants, and residents in training. A basic concept of care redesign is that each provider work to the highest level of their degree and training. Applying TDABC to other clinical care settings could help to design care that is less costly. Mapping clinical processes across specialties could highlight other areas for cost savings across an institution or multi-specialty practice in addition to the optimization of staffing ratios of all MD to MLP's illustrated by the anesthesia example in this study. TDABC is a tool to help predict cost savings prior to implementing change. However, in all care redesign the outcomes of that care must be evaluated to be sure that less costly care does not diminish the quality of the care provided. Further investigations need to be developed to study how various staffing ratios within anesthesia and other healthcare specialties affect outcomes.
TDABC identifies areas of potential cost savings
Personnel was identified as the primary driver of cost and quantified the relationship between personnel cost and total surgical procedure process time. Opportunity to potentially decrease costs exists via two pathways, decrease overall process time or increase productivity of the personnel. This study assessed augmenting personnel productivity by increasing the number of CRNA's each anesthesiologist would supervise, or staffing ratios. Using TDABC, proposed changes to the current 2:1 staffing ratio were applied to assess the total costs for each procedure using 3:1 and 6:1 staffing ratios. These proposed changes modeled potential cost savings between 13-28%, depending on the specific surgical procedure.
Although various CRNA staffing models have not been found to be associated with increased risks to patients13, our study acknowledges that serious thought must continue to go into determining the anesthesia staffing that is appropriate given the complexity of patient comorbidities and case acuity. This study does not presume to suggest there is one best staffing model, or that the most cost saving ratio should be applied in all scenarios. Proper matching of patients and cases with anesthesiologists and CRNA's is essential. In addition to modeling different staffing ratios for CRNA's, this form of analysis can be used to evaluate the costs of care provided by other physician extenders in the operating room such as anesthesia assistants and anesthesia residents. In all situations where care delivery is modified based on cost, it is essential to monitor the outcome of care to be sure that cost reduction does not diminish the quality of care provided.
Secondary cost drivers were identified as drug, supplies and equipment costs. While the contributions of secondary drivers in total comprise just 21% of the overall cost, standardizing and decreasing variability could also lead to decreased costs.
TDABC identifies relationship between anesthesia costs and procedure duration
TDABC illustrates an important connection, the relationship between surgical duration and cost of anesthesia. Phase 2 of the process map (Figure A) contributes the largest amount of time to the total process time, approximately 64%. Phase 2 is almost entirely comprised of the surgical duration, the length of which anesthesia providers have little, if any, control over. Current billing of anesthesia services is based on units of time, thus it is imperative to understand this relationship as reimbursement moves towards bundled payments. How will the anesthesia providers and other healthcare providers negotiate their portion of the payment? How is the payment split if surgical times for the same procedure vary greatly due to surgeon and patient variability? This variation can be seen in this study in the form of the standard deviation shown in Figure B. The standard deviation represents the difference in costs based on different surgeons performing the same procedures. Given this correlation, it would behoove all stakeholders to work towards reducing the variability between surgical times. It remains difficult to determine how this standardization should take place, but as payment reform continues to develop, this relationship needs to be acknowledged and addressed.
Limitations of TDABC to estimate costs and unanticipated consequences of bundled payments
There are limits to the accuracy of TDABC methods. TDABC calculates only direct patient contact time. When reviewing the process map, documented times do not include time salaried anesthesia providers are working but not conducting direct patient care. Assigning costs to a process of care based solely on time spent providing direct patient care could lead to underestimation of provider work load, decreasing reimbursement and compensation. This could lead to provider dissatisfaction and inaccuracy of documentation by providers when not in the presence of patients. Conversely too much focus could be placed on documenting, causing distraction while in the presence of patients in order to add more time to this process step.
Basing models for change and cost saving on models that substitute physicians with mid-level providers could lead to patient dissatisfaction, compromise patient safety, and provider burnout as clinicians are asked to do more in less time. How changing staffing models across all specialties of medicine potentially effect patient safety is an area which needs further study with outcomes data. The correct balance of costs while preserving quality of patient care also warrants further investigation.
The implementation of a bundled payment system requires significant startup costs and effort and must be understood before developing and implementing a bundle. The current billing system does not easily support a bundled payment system and would require, at least in the near term, a second system of accounting and billing. This could create additional expense for the administration of this program. An anesthesia bundle that is developed independently from surgery or postoperative care could also be negatively impacted by surgeons and nursing if they do not share the same incentives.
Also absent from the anesthesia care costs in this study are the basic overhead costs of running the outpatient surgical center. This is a limitation in using this model since these costs are not insignificant. However, TDABC identifies baseline costs, cost drivers and how those contribute to overall patient care costs. TDABC and process mapping will be a useful tool in allocating payments to services in a bundled payment structure. It allows for changes to be modeled and costs visualized prior to implementation, such that the highest level of patient care may be maintained, while continuously assessing ways to improve value.
Acknowledgments
My-Hanh V. Phan, Research Programmer, The University of Texas M. D. Anderson Cancer Center
Gilbert Castro, Application Analyst, The University of Texas M. D. Anderson Cancer Center
Financial Support: This research is supported in part by the National Institutes of Health through M. D. Anderson's Cancer Center Support Grant CA 016672 and the Helen Shafer Fly Endowment fund.
Appendix 1
| Outpatient Oncologic Surgical Procedures | CPT Code | Code Description |
|---|---|---|
| Lymphadenectomy Axillary | 00400 | Biopsy Breast w/ Needle Loc |
| Excision Lesion/ Nodule Breast | ||
| 00912 | Lymphadenectomy Axillary | |
| 01610 | Biopsy Lymph Node Axillary | |
| Lymphadenectomy (Other) | ||
| Mastectomy | 00400 | Biopsy Excisional Breast |
| Mastectomy Prophylactic | ||
| Mastectomy Segmental | ||
| 00402 | Excision Additional Margin Breast | |
| Mastectomy w/ Plastic Recon | ||
| 00404 | Mapping & Biopsy Sentinel Lymph Node (IOLM& SNB) | |
| Mastectomy | ||
| 01610 | Mastectomy Total w/ IOLM SNB | |
| 64421 | Mastectomy Total w/ IOLM SNB w/ Plastic Recon | |
| 99100 | Mastectomy Modified Radical | |
| Mastectomy Segmental IOLM SNB | ||
| Mastectomy Segmental Needle Loc IOLM SNB | ||
| Mastectomy Total | ||
| Excision Wide Local | 00300 | Excision Wide Local Facial Area |
| Excision Wide Local Head | ||
| Excision Wide Local IOLM SNB | ||
| Excision Wide Local Neck | ||
| 00400 | Excision Wide Local IOLM SNB Lower Limb | |
| 01470 | Excision Wide Local Lower Limb | |
| 01610 | Excision Wide Local IOLM SNB Upper Limb | |
| 99100 | Excision Wide Local | |
| Excision Wide Local w/ Laser | ||
| Port A Cath | 00400 | Removal Port A Cath |
| 00532 | Placement Central Venous Catheter | |
| Placement Port A Cath | ||
| Biopsy Cervix Cone | 00840 | Laparoscopic Ligation Fallopian Tube |
| Laparoscopic Salpingo Oophorectomy | ||
| 00940 | Ablation Laser Vagina/ Vulva | |
| Biopsy Cervix | ||
| Biopsy Cervix Cone w/ Cold Knife | ||
| Biopsy Cervix w/ Laser | ||
| Biopsy Cervix w/ LEEP | ||
| Biopsy Vulva Lesion | ||
| Colposcopy | ||
| Excision Lesion Wide Local Vagina | ||
| Excision Lesion Wide Local Vulva | ||
| Insertion Intrauterine Device | ||
| Repair Wound Vagina | ||
| Vaginectomy (Colpectomy) | ||
| 99100 | Biopsy Vaginal Lesion | |
| Colporrhaphy | ||
| Exam Under Anesthesia Vaginal | ||
| EUA Dilatation & Curettage w/ Hysteroscopy | 00940 | EUA Dilatation & Curettage |
| 00952 | EUA Dilatation & Curettage w/ Hysteroscopy | |
| EUA Hysteroscopy | ||
| EUA Hysteroscopy w/ Thermal Ablation | ||
| Parathyroid Surgery | 00320 | Parathyroidectomy |
| 36620 | Parathyroidectomy w/ PTH Assay Studies | |
| Thyroid Surgery | 00100 | Parotidectomy |
| 00320 | Dissection Neck Paratracheal | |
| Dissection Neck Selective | ||
| Lobectomy Thyroid | ||
| Thyroidectomy | ||
| Thyroidectomy w/ Isthmusectomy | ||
| Thyroidectomy w/ Neck Dissection | ||
| 00404 | Dissection Neck | |
| 99100 | Exploration Neck | |
| Thyroidectomy Total | ||
| Breast Reconstruction | 00300 | Revision Flap |
| Transfer or Rearrangement Adjacent Tissue | ||
| 00320 | Reconstruction Acquired Defect | |
| 00400 | Autograft Fat | |
| 00402 | Augmentation Mammoplasty | |
| Capsulectomy | ||
| Capsulotomy | ||
| Exchange Breast Implant | ||
| Exchange Tissue Expander (Other) | ||
| Exchange Tissue Expander to Breast Implant | ||
| Placement Tissue Expander Breast | ||
| Reconstruction Breast w/ Breast Implant | ||
| Reconstruction Nipple (Areola) | ||
| Reduction Mammoplasty | ||
| Release Scar | ||
| Removal Breast Implant Fill Port | ||
| Removal Implanted Breast | ||
| Removal Tissue Expander | ||
| Repositioning Breast Implant | ||
| Revision Breast Reconstruction | ||
| Revision Inframammary Fold | ||
| Revision Nipple Areolar Reconstruction | ||
| Revision Scar | ||
| Revision TRAM Flap | ||
| 99100 | Mastopexy | |
| Brachytherapy seeds | 00902 | Biopsy Prostate |
| 99100 | Implantation Brachytherapy Seed/s | |
| Cystoscopy | 00870 | Cystoscopy |
| Cystoscopy w/ Extraction Bladder Stone | ||
| Ureteroscopy | ||
| 00910 | Cystoscopy (Cystourethroscopy) w/ Rectal EUA | |
| Cystoscopy Biopsy EUA | ||
| Cystoscopy Fulguration Bladder | ||
| Cystoscopy Ureteroscopy | ||
| Cystoscopy w/ Bladder Hydrodistention | ||
| Cystoscopy w/ Insertion Ureteral Stent | ||
| Cystoscopy w/ Retrograde Pyelogram EUA | ||
| Exchange Ureteral Stent(s) | ||
| 00918 | Cystoscopy w/ Laser Lithotripsy | |
| 99100 | Cystoscopy Transurethral Resection Prostate EUA | |
| Cystoscopy TURBT EUA |
Footnotes
Picis®, Optum, Inc. Wakefield, MA.
IDX Systems Corporation. South Burlington, VT.
PeopleSoft®, Oracle, Inc. Redwood Shores, CA.
Pyxis Technologies®, Care Fusion Corporation. San Diego, CA.
StataCorp®, LP. College Station, TX.
Conflict of Interest Statement: The article “Bundled Payments: Measuring the Costs of Anesthesia Care in an Outpatient Oncology Surgery Center Using Time-Driven Activity-Based Costing” is authored by Katy French, Alexis Guzman, Augustin Rubio, John Frenzel and Thomas Feeley and submitted to Healthcare as an original article. Below all authors have disclosed relevant commercial associations that might pose a conflict of interest
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Katy E. French, The University of Texas M. D. Anderson Cancer Center.
Alexis B. Guzman, The University of Texas M. D. Anderson Cancer Center.
Augustin C. Rubio, Division of Anesthesiology & Critical Care, The University of Texas M. D. Anderson Cancer Center.
John C. Frenzel, The University of Texas M. D. Anderson Cancer Center.
Thomas W Feeley, The University of Texas M. D. Anderson Cancer Center; Senior Fellow, Harvard Business School.
References
- 1.Porter ME, Lee TH. The strategy that will fix health care. Harv Bus Rev. 2013;91:50–70. [Google Scholar]
- 2.Burwell SM. Setting Value-Based Payment Goals- HHS Efforts to Improve US Health Care. N Engl J Med. 2015;372:897–9. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev. 2011;89:46–52, 54. 56–61 passim. [PubMed] [Google Scholar]
- 4.Kaplan RS, Anderson SR. Time-driven activity-based costing. Harv Bus Rev. 2004;82:131–8. 150. [PubMed] [Google Scholar]
- 5.French KE, Albright HW, Frenzel JC, Incalcaterra JR, Rubio AC, Jones JF, Feeley TW. Measuring the value of process improvement initiatives in a preoperative assessment center using time-driven activity-based costing. Healthcare. 2013;1:136–42. doi: 10.1016/j.hjdsi.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Albright HW, Feeley TW. A cancer center puts the new approach to work. Harv Bus Rev. 2011;89:61–2. [PubMed] [Google Scholar]
- 7.Health Cost Institute. Washington D.C.: 2011. Health Care Cost & Utilization Report 2011. at < http://www.healthcostinstitute.org/files/HCCI_HCCUR2011.pdf>. [Google Scholar]
- 8.Dexter F, Lubarsky DA, Gilbert BC, Thompson C. A method to compare costs of drugs and supplies among anesthesia providers: a simple statistical method to reduce variations in cost due to variations in casemix. Anesthesiology. 1998;88:1350–6. doi: 10.1097/00000542-199805000-00027. [DOI] [PubMed] [Google Scholar]
- 9.Schuster M, Standl T. Effect of different cost drivers on cost per anesthesia minute in different anesthesia subspecialties. Anesthesiology. 2004;101:1435–43. doi: 10.1097/00000542-200412000-00026. [DOI] [PubMed] [Google Scholar]
- 10.Schuster M, Standl T. Cost drivers in Anesthesia: Manpower, Technique and other Factors. Curr Opin Anaesthesiol. 2006;19:177–84. doi: 10.1097/01.aco.0000192790.78139.82. [DOI] [PubMed] [Google Scholar]
- 11.Jones R, Plantes K. Cost containment in anesthesiology: a survey of the association of anesthesia clinical directors. J Clin Anesth. 1994;6:409–10. doi: 10.1016/s0952-8180(05)80012-1. [DOI] [PubMed] [Google Scholar]
- 12.Majstorović BM, Kastratović DA, Vučović DS, Milaković BD, Miličić BR. Operating cost analysis of anaesthesia: activity based costing (ABC analysis) Srp Arh Celok Lek. 139:501–8. doi: 10.2298/sarh1108501m. [DOI] [PubMed] [Google Scholar]
- 13.Dulisse Brian, Cromwell J. No Harm Found When Nurse Anesthetists Work Without Supervision By Physicians. Health Aff. 2010;29:1469–75. doi: 10.1377/hlthaff.2008.0966. [DOI] [PubMed] [Google Scholar]


