Abstract
Background
There are few effective drugs for pediatric functional constipation (FC).
Objectives
Comparing the effectiveness of Cassia fistula’s emulsion (CFE) with Polyethylene glycol (PEG4000) in FC; and evaluation of safety of both drugs in the treatment of FC.
Materials and Methods
A randomized open label, prospective, controlled, parallel-group clinical trial was carried on 109 children (M/F: 63/46; mean age ± SD: 59.7 ± 28.8 months) in Amirkola children’s hospital, Babol, Iran. The inclusion criteria were based on diagnosis of FC according to the Rome III criteria and age range between 2 - 15 years. They received CFE or PEG randomly for 4 weeks. Frequencies of defecation, severity of pain, consistency of stool, fecal incontinence and retentive posturing were compared between the two groups and with baselines. Children were counted as improved when they exited from Rome III criteria of FC.
Results
Fifty seven patients were assigned to receive PEG and 52 patients received CFE. After 4weeks of medication, 86.5% of children in CFE group and 77.1% in PEG group (RR = 1.121, CI95%:0.939 - 1.338) exited from the criteria of FC. All measurable criteria improved in both groups without any significant difference, except in the frequency of defecation that in CFE group (10.96 ± 5.7) was significantly more than PEG group (6.9 ± 3.5) (P < 0.0001). Compliances of PEG were significantly better in the 2 first weeks (P = 0.002, 0.008) but not in third and fourth week (P = 0.061, 0.062). None of these two drugs cause clinically significant side effects.
Conclusions
CFE can be as effective as PEG in the 4-weeks treatment of children with FC.
Keywords: Constipation, Child, Cassia fistula, Polyethylene Glycols, Persian Medicine, Clinical Trial
1. Background
Pediatric functional constipation (FC) is a common gastrointestinal disorder that can impair the child's and his parent's quality of life (1). It ranged from 0.7% to 29.6 % (median 8.9%) internationally (2). In up to 95% of children with complaint of constipation, there is no structural, endocrinal and metabolic cause; so it is called idiopathic or functional constipation (3). Despite treatment, only 50 to 70% of children with FC demonstrate long-term improvement (1). Although there is not any unique definition, Rome III has been used as diagnostic criteria of FC in children since 2006 (4). Oral laxatives and regular toilet training are the principles of successful treatment. The goals of treatment include: establishing a good pattern of defecation (soft stool and painless defecation), elimination of fecal incontinence and preventing the relapse (4). It has been proposed that changing in life style (including high-fiber diet can improve the constipation (5). Recent publication of randomized trials permits a more evidence-based approach; with polyethylene glycol (PEG) based treatments having been proposed to be effective and well-tolerated as first-line treatment (6-8). PEG is a high molecular chemical compound that is not metabolized by colonic bacteria and act as osmotic laxative. PEG 4000 without electrolytes is solvable and because of tastelessness, easily tolerated by children, so it is frequently used medications today (6-8). In spite of the widespread use of laxatives, lack of high quality studies in this field (6), means that the management of childhood constipation, generally has tended to rely on empirical treatment choices (9). Although drug discovery has many various methods, it has very complicated and expensive process (10). The use of ethno-medical information and traditional medicines (11, 12) can facilitate this process.
Persian medicine (PM) is one of the traditional medicine cultures that support various treatment modalities (13, 14). Cassia fistula (called in PM, “Folus” or “Khiar shanbar”) has been known as a safe and effective laxative for more than 10 centuries (15). But there is just one clinical trial on this subject (16).
2. Objectives
To find and introduce novel safe herbal drugs for FC, we decided to evaluate the effectiveness and safety of a pharmaceutical form of cassia fistula compared with PEG in the treatment of FC in children. In this study, we tested the hypotheses that therapeutic effects and tolerance of CFE were better, and its adverse effects were lower than PEG4000.
3. Patients and Methods
3.1. Patients
This randomized open label, prospective, controlled, parallel-group clinical trial study was performed From January to May 2014, on the functional constipated children, referred to the Pediatric Gastroenterology clinic (Amirkola children hospital, Babol, Mazandaran, Iran). This Hospital serves 1.9 million local residents in locations across the Caspian Sea with three large cities (Amol, Babol and Ghaemshahr) and the corresponding urban regions in the provinces of Mazandaran and Golestan. Fortunately, due to the developing socioeconomic conditions of the people in these regions in recent years, we were able to keep in touch with all the patients during the study period by phone call. Inclusion criteria for this study were outpatient cases aged between 2 - 15 years with a diagnosis of FC according to the Rome III criteria (17). The diagnosis of FC was proved by ruling out the organic constipations by taking history, doing physical examination, some paraclinic tests such as thyroid function tests, anti-tTG, and etc. If it remained any doubt, barium study and anorectal manometry would be performed. Children with any symptom of organic cause of constipation, continuous use of any other drug and those with other chronic diseases were excluded. If there was any fecal impaction, disimpaction was done by normal saline.
At the first visit, demographic information and five variations including the average of: frequency of defecation, consistency of stools, and severity of pain during defecation, retentive posturing and fecal incontinence per week in the last weeks before study and without any medication, were recorded. Each of these variations was clearly explained to the parents and they were trained to determine and record them daily, during the study. Severity of pain and consistency of stool were measured on the pattern of visual analog scale (VAS) (18, 19) comparing with the pre-study scores. All patients were followed for four weeks and the data was recorded in 4 questionnaires (one for each week, each one contained 7 boxes for each criteria and for 7 days of the week) by parents. In addition, the parents were asked to report the Compliance of drugs. This scoring has been done according to VAS pattern and it could be chosen by parents, from 1 (the best imaginable acceptance by the child) to 5 (the worst imaginable acceptance by the child).
During the study, we had regular phone calls with the parents to check the probable complications, treatment (taking the prescribed drugs) and data filling process. If there were any serious questions or problems, we visited the child. At the end of 4 weeks of treatment, the children were visited and the filled out forms were taken and evaluated.
All parents gave written informed consent. This study was registered in the Iranian registry of clinical trials (www.irct.ir) with registration number ID: IRCT201303196932N2.
3.2. Sample Size
The sample size for each group was an estimated 51 cases, based on a therapeutic rate of 56% for the PEG regimen in 8 weeks of treatment (10) and a prediction of 84% for the CFE regimen (16). The α and β errors chosen for these calculations were 0.05 and 0.10, respectively.
3.3. Randomization
Each patient according to the simple randomization and random allocation, entered to one arm of study. We could not predict the therapy regimen for any patient.
3.4. Interventions
In each group, patients received 0.7 - 0.8 g/kg/day of water soluble PEG (manufactured by Sepidaj co, Iran) twice daily or 1 cc/kg /day of CFE in three-divided doses, for 4 weeks. Each 1 cc of CFE contained 0.1 g of dried pulp of fruits of Cassia fistula. CFE was formulated according to PM references (15) and in the order of our previous study and its therapeutic dosage was the same (16). If there was any complication such as diarrhea, parents were allowed to reduce the dose of PEG and CFE, up to 25% of the dose.
3.5. Outcomes
The primary endpoints of this study were quantitative and qualitative therapeutic effects. The secondary endpoints included safety and compliance. Quantitative therapeutic effects included increasing the frequency of defecation and decreasing the consistency of stools and severity of pain during defecation, retentive posturing and fecal incontinence per week. The qualitative therapeutic effect (recovery rate) was defined as the rate of total exited cases from the criteria of FC in each arm, after 4 weeks of treatment. Adverse effects of drugs were evaluated on weeks 1, 2, 3 and at the end of treatment. Compliance was recorded based on VAS.
3.6. Statistical Methods
The statistical analyses performed by the determination of means and SDs, t test, χ2 test, ANOVA repeated measures and Fisher’s exact test, with significance accepted at the 5% level. The results are expressed as mean ± SD or percentage. Qualitative results are shown as Relative Risk and 95% confidence interval. The survival function was done by kaplan-miere and log-rank tests. SPSS IBM20 and stata11.2 were used for analysis. The P value < 0.05 was considered significant. An intent-to-treat analysis was used.
The study was approved by ethics committee of Babol University of Medical Sciences.
4. Results
4.1. Flow of Participants
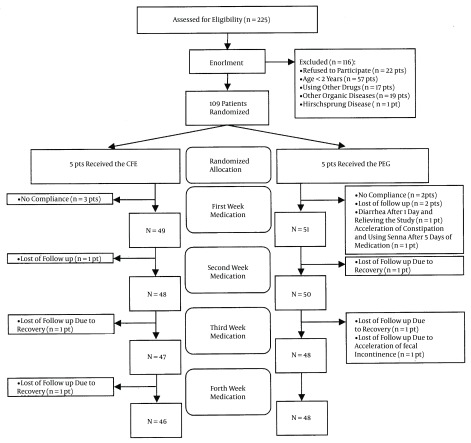
Figure 1 shows a flow chart revealing how the patients in both arms were selected for analysis.
Figure 1. Flow Chart Summarizing the Study Process in the Two Treatment Groups of the Children With Functional Constipation With Cassia Fistula Emulsion (CFE) and Polyethylene Glycol4000 (PEG).
4.2. Recruitment
From January to May 2014, 225 patients were under observation for constipation by a pediatric gastroenterologist that 109 of them [63 (68.6%) boys and 46 (31.4%) girls] completed our inclusion criteria and entered the study .They randomly received one type of treatment. The mean age of all cases was 59.68 (± 28.8 SD) months ranged between 25 to 147 months and the mean duration of constipation was 27.6 (± 23) months.
4.3. Baseline Data
The baseline data in two treatment groups are shown in Table 1.
Table 1. Baseline Data of the Children With Functional Constipation, in the Two Treatment Groupsa,b.
| Variable | CFE Group (n = 52) | PEG Group (n = 57) | P Value |
|---|---|---|---|
| Age, months | 64.6 ± 25.2 | 55.2 ± 31.2 | 0.088 |
| Sex, Boy | 33 | 30 | 0.253 |
| Weight, Kg | 20.5 ± 7.2 | 18.5 ± 8.9 | 0.202 |
| Duration of constipation, months | 31.1 ± 24.6 | 23.5 ± 21.8 | 0.090 |
| Defecation ≤ 2 per week | 41 | 52 | 0.681 |
| Incontinence | 34 | 37 | 0.958 |
| Retentive posturing | 40 | 37 | 0.169 |
| History of previous treatment | 43 | 51 | 0.305 |
aValues are expressed as mean ± SD or No.
bP > 0.05 is not significant.
4.4. Numbers Analyzed
In CFE group, 52 patients and in PEG group, 57 patients were analyzed.
4.5. Primary Outcomes
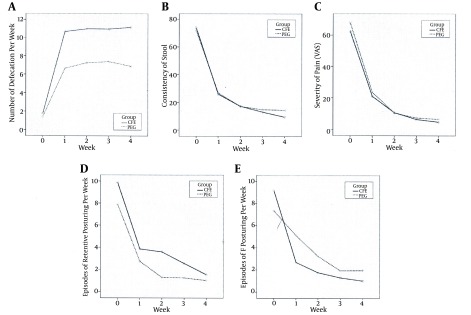
Either of drugs has been used in this two treatment strategies were effective in reducing the severity of pain and consistency of stool. However increase in the frequency of defecation in CFE group was significantly more than PEG group (P < 0.0001). Retentive posturing and fecal incontinence were better treated in CFE group, but there weren’t any significance differences between two groups (P = 0.209), except in retentive posturing at the second week (P = 0.029) (Figure 2). The detailed treatment outcomes are presented in Table 2.
Figure 2. A, Defecation Frequency; B, Consistency of Stool; C, Severity of Pain; D, Retentive Posturing; E, Incontinency of Stool, in the Two Treatment Groups of Cassia Fistula Emulsion (CFE) and Polyethylen Glycol4000 (PEG), in the Children With Functional Constipation, Before and After Medication.
Table 2. Treatment Outcome in Two Studied Groups of the Pediatric Functional Constipation, With Cassia Fistula Emulsion (CFE) and Polyethylene Glycol 4000 (PEG)a,b.
| Before Medication | First Week | Second Week | Third Week | Fourth Week | |
|---|---|---|---|---|---|
| Defecation, w | |||||
| CFE | 1.76 ± 1.71 | 10.67 ± 6.15 | 10.98 ± 5.71 | 10.98 ± 5.78 | 10.96 ± 5.76 |
| PEG | 1.42 ± 1.46 | 6.65 ± 4.3 | 7.25 ± 3.5 | 7.38 ± 3.8 | 6.9 ± 3.5 |
| P Value | 0.191 | < 0.0001 | < 0.0001 | 0.001 | < 0.0001 |
| Severity of pain (VAS) | |||||
| CFE | 62.50 ± 20.24 | 21.02 ± 17.2 | 10.70 ± 11.54 | 6.41 ± 10.37 | 4.74 ± 8.66 |
| PEG | 68.02 ± 23.22 | 23.56 ± 22.61 | 10.46 ± 15.54 | 7.35 ± 12.5 | 6.54 ± 11.98 |
| P Value | 0.082 | 0.541 | 0.995 | 0.648 | 0.407 |
| Consistency of stool (VAS) | |||||
| CFE | 74.13 ± 10.87 | 25.87 ± 21.00 | 17.24 ± 16.82 | 13.07 ± 16.15 | 9.48 ± 14.60 |
| PEG | 72.08 ± 19.46 | 26.75 ± 22.1 | 17.08 ± 20.05 | 14.79 ± 17.04 | 14.35 ± 16.8 |
| P Value | 0.645 | 0.967 | 0.819 | 0.634 | 0.137 |
| Fecal Incontinence, w | |||||
| CFE | 9.17 ± 9.88 | 2.62 ± 4.38 | 1.76 ± 3. 6 | 1.3 ± 4.1 | 1.02 ± 3.45 |
| PEG | 7.33 ± 10.75 | 5.1 ± 9.99 | 3.23 ± 5.8 | 1.94 ± 4.44 | 1.96 ± 4.3 |
| P Value | 0.990 | 0.078 | 0.100 | 0.452 | 0.249 |
| Retentive Posturing, w | |||||
| CFE | 9.87 ± 9.99 | 3.85 ± 6.54 | 3.59 ± 6.61 | 2.54 ± 5.44 | 1.54 ± 4.15 |
| PEG | 7.87 ± 11.80 | 2.73 ± 5.11 | 1.29 ± 3.67 | 1.25 ± 3.39 | 1.02 ± 3.34 |
| P Value | 0.882 | 0.322 | 0.035 | 0.107 | 0.502 |
| Acceptance and Tolerance | |||||
| CFE | - | 2.56 ± 1.2 | 2.52 ± 1.33 | 2.321 ± 1.42 | 2.33 ± 1.42 |
| PEG | - | 1.92 ± 0.89 | 1.9 ± 1.01 | 1.88 ± 0.94 | 1.88 ± 1.02 |
| P Value | - | 0.003 | 0.011 | 0.074 | 0.079 |
aValues are expressed as mean ± SD.
bP > 0.05 is not significant.
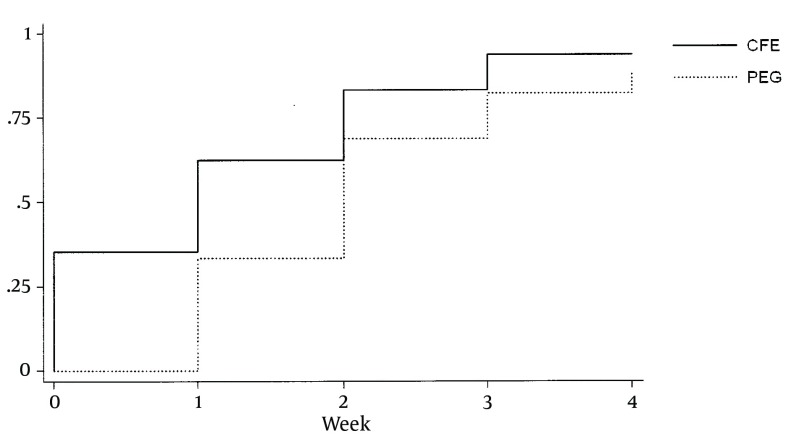
In a qualitative comparison between two groups, after 4 weeks of medication, without any significant differences, 45/52 (86.5%) patients in CFE and 44/57 (77.1%) patients in PEG, exited from the criteria of FC (RR = 1.121, CI 95%:0.939 - 1.338). In survival function test of two drugs, median survival time was 2 weeks in both groups, mean was 2.327 ± 0.162 weeks in CFE and 2.368 ± 0.158 weeks in PEG. Details are shown in Figure 3.
Figure 3. Survival Functions Between Two Groups of Cassia Fistula Emulsion (CFE) and Polyethylen Glycol4000 (PEG).
4.6. Secondary Outcomes
4.6.1. Adverse Events
Diarrhea in 13/52 (25%) and abdominal pain in 2/52 (3.8%) cases of CFE group were reported. All of them recovered by decreasing 25% of the dose, before the third week of taking medication.
PEG caused 15/57 (26.3%) diarrhea cases. Two of them stopped treatment because of severe diarrhea. Five/57 (8.7%) cases in PEG consumers had complained of abdominal pain. Four of them relieved by dose adjustment, but one of them had it even reducing the dose, up to the end of the study.
4.7. Compliance
Generally, PEG was tolerated significantly better, comparing with CFE during the first (P = 0.002) and second weeks (P = 0.008). But it didn’t have any significant difference between two groups, in the third (P = 0.061) and fourth weeks (P = 0.062) (Table 2). Three/52 patients in CFE group and 2/57 in PEG group refused to take them because of their tastes.
5. Discussion
Although in this randomized clinical trial, we expect CFE (as a new herbal drug) to be so better and more effective than PEG, it was similar in efficacy to PEG for 4 weeks treatment of pediatric functional constipation.
At the 1, 2, 3 and 4 week follow up evaluation, similar improvement (without significant differences) in all criteria including consistency of stools, severity of pain during defecation, retentive posturing and fecal incontinence were seen. Frequency of defecation per week was improved in both groups, but it was significantly better in CFE group (P < 0.0001). As a qualitative report, 86.5% of patients in CFE group and 77.1% in PEG group (without any significant difference (P = 0.206)) exited from the criteria of constipation after 4 weeks of medication. The results in CFE group were matched with the study of Mozaffarpur et al. (16).
As the PEG is proposed as first line drug in FC, it was chosen for control group. We found some reviews that studied the clinical trials of PEG versus placebo or other laxatives (6, 20, 21).
In some of those trials, PEG was compared with lactulose (10, 21-27), in two of them with milk of magnesia (28, 29), two with liquid paraffin (30, 31), in one study with a natural product (mixture of Acacia fiber, Psyllium fiber and fructose) (32) and three with placebo (33-35). Some other studies have been done to evaluate long-term safety and efficacy of PEG (36, 37). In some clinical trials PEG is reported to be significantly more effective than control groups (27, 29, 31, 33), but not in some other clinical trials (24, 28, 30, 32, 35). The duration of study was ranged from 2 weeks (25, 26, 34, 35) up to 12 months (28). Although pediatric constipation needs prolonged duration of treatment (1), the duration of our study was not an uncommon period. Besides that in previous study on CFE, it was used for 3 weeks (16) and we prolonged this duration to 4 weeks in this study.
The rate of recovery or improvement in former studies with PEG, was reported between 56% (in 8 weeks) (10) up to 91% (in 11 months) (36). In our study, the improvement was 77% after 4 weeks of treatment that is accommodate with the mean results of other similar studies with PEG (26, 28, 32, 34, 35). Different kinds of PEG including PEG 4000 (8, 22, 23), PEG 3350 (10, 25, 27-30, 34, 36-38) and PEG 3350 plus electrolytes (32, 33, 35) have been used in studies. We chose PEG 4000 because of its accessibility and its safety in long-term therapy, in clinic and with respect to biochemical parameters (8). Dose adjustment in our study was similar to those studies of PEG 4,000 (8, 22, 23).
Potent phenolic antioxidants such as flavonoids, flavan-3-ol derivatives and anthraquinones are the most important phytochemical constituents of Cassia fistula (39). Anthraquinone is probably responsible for its laxative effect and so it can be categorized as stimulant laxative (16). At the first study of CFE on FC it was more effective than mineral oil (16).
Although there are not any unique criteria for FC, we used criteria of RomeIII as inclusion criteria and to measure qualitative outcome of the results. Our quantitative outcome measures were well defined by the use of these criteria. For entering in the study, three steps of explanation, disimpaction and maintenance therapy were taken. Also for disimpactions we used enema with normal saline that has been effective in relieving fecal impaction (40).
Because of close follow-up and calling up the parents every 5 days, the missing was quiet low.
PEG is tasteless and tolerate better that others laxatives (3, 32, 41, 42). Similar results were obtained in this study and PEG had better compliance than CFE in the 2 first weeks. But these differences were not significant in third and fourth weeks. It might be because the children found it effective and tolerated its taste.
Reported adverse effects of PEG in other studies include: flatulence, loose stool, nausea, vomiting, and abdominal cramping, bloating and abdominal pain. However, the most common side effect is diarrhea which subsided on dose reduction (41). Our experience in this study confirms this point. Less complains of abdominal pain with CFE were received. This is a strong point for this new medicine, but needs more clinical trials to endorse.
As our patients were from different cities and somehow different cultures, the results can be generalized to all population.
As the two drugs, differed in colors, tastes and smell and were administered to children in different ways, it was not possible to perform a blind study. Although it is similar to other studies in this subject (23, 25, 27-30, 32, 37), it was one of our study’s limitations and weaknesses. It was better if we could compare the effect of studied drugs on patients with different grades of severity of constipation. It wasn’t possible because of insufficient sample size, so it is one the weaknesses of our study.
Some issues are still to be investigated more deeply in future studies; most importantly, the duration of follow up. We need more randomized clinical trials to assess the long-term effectiveness of these agents for the treatment of childhood constipation.
5.1. Conclusions
In this 4 weeks study, CFE was as effective as PEG 4000 in pediatric functional constipation. In all criteria both drugs were effective without any difference, except in frequency of defecation per week that it was significantly better in CFE group. Compliance of PEG was better in 2 first weeks of treatment, but without any difference during the last two weeks. To evaluate effectiveness and safety of CFE, designing more long-term studies are required.
Acknowledgments
The authors thank Dr. Hasanjani Roshan MR for his excellent comments and helping in editing the manuscript and also to Fatemeh Mirzapour, Ulm University (Germany), for language check of this paper.
Footnotes
Authors’ Contribution:Mohammad Reza Esmaeilidooki conceptualized and designed the project, visited participants, critically reviewed and revised the manuscript, Seyyed Ali Mozaffarpur designed the project, followed up participants, performed data analysis, and critically reviewed, revised and submitted the manuscript, Mohaddese Mirzapour registered the study in IRCT, followed up participants, performed primary data analysis and drafted the initial manuscript, Hoda Shirafkan performed data analysis, reviewed and revised the manuscript, Mohammad Kamalinejad helped designing the project and produced the emulsion of cassia fistula, Ali Bijani designed the whole study, helped in data analysis and revised the manuscript; and all authors approved the final manuscript as submitted.
Funding/Support:All phases of this study, were supported by Babol University of medical sciences.
References
- 1.Biggs WS, Dery WH. Evaluation and treatment of constipation in infants and children. Am Fam Physician. 2006;73(3):469–77. [PubMed] [Google Scholar]
- 2.van den Berg MM, Benninga MA, Di Lorenzo C. Epidemiology of childhood constipation: a systematic review. Am J Gastroenterol. 2006;101(10):2401–9. doi: 10.1111/j.1572-0241.2006.00771.x. [DOI] [PubMed] [Google Scholar]
- 3.Chung S, Cheng A, Goldman RD. Polyethylene glycol 3350 without electrolytes for treatment of childhood constipation. Can Fam Physician. 2009;55(5):481–2. [PMC free article] [PubMed] [Google Scholar]
- 4.Benninga M, Candy DC, Catto-Smith AG, Clayden G, Loening-Baucke V, Di Lorenzo C, et al. The Paris Consensus on Childhood Constipation Terminology (PACCT) Group. J Pediatr Gastroenterol Nutr. 2005;40(3):273–5. doi: 10.1097/01.mpg.0000158071.24327.88. [DOI] [PubMed] [Google Scholar]
- 5.Salehi M, Dehghani M, Imanieh MH. Therapy of chronic functional constipation in children before and after dietary education. Iran Red Crescent Med J. 2010;2010(2):118–21. [Google Scholar]
- 6.Candy D, Belsey J. Macrogol (polyethylene glycol) laxatives in children with functional constipation and faecal impaction: a systematic review. Arch Dis Child. 2009;94(2):156–60. doi: 10.1136/adc.2007.128769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arora R, Srinivasan R. Is polyethylene glycol safe and effective for chronic constipation in children? Arch Dis Child. 2005;90(6):643–6. doi: 10.1136/adc.2005.072918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bae SH. Long-term safety of PEG 4000 in children with chronic functional constipation: A biochemical perspective. Korean J Pediatr. 2010;53(7):741–4. doi: 10.3345/kjp.2010.53.7.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hyman PE, Di Lorenzo C, Prestridge LL, Youssef NN, Ueno R. Lubiprostone for the treatment of functional constipation in children. J Pediatr Gastroenterol Nutr. 2014;58(3):283–91. doi: 10.1097/MPG.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 10.Voskuijl W, de Lorijn F, Verwijs W, Hogeman P, Heijmans J, Makel W, et al. PEG 3350 (Transipeg) versus lactulose in the treatment of childhood functional constipation: a double blind, randomised, controlled, multicentre trial. Gut. 2004;53(11):1590–4. doi: 10.1136/gut.2004.043620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan SY, Zhou SF, Gao SH, Yu ZL, Zhang SF, Tang MK, et al. New Perspectives on How to Discover Drugs from Herbal Medicines: CAM's Outstanding Contribution to Modern Therapeutics. Evid Based Complement Alternat Med. 2013;2013:627375. doi: 10.1155/2013/627375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patwardhan B, Mashelkar RA. Traditional medicine-inspired approaches to drug discovery: can Ayurveda show the way forward? Drug Discov Today. 2009;14(15-16):804–11. doi: 10.1016/j.drudis.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 13.Zargaran A, Mehdizadeh A, Zarshenas MM, Mohagheghzadeh A. Avicenna (980-1037 AD). J Neurol. 2012;259(2):389–90. doi: 10.1007/s00415-011-6219-2. [DOI] [PubMed] [Google Scholar]
- 14.Mojahedi M, Naseri M, Majdzadeh R, Keshavarz M, Ebadini M, Nazem E, et al. Reliability and Validity Assessment of Mizaj Questionnaire: A Novel Self-report Scale in Iranian Traditional Medicine. Iran Red Crescent Med J. 2014;16(3):e33998. doi: 10.5812/ircmj.15924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sina IA. Al-Qanun fi al-tibb. Beirut: Alamy Le-Al Matbooat Institute; 2005. [Google Scholar]
- 16.Mozaffarpur SA, Naseri M, Esmaeilidooki MR, Kamalinejad M, Bijani A. The effect of cassia fistula emulsion on pediatric functional constipation in comparison with mineral oil: a randomized, clinical trial. Daru. 2012;20(1):83. doi: 10.1186/2008-2231-20-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fabricant DS, Farnsworth NR. The value of plants used in traditional medicine for drug discovery. Environ Health Perspect. 2001;109 Suppl 1:69–75. doi: 10.1289/ehp.01109s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18(3):205–7. doi: 10.1136/emj.18.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dexter F, Chestnut DH. Analysis of statistical tests to compare visual analog scale measurements among groups. Anesthesiology. 1995;82(4):896–902. doi: 10.1097/00000542-199504000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Gordon M, Naidoo K, Akobeng AK, Thomas AG. Osmotic and stimulant laxatives for the management of childhood constipation. Cochrane Database Syst Rev. 2012;7:CD009118. doi: 10.1002/14651858.CD009118.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Lee-Robichaud H, Thomas K, Morgan J, Nelson RL. Lactulose versus Polyethylene Glycol for Chronic Constipation. Cochrane Database Syst Rev. 2010;(7):CD007570. doi: 10.1002/14651858.CD007570.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Dupont C, Leluyer B, Maamri N, Morali A, Joye JP, Fiorini JM, et al. Double-blind randomized evaluation of clinical and biological tolerance of polyethylene glycol 4000 versus lactulose in constipated children. J Pediatr Gastroenterol Nutr. 2005;41(5):625–33. doi: 10.1097/01.mpg.0000181188.01887.78. [DOI] [PubMed] [Google Scholar]
- 23.Bouhnik Y, Neut C, Raskine L, Michel C, Riottot M, Andrieux C, et al. Prospective, randomized, parallel-group trial to evaluate the effects of lactulose and polyethylene glycol-4000 on colonic flora in chronic idiopathic constipation. Aliment Pharmacol Ther. 2004;19(8):889–99. doi: 10.1111/j.1365-2036.2004.01918.x. [DOI] [PubMed] [Google Scholar]
- 24.Candy DC, Edwards D, Geraint M. Treatment of faecal impaction with polyethelene glycol plus electrolytes (PGE + E) followed by a double-blind comparison of PEG + E versus lactulose as maintenance therapy. J Pediatr Gastroenterol Nutr. 2006;43(1):65–70. doi: 10.1097/01.mpg.0000228097.58960.e6. [DOI] [PubMed] [Google Scholar]
- 25.Gremse DA, Hixon J, Crutchfield A. Comparison of polyethylene glycol 3350 and lactulose for treatment of chronic constipation in children. Clin Pediatr (Phila). 2002;41(4):225–9. doi: 10.1177/000992280204100405. [DOI] [PubMed] [Google Scholar]
- 26.Wang BX, Wang MG, Jiang MZ, Xu CD, Shao CH, Jia LY, et al. [Forlax in the treatment of childhood constipation: a randomized, controlled, multicenter clinical study]. Zhongguo Dang Dai Er Ke Za Zhi. 2007;9(5):429–32. [PubMed] [Google Scholar]
- 27.Attar A, Lemann M, Ferguson A, Halphen M, Boutron MC, Flourie B, et al. Comparison of a low dose polyethylene glycol electrolyte solution with lactulose for treatment of chronic constipation. Gut. 1999;44(2):226–30. doi: 10.1136/gut.44.2.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loening-Baucke V, Pashankar DS. A randomized, prospective, comparison study of polyethylene glycol 3350 without electrolytes and milk of magnesia for children with constipation and fecal incontinence. Pediatrics. 2006;118(2):528–35. doi: 10.1542/peds.2006-0220. [DOI] [PubMed] [Google Scholar]
- 29.Loening-Baucke V. Polyethylene glycol without electrolytes for children with constipation and encopresis. J Pediatr Gastroenterol Nutr. 2002;34(4):372–7. doi: 10.1097/00005176-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Rafati M, Karami H, Salehifar E, Karimzadeh A. Clinical efficacy and safety of polyethylene glycol 3350 versus liquid paraffin in the treatment of pediatric functional constipation. Daru. 2011;19(2):154–8. [PMC free article] [PubMed] [Google Scholar]
- 31.Karami H, Khademloo M, Niari P. Polyethylene glycol versus paraffin for the treatment of childhood functional constipation. Iran J Pediatr. 2009;19(3):255–61. [Google Scholar]
- 32.Quitadamo P, Coccorullo P, Giannetti E, Romano C, Chiaro A, Campanozzi A, et al. A randomized, prospective, comparison study of a mixture of acacia fiber, psyllium fiber, and fructose vs polyethylene glycol 3350 with electrolytes for the treatment of chronic functional constipation in childhood. J Pediatr. 2012;161(4):710–5 e1. doi: 10.1016/j.jpeds.2012.04.043. [DOI] [PubMed] [Google Scholar]
- 33.Corazziari E, Badiali D, Habib FI, Reboa G, Pitto G, Mazzacca G, et al. Small volume isosmotic polyethylene glycol electrolyte balanced solution (PMF-100) in treatment of chronic nonorganic constipation. Dig Dis Sci. 1996;41(8):1636–42. doi: 10.1007/BF02087913. [DOI] [PubMed] [Google Scholar]
- 34.Nurko S, Youssef NN, Sabri M, Langseder A, McGowan J, Cleveland M, et al. PEG3350 in the treatment of childhood constipation: a multicenter, double-blinded, placebo-controlled trial. J Pediatr. 2008;153(2):254–61. doi: 10.1016/j.jpeds.2008.01.039. 261 e1. [DOI] [PubMed] [Google Scholar]
- 35.Thomson MA, Jenkins HR, Bisset WM, Heuschkel R, Kalra DS, Green MR, et al. Polyethylene glycol 3350 plus electrolytes for chronic constipation in children: a double blind, placebo controlled, crossover study. Arch Dis Child. 2007;92(11):996–1000. doi: 10.1136/adc.2006.115493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pashankar DS, Bishop WP, Loening-Baucke V. Long-term efficacy of polyethylene glycol 3350 for the treatment of chronic constipation in children with and without encopresis. Clin Pediatr (Phila). 2003;42(9):815–9. doi: 10.1177/000992280304200907. [DOI] [PubMed] [Google Scholar]
- 37.Loening-Baucke V, Krishna R, Pashankar DS. Polyethylene glycol 3350 without electrolytes for the treatment of functional constipation in infants and toddlers. J Pediatr Gastroenterol Nutr. 2004;39(5):536–9. doi: 10.1097/00005176-200411000-00016. [DOI] [PubMed] [Google Scholar]
- 38.Michail S, Gendy E, Preud'Homme D, Mezoff A. Polyethylene glycol for constipation in children younger than eighteen months old. J Pediatr Gastroenterol Nutr. 2004;39(2):197–9. doi: 10.1097/00005176-200408000-00014. [DOI] [PubMed] [Google Scholar]
- 39.Bahorun T, Neergheen VS, Aruoma OI. Phytochemical constituents of Cassia fistula. Afr J Biotechnol. 2005;4(13) [Google Scholar]
- 40.Bautista CA, Arguelles MF, Pena QL, Polanco AI, Sanchez RF, Varea CV. Guidelines for the treatment of functional constipation. Barcelona: Anales de pediatria; 2011. [DOI] [PubMed] [Google Scholar]
- 41.Ahmed M, Pai B, Reynolds T. Use of polyethylene glycol in children less than 3 years of age. J Coll Physicians Surg Pak. 2012;22(4):267–8. [PubMed] [Google Scholar]
- 42.Dziechciarz P, Horvath A, Szajewska H. Polyethylene glycol 4000 for treatment of functional constipation in children. J Pediatr Gastroenterol Nutr. 2015;60(1):65–8. doi: 10.1097/MPG.0000000000000543. [DOI] [PubMed] [Google Scholar]