Abstract
The New York City (NYC) Longitudinal Study of Wellbeing, or “Poverty Tracker,” is a survey of about 2,300 New York City residents. Its purpose is to provide a multidimensional and dynamic understanding of economic disadvantage in NYC. Measures of disadvantage were collected at baseline and a 12-month follow-up, and include three types of disadvantage: (1) income poverty, using a measure based on the new Supplemental Poverty Measure; (2) material hardship, including indicators of food insecurity, housing hardship, unmet medical needs, utility cutoffs, and financial insecurity; and (3) adult health problems, which can drain family time and resources. This paper presents initial results for NYC families with children under 18. At baseline, 56% of families with children had one or more type of disadvantage, including 28% with income poverty, 39% with material hardship, and 17% with an adult health problem. Even among nonpoor families, 33% experienced material hardship and 14% reported an adult health problem. Two-thirds of all families faced disadvantage at either baseline or follow-up, with 46% experiencing some kind of disadvantage at both time points. Respondents with a college education were much less likely to face disadvantage. Even after adjusting for educational attainment and family characteristics, the families of black and Hispanic respondents had elevated rates of disadvantage. Considering income poverty alone greatly understates the extent of disadvantage among families with children in New York City. These results suggest that in addition to addressing income poverty, policymakers should give priority to efforts to reduce material hardship and help families cope with chronic physical or mental illness. The need for these resources extends far above the poverty line.
Keywords: Poverty, material hardship, children
A good deal of attention has focused on measuring and alleviating income poverty, and rightly so. Money matters for child health and development, and a number of social programs have as their aim to help raise the living standards of the poor or near-poor. But society's concern about poor children extends beyond income poverty. We also are concerned if children lack adequate housing, food, and medical care, or if their families face significant health challenges that drain time and resources. Ideally, we'd like to know not just how many families are poor in income terms, but also how many are disadvantaged in other respects – in particular, with regard to material hardship and health and well-being.
To better understand the links among income poverty, material hardship, and health, a group of researchers at Columbia University, in partnership with the Robin Hood Foundation, launched the New York City Longitudinal Study of Wellbeing, or “Poverty Tracker,” a survey of approximately 2,300 New York City residents that gathered data on income poverty, material hardship, and health and well-being. The Poverty Tracker is unusual in gathering information from the same sample about these multiple aspects of disadvantage, and in conducting interviews every three months over two years, to provide a more comprehensive and dynamic picture of poverty and how it relates to material hardship and well-being.
This article briefly describes the Poverty Tracker survey and how it measures disadvantage, and summarizes some of our initial findings for families with children in New York City. Drawing on the baseline and 12-month follow-up surveys, this article has several objectives. The first is to describe the prevalence and interrelationship of income poverty, material hardship, and adult health problems among families with children. The second is to describe the “dynamics of disadvantage,” or the patterns of stability and change in disadvantage over time. The third is to examine how the risk of disadvantage varies by individual and family characteristics. By combining a measure of poverty with indicators of material hardship and adult health problems, the results provide a distinctive picture of economic disadvantage in a representative sample of urban families with children.
Conceptualizing and measuring disadvantage
The purpose of the Poverty Tracker is to provide a multidimensional and dynamic understanding of economic disadvantage. Income poverty is an important element of this construct; it is well-established that poverty is detrimental for children's development, health, and wellbeing.1-3 The poverty measure we use is based on the Census Bureau and Bureau of Labor Statistics' new Supplemental Poverty Measure, which is widely considered to be an improved measure of income poverty relative to official statistics because it takes into account government transfers such as the EITC and Food Stamps not counted in the official measure, geographic differences in cost of living, as well as costs such as medical expenses, child care, and commuting.4 Families are classified as poor if their annual income (defined as post-tax cash income plus in-kind benefits, less expenditures for medical care, child care, or commuting) falls below a poverty line specific to New York City.
However, it is important to go beyond income to understand conditions that can reinforce disadvantage and cause families to struggle. Capturing multiple dimensions of disadvantage provides a fuller picture of the challenges and stressors faced by low- and moderate-income families. The Poverty Tracker study examines two such conditions. One is material hardship, or the inability to make ends meet, as measured by indicators such as food insecurity or inability to afford rent, utilities, or medical care. Material hardship has received increasing attention as an influence on child health and well-being5-8 and as a mediator of the effects of income poverty on children.9, 10 The Poverty Tracker survey asked about five types of hardship: financial (running out of money), bills (utility cutoffs due to nonpayment of bills), food insecurity, unmet medical need, and housing hardship.
The Poverty Tracker also included an indicator of family health: whether the adult survey respondent reported a work-limiting disability or poor self-rated health. Although family health is not commonly used as an indicator of disadvantage, a parent's illness can place a significant strain on the family, making it more difficult for parents to provide and care for their children. Parental depression and other mental illnesses have significant implications for children's psychosocial and health outcomes.11-16 A parent's physical illness or disability can also have detrimental effects on children and families,17-21 in part because it increases the risk of joblessness, poverty, and material hardship.22-25
The Poverty Tracker builds on previous efforts to document the prevalence of material hardship and its association with income poverty, both for the overall population and for families with children.6, 26-30 By adding adult health problems to our measure of disadvantage, the Poverty Tracker reflects the insights of extensive research on health disparities and on the links between health and social, psychological, and economic well-being.31 The current paper documents the prevalence and patterns of change in this more comprehensive disadvantage measure for families with children.
Data and Methods
This article presents data from the baseline and 12-month follow-up waves of the New York City Longitudinal Study of Wellbeing, a representative survey of New York City residents aged 18 or older. The Columbia University Institutional Review Board reviewed and approved the study.
Sample and data collection
The baseline survey was conducted between December 2012 and March 2013. A sample of 2,002 NYC residents was recruited via random digit dial by the survey research firm Abt-SRBI. In addition, a random sample (n=226) of clients recruited from a probability sample of Robin Hood Foundation-funded social service agencies. Baseline surveys with agency participants were usually conducted face-to-face. This “agency sample” was included to augment the number of low- and moderate-income study participants, increasing statistical power for subgroup analyses and providing insight into the lives of very disadvantaged individuals, such as the homeless, who are often missed in phone surveys. About one in five agency participants was provided with a basic cell phone in lieu of cash incentives for survey completion; the phone facilitated study retention for participants who did not have a stable address or means of communication. After completing the baseline survey, all study participants were then re-contacted by phone and/or email roughly every 3 months to participate in follow-up surveys; a small number of study participants completed paper surveys sent by mail. Consent was verbal for in-person and phone interviews and written for online and paper surveys.
Weights
Baseline and follow-up samples are weighted so that they are representative of the adult population of New York City. Survey weights account for survey nonresponse and attrition, differential selection probabilities between and within households, and post-stratification adjustments based on the American Community Survey (ACS).
Measures
The study employed three indicators of disadvantage. The first was a measure of income poverty based on the Census Bureau's new Supplemental Poverty Measure (SPM). Unlike the official poverty measure, the SPM includes unmarried domestic partners and their relatives, unrelated children under age 15, and foster children under age 22 in calculating income thresholds and household size. To develop poverty thresholds, 2012 SPM thresholds were adjusted to reflect New York City's cost of living using data on fair market rents. Household income included annual earnings, retirement income, and transfer income including food stamps, disability, cash welfare, unemployment insurance, WIC, housing benefits, and school lunches. After-tax income was used in order to include the value of refundable tax credits such as EITC, as well as to subtract income and payroll taxes. The annual costs of child care, commuting and work expenses, and medical out-of-pocket expenses were deducted from household income, following procedures outlined by the Census Bureau and Bureau of Labor Statistics.
The second measure, material hardship, taps a family's inability to meet its basic needs. Material hardship was measured with ten items in the baseline and follow-up surveys; these questions asked respondents to describe their status over the previous 12 months, and were based on used validated scales from other surveys such as the Survey of Income and Program Participation (SIPP) and the Fragile Families and Child Wellbeing survey. Five types of hardship were measured. Financial hardship was defined as often running out of money between paychecks or before the end of the month. Bill hardship was defined as having electricity or other utilities cut off for nonpayment of bills. Food insecurity was defined as reporting it was often the case that the family did not have enough food to eat, the food didn't last, or the respondent worried that the food would run out. Medical hardship was defined as having to forgo needed medical services because of lack of money for care. Housing hardship was defined as having to move in with others or live in a shelter because the family did not have a place to live. Our summary measure of hardship was coded as “1” for study participants who had at least one of these hardship types.
The third measure, adult health problems, was based on survey items about the survey respondent's self-rated health and work-limiting disability. Study participants who described their health as “poor” or who reported that health problems limited the kind or amount of work they could do were classified as having a health problem. Both indicators were assessed at baseline and follow-up.
Several individual and family characteristics were included in analyses reported in this paper: respondent race and Hispanic ethnicity, level of education, age in years, presence of a co-resident spouse or domestic partner, and number of children under 18 in the household. Families with children were defined as those in which the study participant reported living with a related or foster child under the age of 18.
Missing data for variables used in the analysis were imputed using chained equations in MICE for R; 3-5 datasets were imputed.
Analysis
Analyses included only families with at least one child under age 18 at both baseline and 1-year follow-up. We first analyzed the prevalence of disadvantage at baseline for all families with children and for subgroups defined by race and ethnicity, family characteristics, and education. Next, we looked at the dynamics of disadvantage between baseline and follow-up survey waves, categorizing families as having experienced no disadvantage at either wave, no disadvantage at baseline and disadvantage at follow-up (“entry”), disadvantage at baseline and no disadvantage at follow-up (“exit”), or disadvantage at both waves (“persistent disadvantage”). As with baseline prevalence, the dynamics of disadvantage were examined for all families with children and for subgroups defined by race and ethnicity, family characteristics, and education. We also examined the relationship of income poverty to the other two measures of disadvantage. The baseline analytic sample included study participants who reported living with at least one child under 18 at baseline. Analysis of the dynamics of disadvantage included follow-up study participants who still lived in New York City at follow-up and who reported living with at least one child under 18 at both baseline and follow-up. All prevalence figures were weighted. P-values for these bivariate associations were based on the corrected Pearson Chi-square statistic.32
We used logistic regression to evaluate associations between individual and family characteristics and both baseline and persistent disadvantage, as well as the three specific types of disadvantage. For all of these outcomes, the model included black race, Hispanic ethnicity, respondent age, presence of spouse or domestic partner, number of children, and level of educational attainment. All analyses were conducted in Stata 14.0.
An online supplement displays associations between individual/family characteristics and the dynamics of income poverty, material hardship, and adult health problems.
Results
Of the baseline sample of 2,228 respondents, 798 (36%) reported living with a child under the age of 18 and were included in the analyses of baseline disadvantage. Of the 1,330 participants who completed the 12-month follow-up survey, 383 (29%) reported living with a child under the age of 18 at both baseline and follow-up; of these study participants, 10 had moved out of New York City by the 12-month follow-up and were omitted from the analysis, leaving a sample of 373 for analyses of the dynamics of disadvantage.
Prevalence of disadvantage
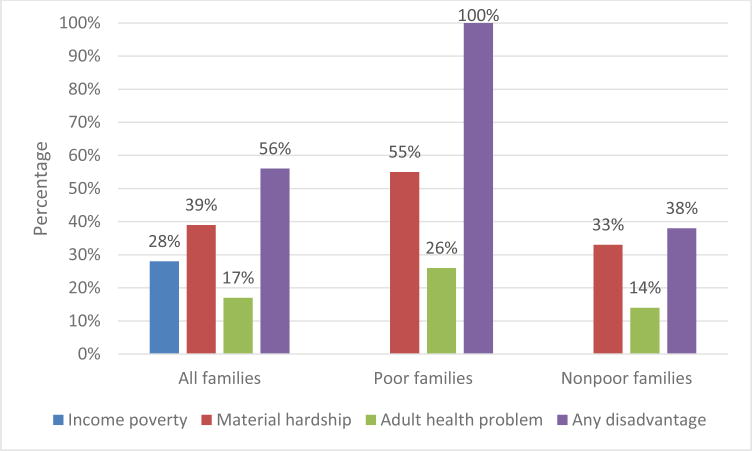
Figure 1 displays the baseline prevalence of income poverty, hardship, and health problems, as well as the proportion of families with any of these three types of disadvantage. About 56% of families with children experienced at least one type of disadvantage. Material hardship was the most common of these disadvantages. About 39% of families with children experienced at least one type of hardship; financial hardship (18%) and bill hardship (17%) were the most common, followed by medical hardship (14%), food insecurity (12%), and housing hardship (6%). The three types of disadvantage were correlated; poor families were more likely to experience material hardship (55%) or an adult health problem (26%). Even among nonpoor families, however, 33% experienced material hardship in the previous year, and 14% had an adult health problem. Among nonpoor families, material hardship was most common among those between 100% and 200% of poverty – 42% reported material hardship at baseline – but even among those above 200% of the poverty line, 22% reported material hardship at baseline.
Figure 1.
Baseline prevalence of income poverty, material hardship, adult health problems, and any disadvantage for all families with children and by family poverty; Note: All figures are weighted. Family poverty was assessed at baseline using the supplemental poverty measure.
The prevalence of disadvantage differed by race and ethnicity and other individual and family characteristics (Table 1). About two-thirds of all black and Hispanic families experienced at least one type of disadvantage in the previous year, with more than half reporting material hardship and more than one in five facing an adult health problem. Among families from other ethnic backgrounds, including Asian-American, nearly half faced some kind of disadvantage in the previous year. While rates of disadvantage were lowest for white families, almost a third experienced at least one type of disadvantage. Survey participants who had no partner were more likely to face disadvantage. In addition, there were striking differences by level of education; study participants without a college degree had much higher prevalence of all types of disadvantage. Number of children was not significantly associated with measures of disadvantage.
Table 1.
Baseline prevalence of income poverty, material hardship, adult health problem, and any disadvantage by individual and family characteristics
| Income poverty (%) | Material hardship (%) | Adult health problem (%) | Any dis-advantage (%) | Unweighted N | |
|---|---|---|---|---|---|
| Race/ethnicity | |||||
| Black | 30 | 54 | 21 | 68 | 235 |
| Hispanic | 37 | 53 | 23 | 70 | 287 |
| White | 16 | 14 | 8 | 32 | 195 |
| Other | 28 | 31 | 14 | 46 | 81 |
| p-values | 0.002 | 0.000 | 0.009 | 0.000 | |
| Respondent partner status | |||||
| Partner | 19 | 34 | 15 | 46 | 410 |
| No partner | 42 | 47 | 21 | 70 | 388 |
| p-values | 0.000 | 0.003 | 0.113 | 0.000 | |
| Number of children | |||||
| 1-2 children | 27 | 38 | 18 | 55 | 649 |
| 3+ children | 33 | 45 | 14 | 60 | 149 |
| p-values | 0.263 | 0.202 | 0.413 | 0.380 | |
| Education | |||||
| Less than HS | 54 | 58 | 29 | 80 | 127 |
| High school | 30 | 47 | 16 | 61 | 210 |
| Some college | 23 | 41 | 18 | 57 | 204 |
| College graduate | 14 | 17 | 9 | 33 | 257 |
| p-values | 0.000 | 0.000 | 0.001 | 0.000 |
Note: All percentages are weighted.
The dynamics of disadvantage
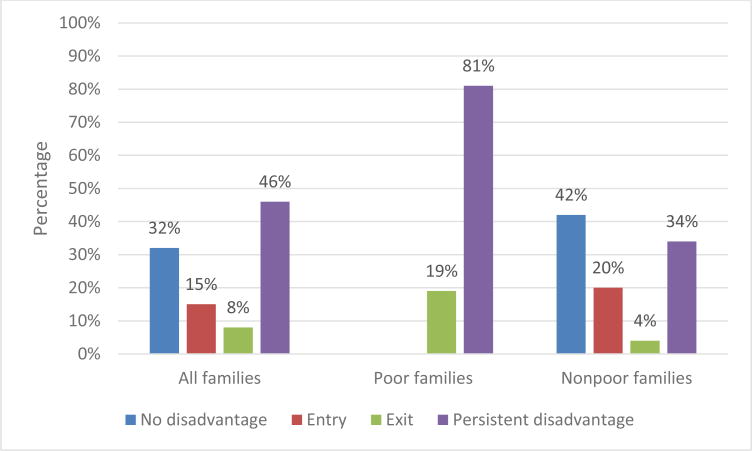
Figure 2 displays information on the dynamics of disadvantage. Nearly half of all families with children experienced “persistent” disadvantage – in other words, they faced at least one form of disadvantage at both baseline and follow-up. Only a third of all families faced none of these disadvantages at either time point. It is clear that figures on persistent poverty understate the level of sustained disadvantage that some families face: only 11% of families with children were poor at both time points, while 46% experienced some type of disadvantage at both time points. Among families who were poor at baseline, 81% experienced at least one type of disadvantage at follow-up. Even among nonpoor families, more than half faced some type of disadvantage at either baseline or follow-up.
Figure 2.
Change in disadvantage status between baseline and follow-up for all families with children and by family poverty; Note: All figures are weighted. Family poverty was assessed at baseline using the supplemental poverty measure. Disadvantaged families had at least one of these three characteristics: (1) poverty as assessed using the supplementary poverty measure, (2) material hardship, or (3) adult health problem. Families with “no disadvantage” were not classified as disadvantaged in either year. Families in the “entry” category were not disadvantaged at baseline and were disadvantaged at follow-up. Families in the “exit” category were disadvantaged at baseline and were not disadvantaged at follow-up. Families in the “persistent disadvantage” category were disadvantaged at both baseline and follow-up.
Differences in the dynamics of disadvantage largely parallel those for baseline disadvantage (Table 2). Black and Hispanic families had higher rates of persistent disadvantage, as did families in which the survey respondent did not have a spouse or domestic partner. Differences by number of children were not significant. Study participants with less education were much more likely to face disadvantage in one or both years.
Table 2. Dynamics of disadvantage by individual and family characteristics.
| No dis-advantage (%) | “Entry” to disadvantage (%) | “Exit” from disadvantage (%) | Persistent disadvantage (%) | UnweightedN | |
|---|---|---|---|---|---|
| Disadvantage at baseline | No | No | Yes | Yes | |
| Disadvantage at follow-up | No | Yes | No | Yes | |
| Race/ethnicity | |||||
| Black | 16 | 11 | 12 | 61 | 114 |
| Hispanic | 16 | 12 | 7 | 65 | 133 |
| White | 58 | 16 | 7 | 19 | 94 |
| Other race/ethnicity | 53 | 28 | 3 | 16 | 32 |
| p-value | 0.000 | ||||
| Respondent partner status | |||||
| Partner | 40 | 13 | 7 | 41 | 199 |
| No partner | 16 | 19 | 10 | 55 | 174 |
| p-value | 0.015 | ||||
| Number of children | |||||
| 1-2 children | 32 | 14 | 6 | 47 | 299 |
| 3+ children | 30 | 17 | 13 | 40 | 74 |
| p-value | 0.542 | ||||
| Education | |||||
| Less than HS | 9 | 13 | 8 | 71 | 42 |
| High school | 20 | 16 | 7 | 57 | 95 |
| Some college | 37 | 16 | 6 | 41 | 105 |
| College graduate | 56 | 13 | 11 | 20 | 131 |
| p-value | 0.002 | ||||
Note: All percentages are weighted.
Factors associated with risk of disadvantage
The first column of Table 3 displays odds ratios from multivariable logistic regressions predicting baseline and persistent disadvantage. Compared with white families, black and Hispanic families had significantly higher rates of baseline and persistent disadvantage. Study participants without a spouse or domestic partner were at higher risk of baseline disadvantage. Older respondents were more likely than younger respondents to experience persistent disadvantage. Compared with college graduates, study participants with less education were at significantly higher risk of both baseline and persistent disadvantage.
Table 3. Odds ratios from logistic regressions predicting any type of disadvantage and specific types of disadvantage at baseline and at both baseline and follow-up.
| Any disadvantage | Income poverty | Material hardship | Adult health problem | |
|---|---|---|---|---|
| Disadvantage at baseline | ||||
| Black | 2.17** | 1.19 | 3.41*** | 1.49 |
| Hispanic | 2.45*** | 1.35 | 3.38*** | 1.62 |
| Other race/ethnicity | 1.20 | 1.20 | 1.52 | 1.15 |
| No spouse or domestic partner | 2.00*** | 2.22*** | 1.24 | 1.81** |
| Three or more children | 1.36 | 1.25 | 1.20 | 1.13 |
| Age | 1.01 | 0.99 | 1.02** | 1.05*** |
| Less than high school | 6.38*** | 6.24*** | 3.19*** | 4.70*** |
| High school graduate | 3.08*** | 2.59*** | 2.97*** | 2.21** |
| Some college | 2.40*** | 1.68* | 2.53*** | 3.24*** |
| N | 798 | 798 | 798 | 798 |
| Disadvantage at both baseline and follow-up | ||||
| Black | 2.45* | 2.79 | 2.62* | 1.31 |
| Hispanic | 3.45*** | 3.03 | 2.76* | 1.97 |
| Other race/ethnicity | 0.99 | 0.76 | 0.91 | 0.71 |
| No spouse or domestic partner | 1.28 | 1.63 | 0.94 | 1.46 |
| Three or more children | 1.16 | 0.99 | 1.01 | 1.22 |
| Age | 1.04** | 1.01 | 1.03** | 1.07*** |
| Less than high school | 6.07*** | 10.10*** | 2.79* | 4.22** |
| High school graduate | 5.66*** | 5.62** | 3.37** | 1.07 |
| Some college | 3.20*** | 3.00 | 2.37* | 2.67* |
| N | 373 | 373 | 373 | 373 |
P-values:
<.05,
<.01,
<.001
The last three columns of Table 3 display odds ratios from models predicting baseline and persistent income poverty, material hardship, and adult health problems. Lower levels of education are associated with all three types of disadvantage, but there are differences across outcome in associations with other predictors. Race and ethnicity are associated with material hardship but not with poverty or adult health problems. Age is associated with material hardship and adult health problems but not with poverty.
Discussion and conclusion
Our survey of New Yorkers confirms that we would vastly underestimate the extent of disadvantage among families with children if we focused only on income poverty. The share of families experiencing disadvantage is twice as high as the share who experienced income poverty alone. This is because many families with incomes above the poverty line nevertheless experience material hardship and/or have family members who are in poor health. Figures on the dynamics of disadvantage also indicate high prevalence, with two-thirds of all families with children experiencing some kind of disadvantage at either baseline or follow-up; nearly half were disadvantaged at both time points.
Notably, survey respondents who had not graduated from college were much more likely to face either baseline or persistent disadvantage. They were also more likely to face all three specific types of disadvantage. Associations with other characteristics varied by outcome: income poverty was more common among respondents with no partner; material hardship was more common among older respondents and those who were black or Hispanic; and adult health problems were more common among older respondents and those with no partner. This heterogeneity is important to keep in mind particularly when we consider the causes of disadvantage.
In previous research, disadvantage has been defined as encompassing material hardship and income poverty.6, 26 The current study extends that work both by adding a new dimension of disadvantage – adult health problems – and by examining short-term change in patterns of disadvantage. Using this combined measure of disadvantage, the Poverty Tracker survey shows that economic disadvantage is widespread, with more than half of families with children in New York City experiencing disadvantage at baseline and two-third of such families experiencing disadvantage either at baseline or a year later. Future research will exploit the panel nature of the data to examine the implications of disadvantage for child and family well-being.
These findings suggest that in addition to addressing income poverty, policymakers should develop or expand initiatives that address material hardship and support families who are coping with chronic physical or mental illness. Examples of such initiatives include direct service provision, such as emergency food assistance, eviction prevention, and respite care for caregivers, as well as case manager or navigator-type services that connect families with existing resources. The results described here make it clear that the need for these resources extends far above the poverty line.
Strengths of the study include the use of a novel, multidimensional measure of disadvantage, as well as longitudinal data collection from a diverse sample. Readers should keep several limitations in mind. First, the sample represents residents of New York City and findings may not be generalizable to other locales. Second, the measure of adult health problems is based on the health and disability status of the survey respondent, not the entire household; therefore it understates the prevalence of serious health problems among New York City families. (Beginning with the 12-month follow-up, the Poverty Tracker survey includes questions about health and disability of the respondent's spouse or domestic partner, improving the quality of this measure.) Third, the Poverty Tracker excludes residents of institutions such as nursing homes, and may for that reason undercount individuals with very poor health. Fourth, although poverty, material hardship, and adult health problems put children at greater risk, the effects of these risk factors on child outcomes are moderated by other characteristics including social support networks and the quality of parent-child interactions.33, 34 Lastly, although baseline and follow-up study participants are both weighted so that they represent the population of New York City, attrition might have altered the composition of the sample in terms of unobservable characteristics, affecting the comparability of baseline and follow-up.
The Columbia Population Research Center recently launched a new cohort of the Poverty Tracker study. This new cohort is substantially larger, which will allow more detailed analyses of economic disadvantage especially when pooled with the first cohort. In addition, informed by analyses of the first cohort, we have expanded measures of health and other indicators of well-being. Future work based on this study will provide more insight into both the causes and the consequences of economic disadvantage.
Supplementary Material
Acknowledgments
Funding for this study was provided by the Robin Hood Foundation. The funder had no role in the preparation of this report.
Footnotes
Corporate support and conflicts of interest: The authors have no corporate support or conflicts of interest to report.
Contributor Information
Kathryn M. Neckerman, Email: kmn2@columbia.edu.
Irwin Garfinkel, Email: ig3@columbia.edu.
Julien O. Teitler, Email: jot8@columbia.edu.
Jane Waldfogel, Email: j.waldfogel@columbia.edu.
Christopher Wimer, Email: cw2727@columbia.edu.
References
- 1.Brooks-Gunn J, Duncan GJ. The Effects of Poverty on Children. The Future of Children. 1997;7:55–71. [PubMed] [Google Scholar]
- 2.Aber JL, Bennett NG, Conley DC, Li J. The Effects of Poverty on Child Health and Development. Annual Review of Public Health. 1997;18:463–483. doi: 10.1146/annurev.publhealth.18.1.463. [DOI] [PubMed] [Google Scholar]
- 3.Wood D. Effect of Child and Family Poverty on Child Health in the United States. Pediatrics. 2003;112:707–711. [PubMed] [Google Scholar]
- 4.Fox L, Wimer C, Garfinkel I, Kaushal N, Waldfogel J. Waging War on Poverty: Poverty Trends Using a Historical Supplemental Poverty Measure. Journal of Policy Analysis and Management. 2015;34:567–592. doi: 10.1002/pam.21833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frank DA, Casey PH, Black MM, et al. Cumulative Hardship and Wellness of Low-Income, Young Children: Multisite Surveillance Study. Pediatrics. 2010;125:e1115–e1123. doi: 10.1542/peds.2009-1078. [DOI] [PubMed] [Google Scholar]
- 6.Gershoff ET, Aber JL, Raver CC, Lennon MC. Income Is Not Enough: Incorporating Material Hardship Into Models of Income Associations With Parenting and Child Development. Child Development. 2007;78:70–95. doi: 10.1111/j.1467-8624.2007.00986.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zilanawala A, Pilkauskas NV. Material hardship and child socioemotional behaviors: Differences by types of hardship, timing, and duration. Children and Youth Services Review. 2012;34:814–825. doi: 10.1016/j.childyouth.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoo JP, Slack KS, Holl JL. Material Hardship and the Physical Health of School-Aged Children in Low-Income Households. American Journal of Public Health. 2009;99:829–836. doi: 10.2105/AJPH.2007.119776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashiabi GS, O'Neal KK. Children's Health Status: Examining the Associations among Income Poverty, Material Hardship, and Parental Factors. PLoS ONE. 2007;2:e940. doi: 10.1371/journal.pone.0000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spencer N. Does material disadvantage explain the increased risk of adverse health, educational, and behavioural outcomes among children in lone parent households in Britain? A cross sectional study. Journal of Epidemiology and Community Health. 2005;59:152–157. doi: 10.1136/jech.2004.020248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodman S, Rouse M, Connell A, Broth M, Hall C, Heyward D. Maternal Depression and Child Psychopathology: A Meta-Analytic Review. Clin Child Fam Psychol Rev. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 12.Minkovitz CS, Strobino D, Scharfstein D, et al. Maternal Depressive Symptoms and Children's Receipt of Health Care in the First 3 Years of Life. Pediatrics. 2005;115:306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- 13.Brennan PA, Hammen C, Andersen MJ, Bor W, Najman JM, Williams GM. Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology. 2000;36:759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- 14.Lieb R, Isensee B, Höfler M, Pfister H, Wittchen H. Parental major depression and the risk of depression and other mental disorders in offspring: A prospective-longitudinal community study. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- 15.Meadows SO, McLanahan SS, Brooks-Gunn J. Parental Depression and Anxiety and Early Childhood Behavior Problems Across Family Types. Journal of Marriage and Family. 2007;69:1162–1177. [Google Scholar]
- 16.Frech A, Kimbro RT. Maternal Mental Health, Neighborhood Characteristics, and Time Investments in Children. Journal of Marriage and Family. 2011;73:605–620. [Google Scholar]
- 17.Thastum M, Watson M, Kienbacher C, et al. Prevalence and predictors of emotional and behavioural functioning of children where a parent has cancer. Cancer. 2009;115:4030–4039. doi: 10.1002/cncr.24449. [DOI] [PubMed] [Google Scholar]
- 18.Bogosian A, Moss-Morris R, Hadwin J. Psychosocial adjustment in children and adolescents with a parent with multiple sclerosis: a systematic review. Clinical Rehabilitation. 2010;24:789–801. doi: 10.1177/0269215510367982. [DOI] [PubMed] [Google Scholar]
- 19.Rotheram-Borus M, Lee M, Lin Y, Lester P. SIx-year intervention outcomes for adolescent children of parents with the human immunodeficiency virus. Archives of Pediatrics & Adolescent Medicine. 2004;158:742–748. doi: 10.1001/archpedi.158.8.742. [DOI] [PubMed] [Google Scholar]
- 20.Romer G, Barkmann C, Schulte-Markwort M, Thomalla G, Riedesser P. Children of Somatically Ill Parents: A Methodological Review. Clinical Child Psychology and Psychiatry. 2002;7:17–38. [Google Scholar]
- 21.Hardie JH, Landale NS. Profiles of Risk: Maternal Health, Socioeconomic Status, and Child Health. Journal of Marriage and Family. 2013;75:651–666. doi: 10.1111/jomf.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brucker DL. Food security among young adults with disabilities in the United States: Findings from the National Health Interview Survey. Disability and Health Journal. 2015 doi: 10.1016/j.dhjo.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Heflin CH, Butler JS. Why Do Women Enter and Exit From Material Hardship? Journal of Family Issues. 2013;34:631–660. [Google Scholar]
- 24.Parish SL, Rose RA, Andrews ME. Income Poverty and Material Hardship among U.S. Women with Disabilities. Social Service Review. 2009;83:33–52. [Google Scholar]
- 25.Huang J. Work Disability, Mortgage Default, and Life Satisfaction in the Economic Downturn: Evidence from the Panel Study of Income Dynamics. Journal of Disability Policy Studies. 2012;22:237–246. [Google Scholar]
- 26.Mayer SE, Jencks C. Poverty and the Distribution of Material Hardship. The Journal of Human Resources. 1989;24:88–114. [Google Scholar]
- 27.Beverly SG. Material hardship in the United States: Evidence from the Survey of Income and Program Participation. Social Work Research. 2001;25:143–151. [Google Scholar]
- 28.Heflin CM. Dynamics of Material Hardship in the Women's Employment Study. Social Service Review. 2006;80:377–397. [Google Scholar]
- 29.Iceland J, Bauman KJ. Income poverty and material hardship: How strong is the association? The Journal of Socio-Economics. 2007;36:376–396. [Google Scholar]
- 30.Sullivan JX, Turner L, Danziger S. The relationship between income and material hardship. Journal of Policy Analysis and Management. 2008;27:63–81. [Google Scholar]
- 31.Adler NE, Rehkopf DH. U.S. Disparities in Health: Descriptions, Causes, and Mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 32.Rao J, Scott A. On Chi-Squared Tests for Multiway Contingency Tables with Cell Proportions Estimated from Survey Data. Ann Statist. 1984;12:46–60. [Google Scholar]
- 33.Ryan RM, Kalil A, Leininger L. Low-Income Mothers' Private Safety Nets and Children's Socioemotional Well-Being. Journal of Marriage and Family. 2009;71:278–297. [Google Scholar]
- 34.Murphy DA, Marelich WD, Herbeck DM, Payne DL. Family Routines and Parental Monitoring as Protective Factors Among Early and Middle Adolescents Affected by Maternal HIV/AIDS. Child Development. 2009;80:1676–1691. doi: 10.1111/j.1467-8624.2009.01361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.