Abstract
Background: Multiple sclerosis (MS) is a neurological disease with a variety of signs and symptoms. Exercise therapy has been shown to improve physical functions in MS. However, questions about an optimal exercise therapy remain. In this regard, we suggest a combined exercise therapy including aerobic and resistance exercises for MS patients. The study is designed to observe, test and compare the effects of proposed combined exercises on strength, balance, agility, fatigue, speed, and walking distance in people with mild to moderate MS [0 < expanded disability status scale (EDSS) < 5].
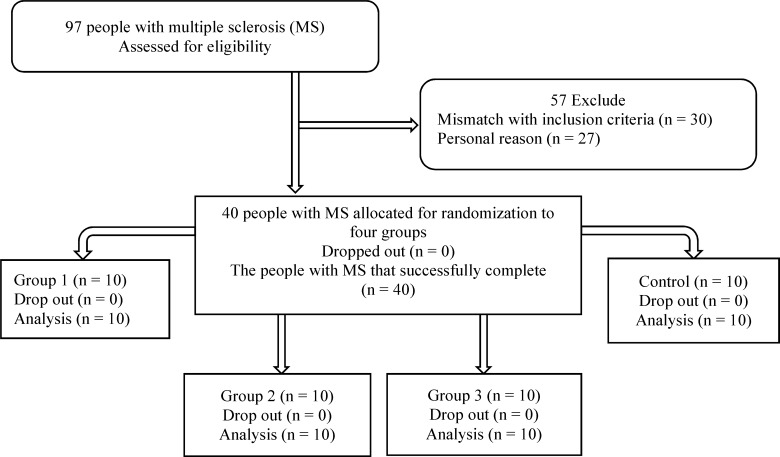
Methods: A total of 40 people with relapse-remitting MS (16 male, 0 < EDSS < 5) were randomized into one of the four groups (3 intervention and one control). The intervention consisted of various combinations of aerobic and resistance exercises with different repetition rates. Pre- and post-intervention scores of fatigue severity scale (FSS), timed up and go (TUG) test, 6-minute walk test (6MWT), 10- and 20-MWT, Berg balance scale (BBS), and one repetition maximum (1RM) test were recorded and analyzed.
Results: For most tests, post-intervention values of the group 1, with 3-aerobic and 1-resistance exercises, were significantly higher compared to control group (P < 0.050). However, no significant progression was observed in the other two intervention groups.
Conclusion: A combination of three aerobic exercises with one resistance exercise may result in improved balance, locomotion, and endurance in MS patients.
Key Words: Multiple Sclerosis, Exercise Therapy, Aerobic Exercise, Resistance Training
Introduction
Multiple sclerosis (MS) is an inflammatory demyelinating disorder of the central nervous system with both inflammation and neurodegeneration outcomes such as inflammatory attacks.1 Adults between 18 and 40 are commonly affected by MS with a relapsing-remitting and sometimes a steady progression course.2,3 The most common symptoms of MS include weakness, fatigue, and imbalance.2,3 Balance impairment, which can lead to falls and injuries, is reported in 78% of people with MS.4 There is no uniform and/or well-established pharmacologic method to resolve imbalance, fatigue and weakness in MS. However, rehabilitation methods may be helpful.5,6 A number of studies have reported the benefits of exercise and physical activity.7 On one hand, power exercises can ameliorate muscle weakness and improve coordination which, in turn, can improve balance, agility and decrease muscle spasticity.7-10 Further, studies have reported increased muscle strength and functional capacity, using different power exercises in people with MS.11-13 On the other hand, aerobic exercise has been shown to significantly decrease fatigue14 and increase walking distance15 or speed.16
Although several studies have approved the efficacy of exercise to improve balance in people with MS, each has followed a different exercise protocol and yielded different results. A gradual progression from simple exercises such as stationary biking or weight lifting, to a combination of exercises has been reported to be beneficial.6 For instance, combined exercises improved patients’ balance17-19 as well as endurance.20-22
Although combined exercises have proved effective,19,23 their complexity may force patients and professionals to do them in well-equipped centers. Besides, these types of interventions were conducted on patients with mild relapsing-remitting MS, with an expanded disability status scale (EDSS) of < 3.5. To best of our knowledge, there are no studies on the effects of exercise in MS patients with moderate to severe disability and in progressive type.5,8 Hence, the objective of this study is to observe, test and compare the effects of proposed combined exercises on strength, walking speed, walking distance, balance, agility and fatigue, in mild to moderate people with MS (0 < EDSS < 5).
Materials and Methods
This is a case-control randomized clinical trial. Due to obvious limitations, only those assessing the outcomes were blinded to group assignment. Members of Iranian MS Society (IMSS) were referred to IMSS physiotherapy center in Tehran, Iran, by their neurologists for rehabilitation program from September until November 2012. Demographic information of all patients was recorded in the center database, and those met the inclusion/exclusion criteria were advised to participant in the study. Finally, 40 people with MS were recruited and randomly assigned to four groups: three experimental and one control group. To avoid confounding effects, the four groups were matched on group characteristics [namely age, gender, body mass index (BMI), and social status].
Inclusion/exclusion criteria
The inclusion criteria include:
Definite relapse-remaining MS (RRMS)
Adults between 18 and 50 years of age
An EDSS level of 0-5
Right-handed
No history of systemic disease, concomitant neurological disorders, epilepsy, heart diseases, anemia, or severe depression.
The exclusion criteria include:
Under treatment with corticosteroid (in relapse time), or a history of recent attack (< 3 months)
Participants who completed < 30 sessions of exercise for any reason.
Participants were randomly assigned to four groups:
Group 1, which performed 1 aerobic exercise training and 3 resistance exercise training sessions per week
Group 2, which performed 2 aerobic exercise training and 2 resistance exercise training sessions per week
Group 3, Group 1, which performed 3 aerobic exercise training and 1 resistance exercise training session per week
Control group: All participants voluntarily filled the informed consent. Baseline scores were recorded within 5 days before the intervention and post-test scores were recorded exactly 72 hours after the end of the protocol for each group.
Outcome measures evaluated in this study are defined and measured as below:
One repetition maximum (1RM) test: To measure strength (heaviest weight a person can lift using quadriceps and hamstring muscles at first attempt)24,25
Berg balance scale (BBS): To measure balance26
10-minute walk test (10MWT) and 20MWT: To measure speed of movement29
BMI: Weight in kilograms divided by the square of height in centimeters.32
A JEXERS® exercise machine with a tolerance of 1 kg was used to measure the quadriceps and hamstring strength based on 1RM. Furthermore, a metal meter was used to measure the height of subjects in centimeters and a G200 BEURER® (China) digital scale with 100 g tolerance to measure the weight of cases.
In addition, BBS test was based on the Farsi version, which is a standard device in the IMSS rehabilitation center.26 To test for the walking speed, a running track in the gymnasium of rehabilitation center was measured and marked exactly at 10 and 20 m.33 For the TUG test, as mentioned in the manual, a chair, and a digital chronometer were used. The 6MWT was performed in a big gymnasium out of rehabilitation center.
Participants in the intervention groups performed exercises in groups. However, due to space and time limitations, it was not possible for all the groups to do the exercises simultaneously.34 Each group had four exercise sessions per week for 8 weeks (32 sessions). The interventions consisted of three stages per session: Stage 1: Warm up, Stage 2: main intervention and Stage 3: cool down.
Stage 1: in this stage, one of the trainers demonstrated simple stretches for the neck, upper/lower extremities, and the trunk. Subjects were asked to follow.
Stage 2: during the main interventional stage, each group followed their own program. For example, group 1 patients practiced individually tailored resistance exercises one session each week. For the next three sessions of the week, participants did two aerobic exercises: stationary bike and treadmill. Table 1 illustrates the workout routine for both resistance and aerobic exercises. For groups 2 and 3, the exercise sessions changed to 2 resistance/2 aerobic and 3 resistance/1 aerobic sessions per week, respectively. Maximum heart rate (MHR) of each person was tracked to prevent exhaustion while biking or using treadmill. During the 1st week, the aerobic exercise begun with about 40% of MHR and 10 minutes per each device, then it gradually increased up to 70% of MHR and 20 minutes for each aerobic exercise. In addition, strength exercises started with 50% of 1RM with 10 repetitions of 3 sets and increased up to 70% of 1RM with 10 repetitions and three sets of exercise for each flexor or extensor of both knees.24,25
Between two aerobic activities, bike and treadmill, and resistance sessions, extensors and flexors of the both knees, patients had a 10-minute and 5-minute inactive rest, respectively. If a patients’ heart rate reached above the limit, the exercise was stopped and the participant had to rest until the heart rate decreased (Tables 1 and 2).
Table 1.
Endurance exercises mode
| Exercise types | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | Week 7 | Week 8 |
|---|---|---|---|---|---|---|---|---|
| Cycling | 10 minutes | 10 minutes | 15 minutes | 15 minutes | 15 minutes | 20 minutes | 20 minutes | 20 minutes |
| 40% | 50% | 50% | 55% | 55% | 55% | 60% | 70% | |
| MHR | MHR | MHR | MHR | MHR | MHR | MHR | MHR | |
| Rest | 10 minutes | 10 minutes | 10 minutes | 10 minutes | 10 minutes | 10 minutes | 10 minutes | 10 minutes |
| Inactive | Inactive | Inactive | Inactive | Inactive | Inactive | Inactive | Inactive | |
| Walking on treadmill | 10 minutes | 10 minutes | 15 minutes | 15 minutes | 15 minutes | 20 minutes | 20 minutes | 20 minutes |
| 40% | 50% | 50% | 55% | 55% | 55% | 60% | 70% | |
| MHR | MHR | MHR | MHR | MHR | MHR | MHR | MHR |
MHR: Maximum heart rate
Table 2.
Strength exercises model
| Exercise kind | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | Week 7 | Week 8 |
|---|---|---|---|---|---|---|---|---|
| Knee extension | Intensity 50% 1RM | Intensity 55% 1RM | Intensity 60% 1RM | Intensity 60% 1RM | Intensity 65% 1RM | Intensity 65% 1RM | Intensity 70% 1RM | Intensity 70% 1RM |
| 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | |
| 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | |
| Rest time | 5 minutes | 5 minutes | 5 minutes | 5 minutes | 5 minutes | 5 minutes | 5 minutes | 5 minutes |
| Inactive | Inactive | Inactive | Inactive | Inactive | Inactive | Inactive | Inactive | |
| Knee flexion | Intensity 50% 1RM’ | Intensity 55% 1RM’ | Intensity 60% 1RM’ | Intensity 60% 1RM’ | Intensity 65% 1RM’ | Intensity 65% 1RM’ | Intensity 70% 1RM’ | Intensity 70% 1RM’ |
| 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | 3 times’ | |
| 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time | 10 repetitions each time |
1RM: One repetition maximum
Stage 3: one of the trainers demonstrated some simple stretching movements to ensure that all participants cooled down at the end of exercise sessions. Participants were further encouraged to take some fruit juice, date, biscuits, and milk.35
Ethical issues (including plagiarism, informed consent, research misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors. The Ethics Committee of Sport Science Research Institute of Iran approved the study protocol with Code No: S/93/398. For ethical reasons, at the end of the study the control group also received combinational exercises. All participants gave informed consent (both oral and written) in accordance with the declaration of Helsinki.
The normality of data was tested and confirmed by Kolmogorov-Smirnov test. Homogeneity of the four groups at baseline was confirmed using one-way ANOVA. Values from pre- (5 days before the intervention) and post-test (3 days after the intervention) were compared based on paired t-test. All data were analyzed using SPSS software (version 22, SPSS Inc., Chicago, IL, USA). An α-level of < 0.05 was considered significant.
Results
IMSS referred 97 RRMS patients to our rehabilitation center. According to the inclusion/exclusion criteria, 40 patients (24 female and 16 male) participated in the study; with mean disease duration of 2 years and BMI range of 18.5-25 kg/m2. All the patients successfully completed the procedure (Figure 1). There were 4 men and 6 women in each group. Table 3 gives descriptive statistics for age, height, weight, BMI and EDSS variables, separately for each group.
Figure 1.
Consort flowchart
Table 3.
Mean of age, height, weight, body mass index (BMI), and expanded disability status scale (EDSS) for all groups
| Groups |
Age (years)
|
Length (cm)
|
Weight (kg)
|
BMI (kg/m
2
)
|
EDSS (score)
|
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Experimental 1 (n = 10) | 35.80 ± 8.42 | 166.48 ± 6.99 | 68.13 ± 9.48 | 24.92 ± 2.76 | 1.33 ± 0.66 |
| Experimental 2 (n = 10) | 31.33 ± 8.21 | 164.97 ± 7.90 | 63.55 ± 13.65 | 23.99 ± 5.78 | 2.06 ± 0.86 |
| Experimental 3 (n = 10) | 33.91 ± 7.94 | 165.06 ± 8.56 | 66.92 ± 12.35 | 24.01 ± 3.35 | 1.95 ± 1.12 |
| Control (n = 10) | 33.63 ± 6.92 | 165.12 ± 7.59 | 63.00 ± 11.25 | 24.44 ± 4.78 | 1.81 ± 0.53 |
SD: Standard deviation; BMI: Body mass index; EDSS: Expanded disability status scale
Test results
6MWT: 6MWT score of the control group and the intervention group 1 did not change significantly comparing pre- and post-intervention values, whereas both intervention group 2 and 3 showed significant changes (P < 0.050) (Table 4). A comparison of post-test scores changes between groups declared a significantly higher score for groups 1 and 2 compared to the control group (P < 0.050).
Table 4.
Descriptive statistics for four studied groups’ variables before and after test
| Variable | Group | n | Average before test | SD | Average after test | SD | Difference between average after test and average before test | Difference percentage | P |
|---|---|---|---|---|---|---|---|---|---|
| 10MW speed (s) | Control | 10 | 15.217 | 18.94777 | 15.122 | 19.02946 | −0.095 | −0.624281255 | 0.758 |
| Group 1 | 10 | 9.828 | 4.89645 | 7.422 | 2.42591 | −2.4056 | −24.47750259 | 0.040* | |
| Group 2 | 10 | 8.109 | 2.08783 | 6.567 | 1.29852 | −1.5413 | −19.00774467 | 0.037* | |
| Group 3 | 10 | 9.874 | 5.56309 | 7.949 | 5.55153 | −1.925 | −19.49564513 | 0.014* | |
| 20MW speed (s) | Control | 10 | 29.085 | 32.02146 | 28.985 | 32.13234 | −0.1 | −0.343819838 | 0.908 |
| Group 1 | 10 | 19.953 | 10.04469 | 14.876 | 5.00254 | −5.0777 | −25.4479209 | 0.045* | |
| Group 2 | 10 | 17.124 | 4.31811 | 13.306 | 2.03388 | −3.8175 | −22.29353298 | 0.012* | |
| Group 3 | 10 | 17.248 | 5.31164 | 13.919 | 3.99213 | −3.329 | −19.3007885 | 0.014* | |
| Balance (score) | Control | 10 | 45.000 | 10.04277 | 45.000 | 9.74500 | 0 | 0 | 0.214 |
| Group 1 | 10 | 43.111 | 4.96096 | 49.000 | 2.34521 | 5.8889 | 13.65982311 | 0.010* | |
| Group 2 | 10 | 49.375 | 3.06769 | 50.625 | 1.84681 | 1.25 | 2.53164557 | 0.080 | |
| Group 3 | 10 | 45.400 | 8.93433 | 48.500 | 4.99444 | 3.1 | 6.828193833 | 0.060 | |
| Left knee extension strength (kg) | Control | 10 | 10.667 | 5.04645 | 11.333 | 6.43946 | 0.6666 | 6.249355471 | 0.146 |
| Group 1 | 10 | 12.000 | 5.3619 | 20.444 | 6.12599 | 8.4444 | 70.37 | 0.004* | |
| Group 2 | 10 | 19.000 | 10.01428 | 24.750 | 10.93814 | 5.75 | 30.26315789 | 0.029* | |
| Group 3 | 10 | 14.580 | 7.16377 | 23.200 | 8.70249 | 8.62 | 59.12208505 | 0.001* | |
| Right knee extension strength (kg) | Control | 10 | 14.667 | 3.26599 | 16.667 | 7.44759 | 2 | 13.63633264 | 0.458 |
| Group 1 | 10 | 12.111 | 5.1099 | 19.000 | 6.61438 | 6.8889 | 56.88087787 | 0.002* | |
| Group 2 | 10 | 21.375 | 9.31876 | 25.000 | 10.91526 | 3.625 | 16.95906433 | 0.340 | |
| Group 3 | 10 | 16.000 | 6.8313 | 24.300 | 8.53815 | 8.3 | 51.875 | 0.001* | |
| Left knee flexion strength (kg) | Control | 10 | 5.346 | 2.761 | 4.917 | 2.61566 | −0.42897 | −8.024625538 | 0.2390 |
| Group 1 | 10 | 7.422 | 3.50955 | 13.000 | 4.03113 | 5.5778 | 75.150225 | 0.015* | |
| Group 2 | 10 | 12.375 | 4.89716 | 15.500 | 5.47723 | 3.125 | 25.25252525 | 0.151 | |
| Group 3 | 10 | 7.060 | 2.49275 | 12.600 | 2.79682 | 5.54 | 78.47025496 | 0.001* | |
| Right knee flexion strength (kg) | Control | 10 | 8.205 | 3.55624 | 7.750 | 2.80624 | −0.4555 | −5.551154713 | 0.100 |
| Group 1 | 10 | 7.722 | 3.64958 | 12.333 | 4.74342 | 4.6111 | 59.71225816 | 0.080 | |
| Group 2 | 10 | 13.375 | 5.15302 | 17.250 | 5.94619 | 3.875 | 28.97196262 | 0.098 | |
| Group 3 | 10 | 8.850 | 2.80921 | 12.900 | 3.38132 | 4.05 | 45.76271186 | 0.012* | |
| 6MWT | Control | 10 | 361.500 | 238.86757 | 367.500 | 258.75692 | 6.0000 | 1.659751037 | 0.249 |
| Group 1 | 10 | 380.222 | 136.77790 | 461.444 | 139.61206 | 81.2222 | 21.36177674 | 0.057 | |
| Group 2 | 10 | 422.500 | 106.39012 | 491.500 | 108.79338 | 69.0000 | 16.33136095 | 0.034* | |
| Group 3 | 10 | 363.000 | 159.48319 | 396.500 | 154.32739 | 33.5000 | 9.228650138 | 0.043* |
SD: Standard deviation; 6MWT: 6 minute walking test; 10MW: 10 m walk
Significant at α level less than 0.05
10MWT: For 10MWT, all the three experimental groups showed a significant decrease in time taken to walk after the intervention (P < 0.050) (Table 4). The decreases in groups 1 to 3 were 2.4, 1.5 and 1.9 seconds, respectively. An average change in time taken to walk for group 1 was significantly different from control group (P = 0.030) (Table 5).
Table 5.
The groups compare to control group
| The tests | Groups | Mean difference | SE | P |
|---|---|---|---|---|
| Left knee flexion | Control group | |||
| Group 1 | −5.57 | 2.09 | 0.010* | |
| Group 2 | −3.12 | 2.14 | 0.150 | |
| Group 3 | −5.54 | 2.04 | 0.010* | |
| Right knee flexion | Control group | |||
| Group 1 | −4.61 | 1.89 | 0.020* | |
| Group 2 | −3.87 | 1.94 | 0.040* | |
| Group 3 | −4.05 | 1.85 | 0.010* | |
| Left knee extension | Control group | |||
| Group 1 | −7.77 | 2.73 | 0.010* | |
| Group 2 | −5.08 | 2.80 | 0.080 | |
| Group 3 | −7.95 | 2.68 | 0.010* | |
| Right knee extension | Control group | |||
| Group 1 | −4.88 | 3.48 | 0.170 | |
| Group 2 | −1.62 | 3.56 | 0.650 | |
| Group 3 | −6.30 | 3.41 | 0.070 | |
| Balance | Control group | |||
| Group 1 | −5.88 | 1.80 | < 0.001* | |
| Group 2 | −1.25 | 1.85 | 0.500 | |
| Group 3 | −3.10 | 1.75 | 0.090 | |
| 6MWT | Control group | |||
| Group 1 | −75.22 | 28.21 | 0.010* | |
| Group 2 | −63.00 | 29.03 | 0.040* | |
| Group 3 | −27.50 | 27.54 | 0.330 | |
| 10MW test | Control group | |||
| Group 1 | 2.31 | 1.04 | 0.030* | |
| Group 2 | 1.45 | 1.07 | 0.190 | |
| Group 3 | 1.83 | 1.01 | 0.080 | |
| 20MW test | Control group | |||
| Group 1 | 4.98 | 2.05 | 0.020* | |
| Group 2 | 3.72 | 2.11 | 0.090 | |
| Group 3 | 3.23 | 2.00 | 0.120 |
Significant at α level less than 0.05, SE: Standard error; 6MWT: 6 minute walking test; 10MW: 10 m walk
20MWT: In the 20MWT, time taken to walk significantly decreased after the intervention in experimental groups 1 (P = 0.045), 2 (P = 0.012) and 3 (P = 0.014) compared to the baseline values (day-0) (Table 4). In the control group, however, no significant change was observed (Table 4). An average change in time taken to walk for group 1 was significantly different from control group (P = 0.020) (Table 5).
BBS: BBS score significantly raised (about 6 points) after the intervention only for group 1 (P = 0.010) (Table 4). Group 1 score change was also significantly higher compared to the control group (P < 0.001) (Table 5).
Right knee extension and flexion strength (dominant leg): Right knee extension strength significantly increased in experimental groups 1 and 3 (P < 0.050). However, only group 3 showed a significant improvement of flexion strength (P = 0.012) (Table 4). A comparison of mean score change (post- and pre-score) indicated that flexion strength changes for intervention groups were significantly different from control group (P = 0.020, P = 0.040 and P = 0.010, respectively) (Table 5).
Left knee extension and flexion strength (non-dominant leg): Extension strength score significantly changed in all the intervention groups (P < 0.050). Average scores increased 8.4, 5.7 and 8.6 kg in groups 1 to 3, respectively. Moreover, flexion strength significantly changed in groups 1 and 3 (P = 0.015 and P = 0.001, respectively) (Table 4). A comparison of mean change in flexion and extension strength between groups showed that in groups 1 and 3, changes were significantly different from that of the control group (P = 0.010) (Table 5).
TUG test and FSS: A statistical analysis of both TUG test and FSS values did not indicate any significant change within groups.
In addition, based on post-hoc analysis of mean score change, none of the pair-wise comparisons of intervention groups were significantly different in 6MWT, 10MWT, 20MWT, right and left knee extension/flexion (P > 0.050).
Discussion
Our study was a randomized clinical trial to evaluate the effects of proposed combined exercises to improve muscle strength, balance, walking distance, and motor agility in patients with MS. We can divide the result into four sub-categories to discuss; the first part relates to tests that evaluated the strength of flexor and extensor muscles of the knees. The second part includes the tests that evaluated features of walking. The third and fourth parts are balance and fatigue scales.
Our findings showed a significant improvement of measures in intervention group 1, for which the dominant activity was aerobic exercise. Furthermore, they were in accordance with the studies of Dalgas et al.,5 Le Page et al.,8 Kjolhede et al.,9 Motl et al.,36 and Sangelaji et al.,19 However, Hansen et al.37 reported ineffectiveness of combined exercises, which may be due to application of different methods and measures as he used heart rate and blood examination. Significant strength improvements were observed in almost all knee flexor and extensor muscles in groups 1 and 3, but not group 2. These findings are in concordance with those of DeBolt and McCubbin,38 Kjolhede et al.,9 Le Page et al.8 and Medina-Perez et al.39 Although one would expect increase in muscle strength through resistance exercises, it was remarkable to note the increase in muscle strength with endurance exercises for group 1. A reason could be the fact that exercises such as stationary bike and treadmill walking may strengthen people with MS who lack regular exercise. This may also be a reason why significant improvement was detected for the non-dominant leg (left) and not the dominant leg (right).
Walking features, namely duration and speed were tested by 10MW and 20MW tests as well as 6MWT. The results showed a pattern of effectiveness for aerobic exercises. For all three tests, group 1 showed a greater improvement compared to control group. In addition, a significant change was observed for group 2 in 6MWT. These results are in agreement with those of other studies including Cakt et al.,40 Rampello et al.,16 Geddes et al.,41 Motl et al.,36 Sangelaji et al.,19 and van den Berg et al.,42 which showed an improvement in walking endurance and speed after combined exercises. In addition, a systematic review by Citaker et al.43 showed a small significant change in mobility after exercise therapy. Hansen et al.,37 however, showed that combined exercises have no effects on endurance. The discrepancy between results could be explained by the differences in employed exercises and mobility measures. It seems that aerobic exercises such as treadmill can improve the gait style of the people with MS as well as their endurance and strength. With respect to our study design, no specific balance exercise was performed by the patients but the results showed a significantly greater post-intervention balance score for group 1 compared to both baseline and control group. The difference in the scores of two groups which reached nearly 6 points (P = 0.001) is noteworthy. This is in line with a study by Donoghue and Stokes44 that investigated the changes in Berg test corresponding to real changes in patients.
In addition, our results matches, other studies like Paltamaa et al.,21 Kjolhede et al.,9 Sangelaji et al.,19 and Tarakci et al.23 In a study by Tarakci et al., the main reason for a significant difference between intervention and control groups was the odd point decrease of BBS in the control group in just 12 weeks and no increase in intervention group. It seems that treadmill as an aerobic exercise has some collateral effect such as balance improvement. Due to the nature of this kind of physical activity, some muscles that are effective in balance such as erector spinal muscles,23 may have strengthen and this phenomena may lead to improve balance in group 1 only and no the other groups. Studies by DeBolt and McCubbin38 and Rietberg et al.7 were in line with this concept. Some recent studies have focused on more specific muscles, such as Cakt et al.,40 Cattaneo et al.20 and Citaker et al.43 they all confirmed the effectiveness of resistance exercise on balance. Our results did not show any significant effect on fatigue.
Fatigue is one of the most complicated symptoms in MS and the results of various studies on fatigue are contradicting. For instance, Sangelaji et al.,19 Cakt et al.,40 Schmidt and Wonneberger45 and Tarakci et al.23 reported a mild to moderate effect of aerobic, resistance and combined exercises on fatigue; however, van den Berg et al.,42 Rietberg et al.,7 Hansen et al.,37 and Geddes et al.41 did not find any significant effect of various type of exercise on fatigue. In addition, Surakka et al.46 reported a significant effect of aerobic activities on fatigue just in females. This discrepancy may be a result of varying interventions, insufficient intervention periods and examined population. Although TUG test score changes in groups 1 and 3 were significantly before and after the intervention, no significant change was detected in comparison with control group. Motl et al.,36 and Golzari et al.,17 however, showed that combined exercises have a significant effect on TUG test. This paradox could be due to the small sample size of intervention groups.
Main highlights of the present study are the choice of accessible exercises, use of a randomized controlled trial (RCT) study design and collaboration of various professionals (e.g., neurologist, physiotherapist, physical educator and epidemiologist).
Two major limitations were inability to control for diet attitude or sleep-wakefulness schedule of the participants. Furthermore, mood state of the participants was not controlled during the study course. In addition, because of space and time limitations, groups did their exercises in different sessions, so we could not match the groups based on the exact time of physical activity.
Conclusion
Our study showed that a combined exercise schedule with a predominant aerobic component was more effective. The proposed model may help people with MS and can lead to improved balance skills, better walking abilities, and enhanced muscle strength. Furthermore, all modalities used in this model are simple, convenient and feasible. Hence, the proper combination of aerobic exercises with smaller portions of resistance exercises may be much more suitable for patients with MS. On the other hand, we showed a tangible improvement in test scores and scales after the intervention, specifically for groups 1 and 3; so we may speculate that rehabilitation and exercise therapy can help people with MS even in short-term. Finally, RCTs with large sample size and various exercise combinations are recommended to select the best rehabilitation regimen for people with MS.
Acknowledgments
The authors would like to thank all patients for their participation, as well as Ms. Zahra Gholami and her Colleagues at Iran MS Society and Ms. Maghsodi for their kind assistance. Finally yet importantly, we are grateful for the help of Dr. Catherine Smith and Mr. Kesava Kovanur Sampath in translation and methodological advice. The study is funded by Sport Science Research Institute of Iran.
Conflict of Interests
The authors declare no conflict of interest in this study.
Notes:
How to cite this article: Sangelaji B, Kordi M, Banihashemi F, Nabavi SM, Khodadadeh S, Dastoorpoor M. A combined exercise model for improving muscle strength, balance, walking distance, and motor agility in multiple sclerosis patients: A randomized clinical trial. Iran J Neurol 2016; 15(3): 111-20.
References
- 1.Dua T. In: Atlas: Multiple sclerosis resources in the world, 2008. Switzerland , editor. Geneva: World Health Organization; 2008. [Google Scholar]
- 2.Hauser S, Josephson S. Harrison's neurology in clinical medicine. 3rd ed. New York, NY: McGraw Hill Professional; 2013. [Google Scholar]
- 3.Umphred DA, Roller M. Neurological rehabilitation: Neurological rehabilitation. 6th ed. . Philadelphia, PA: Elsevier Health Sciences; 2013. [Google Scholar]
- 4.Nilsagard YE, von Koch LK, Nilsson M, Forsberg AS. Balance exercise program reduced falls in people with multiple sclerosis: a single-group, pretest-posttest trial. Arch Phys Med Rehabil. 2014;95(12):2428–34. doi: 10.1016/j.apmr.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 5.Dalgas U, Stenager E, Ingemann-Hansen T. Multiple sclerosis and physical exercise: recommendations for the application of resistance-, endurance- and combined training. Mult Scler. 2008;14(1):35–53. doi: 10.1177/1352458507079445. [DOI] [PubMed] [Google Scholar]
- 6.Sa MJ. Exercise therapy and multiple sclerosis: A systematic review. J Neurol. 2014;261(9):1651–61. doi: 10.1007/s00415-013-7183-9. [DOI] [PubMed] [Google Scholar]
- 7.Rietberg MB, Brooks D, Uitdehaag BM, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;(1):CD003980. doi: 10.1002/14651858.CD003980.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Page C, Ferry A, Rieu M. Effect of muscular exercise on chronic relapsing experimental autoimmune encephalomyelitis. J Appl Physiol (1985) 1994;77(5):2341–7. doi: 10.1152/jappl.1994.77.5.2341. [DOI] [PubMed] [Google Scholar]
- 9.Kjolhede T, Vissing K, Dalgas U. Multiple sclerosis and progressive resistance training: a systematic review. Mult Scler. 2012;18(9):1215–28. doi: 10.1177/1352458512437418. [DOI] [PubMed] [Google Scholar]
- 10.Sosnoff J, Motl RW, Snook EM, Wynn D. Effect of a 4-week period of unloaded leg cycling exercise on spasticity in multiple sclerosis. NeuroRehabilitation. 2009;24(4):327–31. doi: 10.3233/NRE-2009-0486. [DOI] [PubMed] [Google Scholar]
- 11.Dalgas U, Stenager E, Jakobsen J, Petersen T, Hansen HJ, Knudsen C, et al. Resistance training improves muscle strength and functional capacity in multiple sclerosis. Neurology. 2009;73(18):1478–84. doi: 10.1212/WNL.0b013e3181bf98b4. [DOI] [PubMed] [Google Scholar]
- 12.White LJ, McCoy SC, Castellano V, Gutierrez G, Stevens JE, Walter GA, et al. Resistance training improves strength and functional capacity in persons with multiple sclerosis. Mult Scler. 2004;10(6):668–74. doi: 10.1191/1352458504ms1088oa. [DOI] [PubMed] [Google Scholar]
- 13.Taylor NF, Dodd KJ, Prasad D, Denisenko S. Progressive resistance exercise for people with multiple sclerosis. Disabil Rehabil. 2006;28(18):1119–26. doi: 10.1080/09638280500531834. [DOI] [PubMed] [Google Scholar]
- 14.Petajan JH, Gappmaier E, White AT, Spencer MK, Mino L, Hicks RW. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann Neurol. 1996;39(4):432–41. doi: 10.1002/ana.410390405. [DOI] [PubMed] [Google Scholar]
- 15.Rodgers MM, Mulcare JA, King DL, Mathews T, Gupta SC, Glaser RM. Gait characteristics of individuals with multiple sclerosis before and after a 6-month aerobic training program. J Rehabil Res Dev. 1999;36(3):183–8. [PubMed] [Google Scholar]
- 16.Rampello A, Franceschini M, Piepoli M, Antenucci R, Lenti G, Olivieri D, et al. Effect of aerobic training on walking capacity and maximal exercise tolerance in patients with multiple sclerosis: a randomized crossover controlled study. Phys Ther. 2007;87(5):545–55. doi: 10.2522/ptj.20060085. [DOI] [PubMed] [Google Scholar]
- 17.Golzari Z, Shabkhiz F, Soudi S, Kordi MR, Hashemi SM. Combined exercise training reduces IFN-gamma and IL-17 levels in the plasma and the supernatant of peripheral blood mononuclear cells in women with multiple sclerosis. Int Immunopharmacol. 2010;10(11):1415–9. doi: 10.1016/j.intimp.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Latimer-Cheung AE, Pilutti LA, Hicks AL, Martin Ginis KA, Fenuta AM, MacKibbon KA, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94(9):1800–28. doi: 10.1016/j.apmr.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 19.Sangelaji B, Nabavi SM, Estebsari F, Banshi MR, Rashidian H, Jamshidi E, et al. Effect of combination exercise therapy on walking distance, postural balance, fatigue and quality of life in multiple sclerosis patients: a clinical trial study. Iran Red Crescent Med J. 2014;16(6):e17173. doi: 10.5812/ircmj.17173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cattaneo D, Jonsdottir J, Zocchi M, Regola A. Effects of balance exercises on people with multiple sclerosis: a pilot study. Clin Rehabil. 2007;21(9):771–81. doi: 10.1177/0269215507077602. [DOI] [PubMed] [Google Scholar]
- 21.Paltamaa J, Sjogren T, Peurala SH, Heinonen A. Effects of physiotherapy interventions on balance in multiple sclerosis: a systematic review and meta-analysis of randomized controlled trials. J Rehabil Med. 2012;44(10):811–23. doi: 10.2340/16501977-1047. [DOI] [PubMed] [Google Scholar]
- 22.Giesser B, Beres-Jones J, Budovitch A, Herlihy E, Harkema S. Locomotor training using body weight support on a treadmill improves mobility in persons with multiple sclerosis: a pilot study. Mult Scler. 2007;13(2):224–31. doi: 10.1177/1352458506070663. [DOI] [PubMed] [Google Scholar]
- 23.Tarakci E, Yeldan I, Huseyinsinoglu BE, Zenginler Y, Eraksoy M. Group exercise training for balance, functional status, spasticity, fatigue and quality of life in multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2013;27(9):813–22. doi: 10.1177/0269215513481047. [DOI] [PubMed] [Google Scholar]
- 24.Kisner C, Colby LA. Therapeutic Exercise: Foundations and Techniques. Philadelphia, PA: F.A. Davis; 2012. [Google Scholar]
- 25.Cormie P, McCaulley GO, Triplett NT, McBride JM. Optimal loading for maximal power output during lower-body resistance exercises. Med Sci Sports Exerc. 2007;39(2):340–9. doi: 10.1249/01.mss.0000246993.71599.bf. [DOI] [PubMed] [Google Scholar]
- 26.Azad A, Taghizadeh G, Khaneghini A. Assessments of the reliability of the Iranian version of the Berg Balance Scale in patients with multiple sclerosis. Acta Neurol Taiwan. 2011;20(1):22–8. [PubMed] [Google Scholar]
- 27.Cattaneo D, Regola A, Meotti M. Validity of six balance disorders scales in persons with multiple sclerosis. Disabil Rehabil. 2006;28(12):789–95. doi: 10.1080/09638280500404289. [DOI] [PubMed] [Google Scholar]
- 28.Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 29.Kieseier BC, Pozzilli C. Assessing walking disability in multiple sclerosis. Mult Scler. 2012;18(7):914–24. doi: 10.1177/1352458512444498. [DOI] [PubMed] [Google Scholar]
- 30.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 31.Chipchase SY, Lincoln NB, Radford KA. Measuring fatigue in people with multiple sclerosis. Disabil Rehabil. 2003;25(14):778–84. doi: 10.1080/0963828031000093477. [DOI] [PubMed] [Google Scholar]
- 32.NIH. Calculate your body mass index [Online] [[cited 2011]]. Available from: URL: http://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm.
- 33.Wolf SL, Catlin PA, Gage K, Gurucharri K, Robertson R, Stephen K. Establishing the reliability and validity of measurements of walking time using the Emory Functional Ambulation Profile. Phys Ther. 1999;79(12):1122–33. [PubMed] [Google Scholar]
- 34.Feys P, Gijbels D, Romberg A, Santoyo C, Gebara B, de Noordhout BM, et al. Effect of time of day on walking capacity and self-reported fatigue in persons with multiple sclerosis: a multi-center trial. Mult Scler. 2012;18(3):351–7. doi: 10.1177/1352458511419881. [DOI] [PubMed] [Google Scholar]
- 35.Sangelaji B, Hatamizadeh N, Rashvand F, Kazemnejad A. Study about the effects of rehabilitation on quality of life in multiple sclerosis patients. J Nurs Midwifery Shahid Beheshti Univ Med Sci. 2010;20(71):36–41. [Google Scholar]
- 36.Motl RW, Smith DC, Elliott J, Weikert M, Dlugonski D, Sosnoff JJ. Combined training improves walking mobility in persons with significant disability from multiple sclerosis: a pilot study. J Neurol Phys Ther. 2012;36(1):32–7. doi: 10.1097/NPT.0b013e3182477c92. [DOI] [PubMed] [Google Scholar]
- 37.Hansen D, Wens I, Keytsman C, Eijnde BO, Dendale P. Is long-term exercise intervention effective to improve cardiac autonomic control during exercise in subjects with multiple sclerosis? A randomized controlled trial. Eur J Phys Rehabil Med. 2015;51(2):223–31. [PubMed] [Google Scholar]
- 38.DeBolt LS, McCubbin JA. The effects of home-based resistance exercise on balance, power, and mobility in adults with multiple sclerosis. Arch Phys Med Rehabil. 2004;85(2):290–7. doi: 10.1016/j.apmr.2003.06.003. [DOI] [PubMed] [Google Scholar]
- 39.Medina-Perez C, de Souza-Teixeira F, Fernandez-Gonzalo R, de Paz-Fernandez JA. Effects of a resistance training program and subsequent detraining on muscle strength and muscle power in multiple sclerosis patients. NeuroRehabilitation. 2014;34(3):523–30. doi: 10.3233/NRE-141062. [DOI] [PubMed] [Google Scholar]
- 40.Cakt BD, Nacir B, Genc H, Saracoglu M, Karagoz A, Erdem HR, et al. Cycling progressive resistance training for people with multiple sclerosis: a randomized controlled study. Am J Phys Med Rehabil. 2010;89(6):446–57. doi: 10.1097/PHM.0b013e3181d3e71f. [DOI] [PubMed] [Google Scholar]
- 41.Geddes EL, Costello E, Raivel K, Wilson R. The effects of a twelve-week home walking program on cardiovascular parameters and fatigue perception of individuals with multiple sclerosis: a pilot study. Cardiopulm Phys Ther J. 2009;20(1):5–12. [PMC free article] [PubMed] [Google Scholar]
- 42.van den Berg M, Dawes H, Wade DT, Newman M, Burridge J, Izadi H, et al. Treadmill training for individuals with multiple sclerosis: a pilot randomised trial. J Neurol Neurosurg Psychiatry. 2006;77(4):531–3. doi: 10.1136/jnnp.2005.064410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Citaker S, Guclu-Gunduz A, Yazici G, Bayraktar D, Nazliel B, Irkec C. Relationship between lower extremity isometric muscle strength and standing balance in patients with multiple sclerosis. NeuroRehabilitation. 2013;33(2):293–8. doi: 10.3233/NRE-130958. [DOI] [PubMed] [Google Scholar]
- 44.Donoghue D, Stokes EK. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med. 2009;41(5):343–6. doi: 10.2340/16501977-0337. [DOI] [PubMed] [Google Scholar]
- 45.Schmidt S, Wonneberger M. Long-term endurance exercise improves aerobic capacity in patients with relapsing-remitting multiple sclerosis: impact of baseline fatigue. J Neurol Sci. 2014;336(1-2):29–35. doi: 10.1016/j.jns.2013.09.035. [DOI] [PubMed] [Google Scholar]
- 46.Surakka J, Romberg A, Ruutiainen J, Aunola S, Virtanen A, Karppi SL, et al. Effects of aerobic and strength exercise on motor fatigue in men and women with multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2004;18(7):737–46. doi: 10.1191/0269215504cr780oa. [DOI] [PubMed] [Google Scholar]