Abstract
Objectives: Unexpected systemic inflammatory response with high fever and increase in C-reactive protein (CRP) occurred frequently after endovascular abdominal aortic aneurysm repair (EVAR). This excessive inflammatory response affects the postoperative course. We evaluated the effects of steroid on the postoperative inflammatory response after EVAR.
Methods: Steroid therapy, intravenous infusion of methylprednisolone 1000 mg just after the anesthesia induction, was started since December 2012. After induction of the steroid therapy, 25 patients underwent EVAR with steroid therapy (Group S). These patients were compared with the 65 patients who underwent EVAR without steroid therapy (Group C) in white blood cell count (WBC), CRP and maximum body temperature (BT) on postoperative day 1–5.
Results: There was no significant difference in age, female gender, operation time, maximum aneurysm diameter between the two groups. There was no postoperative infective complication in the both groups. WBC did not differ between the two groups; however, CRP was significantly suppressed in Group S than in Group C on POD 1, 3 and 5. Also BT was significantly lower in Group S than Group C on POD 1, 2 and 3.
Conclusions: Steroid pretreatment before implantation of the stent graft reduces the early postoperative inflammatory response after EVAR, without increasing postoperative infection. (This is a translation of Jpn J Vasc Surg 2015; 24: 861–865.)
Keywords: stent graft, inflammation, steroid
Introduction
After endovascular abdominal aortic aneurysm repair (EVAR), fever and an increase in the inflammatory response frequently occur, and fever reduces appetite or activities of daily living (ADL) in some cases. We examined the effects of steroids with potent anti-inflammatory actions on inflammation after EVAR.
Subjects and Methods
Of 106 patients who underwent elective surgery after August 2009, when EVAR was introduced in our hospital, the subjects were 90, excluding emergencies, patients with inflammatory aortic aneurysms, those who had received steroids due to concomitant diseases before surgery, and one who died of postoperative disseminated intravascular coagulation (DIC) during the perioperative period (non-steroid-treated patient). The administration of an antibiotic after surgery was completed on the 1st postoperative day, and a non-opioid was used to relieve postoperative pain.
From February 2013, methylprednisolone at 1000 mg was intravenously administered on anesthesia induction, and the subjects were divided into two groups: methylprednisolone-treated (Group S, n = 25) and non-methylprednisolone-treated (Group C, n = 65) groups. The white blood cell count (WBC) and C-reactive protein (CRP) level were measured on admission, immediately after surgery, and 1, 3, and 5 days after surgery. The body temperature was determined every day until 5 days after surgery, and the maximum body temperature per day was regarded as the body temperature on the day. Furthermore, dietary intake was used as an index of activity. Each dietary intake was recorded using 10 grades, and the mean daily dietary intake was calculated. As there are individual differences in dietary intake at ordinary times, we investigated postoperative dietary intake as a percentage of dietary intake the day before surgery. For statistical analysis, the t- and chi square tests were used. A p-value of 0.05 was regarded as significant.
Results
There were no significant differences in the age, sex, operation time, or aneurysmal diameter between the two groups. There was no postoperative infection in any patient. Furthermore, there was no type-I/-III/-IV postoperative endoleak in any patient. There was no difference in the incidence of type-II postoperative endoleak between the two groups (Table 1).
Table 1.
Patient profile
| Group C (n = 65) | Group S (n = 25) | p-value | |
|---|---|---|---|
| Age (year) | 77.0 ± 6.8 | 77.4 ± 7.8 | 0.800 |
| Female gender | 16 (24.6%) | 7 (28%) | 0.952 |
| Operation time (min) | 123 ± 28 | 121 ± 34 | 0.837 |
| Aneurysm diameter (mm) | 49.7 ± 9.9 | 52.0 ± 9.1 | 0.319 |
| Postoperative infection | 0 | 0 | |
| Postoperative endoleak (type II) | 9 (13.8%) | 4 (16%) | 0.941 |
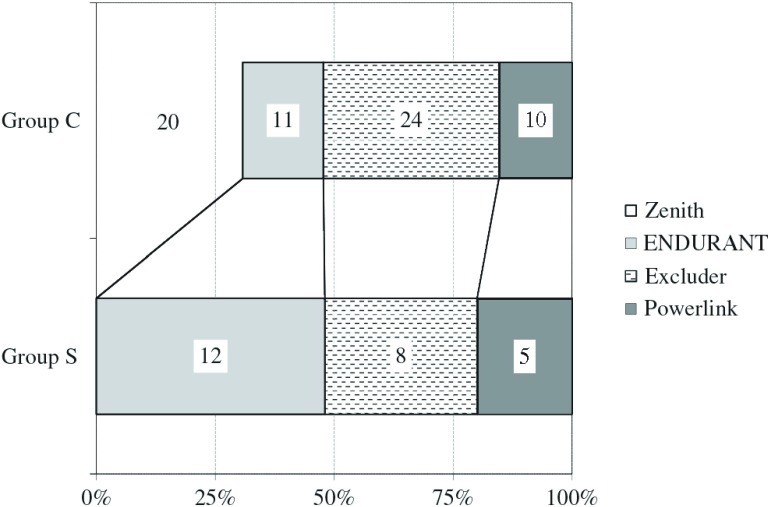
Devices varied, as there were differences in the timing of surgery. However, as a graft material, woven accounted for 48% in the two groups; there was no difference between the two groups (Fig. 1).
Fig. 1.
Device types.
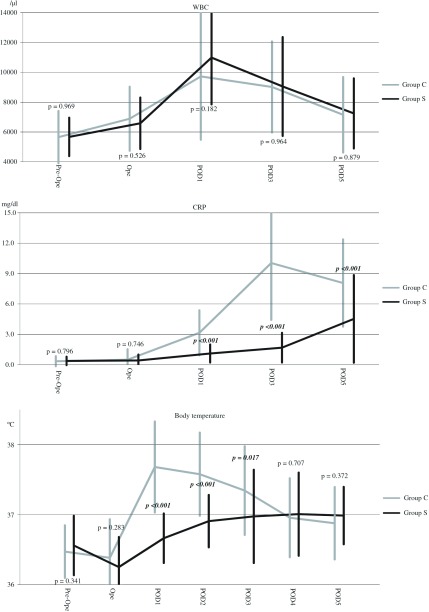
There was no significant difference in the WBC between the two groups at any point before/after surgery. In Group S, the CRP level was significantly lower than in Group C on the 1st, 3rd, and 5th postoperative days. In Group S, the body temperature was also significantly lower on the 1st, 2nd, and 3rd postoperative days (Fig. 2). In Group C, patients with fever (38°C or higher) after surgery accounted for 72% (n = 18) on the 1st postoperative day and 60% (n = 15) on the 2nd postoperative day. In Group S, there was no patient with fever (38°C or higher) until the 2nd postoperative day (Table 2).
Fig. 2.
Postoperative white blood cell, C-reactive protein and maximum body temperature in Group C and Group S. WBC: white blood cell; CRP: C-reactive protein; BT: maximum body temperature; POD: postoperative day; CRP: C-reactive protein; WBC: white blood cell count; Ope: operation
Table 2.
Occurrence of high fever (>38°C) on postoperative day 1 and 2
| Group C (n = 25) | Group S (n = 65) | p-value | |
|---|---|---|---|
| Ope | 1 (4%) | 0 (0%) | 1.000 |
| POD1 | 18 (72%) | 0 (0%) | 0.002 |
| POD2 | 15 (60%) | 0 (0%) | 0.009 |
| POD3 | 12 (48%) | 2 (3.1%) | 0.333 |
| POD4 | 2 (8%) | 1 (1.5%) | 1.000 |
| POD5 | 0 (0%) | 0 (0%) | 1.000 |
POD: postoperative day; Ope: operation
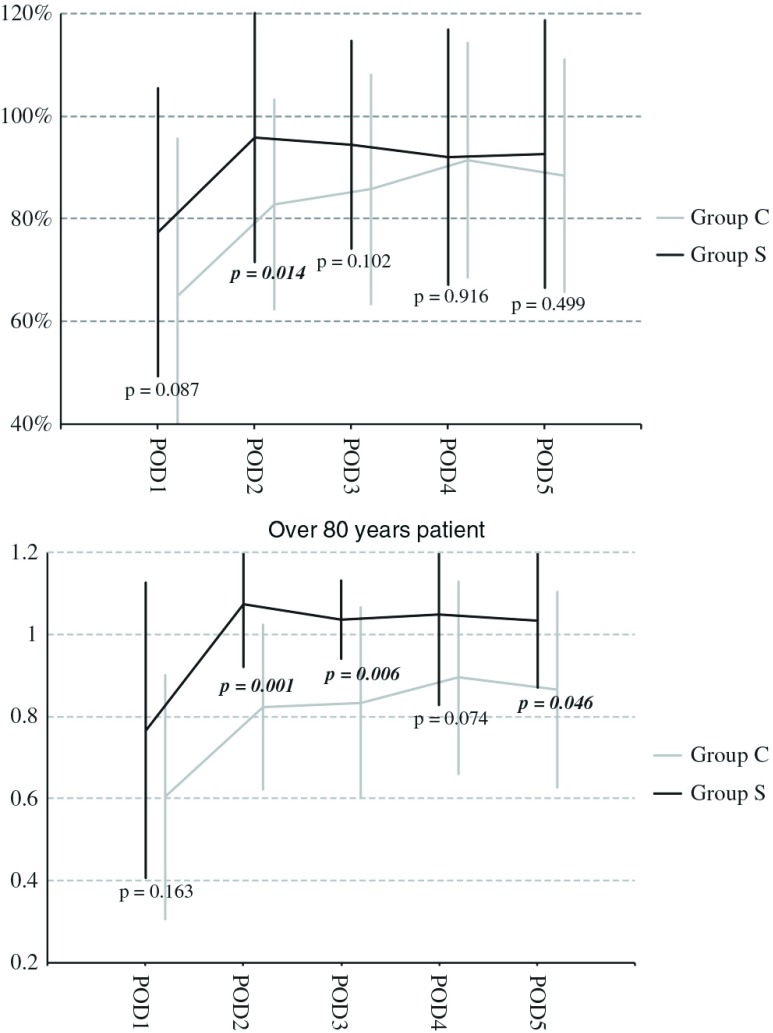
Dietary intake was significantly lower in Group C on the 2nd postoperative day. Among patients aged 80 years or older, it was slightly lower in Group C until the 5th postoperative day. There were significant differences on the 2nd, 3rd, and 5th postoperative days (Fig. 3).
Fig. 3.
Perioperative meal intake in all patients (above) and patients over 80 years (below). POD: postoperative day
Discussion
Since the era of self-making stent grafts, it has been known that systemic inflammatory responses occur after EVAR.1) The condition is termed post-implantation syndrome (PIS).2) PIS causes fever, leukocytosis, an increase in the CRP level, and increases in the levels of inflammatory markers, such as interleukin (IL)-6 and -8.3–6) Pyretolysis is not achieved by antibiotic therapy, and there is a negative reaction on blood culture; therefore, the possibility of infection-related inflammation is ruled out. Concerning the mechanism of PIS, a study reported that the insertion of a stent graft led to the rapid progression of intra-aneurysmal thrombosis, causing inflammation.7) Others suggested the influence of surgical procedures and device materials; the detailed mechanism remains to be clarified. Furthermore, the incidence of PIS ranges from 3 to 94% due to differences in the definition of PIS.2,8) A study compared EVAR with open surgery, and indicated that fever after open surgery was observed in 38% of the patients, whereas post-EVAR fever was noted in 72%,9) suggesting that PIS is a phenomenon specific to EVAR. We consider that even EVAR, which is minimally invasive, may reduce appetite or ADL through fever, and that inhibition of postoperative inflammation leads to an improvement in the quality of life (QOL). A study reported that steroid therapy was useful for reducing inflammation after off pump coronary artery bypass.10) Assuming that steroids may be effective for PIS after EVAR, the inhibitory effects of steroids on PIS were investigated. Although preoperative steroid therapy may lead to postoperative infection, Stuck et al. indicated that the risk of infection was high in patients continuously treated with prednisolone at 10 mg or more (every day) or at a cumulative dose of 700 mg or more.11) Many studies reported the dose of methylprednisolone for reducing postoperative inflammation: an initial dose of 10 to 30 mg/kg or 250 to 1000 mg.12–14) Based on this, in our hospital, we adopted a strategy to administer methylprednisolone at 1000 mg, as a maximum dose to obtain anti-inflammatory actions without increasing the incidence of postoperative infection, on anesthesia induction.
The results showed that an increase in the CRP level and fever were significantly inhibited until 3 days after surgery in the steroid-treated group, and that dietary intake was significantly higher in the steroid-treated group 2 days after surgery. Among patients aged 80 years or older, dietary intake was higher in the steroid-treated group between 1 and 5 days after surgery, suggesting that the effects of PIS inhibition are more marked in elderly patients.
Drugs that may inhibit PIS, other than steroids, include statins. A study reported the usefulness of statins for reducing PIS.15) Statins exhibit multifocal effects: anti-inflammatory, arteriosclerotic plaque-stabilizing, and platelet function-inhibiting actions. Another study indicated that statin therapy decreased the incidence of post-EVAR complications such as embolism. However, in the study, a strong statin significantly inhibited an increase in the CRP level, but there were no significant inhibitory effects on postoperative fever. Therefore, even in statin-treated patients, combination therapy with steroids may more markedly inhibit PIS.
In this study, we administered methylprednisolone at 1000 mg on anesthesia induction. However, in the future, the optimal dose of a steroid and timing of administration must be examined.
Conclusion
The administration of a steroid (methylprednisolone at 1000 mg) on anesthesia induction inhibited fever and an increase in the CRP level early after surgery without the risk of infection.
Disclosure Statement
The first author and co-authors have no conflicts of interest.
Footnotes
This is a translation of Jpn J Vasc Surg 2015;24:861–865.
This study was presented at the 55th Annual Meeting of Japanese College of Angiology (2014, Kurashiki).
References
- 1).Blum U, Voshage G, Lammer J, et al. Endoluminal stent-grafts for infrarenal abdominal aortic aneurysms. N Engl J Med 1997; 336: 13-20. [DOI] [PubMed] [Google Scholar]
- 2).Velázquez OC, Carpenter JP, Baum RA, et al. Perigraft air, fever, and leukocytosis after endovascular repair of abdominal aortic aneurysms. Am J Surg 1999; 178: 185-9. [DOI] [PubMed] [Google Scholar]
- 3).Galle C, De Maertelaer V, Motte S, et al. Early inflammatory response after elective abdominal aortic aneurysm repair: a comparison between endovascular procedure and conventional surgery. J Vasc Surg 2000; 32: 234-46. [DOI] [PubMed] [Google Scholar]
- 4).Morikage N, Esato K, Zenpo N, et al. Is endovascular treatment of abdominal aortic aneurysms less invasive regarding the biological responses? Surg Today 2000; 30: 142-6. [DOI] [PubMed] [Google Scholar]
- 5).Aho PS, Niemi T, Piilonen A, et al. Interplay between coagulation and inflammation in open and endovascular abdominal aortic aneurysm repair—impact of intra-aneurysmal thrombus. Scand J Surg 2007; 96: 229-35. [DOI] [PubMed] [Google Scholar]
- 6).Tzilalis B, Papoutsis K, Douliotis I, et al. Latest data on postimplantation syndrome. Hellenic Vascular Surgery 2008; 14: 132-45. (in Greek) [Google Scholar]
- 7).Akowuah E, Wilde P, Angelini G, et al. Systemic inflammatory response after endoluminal stenting of the descending thoracic aorta. Interact Cardiovasc Thorac Surg 2007; 6: 741-3. [DOI] [PubMed] [Google Scholar]
- 8).Rowlands TE, Homer-Vanniasinkam S. Paradoxical neutrophil elastase release in endovascular abdominal aortic aneurysm repair. Vasc Endovascular Surg 2007; 41: 48-54. [DOI] [PubMed] [Google Scholar]
- 9).Storck M, Scharrer-Pamler R, Kapfer X, et al. Does a postimplantation syndrome following endovascular treatment of aortic aneurysms exist? Vasc Surg 2001; 35: 23-9. [DOI] [PubMed] [Google Scholar]
- 10).Suezawa T, Aoki A, Kotani M, et al. Clinical benefits of methylprednisolone in off-pump coronary artery bypass surgery. Gen Thorac Cardiovasc Surg 2013; 61: 455-9. [DOI] [PubMed] [Google Scholar]
- 11).Stuck AE, Minder CE, Frey FJ. Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis 1989; 11: 954-63. [DOI] [PubMed] [Google Scholar]
- 12).Liakopoulos OJ, Schmitto JD, Kazmaier S, et al. Cardiopulmonary and systemic effects of methylprednisolone in patients undergoing cardiac surgery. Ann Thorac Surg 2007; 84: 110-8; discussion 118-9. [DOI] [PubMed] [Google Scholar]
- 13).Mayumi H, Zhang QW, Nakashima A, et al. Synergistic immunosuppression caused by high-dose methylprednisolone and cardiopulmonary bypass. Ann Thorac Surg 1997; 63: 129-37. [DOI] [PubMed] [Google Scholar]
- 14).Schurr UP, Zünd G, Hoerstrup SP, et al. Preoperative administration of steroids: influence on adhesion molecules and cytokines after cardiopulmonary bypass. Ann Thorac Surg 2001; 72: 1316-20. [DOI] [PubMed] [Google Scholar]
- 15).Yamamoto S, Aoki A, Suezawa T, et al. Effect of statin on the inflammatory response and postoperative course after endovascular abdominal aortic aneurysm repair. Jpn J Vasc Surg 2013; 22: 951-4. (in Japanese) [Google Scholar]