Abstract
Purpose: This study aimed at clarifying the changes in treatments for primary varicose veins in Japan.
Methods: A questionnaire was mailed to the members of the Japanese Society of Phlebology. The contents of the survey covered the treatment and treatment strategy of varicose vein cases in 2013. The results were examined and compared with the results of previous surveys conducted by the aforesaid society in 1998, 2004 and 2009.
Results: Of 36078 patients, 43958 limbs were reported from 201 institutions. Saphenous type was the most common type of varicose veins that developed in patients aged 70–79 years. The C4–6 cases according to the Clinical-Etiology-Anatomy-Pathophysiology (CEAP) classification occurred significantly more in males than in females (p <0.01). For the treatments of saphenous type and of segment type (dilatation of peripheral branch), endovenous laser ablation (EVLA) was performed most frequently (51%), while the frequency of stripping and of high ligation decreased. EVLA was performed with tumescent local anesthesia, which required one day of hospitalization.
Conclusion: In our study, the number of patients with varicose veins increased especially in the elderly. Surgical treatments were selected for a number of patients, and EVLA was the most commonly adopted method of treatment in Japan. (This article is a translation of Jpn J Phlebol 2016: 27; 249-57.)
Keywords: varicose veins, survey, endovenous laser ablation, endovenous radiofrequency ablation
Introduction
The Japanese Society of Phlebology conducts surveys of venous diseases in Japan every year, including varicose vein treatment surveys in 1998,1) 20042) and 2009.3) The guidelines for endovenous treatment of lower extremity varicose veins were developed in 2010,4) and endovenous laser ablation (EVLA) was covered by national health insurance in 2011. Therapy for varicose veins has since rapidly changed. Therefore, in the present study we conducted a cross-sectional multi-center survey of patients with varicose veins.
Subjects and Methods
A questionnaire survey on primary lower extremity varicose veins was mailed to active members of the Japanese Society of Phlebology. The questionnaire covered the treatment of new varicose vein cases in 2013 as well as its strategy for treatment. The contents of the questionnaire included: 1) the number of patients, age, symptoms and signs, treatment performed; 2) the strategy (EVLA procedure, stripping, ligation operation and sclerotherapy); and 3) complications. The results were examined and compared with the results of previous surveys conducted by the aforementioned society in 1998, 2004 and 2009. The analyses were performed using the answers given, although some respondents did not answer all the questions. Data were expressed as mean ± 1 standard deviation. The frequencies of symptoms and of signs were compared between male and female patients using x2-test. A p value less than 0.05 was considered statistically significant.
Results
Epidemiologic characteristics and performed treatments
Patient number
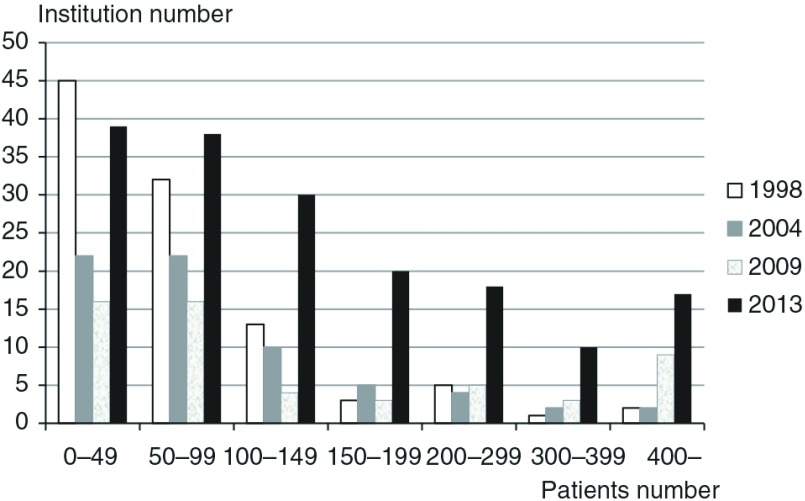
The questionnaire was answered by 201 institutions which reported 43958 limbs from 36078 cases. The male to female ratio of total patients was 1:2.4, and that of patients with bilateral varicose veins was 1:2.1. The number of varicose vein cases ranged between 1 and 4288 (mean 210 ± 402) per institution. The institutions were classified into several groups according to the number of patients treated. The number of institutions that treated 49 cases or fewer was highest, at 39 institutions. (Fig. 1) The number of institutions increased in all groups in comparison with the surveys in 1998, 2004 and 2009.
Fig. 1.
Number of institutions according to the number of treated patients in a year.
Some data were quoted from literature 1–3.
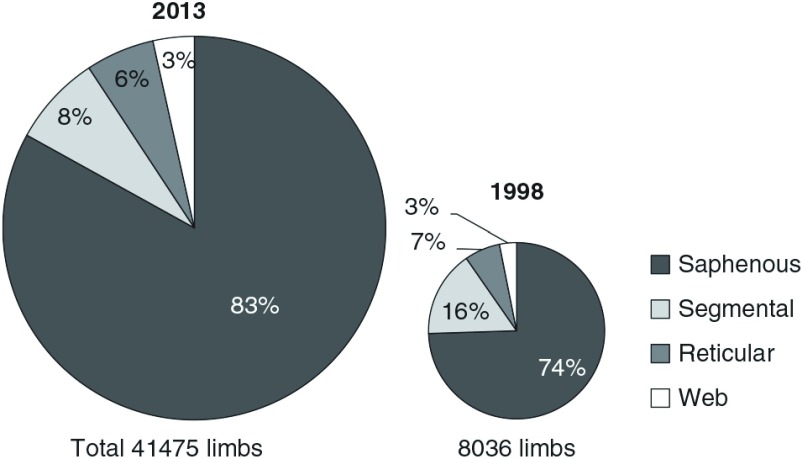
Types of varicose veins
According to the macroscopic findings, varicose veins were classified into saphenous type (dilatation of saphenous vein or of its big branch), segment type (dilatation of peripheral branch), reticular type (small varicose vein 1–3 mm in diameter), and web type (spider web with 0.1–1 mm). The type of varicose veins was determined by a doctor based on the appearance (Fig. 2). There were 34442 limbs with saphenous type varicose veins (83%), 3184 limbs with segment type (8%), 2408 limbs with reticular type (3%) and 1441 limbs with web type (4%). The patients with saphenous type had varices of the great saphenous vein (GSV) (79%), short saphenous vein (15%), and both GSV and short saphenous vein (6%). The sum of patients with saphenous type and those with segment type varicose was 91% of all varicose veins. The distribution of varicose vein types did not much differ from those found the surveys in 1998, 2004 and 2009.
Fig. 2.
Type of varicose veins.
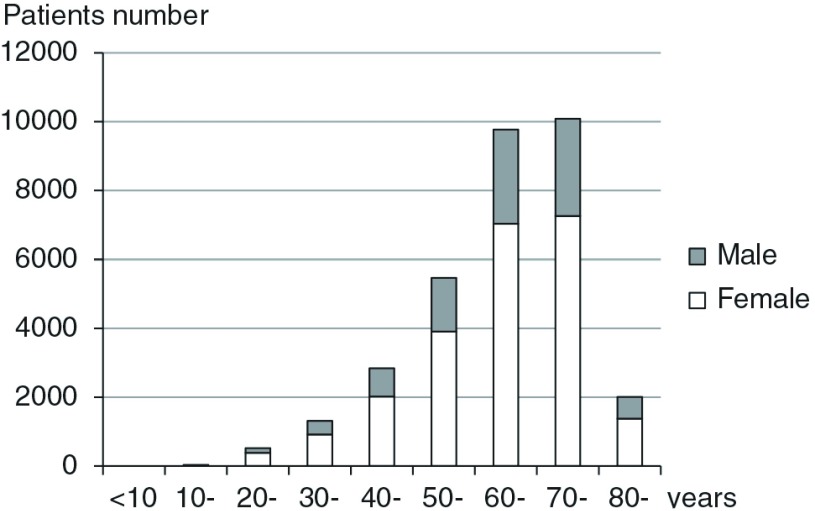
Age distribution of patients
Age distribution of the patients was 33 (10–19 yrs), 521 (20–29), 1326 (30–39), 3196 (40–49), 5471 (50–59), 9772 (60–69), 10087 (70–79), and 2008 (80 and over). The patients in the 70–79 years age group accounted for 31% of all patients, which was highest among all age groups. (Fig. 3) The age group with the highest number of patients was more advanced in age in comparison with the 2009 survey, in which the highest was the 60–69 years age group.
Fig. 3.
Ages of patients with varicose veins.
Symptoms and signs (Table 1)
Answers to questions on symptoms and signs were multiple-choice. The most frequent answers were edema (41.2%), pigmentation (20.7%), eczema (13.6%), and lipodermatosclerosis (8.8%). The CEAP classification (Clinical-Etiology-Anatomy-Pathophysiology) is a consensus that is adopted worldwide, and C4–6 cases with skin changes are classified as severe state chronic venous diseases.5) The signs with a CEAP classification of more than C4 as well as bleeding were significantly more common in males than in females. These differences were also observed in the 1998 and 2004 surveys, but not in the 2009 survey. Each occurrence ratio of thrombophlebitis (6.6%) and pulmonary embolism (0.2%) in the current study was similar to that of the 2009 survey.
Table 1.
Representative symptoms and signs
| Total no. (%) | Male (%) | Female (%) | |
|---|---|---|---|
| Edema | 5783 (41.2) | 1642 (33.9) | 4141 (45.0)* |
| Lipodermatosclerosis | 1232 (8.8) | 481 (9.9) | 751 (8.2)* |
| Pigmentation | 2906 (20.7) | 1360 (28.0) | 1546 (16.8)* |
| Eczema | 1911 (13.6) | 793 (16.3) | 1118 (12.2)* |
| Healed ulcer | 379 (2.7) | 191 (4.0) | 188 (2.0)* |
| Active ulcer | 459 (3.3) | 222 (4.6) | 237 (2.6)* |
| Thrombophlebitis | 930 (6.6) | 314 (6.5) | 616 (6.7) |
| Pulmonary embolism | 23 (0.2) | 7 (0.1) | 16 (0.2) |
| Bleeding | 112 (0.8) | 64 (1.3) | 48 (0.5)* |
There were 14051 patients exhibiting symptoms (male 4850, female 9201) and the number of patients with each symptom is shown.
*: p <0.01
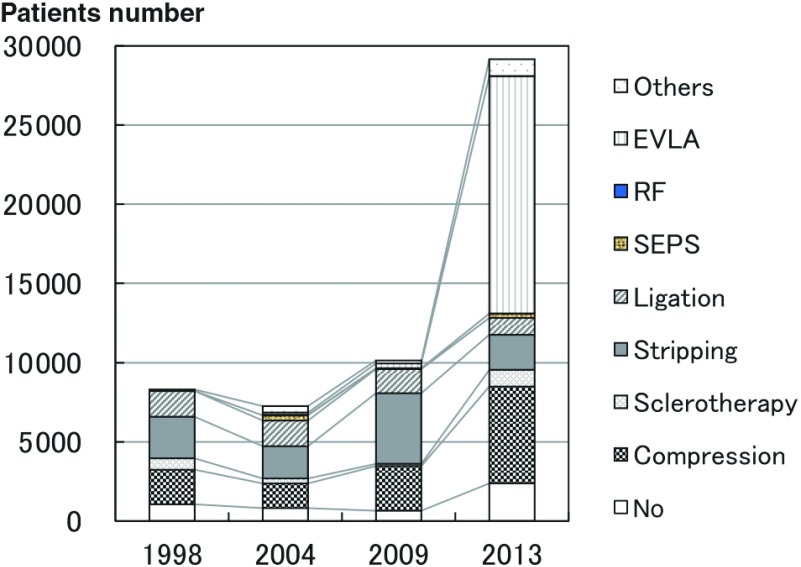
Performed treatment (Table 2, Fig. 4)
Performed treatments for 32764 limbs were recorded. Regarding treatment of saphenous type varicose vein, stripping alone or stripping combined with avulsion or sclerotherapy was performed in 2079 limbs (7.9%), which was a decrease from 47.2% in the 2009 survey. On the other hand, EVLA alone or EVLA combined with other techniques was performed in 14756 limbs (56.2%) for saphenous type.
Table 2.
Performed treatments
| Treatment | Saphenous | Segmental | Reticular | Web |
|---|---|---|---|---|
| No treatment | 1924 (0.7) | 460 (14.9) | 599 (32.1) | 776 (50.3) |
| Compression therapy | 5257 (20.0) | 863 (28.0) | 543 (29.1) | 454 (29.4) |
| Sclerotherapy | 535 (2.0) | 517 (16.8) | 723 (38.8) | 314 (20.3) |
| Stripping | 1103 (4.2) | 34 (1.1) | 0 | 0 |
| Stripping + avulsion | 677 (2.6) | 105 (3.4) | 0 | 0 |
| Stripping + sclerotherapy | 299 (1.1) | 1 (0.0) | 0 | 0 |
| Ligation | 214 (0.8) | 23 (0.7) | 8 (0.4) | 0 |
| Ligation + sclerotherapy | 333 (1.3) | 54 (1.8) | 18 (1.0) | 0 |
| Ligation + avulsion | 589 (2.2) | 43 (1.4) | 0 | 0 |
| EVLA | 3879 (14.8) | 97 (3.1) | 0 | 0 |
| EVLA + avulsion | 8227 (31.3) | 116 (3.8) | 0 | 0 |
| EVLA + sclerothrapy | 2344 (8.9) | 6 (0.2) | 0 | 0 |
| EVLA + others | 306 (1.2) | 0 | 0 | 0 |
| RF | 0 | 0 | 0 | 0 |
| SEPS (+ Stripping) | 256 (1.0) | 19 (0.6) | 0 | 0 |
| IP ligation | 320 (1.2) | 744 (24.1) | 0 | 0 |
| Unknown | 10 (0.0) | |||
| Total | 26273 | 3082 | 1865 | 1544 |
EVLA: endovenous laser ablation; RF: radiofrequency ablation; SEPS: subfascial endoscopic perforating vein surgery; IP: incompetent perforating vein
Fig. 4.
Changes of varicose vein treatments (saphenous and segmental type) EVLA: endovenous laser ablation; RF: radiofrequency ablation; SEPS: subfascial endoscopic surgery
Some data were quoted from literature 1–3.
For the saphenous and segment types, EVLA was carried out in 51.0%, stripping in 7.6%, and ligation operation in 4.3%. The frequency of EVLA remarkably increased from 3.1% in the 2009 survey. No patient was treated using radiofrequency ablation (RF) in the present survey. Those treated using ligation operation had decreased since the 2009 survey. Subfascial endoscopic surgery (SEPS) was performed in only 275 limbs (0.9%).
Treatment strategy and procedures for primary varicose veins
Selection of treatment procedure
Treatment plan
Questions regarding the treatment selection for saphenous type were answered by 201 institutions. EVLA was chosen by 89 institutions (44%), stripping by 42 institutions (21%), and high ligation with sclerotherapy by two institutions (2%). There were 54 institutions (27%) who changed the treatment method depending on the saphenous vein diameter or degree of reflux (by pathophysiology), and 14 institutions (7%) who chose procedures according to the patient’s request. There was a large increase in EVLA treatment and a decrease in stripping or high-ligation surgery in the 2013 survey in comparison to the 2009 survey.
Newly applied procedure
From 2009 to 2014 EVLA was newly adopted in 107 institutions, SEPS in five, stab avulsion in four, RF in two, and sclerotherapy for saphenous reflux in two.
High-ligation procedure
Number of ligations
For high-ligation of the GSV, ligation of the saphenous vein was performed at one site in 58 institutions (41%), at two sites in 38 institutions (27%), and at more than two sites in 39 institutions (27%). The number of institutions that opted for the high-ligation procedure decreased in the 2013 survey in comparison with the 2009 survey.
Ligation of sapheno-femoral junction tributaries
Tributaries of the sapheno-femoral junction (S-F J) were ligatured at 139 institutions (89%) and not tied at 18 institutions (11%). Most doctors did not add other saphenous vein ligation in high-ligation procedures and almost all doctors chose the ligature of the tributaries.
Procedure of stripping surgery
Anesthesia
Questions regarding anesthesia in the stripping operation were multiple-choice. This surgery was performed using tumescent local anesthesia (TLA) at 91 institutions, general anesthesia at 85 institutions, intravenous anesthesia at 47, spinal anesthesia at 45, local anesthesia at 26, femoral nerve block at 16, and epidural anesthesia at five.
Contrivances of stripping surgery
The selective stripping procedure was used at 168 institutions (94%). The invagination stripping method was routinely applied at 122 institutions (70%), sometimes applied at 23 (13%), and was not applied at 30 (17%). The stab avulsion technique for the extirpation of varicose veins was frequently used at 115 institutions (64%), sometimes used at 44 (24%), and not used at 21 (12%). The frequency of application of these techniques increased compared to that in the 2009 survey.
Hospitalization
In the stripping operation, the length of hospitalization ranged from 0 to 10 (2.6 ± 1.8) days. Ambulatory surgery was adopted at 55 institutions (29%), in which 19 institutions (10%) selected stripping depending on the patient's condition. One hundred thirty-two institutions (71%) did not adopt ambulatory surgery. Forty-three institutions (23%) replied that their system for ambulatory surgery was not sufficient, and the doctors of the other 25 institutions (13%) answered that they had no intention of performing such surgery. The number of institutions where outpatient stripping surgery was applied did not significantly increase in comparison with the 2009 survey.
EVLA procedure
Laser wavelength and apparatuses
Several kinds of wavelengths were used for the laser instruments as follows: 980 nm at 124 institutions (ELVeS 980, Biolitec, Jena, Germany); 1470 nm at six (ELVeS 1470, Biolitec); 1320 nm at four (CoolTouchCTEV, Cool Touch, Roseville, USA), 1470 nm at two (Atoven, Diotech, Busan, Korea); 2000 nm at two (Revolix Jr, Lisa Laser, Pleasanton, USA); 1319 nm at one (Pro-V, Sciton, Palo Alto, USA); and 810 nm at one (ADL-20, Asuka Medical, Kyoto, Japan). Laser energy was delivered with an output power of 8–12 (mean 10.0 ± 1.3) W and with the linear endovenous energy density of 50–120 (76.7 ± 10.1) joule/cm in EVLA. Laser was delivered in continuous mode at 115 institutions and in pulse wave mode at seven institutions.
Anesthesia
EVLA was performed under TLA at 126 institutions, under intravenous anesthesia at 61 institutions, general anesthesia at 21, and femoral nerve block at eight. Propofol (Diprivan, AstraZeneca, Osaka, Japan) was most often used for intravenous anesthesia. The anesthetic TLA solutions were mostly arranged by diluted lidocaine at a concentration of 0.1%. Commercially available lidocaine solutions containing epinephrine at 1:100000 were used. In addition, 7% sodium bicarbonate was often mixed to the TLA solution to reduce the pain of injection.
Management of varicose veins and high ligation of saphenous trunk
For varicose veins, sclerotherapy or varicectomy was simultaneously performed with EVLA at 96 institutions (71%), or was performed at some time after EVLA at 11 (8%). The disposition of varicose veins was sometimes performed at 19 institutions (14%) and was not applied at ten (7%). High ligation of S-F J was performed at two institutions (2%), was not used at 124 (95%), was only performed when the diameter was over 10 mm at three (2%), and was selected only when there was an aneurysmal change at one (1%).
Hospitalization
The length of hospital stay for EVLA was 0–5 (1.5 ± 1.3) days. Outpatient surgery was routinely performed at 60 institutions (45%), was sometimes performed at 20 (15%), and was not applied at 24 (18%). Doctors at 23 institutions (17%) replied that their systems for outpatient surgery were not sufficient, and doctors of another five institutions replied that they had no intention of performing such surgery.
Post-operative ultrasound examination
Post-operative ultrasound examination was performed for all cases at 126 institutions (97%), in selective cases at one (1%), and not performed at three (2%). Duplex scanning was carried out on the operative day at four institutions, on the 1st day after operation at 76, on the 2nd–3rd day at 22, in the 1st week at 61, in the 2nd–3rd week at five, in the 1st month at 73, in the 3rd month at 38, in the 6th month at 31, and in the 1st year at 25.
Endovenous heat induced thrombosis
There were 121 answers to the question of Endovenous heat induced thrombosis (EHIT).6) Sixty-six institutions (55%) experienced a patient complicated with EHIT, totaling to 308 recorded patients with EHIT. The treatment for patients with EHIT class 2, which was non-occlusive thrombosis with thrombus extension into the deep vein system measuring less than half the diameter of the deep vein, was warfarin with unfractionated heparin at 15 institutions, observation only at nine, wearing of elastic stockings at two, administration of aspirin at two, or other treatment types at one. For patients with EHIT class 3, in which a thrombus extended to a distance measuring more than 50% of the deep vein diameter, warfarin was selected at 21 institutions, warfarin with unfractionated heparin at 13, unfractionated heparin at two, and other treatment types were selected at four.
Sclerotherapy
Application of foam sclerotherapy
Foam sclerotherapy was commonly used at 73 institutions (46%), sometimes used at 43 (27%), and was not applied at 44 (28%).
Main trunk sclerotherapy
Sclerotherapy for saphenous reflux was commonly applied at four institutions (3%), sometimes used at 23 (15%) and was not applied at 129 (83%). High ligation with sclerotherapy for saphenous vein was applied by 18 institutions (28%), and was not used by 47 (72%). Polidocanol (polidocasklerol, Zeria Pharmaceutical Co, Tokyo, Japan) was used in almost all institutions. The administered concentration levels of polidocanol were 0.5% at six institutions, 1% at 16, 2% at four, and 3% at 13. For foam sclerotherapy, sclerosant and gas were mixed with a 1:1 ratio at two institutions, 2:1 at one, 3:1 at 11, 4:1 at 18, and 5:1 at three. Injection volume was decided by ultrasound observation at 15 institutions, by estimation of vein length and diameter at nine, by venography at two, and by using the constant volume at three. Sclerotherapy was performed in the recumbent position at 20 institutions, with a foot lifted at nine institutions, and in the Fowler position at two institutions.
Sclerotherapy of calf varicose veins with obliteration of saphenous reflux by ligation, stripping or heat ablation
Ninety institutions used polidocanol as the sclerosant for adjunctive sclerotherapy for calf varicose veins after high ligation or stripping. The concentration of polidocanol was 0.5% at 32 institutions, 1% at 57, 1.5% at three, and 2% at three. Sclerotherapy of calf varicose veins was performed prior to surgical procedure on the same day at two institutions (2%). At 107 (98%) institutions, sclerotherapy was performed following surgical procedure; on the same day at 32 (29%) institutions, within 2 weeks at 11, after 3 to 4 weeks at five, after 1 month at 35, after 2 to less than 3 months at 11, after 3 months at eight, after more than 3 to 5 months at three, and after 6 months at two. The number of puncture sites was one at six institutions, between one and five at 89 institutions, and between six and nine at seven institutions. Injection volume of sclerosant was less than 1 cc at 26 institutions, 1–2 cc at 34 institutions, 2–3 cc at 15 institutions, 3–4 cc at six institutions, 4–5 cc at four institutions, and over 5 cc at seven institutions.
Sclerotherapy for reticular or web type varicose veins
Sclerotherapy for reticular or web-type varicosis was applied frequently at 36 institutions (30%), sometimes at 47 institutions (38%), and never at 40 institutions (32%).
Complication of sclerotherapy
Eight institutions experienced complications of foam sclerotherapy; deep vein thrombosis (two institutions), visual disturbance (one), headache (one), edema (one), and the detail was unknown (three).
Discussion
The number of members of the Japanese Society of Phlebology has increased over the years, possibly due to venous disorders. Particularly, varicose veins are attracting more and more attention as coverage of endovenous heat ablation treatment fees is permitted by the Japanese medical service under health insurance. Therefore, 193 institutions responded to our questionnaire survey, providing information on a total number of 36078 recorded patients with primary varicose veins, which is significantly more than that of the surveys conducted in 1998, 2004 or 2009. All types of institutions, including outpatient-clinics, small hospitals and special institutions, provide treatment for varicose veins patients and grew in number. The number of institutions who treated more than 400 patients in one year remarkably increased.
The most common types of varicose veins were saphenous and segmental types, which occupied 91% of cases. The frequency of saphenous type and segmental type was similar to that in the 1998, 2004, and 2009 surveys. According to those previous surveys, the largest age group of varicose vein patients was 50–59 in 1988, 50–59 and 60–69 in 2004, 60–69 in 2009. In the present study, the majority shifted to the 70–79 group, and the ratio of elder patients increased. Minimally invasive treatment is desired especially for elderly patients. We recommend endovenous treatment such as EVLA, which is less invasive compared to conventional surgery, for elderly patients without gait disturbance.7)
Edema was the most frequent symptom, which was observed in 50% of all patients in 2009 and 41% in 2013. This showed that many patients with mild varicose veins visited clinics for treatment. On the other hand, patients with skin changes are classified as having severe chronic venous diseases, which have been observed as being more frequent in male patients in the 1998 and 2004 studies, but not the 2009 study.1–3) However, it has been reported that C2 with varicose veins and C3 with edema were more frequent in female patients in Germany,8) and another report emphasized that male patients were not at risk of severe symptoms including skin ulcer or pulmonary thromboembolism (PTE).9) Epidemiologic studies reported that the rates of 0.6%–8.6% of all varicose patients in France, Poland or Italy8,10,11) were diagnosed as having C5 (a healed ulcer), and 0.1%–0.5% of all patients in France or Italy8,10) had C6 (an active ulcer). PTE developed in 0.2% of all patients in the present study, which was consistent with the occurrence ratio observed in the 2009 survey. The guidelines by the Japanese Circulation Society claim that varicose veins are a risk factor of PTE.12) The rate of PTE from varicose veins is not significantly high; however, this should always be taken into consideration during varicose vein treatment.13)
Patients treated by RF were not recorded in this study because RF was admitted by the Japanese medical service under health insurance in 2014. The frequency of high ligation decreased to 4% of all varicose veins surgeries, and the frequency of the stripping dropped to 8% from 47% recorded in the 2009 survey. The annual number of vascular surgeries is reported via the case record system of the Japanese Society for Vascular Surgery. (JSVS, http://www.jsvs.org/ja/enquete/) This report showed that 11103 varicose vein surgeries were performed in 2010, including 2638 (24%) high ligation surgeries (± sclerotherapy), 7766 (70%) stripping surgeries, and 699 (6%) surgeries with other methods. This JSVS record system was integrated into the National Clinical Database (NCD), which is a case record system of the Japan Surgical Society (JSS), and the data revealed that 30088 varicose vein surgeries were performed in 2012. These surgeries included 4651 (15%) high ligation surgeries, 16163 (54%) stripping surgeries, 8186 (27%) EVLA, six (0%) valvuloplasties, and 1082 (4%) surgeries using other methods. The increase in EVLA treatment has begun since 2012. Any doctor who registers patients’ data on the NCD must be a member of the JSS; however, non-JSS member doctors can perform varicose veins surgery. Therefore, the NCD does not cover all cases in Japan. The increase of EVLA use was recognized in the NCD data and in the current study.
Regarding treatment strategy, the first choice treatment was EVLA (44%) in our study, whereas selection of high ligation surgery or stripping surgery had decreased since 2009. A rise in the number of ligation sites in high-ligation surgery was observed in the 2009 survey; however, the present survey revealed that only one site of ligation in high-ligation surgery at S-F J was most commonly (41%) used.
The TLA method, which is less invasive for patients in comparison to general anesthesia or spinal anesthesia, was most often applied in the present survey. The TLA method allows not only quick recovery from anesthetic effects but also early ambulation. However, only 29% of institutions chose to perform ambulatory surgery in stripping operation in the present survey. Doctors in this study used invagination stripping (83%), the selective stripping method (94%) and the stab avulsion technique (88%).
As for endovenous heat ablation, RF was recognized by the Japanese medical service to be covered under health insurance in 2014. Therefore, RF treatment is expected to increase in the future.14) EVLA apparatuses have been improved, and a new type apparatus with 1470 nm wavelength and radial two ring fiber (irradiation in a radial direction) is less invasive. Therefore, use of this apparatus should also increase.15) For anesthesia of EVLA, TLA is most frequently used (63%). High ligation was not performed for most cases of EVLA. Furthermore, EVLA was performed during 1.5 days of hospitalization on average, and 60% of institutions preferred to perform EVLA as outpatient surgery. We suspect that the use of EVLA for outpatient surgery will also increase in the future.
Most complications caused by EVLA, such as bruising and pain, are mild. However, severe adverse events such as venous thromboembolism have been reported, albeit rarely,16) and should be taken into consideration when EVLA is applied. EHIT, in which a thrombus extends into the deep veins, is an expected complication and should be also carefully considered.6) There are reports of EHIT having an incidence rate of 0.8%–16%.6,17) In the current study, 55% of doctors experienced EHIT and follow-up evaluation by postoperative ultrasound was performed by 97% of doctors.
Concerning foam sclerotherapy, its usefulness was recognized widely in Japan, and in 2006, the European guidelines were translated into Japanese.18) In the present study, 73% of institutions apply foam sclerotherapy; however, it is applied to saphenous trunk reflux only by 18% of doctors, and mostly used for the sclerotherapy of calf varicose veins.
A meta-analysis reported that the outcome and recurrence rate after EVLA was equivalent to those of conventional surgery or sclerotherapy.19) EVLA and RF are very useful as they have fewer complications, less pain and allow quicker return to normal activities.20) Therefore, EVLA of the GSV is recommended as safe and effective treatment of saphenous incompetence.21)
A few survey studies of varicose veins have been carried out in other countries. Winterborn et al.22) performed a questionnaire study of the members of the Vascular Society of Great Britain and Ireland, and reported treatments covered by the National Health Service in 2008. According to their report, the vast majority of doctors (336, 96%) offered conventional surgery, 66 surgeons (19%) offered EVLA and only 12 surgeons (3%) offered RF. As far as the National Health Service was concerned, payment for varicose vein treatment was defined, and therefore use of endovenous treatments might be influenced. Van der Velden et al.23) reported a worldwide survey, which demonstrated how to treat varicose vein patients with CEAP classification C2sEpAs2, 5Pr. Two hundred and eleven physiciansTwo hundred and eleven physicians from 36 countries responded to the survey, which showed that endovenous thermal ablation was chosen by 40%–55%. Although there are differences in medical equipment or medical insurance policy by country, the endovenous thermal ablation has become very popular worldwide.24)
Conclusion
Our questionnaire survey of treatments for primary varicose veins in Japan revealed that the number of patients with varicose veins has increased, especially in elderly patients. The surgical treatment of choice by many is EVLA, which has become the leading procedure ahead of conventional surgeries for varicose vein treatment in Japan.
Acknowledgments
We would like to thank all physicians who participated in this survey.
Disclosure Statement
None of the authors have a conflict of interest regarding the work in the study.
Author Contributions
Study conception: all authors
Data collection: HS
Analysis: HS
Investigation: HS, TY
Writing: HS
Funding acquisition: TI
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
Footnotes
This article is a translation of Jpn J Phlebol 2016: 27; 249-57.
The Committee for Survey of the Japanese Society of Phlebology
References
- 1).Hirai M, Ogi S, Ohta T, et al. The Japanese Vein Study: The 1st Survey of Varicose veins. Jpn J Phlebol 1998; 9: 347-57. (in Japanese) [Google Scholar]
- 2).Hirai M, Ohta T, Koyano K, et al. The Japanese Vein Study: The 2nd Survey of Varicose Veins. Jpn J Phlebol 2004; 15: 339-46. (in Japanese) [Google Scholar]
- 3).Iwata H, Satokawa H, Sakata M, et al. The Japanese Veins Study: The 12th Survey of Varicose veins. Jpn J Phlebol 2013; 24: 432-9. (in Japanese) [Google Scholar]
- 4).Satokawa H, Sugiyama S, Hirokawa M, et al. Guidelines for the endovenous treatment of varicose veins. JSP Working Group. Jpn J Phlebol 2010; 21: 289-309. (in Japanese) [Google Scholar]
- 5).EklÖf B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg 2004; 40: 1248-52. [DOI] [PubMed] [Google Scholar]
- 6).Kabnick L, Berland T. Endothermal heat induced thrombosis after endovenous ablation of the great saphenous vein: clinical relevance? In: Wittens C. eds. Best practice in venous procedures. Tulin, Edizioni Minerva Medica, 2010; pp 111-6. [Google Scholar]
- 7).Proebstle TM, Paepcke U, Weisel G, et al. High ligation and stripping of the long saphenous vein using the tumescent technique for local anesthesia. Dermatol Surg 1998; 24: 149-53. [DOI] [PubMed] [Google Scholar]
- 8).Rabe E, Pannier-Fischer F, Bromen K, et al. Bonner Venenstudie der Deutschen Gesellschaft fÜr Phlebologie – Epidemiologische Untersuchung zur Frage der Häufigkeit und Ausprägung von chronischen Venenkrankheiten in der städtischen und ländlichen WohnbevÖlkerung. Phlebologie 2003; 32: 1-14. [Google Scholar]
- 9).Carpentier PH, Maricq HR, Biro C, et al. Prevalence, risk factors, and clinical patterns of chronic venous disorders of lower limbs: a population-based study in France. J Vasc Surg 2004; 40: 650-9. [DOI] [PubMed] [Google Scholar]
- 10).Jawien A, Grzela T, Ochwat A. Prevalence of chronic venous insufficiency in men and women in Poland: multicentre cross-sectional study in 40095 patients. Phlebology 2003; 18: 110-22. [Google Scholar]
- 11).Chiesa R, Marone EM, Limoni C, et al. Chronic venous insufficiency in Italy: the 24-cities cohort study. Eur J Vasc Endovasc Surg 2005; 30: 422-9. [DOI] [PubMed] [Google Scholar]
- 12).JCS Joint Working Group Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (JCS 2009). Circ J 2011; 75: 1258-81. [DOI] [PubMed] [Google Scholar]
- 13).Nakamura M, Sakuma M, Yamada N, et al. Risk factors of acute pulmonary thromboembolism in Japanese patients hospitalized for medical illness: results of a multicenter registry in the Japanese society of pulmonary embolism research. J Thromb Thrombolysis 2006; 21: 131-5. [DOI] [PubMed] [Google Scholar]
- 14).Sugiyama S. Radiofrequency ablation for treatment of varicose veins: Basic technique. Jpn J Phlebol 2014; 25: 421-9. (in Japanese) [Google Scholar]
- 15).Hirokawa M, Ogawa T, Sugawara H, et al. Comparison of 1470 nm laser and radial 2ring fiber with 980 nm laser and bare-tip fiber in endovenous laser ablation of saphenous varicose veins: a multicenter, prospective, randomized, non-blind study. Jpn J Vasc Surg 2014; 23: 964-71. (in Japanese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Merchant R, Jr, Kistner RL, Kabnick LS. Is there an increased risk for DVT with the VNUS closure procedure? J Vasc Surg 2003; 38: 628. [DOI] [PubMed] [Google Scholar]
- 17).Kane K, Fisher T, Bennett M, et al. The incidence and outcome of endothermal heat-induced thrombosis after endovenous laser ablation. Ann Vasc Surg 2014; 28: 1744-50. [DOI] [PubMed] [Google Scholar]
- 18).Iwai T, Hirai M.The Guide of Foam Sclerotherapy: translated issue of 2nd European Consensus Meeting on Foam Sclerotherapy 2006 by Japanese Society of Phlebology; (in Japanese) [Google Scholar]
- 19).Murad MH, Coto-Yglesias F, Zumaeta-Garcia M, et al. A systematic review and meta-analysis of the treatments of varicose veins. J Vasc Surg 2011; 53: 49S-65S. [DOI] [PubMed] [Google Scholar]
- 20).Siribumrungwong B, Noorit P, Wilasrusmee C, et al. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur J Vasc Endovasc Surg 2012; 44: 214-23. [DOI] [PubMed] [Google Scholar]
- 21).Gloviczki P, Comerota AJ, Dalsing MC, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg 2011; 53: 2S-48S. [DOI] [PubMed] [Google Scholar]
- 22).Winterborn RJ, Corbett CR. Treatment of varicose veins: the present and the future—a questionnaire survey. Ann R Coll Surg Engl 2008; 90: 561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23).van der Velden SK, Pichot O, van den Bos RR, et al. Management strategies for patients with varicose veins (C2-C6): results of a worldwide survey. Eur J Vasc Endovasc Surg 2015; 49: 213-20. [DOI] [PubMed] [Google Scholar]
- 24).Enzler MA, van den Bos RR. A new gold standard for varicose vein treatment? Eur J Vasc Endovasc Surg 2010; 39: 97-8. [DOI] [PubMed] [Google Scholar]