Abstract
A urinary tract infection (UTI) is a collective term for infections that involve any part of the urinary tract. It is one of the most common infections in local primary care. The incidence of UTIs in adult males aged under 50 years is low, with adult women being 30 times more likely than men to develop a UTI. Appropriate classification of UTI into simple or complicated forms guides its management and the ORENUC classification can be used. Diagnosis of a UTI is based on a focused history, with appropriate investigations depending on individual risk factors. Simple uncomplicated cystitis responds very well to oral antibiotics, but complicated UTIs may require early imaging, and referral to the emergency department or hospitalisation to prevent urosepsis may be warranted. Escherichia coli remains the predominant uropathogen in acute community-acquired uncomplicated UTIs and amoxicillin-clavulanate is useful as a first-line antibiotic. Family physicians are capable of managing most UTIs if guided by appropriate history, investigations and appropriate antibiotics to achieve good outcomes and minimise antibiotic resistance.
Keywords: cystitis, primary care, urinary tract infections
Yvonne, a successful 26-year-old executive, went to your clinic for dysuria, urinary frequency and urinary urgency of two days’ duration. She had just returned from her honeymoon in Spain. She had no chronic diseases or prior surgical history and was not recently on antibiotics. This was the first time she experienced such symptoms. You performed urine dipstick analysis for her and confirmed the diagnosis of simple cystitis.
WHAT IS URINARY TRACT INFECTION?
Urinary tract infection (UTI) is a collective term that describes any infection involving any part of the urinary tract, namely the kidneys, ureters, bladder and urethra. The urinary tract can be divided into the upper (kidneys and ureters) and lower tract (bladder and urethra).
HOW RELEVANT IS THIS TO MY PRACTICE?
Uncomplicated lower UTI remains one of the most commonly treated infections in primary care. The urinary tract is a common source of infection in children and infants and is the most common bacterial infection in children < 2 years of age, both in the community and hospital setting.(1) During the first six months of life, UTIs are more common in boys.(2) The outcome is usually benign, but UTIs can progress to renal scarring in early infancy, especially when associated with congenital anomalies of the urinary tract. Renal scarring may lead to complications in adulthood including hypertension, proteinuria, renal damage and even chronic renal failure, which requires dialysis treatment.(3)
In general, 40% of women develop a UTI at some point in their life. In Singapore, 4% of young adult women are affected and the incidence increases to 7% at 50 years of age.(2) Adult women are 30 times more likely than men to develop a UTI, with almost half of them experiencing at least one episode of UTI during their lifetime.(4) It is reported that one in three women have their first episode of UTI by the age of 24 years.(4) UTIs are most commonly seen in sexually active young women. Other susceptible adults include the elderly and patients requiring urethral catheterisation.
According to statistics from Singapore’s Ministry of Health, a total of 4,144 patients were admitted to private and government hospitals in Singapore from 1 January 2015 to 31 December 2015 for UTIs, with an average hospital stay of 2–4.8 days.(5) Our article aimed to focus on UTI management in adults.
Uncomplicated versus complicated UTI
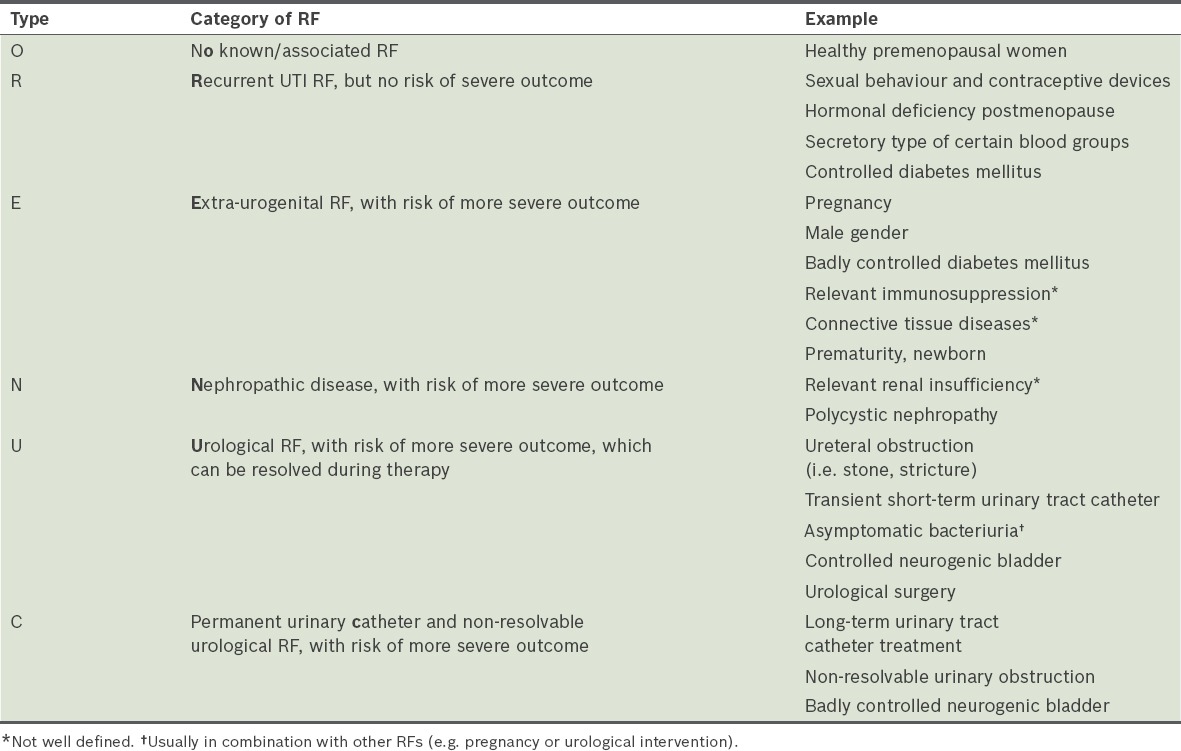
A complicated UTI is an infection associated with a condition, such as a structural or functional abnormality of the genitourinary tract, or the presence of an underlying disease; this increases the risk of the outcome of a UTI being more serious than expected, as compared to its occurrence in individuals without any identified risk factors (i.e. uncomplicated UTI).(4) The European Association of Urology’s classification system for UTIs, known as ORENUC, is based on the clinical presentation of the UTI and its associated host risk factors (Table I). In adults, uncomplicated UTIs fall under categories O, R and partially E, while complicated UTIs are mainly in categories N, U and C.(4)
Table I.
ORENUC classification based on clinical presentation of urinary tract infection (UTI) and risk factors (RFs).
Recurrent UTI
Recurrent UTIs are symptomatic UTIs that follow the resolution of an earlier episode, usually after appropriate treatment. They are common among young, healthy women even though these women generally have anatomically and physiologically normal urinary tracts. Common risk factors are given in Box 1.
Recurrent UTIs can be diagnosed clinically without performing a urine culture, although urine cultures are essential in management. For women with recurrent UTIs, imaging of the upper urinary tract and cystoscopy are not routinely recommended for evaluation. However, they should be performed without delay in patients with atypical symptoms, such as obstructive symptoms or presence of haematuria after resolution of infection.(6)
Asymptomatic bacteriuria
Asymptomatic bacteriuria (ABU) does not cause renal disease or damage. Several studies involving women and the paediatric population have demonstrated that treatment for ABU increases the risk of subsequent symptomatic UTIs; hence, it is not recommended except in diagnostic and therapeutic procedures involving entry to the urinary tract with a risk of mucosal damage, such as endoscopic urological surgery and transurethral resection of the prostate.(7) Although screening and treatment of ABU in pregnant women are recommended in many guidelines to reduce the frequency of low-birth-weight infants and preterm delivery based on studies done in the 1990s,(7) recent studies have shown mixed results in improvement of outcomes following ABU treatment in pregnant women.
WHAT CAN I DO IN MY PRACTICE?
Diagnosis
The diagnosis of acute uncomplicated cystitis can be made with high probability based on a focused history of lower urinary tract symptoms (dysuria, frequency and urgency) in a patient who has no risk factors for complicated UTI. Urine dipstick analysis, as opposed to urinary microscopy, is a reasonable alternative to urine culture to diagnose acute uncomplicated cystitis. Urine cultures are recommended for patients with risk factors for complicated UTIs and in the following situations:(4) (a) suspected acute pyelonephritis; (b) symptoms that do not resolve or recur within 2–4 weeks after completion of treatment; (c) women who present with atypical symptoms; (d) pregnant women; and (e) male patients with suspected UTI.
Box 1. Known and possible age-related risk factors for recurrent urinary tract infection (UTI) in women:(3).
Young and premenopausal women
Sexual intercourse
Use of spermicide
A new sexual partner
A mother with a history of UTI
History of UTI during childhood
Postmenopausal and elderly women
History of UTI before menopause
Urinary incontinence
Atrophic vaginitis due to oestrogen deficiency
Cystocoele
Increased post-void urine volume
Blood group antigen urine secretory status
Urine catheterisation and functional status deterioration in elderly institutionalised women
A practical point to note is the possibility of urogenital tuberculosis (TB) and malignancy presenting with persistent, non-resolving UTI symptoms. Patients with urogenital TB may have received multiple courses of ciprofloxacin, making the isolation of Mycobacterium tuberculosis very difficult, and delaying diagnosis and appropriate therapy. It is also important to consider prostate infections and sexually transmitted infections in all male patients with UTI. However, a detailed description of such infections is beyond the scope of this article.
Management
The choice of management option for UTIs depends on whether it is simple (i.e. uncomplicated) or complicated. Simple uncomplicated cystitis (lower UTI) responds very well to oral antibiotics; studies show that clinical outcomes for UTIs treated with antibiotics are better when compared to those treated with a placebo.(4) In the management of pyelonephritis, clinicians need to correctly differentiate between acute uncomplicated forms and complicated, often obstructive, forms of UTI that require early appropriate imaging. Early appropriate treatment can prevent urosepsis. Referral to the emergency department should be considered if patients are clinically septic or there are limitations to early imaging access.
Patients with a history of previous urological procedures; recent or long-term catherisation; recent or long-term antibiotics; and recent hospitalisation tend to present with complicated UTIs. Regardless of whether the UTI is community- or hospital-acquired, the urine cultures of these patients tend to show a diversity of micro-organisms with a higher prevalence of resistance to antimicrobials. Escherichia coli (E. coli), and the Proteus, Klebsiella, Pseudomonas, Serratia and Enterococci genus are the usual strains found. The treatment strategy for complicated UTIs depends on the severity of the illness and hospitalisation is often necessary.(3)
The Ministry of Health, Singapore, published clinical practice guidelines (CPG) on the use of antibiotics in adults in 2006. It is the latest locally published guideline on the treatment of UTI in adults. The CPG recommended a three-day course of trimethoprim and sulfamethoxazole as first-line therapy for uncomplicated UTI based on the pattern of uropathogen resistance at that time; however, with the increased resistance among uropathogens and changes in the prevalence of UTI-causing organisms, new guidelines have emerged. The following recommendations are adapted from the guidelines on urological infections published by the European Association of Urology in 2015, taking into account drugs that are available locally in the outpatient setting.
Uncomplicated UTIs
E. coli is the predominant uropathogen isolated in acute, community-acquired uncomplicated UTIs in adults and children.(8) Other uropathogens include Staphylococcus saprophyticus, and the Enterococcus, Klebsiella, Enterobacter and Proteus genus.
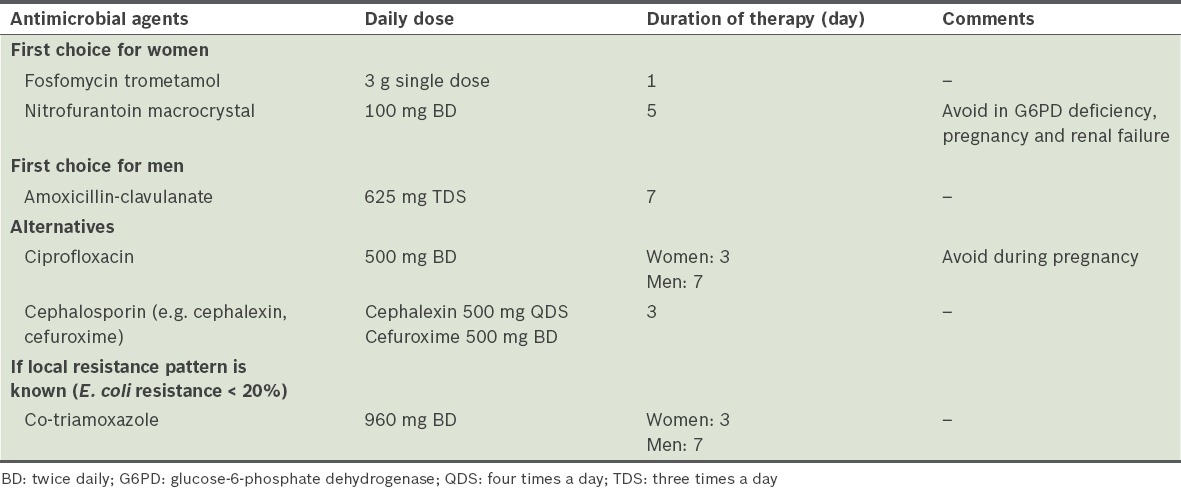
Table II shows the recommended antimicrobial agents for the treatment of acute uncomplicated cystitis in otherwise healthy adults.(3) Some of these antibiotics, such as fosfomycin and nitrofurantoin, are promptly excreted in urine and very low levels are found in tissues, making them excellent choices for cystitis but unsuitable for pyelonephritis.
Table II.
Recommended antimicrobial therapy for acute uncomplicated cystitis in otherwise healthy adults.(3)
A local study, conducted at SingHealth Polyclinics – Bedok, Singapore, in 2011 on community-acquired UTIs, found significant resistance among the Enterobacteriaceae family to commonly available antibiotics in primary care, particularly ampicillin, co-trimoxazole, cephalothin and ciprofloxacin. Both E. coli and Klebsiella were found to have a resistance rate of > 20% to these four common oral antibiotics; for this reason, the authors of the study recommended amoxicillin-clavulanate as the first-choice empirical antimicrobial agent.(9) However, the study had some limitations that may have affected the true resistance patterns in community-acquired UTIs. Notably, it included all patients who visited the polyclinic with a diagnosis code for UTI but did not correlate this with the actual symptoms of these patients. Since patients who were recently discharged from hospitals could have been included in the study as well, nosocomial and community-acquired UTIs were also not accurately differentiated.
For mild and moderate acute uncomplicated pyelonephritis, the recommended initial empirical oral antimicrobial therapy is ciprofloxacin 500 mg twice daily for seven days and co-trimoxazole 960 mg twice daily for 10–14 days.(3) Although local outcome data has not been published, it is likely that in an era of rising rates of ciprofloxacin resistance to E. coli,(9) failure rates of outpatient therapy for pyelonephritis may be as high as 20%. Physicians should follow up on such patients closely.
Complicated UTIs
The choice of a treatment strategy for complicated UTIs depends on the severity of the illness and encompasses three goals: management of the urological abnormality, antimicrobial therapy and supportive care when needed. Hospitalisation is often required and therapy should be guided by urine cultures whenever possible to avoid the emergence of resistant strains. Patients can also be treated as outpatients by confident family physicians; treatment for 7–14 days is generally recommended, but the duration should be closely related to the treatment of the underlying abnormality.
Principles for treating recurrent complicated UTIs include early use of broad-spectrum antibiotics, with adjustment of antibiotic coverage based on culture results, and attempts to relieve any existing urinary obstruction based on results of imaging studies.(8) Recommended oral antibiotic options include fluoroquinolones, amoxicillin-clavulanate and aminoglycosides. Failed empirical treatment warrants hospitalisation, as intravenous antibiotics are usually indicated. Aminopenicillins (i.e. amoxicillin and ampicillin), co-trimoxazole and fosfomycin are not recommended as an empirical treatment.
WHEN SHOULD I REFER TO A SPECIALIST?
Referral to a specialist is recommended for these cases:
All lower urinary tract symptoms in men, especially if they have the following characteristics:(10) (a) bothersome lower urinary tract symptoms that have not responded to conservative management or drug treatment; (b) lower urinary tract symptoms complicated by recurrent or persistent UTIs, retention, or renal impairment that is suspected to be caused by lower urinary tract dysfunction; and (c) suspected urological cancer.
UTIs in the paediatric age group with the following characteristics:(11) (a) infants aged under three months with a possible UTI; and (b) infants and children aged three months or older with acute pyelonephritis/upper UTI.
UTIs with the following characteristics:(3) (a) severe symptoms; (b) failed medical therapy (documented); (c) evidence of retention (acute or chronic); and (d) abnormalities detected on ultrasonography or cytology, such as calculi or bladder tumour.
Recurrent UTIs (defined as ≥ 3 UTIs in 12 months) with the following characteristics:(6) (a) risk factors for complicated UTI are present; (b) a surgically correctable cause is suspected; and (c) a diagnosis of UTI is uncertain for recurrent lower urinary tract symptoms.
You prescribed a course of antibiotics and advised Yvonne to return if her symptoms did not improve after three days. Yvonne brought her mother to see you two weeks later for a cough and mentioned that your treatment for her cystitis had worked very well.
TAKE HOME MESSAGES
ABU does not require antibiotic therapy.
UTIs are one of the most common bacterial infections encountered by primary physicians and most uncomplicated UTIs can be treated in the outpatient setting with appropriate antibiotics.
Differentiating UTIs into simple (uncomplicated) and complicated using the European Association of Urology’s ORENUC classification aids in appropriate clinical management for better patient outcomes.
Simple lower-tract UTIs can be treated with appropriate oral antibiotics with no need for urine culture.
Outpatient treatment for acute pyelonephritis may be associated with a significant failure rate. Such patients should have a urine culture performed and require close follow-up.
A complicated UTI is an infection associated with a condition, such as a structural/functional abnormality of the genitourinary tract or the presence of an underlying disease, which increases the risk of the UTI having an outcome that is more serious than expected when compared to individuals without an identified risk factor; such patients would benefit from a urological review and close follow-up.
All males with a UTI and all infants aged under three months with a possible UTI should be reviewed by a urologist.
REFERENCES
- 1.Hanna-Wakim RH, Ghanem ST, El Helou MW, et al. Epidemiology and characteristics of urinary tract infections in children and adolescents. Front Cell Infect Microbiol. 2015;5:45. doi: 10.3389/fcimb.2015.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Health Promotion Board Singapore. Urinary tract infection. [Accessed February 1 2016]. Available at: http://www.healthhub.sg/a-z/diseases-and-conditions/210/urinarytractinfection .
- 3.Grabe M, Bjerklund-Johansen TE, Botto H, et al. European Association of Urology. Guidelines on urological infections 2015. [Accessed February 1 2016]. Available at: http://uroweb.org/wp-content/uploads/19-Urological-infections_LR2.pdf .
- 4.Foxman B. Epidemiology of urinary tract infections:incidence, morbidity, and economic costs. Am J Med. 2002;113(Suppl 1A):5S–13S. doi: 10.1016/s0002-9343(02)01054-9. [DOI] [PubMed] [Google Scholar]
- 5.Ministry of Health Singapore. Costs and financing: kidney&urinary tract infections. [Accessed February 1 2016]. Available at: https://www.moh.gov.sg/content/moh_web/home/costs_and_financing/hospital-charges/Total-Hospital-Bills-By-condition-procedure/kidney_urinary_tractinfections.html .
- 6.Dason S, Dason JT, Kapoor A. Guidelines for the diagnosis and management of recurrent urinary tract infection in women. Can Urol Assoc J. 2011;5:316–22. doi: 10.5489/cuaj.11214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America;American Society of Nephrology;American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643–54. doi: 10.1086/427507. [DOI] [PubMed] [Google Scholar]
- 8.Kodner CM, Thomas Gupton EK. Recurrent urinary tract infections in women:diagnosis and management. Am Fam Physician. 2010;82:638–43. [PubMed] [Google Scholar]
- 9.Bahadin J, Teo SS, Mathew S. Aetiology of community-acquired urinary tract infection and antimicrobial susceptibility patterns of uropathogens isolated. Singapore Med J. 2011;52:415–20. [PubMed] [Google Scholar]
- 10.National Institute for Health and Care Excellence. Lower urinary tract symptoms in men: management. NICE guidelines [CG97] [Accessed February 1 2016]. Available at: https://www.nice.org.uk/guidance/CG97 . [PubMed]
- 11.National Institute for Health and Care Excellence. Urinary tract infection in under 16s: diagnosis and management. NICE guidelines [CG54] [Accessed February 1 2016]. Available at https://www.nice.org.uk/guidance/cg54 .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


