Abstract
Background
The frequency of lethal overdose due to prescription and non-prescription drugs is increasing in North America. The aim of this study was to estimate overall and regional variation in incidence and outcomes of out-of-hospital cardiac arrest due to overdose across North America.
Methods
We conducted a retrospective cohort study using case data for the period 2006–2010 from the Resuscitation Outcomes Consortium, a clinical research network with 10 regional clinical centers in United States and Canada. Cases of out-of-hospital cardiac arrest due to drug overdose were identified through review of data derived from prehospital clinical records. We calculated incidence of out-of-hospital cardiac arrest due to overdose per 100,000 person-years and proportion of the same among all out-of-hospital cardiac arrests. We analyzed the association between overdose cardiac arrest etiology and resuscitation outcomes.
Results
Included were 56,272 cases, of which 1351 were due to overdose. Regional incidence of out-of-hospital cardiac arrest due to overdose varied between 0.5 and 2.7 per 100,000 person years (p < 0.001), and proportion of the same among all treated out-of-hospital cardiac arrests ranged from 0.8% to 4.0%. Overdose cases were younger, less likely to be witnessed, and less likely to present with a shockable rhythm. Compared to non-overdose, overdose was directly associated with return of spontaneous circulation (OR: 1.55; 95% CI: 1.35–1.78) and survival (OR: 2.14; 95% CI: 1.72–2.65).
Conclusions
Overdose made up 2.4% of all out-of-hospital cardiac arrest, although incidence varied up to 5-fold across regions. Overdose cases were more likely to survive than non-overdose cases.
Keywords: Drug overdose, Epidemiology, Non-cardiac etiology
Introduction
Out-of-hospital cardiac arrest (OHCA) is the common endpoint of many pathological processes. In the resuscitation literature, the etiology of OHCA is often dichotomized into OHCA of presumed cardiac origin and those of non-cardiac origin. This dichotomy largely corresponds to major differences in treatment strategies, with many focusing on the reversal of conditions that prevent an otherwise sound heart from functioning. One such condition is OHCA resulting from drug overdose (OD-OHCA).
Drug overdose is currently a major public health problem in the United States and Canada. According to the most recent statistics, in the United States the cause specific mortality rate for drug overdose in 2013 was approximately 9.5 per 100,000.1 This estimate accounts for intentional and unintentional events, as well as legal and illegally obtained drugs. OD in the prehospital environment may frequently present to EMS as OD-OHCA, although the epidemiology of OD-OHCA – as opposed to drug-related mortality – is limited. Previous studies have described incidence and characteristics of OD-OHCA and its subsequent resuscitation.2–7 A broad geographic analysis of OD-OHCA has not been conducted. Additionally, as OD continues to grow as a public health problem, the treatment of OD-OHCA may become more frequent and evidence-based treatment guidelines will be essential. Current advanced cardiac life support (ACLS) guidelines from the American Heart Association do not differ appreciably between the resuscitation of OD-OHCA and non-OD-OHCA.8 However, previous studies suggest that real world ACLS care is different for OD-OHCA.7,9
We investigated regional variation in incidence, outcomes and characteristics of OD-OHCA in a large population-based cohort of OHCA across North America representing a population of 19.5 million. We further sought to determine whether previous observed differences in treatment of OD-OHCA reflect general phenomena throughout the US and Canada.
Methods
This study was conducted with de-identified data obtained from the Resuscitation Outcomes Consortium (ROC) through the cooperation of the University of Washington Clinical Trials Center (ROC Data Coordinating Center (DCC)). The structure, surveillance methodology, and participants of the ROC have been reported elsewhere.10 In brief, the ROC is a clinical research consortium with 10 sites in the United States and Canada. The ROC conducts population-level regional OHCA surveillance, as well as clinical trials for the prehospital treatment of OHCA and major trauma. All non-traumatic cases of OHCA treated by emergency medical services (EMS) in 10 sites of the ROC in the time period spanning 2006–2010 were included in this analysis. Sites included Birmingham, Alabama; Dallas, Texas; Milwaukee, Wisconsin; Ottawa, Ontario; Pittsburgh, Pennsylvania; Portland, Oregon; San Diego, California; Seattle (King County), Washington; Toronto, Ontario; and Vancouver, British Columbia. Data from later than 2010 were not available due to clinical trial-related data availability limitations. For perspective, while this capture period includes the ROC-PRIMED clinical trial,11 it excludes the currently on-going CCC and ALPS studies whose methodology have been published.12–13
Cases of OD-OHCA were identified through case record review by local data abstractors. These individuals had access to electronic and written prehospital patient care reports produced by emergency medical technicians and paramedics, digital defibrillator download files, and limited in-hospital records. Sufficient evidence of OD-OHCA necessitated explicit indication of the acute use of drugs at the time of the OHCA; case definition rules for OD required near certainty of case status. Examples of positively identifying circumstances included: in-hospital clinical notes indicating a positive toxicological screen, prehospital administration of naloxone (an opioid reversal agent), and paramedic notes explicitly stating that the patient had overdosed. Not all of these conditions were ascertainable for all cases due to differential case data availability throughout the study period. For example, prehospital naloxone administration was only collected globally throughout the ROC until 2009. Examples of insufficient identifying circumstances for OD-OHCA included: presence of drug paraphernalia at the scene of the OHCA, prior history of drug use, and patient characteristics suggesting drug overdose (e.g. young, asystolic patient).
The structure of the ROC necessitated a specialized incidence calculation methodology. Incidence of OD-OHCA was calculated by accounting for individual EMS agencies’ participation in the ROC, ROC PRIMED trial, and associated surveillance activities. The service area of each EMS agency was used to approximate a service population from census data. For US agencies, 2000 US Census data was used, while Statistics Canada 2006 was used for Canadian agencies. Total person-years for each agency's service area were calculated by multiplying its participation period by its approximate service population. Incidence of OHCA and OD-OHCA were then calculated at the site level by dividing the number of events in each site by the accumulated person time of all of its participating agencies between 2006 and 2010. Incidence was reported per 100,000 person-years for ROC overall and by anonymized site ID.
The total catchment area of the participating ROC sites encompassed 35,331 square miles with an estimated combined population of 19.5 million. Underlying rates, outcomes and characteristics of all-cause OHCA throughout the participating areas have been described previously.14 Environments include a mix of urban, suburban and rural settings, and EMS agencies included both basic and advanced life support capabilities.
Key covariates
The ability to assess individual patient characteristics was limited by the design of the underlying (or parent) OHCA surveil-lance system. Patient age, sex and presenting electrocardiogram (ECG) rhythm were the only universally available patient specific characteristics. Other factors of interest such as race, body-mass index, current medications and medical history were often not available. Presenting ECG rhythm was categorized as ventricular fibrillation/ventricular tachycardia (VF/VT), shockable by automated external defibrillator (AED), pulseless electrical activity (PEA), asystole, and no shock advised by an AED. However, numerous resuscitation characteristics were available, including event timing, witness status, cardiopulmonary resuscitation (CPR) quality characteristics, advanced airway placement, defibrillation, and administration of drugs. Available resuscitation drug variables included epinephrine, sodium bicarbonate, and atropine. Total medication dosage was available for epinephrine was reported in milligrams.
The earliest available CPR quality parameters for up to 20 min of CPR were compared between patients with and without OD-OHCA. The ROC captures chest compression rate (CCR), chest compression fraction (CCF), and depth when sufficient data streams are available in digital defibrillator files. Unfortunately, chest compression depth requires specialized hardware, which not all EMS agencies currently deploy. Therefore, we were only able to compare cases on the basis of CCR and CCF, which are nearly universally calculable with standard prehospital equipment.
Outcome measures
Three primary outcomes were ascertained in order to understand the effect of OD-OHCA case status on patient prognosis: return of spontaneous circulation (ROSC), survival to emergency department (ED), and survival to hospital discharge. ROSC was defined as the return of pulses at any time during the course of prehospital treatment, as indicated by prehospital patient care reports or digital defibrillator data. Survival to ED was defined as the patient attaining ROSC and maintaining ROSC for any duration until arrival at the ED. Survival to hospital discharge was defined as post-resuscitation discharge or transfer from the receiving hospital alive regardless of neurologic status.
Data management and quality assurance
Basic data quality was supported by ROC site-level and central quality assurance measures. Each ROC site conforms to uniform ROC data collection forms and procedures, but implements its own quality assurance procedures. These may, for instance, include re-review of randomly selected cases or prescreening of abstracted data for erroneous outlying values. The ROC DCC conducts internal quality control through self-checking electronic data entry forms, as well as through periodic random review of case data from regional sites.
Statistical analysis
Case characteristics were summarized and then compared between OD-OHCA and non-OD-OHCA cases. Dichotomous variables were reported as totals with proportions. Continuous variables were reported as means with standard deviations (SD) or as medians with interquartile ranges (IQR). Multiple logistic regression analysis was used to separately assess the relationship between OD-OHCA cases status and the outcomes of ROSC, survival to ED, and survival to hospital discharge while accounting for select patient and resuscitation covariates. Model covariates were chosen a priori from characteristics known to correlate with resuscitation outcomes, including in the context of OD-OHCA.7 ODOHCA incidence and case proportions were compared between ROC sites using the chi-squared test. Both CCR and CCF were compared between OD-OHCA and non-OD-OHCA cases while accounting for early/late resuscitation phases with generalized estimating equations (GEE). We included this analysis because a previous study demonstrated a difference between CPR quality between OD-OHCA and non-OD-OHCA cases that appeared to be driven by differences in late resuscitation CPR quality. In the present study, to accommodate a wide range of available durations of CPR, early and late resuscitation phases were arbitrarily defined as during or after the first 3 min or 5 min of attempted resuscitation by EMS providers, where these 2 criteria were used in 2 separate GEE models. Without a specific basis for delineating between physiologically significant early and late phases of CPR, we chose to explore both of these cutoff criteria. CPR process parameters were not available consistently for all cases. Therefore only the subset of all cases with CCR and/or CCF was utilized for analyses. Model diagnostics were run to determine any overly influential subjects. An alpha level of 0.05 was used as the criteria of statistical significance for all tests.
Results
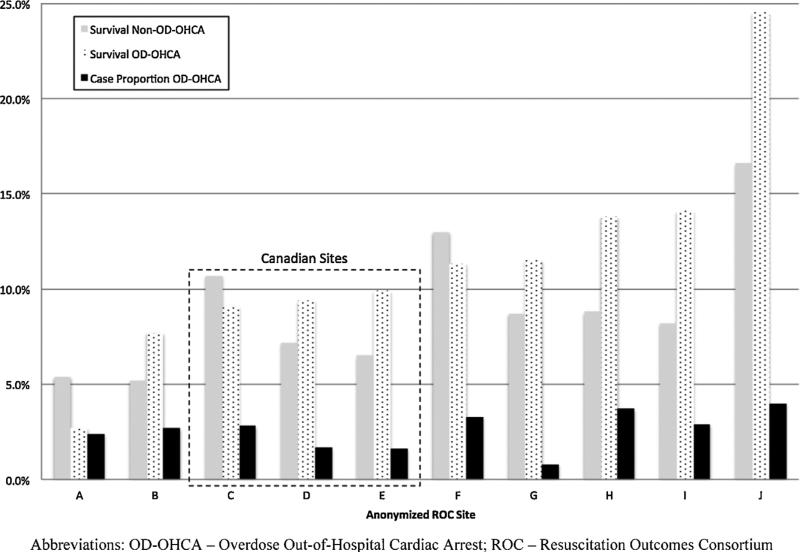
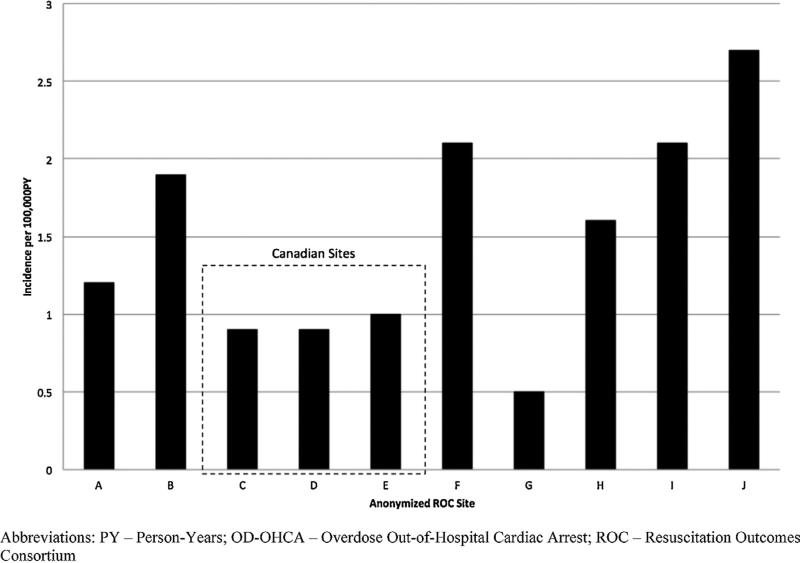
Fig. 1 illustrates a consort diagram for this study. A total of 56,272 cases of EMS-treated OHCA were captured in all sites over the designated study period. Of these, 1351 (2.4%) were classified as OD-OHCA, with a range of 0.8–4.0% among the individual sites. Numerical ranges, participation counts and population estimates are tabulated in Table 1. Case proportions of OD-OHCA, as well as OD-OHCA survival and non-OD-OHCA survival, are visualized in Fig. 2 stratified by anonymized ROC site with Canadian sites highlighted for comparison. Population incidences of OD-OHCA for the study period are shown in Fig. 3, stratified by anonymized ROC site. Both OD-OHCA case proportion (p < 0.001) and population incidence (p < 0.001) differed significantly across the 10 sites.
Fig. 1.
Cohort diagram.
Table 1.
Incidence and OD-OHCA case proportion by site.
| Site | All OHCA, n | OD-OHCA, n | Proportion OD-OHCA | Catchment population (in person-years) | Average OD-OHCA incidence (per 100,000 person-years) |
|---|---|---|---|---|---|
| A | 1555 | 37 | 2.4% | 2,827,529 | 1.2 |
| B | 5459 | 147 | 2.7% | 4,981,666 | 1.9 |
| C | 6674 | 189 | 2.8% | 9,452,687 | 0.9 |
| D | 8553 | 142 | 1.7% | 12,091,062 | 0.9 |
| E | 13,679 | 213 | 1.6% | 18,376,190 | 1 |
| F | 4538 | 152 | 3.3% | 6,418,841 | 2.1 |
| G | 3640 | 29 | 0.8% | 4,289,383 | 0.5 |
| H | 3350 | 123 | 3.7% | 1,592,427 | 1.6 |
| I | 2724 | 78 | 2.9% | 2,961,489 | 2.1 |
| J | 6100 | 241 | 4.0% | 6,852,373 | 2.7 |
| ROC | 56,272 | 1351 | 2.4% | 69,843,645 | 1.3 |
Abbreviations: OD-OHCA – overdose out-of-hospital cardiac arrest; ROC – Resuscitation Outcomes Consortium.
Fig. 2.
OD-OHCA case proportion and survival rates stratified by anonymized site.
Fig. 3.
2006–2010 aggregate incidence of OD-OHCA stratified by anonymized site.
Patient and resuscitation characteristics are shown in Table 2. OD-OHCA cases were younger than non-OD-OHCA cases. Likewise OD-OHCA cases were more likely to present in asystole and were less than half as likely than non-OD-OHCA cases to present in VF/VT. Time intervals, including time to dispatch, time to EMS arrival and time to first CPR, did not differ substantially between cases with and without OD-OHCA. Interestingly, cases with OD-OHCA were half as likely to be bystander witnessed and subsequently about 50% more likely than non-OD-OHCA cases to be unwitnessed by either bystanders or EMS. OD-OHCA cases were slightly more likely than non-OD-OHCA cases to get epinephrine and almost twice as likely to receive sodium bicarbonate. Advanced airways were slightly more common in OD-OHCA cases, while non-OD-OHCA cases were substantially more likely to receive a defibrillation prior to hospital arrival, reflecting in large part the prevalence of VF/VT initial ECG rhythm among non-OD-OHCA cases.
Table 2.
Descriptive Statistics by OD Status
| Demographic/Characteristic | OD-OHCA, n = 1351 | Non-OD-OHCA, n = 54921 | All, n = 56272 |
|---|---|---|---|
| Age, median* (IQR), y | 41 (30, 50) | 67 (54, 80) | 67 (53, 80) |
| Male sex*, n (%) | 893 (66.2%) | 34790 (63.5%) | 35683 (63.5%) |
| Location of Arrest*, n (%) | |||
| Public | 207 (15.3%) | 8226 (15.0%) | 8433 (15.0%) |
| Private | 1139 (84.3%) | 45423 (82.7%) | 46562 (82.7%) |
| Other | 5 (0.4%) | 1272 (2.3%) | 1277 (2.3%) |
| First Rhythm*, n (%) | |||
| VT/VF/Shockable | 109 (8.2%) | 12497 (23.3%) | 12606 (22.9%) |
| Asystole | 806 (60.7%) | 23367 (43.5%) | 24173 (43.9%) |
| PEA | 242 (18.2%) | 11239 (20.9%) | 11481 (20.9%) |
| No Shock Advised/Not Shockable | 126 (9.5%) | 5220 (9.7%) | 5346 (9.7%) |
| Witnessed Status, n (%) | |||
| Bystander* | 252 (21.8%) | 20782 (44.4%) | 21034 (43.8%) |
| EMS* | 121 (9.0%) | 5512 (10.0%) | 5633 (10.0%) |
| Unwitnessed* | 895 (77.4%) | 25598 (54.6%) | 26493 (55.2%) |
| Bystander CPR, n(%) | 461 (37.2%) | 19508 (38.3%) | 19969 (38.3%) |
| Vehicle Dispatch Time, mean (SD), minutes | 1.08 (1.59) | 1.08 (4.43) | 1.08 (4.39) |
| EMS Arrival Time*, mean (SD), minutes | 5.72 (3.26) | 6.00 (4.82) | 5.99 (4.79) |
| 1st CPR Time*, mean (SD), minutes | 9.54 (7.03) | 10.14 (7.61) | 10.13 (7.60) |
| 1st Shock Time*, mean (SD), minutes | 19.31 (10.54) | 16.38 (11.43) | 16.42 (11.43) |
| 1st ROSC Time, mean (SD), minutes | 24.60 (11.83) | 24.86 (15.37) | 24.86 (15.29) |
| Transport Time*, mean (SD), minutes | 35.66 (13.18) | 32.85 (15.34) | 32.91 (15.30) |
| ED Arrival Time*, mean (SD), minutes | 43.77 (15.22) | 41.04 (17.13) | 41.11 (17.09) |
| Survival to Discharge* | 170 (12.7%) | 4838 (8.9%) | 5008 (9.0%) |
| ROSC* | 452 (33.5%) | 16825 (30.7%) | 17277 (30.7%) |
| Epinephrine | |||
| Proportion given* | 0.81 | 0.78 | 0.78 |
| Amount administered, mean (SD), mg | 3.46 (1.94) | 3.41 (1.96) | 3.41 (1.96) |
| Sodium Bicarbonate*, Proportion Given | 0.30 | 0.18 | 0.19 |
| Atropine*, Proportion Given | 0.71 | 0.64 | 0.64 |
| Advanced Airway*, Proportion Given | 0.85 | 0.80 | 0.81 |
| EMS Defibrillation | |||
| Proportion given* | 0.21 | 0.36 | 0.35 |
| Number of shocks given*, mean (SD) | 2.27 (2.05) | 3.14 (2.69) | 3.13 (2.69) |
statistically significant at the 0.05 level.
Abbreviations: CPR – Cardiopulmonary Resuscitation; ED – Emergency Department; EMS – Emergency Medical Services; IQR – Interquartile Range; OD-OHCA – Overdose Out-of-Hospital Cardiac Arrest; PEA – Pulseless Electrical Activity; ROC – Resuscitation Outcomes Consortium; ROSC – Return of Spontaneous Circulation; SD – Standard Deviation.
Overall, mean (SD) CCF in the study cohort was 0.71 (0.16), while mean (SD) CCR was 112 (19) compressions per minute. Mean (SD) CCF among OD-OHCA cases was 0.72 (0.17) compared to 0.71 (0.16) in non-OD-OHCA cases. Mean (SD) CCR among OD-OHCA and non-OD-OHCA cases were identical at 112 (19) for each.
The relationship between CPR process measures and time was considered separately with both a 3- and 5-min cutoff value for demarcating between Early and Late CPR. CCF increased between Early and Late phase CPR when either 3 min (coeff. = 0.030, p < 0.01) or 5 min (coeff. = 0.032, p < 0.01) were used as the cutoff. CCF did not differ between OD-OHCA and non-OD-OHCA cases during Early or Late phase CPR using either cutoff. CCR increased between Early and Late phase CPR regardless of whether 3 min (coeff. = 1.92, p < 0.01) or 5 min (coeff. = 1.23, p < 0.01) were used as the cutoff. CCR only differed between OD-OHCA and non-OD-OHCA cases during Early phase CPR (coeff. = 2.19, p < 0.43) using the 5-min cutoff.
Logistic regression model results are summarized in Table 3. Cases with OD-OHCA were more likely than non-OD-OHCA cases to achieve prehospital ROSC, survive to ED, and to survive to hospital discharge. In multivariable models, all outcomes were significantly, directly associated with OD-OHCA case status after adjustment for common predictors of OHCA outcomes.
Table 3.
Adjusted Predictors of Resuscitation Outcomes.
| Predictor | ROSC Odds ratio | ROSC at ED arrival Odds ratio | Survival to discharge Odds ratio |
|---|---|---|---|
| OD-OHCA Status | 1.551 (1.353–1.779) | 1.766 (1.491–2.091) | 2.135 (1.722–2.647) |
| Age (in years) | 1.004 (1.003–1.005) | 1.005 (1.003–1.006) | 0.982 (0.981–0.984) |
| Male | 0.769 (0.735–0.805) | 0.726 (0.687–0.768) | 0.817 (0.752–0.888) |
| Public Location | 1.216 (1.146–1.290) | 1.030 (0.962–1.102) | 2.007 (1.846–2.182) |
| VF/VT | 2.884 (2.744–3.032) | 2.212 (2.086–2.347) | 7.516 (6.924–8.158) |
| Bystander CPR | 1.100 (1.052–1.151) | 1.073 (1.017–1.132) | 1.140 (1.055–1.231) |
| Bystander Wit. | 1.859 (1.786–1.936) | 1.697 (1.616–1.784) | 2.087 (1.947–2.238) |
| EMS Wit. | 1.825 (1.499–2.220) | 1.658 (0.734–3.744) | 4.317 (3.194–5.834) |
| Site A | 0.238 (0.200–0.283) | 0.178 (0.147–0.215) | 0.465 (0.343–0.632) |
| Site B | 0.232 (0.207–0.261) | 0.164 (0.143–0.188) | 0.463 (0.377–0.568) |
| Site C | 1.000 (–) | 1.000 (–) | 1.000 (–) |
| Site D | 0.440 (0.407–0.475) | 0.357 (0.325–0.393) | 0.650 (0.565–0.746) |
| Site E | 0.473 (0.441–0.507) | 0.391 (0.358–0.426) | 0.641 (0.564–0.727) |
| Site F | 0.830 (0.759–0.907) | 0.874 (0.783–0.975) | 1.102 (0.953–1.274) |
| Site G | 0.514 (0.463–0.570) | 0.681 (0.595–0.778) | 1.188 (0.992–1.424) |
| Site H | 0.752 (0.679–0.833) | 1.385 (1.203–1.595) | 1.131 (0.944–1.355) |
| Site I | 0.525 (0.466–0.591) | 0.422 (0.364–0.488) | 0.829 (0.675–1.018) |
| Site J | 1.284 (1.188–1.388) | 1.280 (1.159–1.414) | 1.915 (1.685–2.177) |
Abbreviations: CPR – cardiopulmonary resuscitation; ED – emergency department; EMS – emergency medical services; OD-OHCA – overdose out-of-hospital cardiac arrest; ROSC – return of spontaneous circulation; SD – standard deviation; VF/VT – ventricular fibrillation/ventricular tachycardia; Wit. – witnessed.
Discussion
Our principal findings relate to the general epidemiologic description of OD-OHCA across a broad, demographically diverse geographic area. Our absolute incidence estimates have the major limitation of being not directly applicable to the current time period. Even so, the variability of OD-OHCA incidence between regions, characteristics of OD-OHCA patients, OD-OHCA resuscitation outcomes, and to a lesser extent the proportion of all OHCA due to OD-OHCA still hold valuable information despite the age of our data.
We observed that the incidence of OD-OHCA varied significantly across the US and Canada, demonstrating variability comparable to all-cause OHCA incidence over the same region. Regional differences in pathology, resuscitation practices and performance, and post-resuscitation care are likely responsible for variation in outcomes overall and among OD-OHCA, although it is impossible to determine the critical factors in the variability seen in this study from the available data. Underlying regional differences in drug abuse and drug availability likely also contribute to the etiologyspecific OD-OHCA incidence and survival rates. Differential regional patterns of drug abuse throughout the US have been demonstrated in the results of the National Institute on Drug Abuse Community Epidemiology Workgroup (CEWG).15 The primary agent implicated in drug-related ED visits has been shown to vary between metropolitan areas in the participating CEWG areas, and likewise the incidence rates of drug related visits for individual agents vary regionally. In the current study we are unable to connect the regional identity of ROC sites to site-specific incidence estimates, however we expect that uniform case classification methodology, if present, would result in a proportional relationship between our estimates and epidemiologic trends in drug-related ED visits and OD mortality if we were able to conduct such an analysis. In Figs. 2 and 3, we provide what limited geographic identification that we can, highlighting the incidence, case proportion and survival rates of individual Canadian sites, for comparison with US sites. It is worth noting that Canadian sites seem to demonstrate close agreement in OD-OHCA survival rates despite what we know of the sites’ geographic distribution. The same is not explicitly obvious for US sites.
Our findings indicate that OD-OHCA does not make up a large proportion of all OHCA cases when compared to non-OD-OHCA. Non-OD-OHCA cases are predominantly of cardiac origin, and their incidence reflects the burden of chronic cardiovascular disease in the US and Canada. However, despite the relatively small proportion of overall OHCA made up by OD-OHCA cases, the absolute number of cases is non-trivial. We can approximate a figure by extrapolating from Nichol's estimate of OHCA incidence from the ROC.14 If we expect approximately 180,000 EMS-treated OHCA cases per year in the US, or 20,000 in Canada, and if 2.4% of these cases are OD-OHCA, this yields over 4000 OD-OHCA cases annually in the US and 480 in Canada.
OD-OHCA rates in the present study likely are underestimated due to a number of factors. First, OD-OHCA case classification criteria were stringent in the presence of limited data. ROC data collection forms provided some information for inferring to the OD-OHCA status of cases, but they were not designed specifically for this purpose, nor is prehospital data necessarily ideal for determining the precise etiology of any OHCA. EMS patient care reports contained varying levels of detail from which inference about OD status could be derived, and it is likely that the level of detail available for determining case status largely depended on EMS agency-level reporting practices. Second, our study only considered cases that were EMS-treated. A true estimate of ODOHCA incidence would include those cases that were not treated either due to delayed discovery, the medical futility of resuscitation, or regional legislated standards for the termination of resuscitation. Insufficient data were available in the present study for this more comprehensive, EMS-assessed OD-OHCA estimate. Lastly, despite uniformly stringent classification standards, ROC sites may be differentially vigilant in ascertainment of OD-OHCA cases, as ODOHCA has neither historically been a resuscitation research priority in general nor a specific founding research priority of the ROC. Conversely, it is also possible that some cases identified as OD-OHCA through presence of naloxone administration may have in fact been non-OD-OHCA that received naloxone for mere suspicion of OD. The data available to us for this study do not allow us to definitively rule out this possibility. Similarly, we are likewise unable to definitively determine whether, in those cases with a positive toxicological screen, the drugs detected on the screen actually played a mechanistic role in the OHCA event.
Our findings reiterate previous work showing the relationship between OD etiology of OHCA and resuscitation outcomes. Local analysis of Pittsburgh OHCA cases showed a survival advantage for OD-OHCA cases.7 While the obvious conclusion is that OD-OHCA cases are younger on average and therefore are more likely to survive, the effect of OD-OHCA persists in models adjusting for age. One hypothesis for the association between OD-OHCA and survival is that some OD-OHCA cases may be erroneously classified as cardiac arrests, and may have in fact never lost pulses. Review of digital defibrillator data affords ROC data abstractors the luxury of identifying the presence of lethal arrhythmia. Under these circumstances, asystole and VF/VT are unambiguously differentiable from organized rhythms. However, within PEA cases, there exists significant ambiguity. No definitive criteria are available for differentiating non-pulsatile organized rhythms from pulsatile rhythms through ECG analysis alone. ROC data abstractors are not instructed to make judgments about the presence of a pulse or not based on speculation related to heart rate, complex width, or similar features. Instead ROSC is ruled out by the presence of on-going chest compressions. So it may be the case that the OD-OHCA cases in this study were disproportionally made up of cases that did not have a complete cardiac arrest, and therefore would appear to have had among them a higher proportion of survivors. This finding may be supported by the observation that even after multivariable adjustment, both OD-OHCA status (which correlated strongly with PEA/Asystole) and VF/VT were predictive of survival in the same model.
We observed some patient and treatment differences between OD-OHCA and non-OD-OHCA cases, supporting some of our previous findings. However, there is not complete agreement with our previous work. We had previously demonstrated that ODOHCA and no-OD-OHCA cases differed in CCF during later phases of resuscitation.7 We suspected that this phenomenon reflected differential distributions of ECG rhythms as time passed in cases of either etiology. Predominance of non-shockable rhythms in ODOHCA cases during late-phase resuscitation might have resulted in fewer pauses for rhythm analysis and shock delivery. That this was not observed in the present study was surprising, although this may reflect variability of treatment characteristics introduced by inclusion of multiple geographic regions. While we did find a difference CCR between OD-OHCA and non-OD-OHCA cases during early phase CPR, the magnitude of this difference may not be clinically significant.
The question of whether OD-OHCA cases should be treated differently from non-OD-OHCA cases remains open, and the present study does not independently provide grounds for indicating a differential course of resuscitation. Previous studies have considered agent-specific intra-resuscitation drug administration in the context of OD-OHCA, although to date insufficient evidence exists for their use.15 Hypothetically, these could include administration of drugs such as naloxone, flumazenil, or lipid emulsion. These treatments are intended to block or immobilize the agents that caused cardiac arrest and are differentiated from treatments intended to mitigate conditions secondary to the cardiac arrest itself, such as sodium bicarbonate for the correction of prolonged acidosis secondary to respiratory arrest. In either case, high quality CPR is the most generally applicable approach to treating OD-OHCA. If reversal agents or metabolic corrective therapies are applied, care should be taken that they not interfere with effective chest compressions until ROSC is achieved.
This study faces many of the limitations of similar retrospective observational resuscitation studies. A major epidemiologic limitation is the restriction of the current study to data between 4 and 9 years old. Compounding this limitation is the inability to draw conclusions about temporal changes in the primary study variables due to the specific method in which incidence was calculated. As mentioned previously, the structure of the ROC limits patient-specific data available for analysis. Therefore, our analyses lack texture regarding medical history, post-resuscitation care, and with respect to OD in particular, the class of drug implicated in the OD.
Conclusions
OD-OHCA cases constitute 2.4% of all OHCA throughout several regions in the US and Canada. Incidence of OD-OHCA varies significantly from 0.5 to 2.7 per 100,000 person years between geographic regions. The incidence is consistently lower in Canadian sites with less variability in both incidence and outcome when compared to the US sites in this study. OD-OHCA cases were more likely to survive than non-OD-OHCA cases, even when adjustment was made for key patient and treatment characteristics predictive of survival.
Supplementary Material
Acknowledgments
The ROC is supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01 HL077863 – University of Washington Data Coordinating Center, HL077865 – University of Iowa, HL077866 – Medical College of Wisconsin, HL077867 – University of Washington, HL077871 – University of Pittsburgh, HL077872 – St. Michael's Hospital, HL077873 – Oregon Health and Science University, HL077881 – University of Alabama at Birmingham, HL077885 – Ottawa Hospital Research Institute, HL077887 – University of Texas SW Medical Ctr/Dallas, HL077908 – University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) – Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada and the American Heart Association. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health.
Dr. Salcido received a small grant from the Pittsburgh Emergency Medicine Foundation in support of this project.
Dr. Nichol receives salary support from the University of Washington via the Leonard A Cobb Medic One Foundation Endowed Chair in Prehospital Emergency Care. He holds Research Grants from the following: (1) National Heart, Lung, and Blood Institute, Bethesda, MD. Resuscitation Outcomes Consortium (NIH U01 HL077863-05) 2004–2015; Co-PI; (2)Food and Drug Administration, Silver Spring, MD; Cardiac Science Corp, Waukesha, WI; Heartsine Technologies Inc., Newtown, PA; Philips Healthcare Inc., Bothell, WA; Physio-Control Inc., Redmond, WA; ZOLL Inc., Chelms-ford, MA. University of Washington Dynamic AED Registry, PI. 2013–2015 (4) Velomedix Inc., Menlo Park, CA. Velocity Pilot Study of Ultrafast Hypothermia in Patients with ST-Elevation Myocardial Infarction, National Co-PI. 2014–2015. *Waived personal compensation. He did not receive any other Research Support. He is not a member of Speakers Bureau and does not hold an Honorary post in any company. He has no other conflict of interest to declare. He received travel reimbursement from Abiomed Inc., Danvers, MA.
Dr Morrison holds the Robert and Dorothy Pitts chair in Acute Care and Emergency Medicine, St Michael's Hospital and University of Toronto, and receives salary support from the NIH NHLBI grant supporting the University of Toronto Resuscitation Outcomes Consortium Regional Coordinating Center Grant.
Footnotes
A Spanish translated version of the abstract of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2015.11.010.
Conflict of interest statement
The authors do not believe that any current or past financial relationships represent conflicts of interest with respect to the scientific or ethical integrity of this study.
References
- 1.Centers for Disease Control [15.02.15];CDC Wonder. http://wonder.cdc.gov.
- 2.Paredes VL, Rea TD, Eisenberg MS, et al. Out-of-hospital care of critical drug overdoses involving cardiac arrest. Acad Emerg Med. 2004;11:71–4. doi: 10.1197/j.aem.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Boyd JJ, Kuisma MJ, Alaspää AO, Vuori E, Repo JV, Randell TT. Outcome after heroin overdose and cardiopulmonary resuscitation. Acta Anaesthesiol Scand. 2006;50:1120–4. doi: 10.1111/j.1399-6576.2006.01142.x. [DOI] [PubMed] [Google Scholar]
- 4.Hess EP, Campbell RL, White RD. Epidemiology, trends, and outcome of out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation. 2007;72:200–6. doi: 10.1016/j.resuscitation.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 5.Deasy C, Bray JE, Smith K, Harriss LR, Bernard SA, Cameron P. Out-of-hospital cardiac arrests in young adults in Melbourne, Australia. Resuscitation. 2011;82:830–4. doi: 10.1016/j.resuscitation.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Park JH, Shin SD, Song KJ, Park CB, Ro YS, Kwak YH. Epidemiology and outcomes of poisoning-induced out-of-hospital cardiac arrest. Resuscitation. 2012;83:51–7. doi: 10.1016/j.resuscitation.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Koller AC, Salcido DD, Callaway CW, Menegazzi JJ. Resuscitation characteristics and outcomes in suspected drug overdose-related out-of-hospital cardiac arrest. Resuscitation. 2014;85:1375–9. doi: 10.1016/j.resuscitation.2014.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lavonas EJ, Drennan IR, Gabrielli A, et al. Part 10: special circumstances of resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S501–18. doi: 10.1161/CIR.0000000000000264. [DOI] [PubMed] [Google Scholar]
- 9.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of emergency medical service systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11:369–82. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 10.Aufderheide TP, Kudenchuk PJ, Hedges JR, et al. Resuscitation Outcomes Consortium (ROC) PRIMED cardiac arrest trial methods part 1: rationale and methodology for the impedance threshold device (ITD) protocol. Resuscitation. 2008;78:179–85. doi: 10.1016/j.resuscitation.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kudenchuk PJ, Brown SP, Daya M, et al. Resuscitation Outcomes Consortium-Amiodarone, Lidocaine or Placebo Study (ROC-ALPS): rationale and methodology behind an out-of-hospital cardiac arrest antiarrhythmic drug trial. Am Heart J. 2014;167:653–9. e4. doi: 10.1016/j.ahj.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang HE, Schmicker RH, Herren H, et al. Classification of cardiopulmonary resuscitation chest compression patterns: manual versus automated approaches. Acad Emerg Med. 2015;22:204–11. doi: 10.1111/acem.12577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute on Drug Abuse Epidemiologic trends in drug abuse. Proceedings of the Community Epidemiology Work Group. 2013 [Google Scholar]
- 15.Morrison LJ, Deakin CD, Morley PT, et al. Part 8: advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122:S345–421. doi: 10.1161/CIRCULATIONAHA.110.971051. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.