Abstract
We study how the health insurance coverage of Mexican immigrants changes with time in the U.S. Cross sectional estimates indicate that time since arrival is negatively correlated with the probability of being uninsured for both male and female Mexican immigrants, and about a third of the decline could be attributed to civic and labor market incorporation of Mexican immigrants. However, much of the relationship between time in the U.S. and health insurance coverage, after adjusting for demographic and labor market factors, is due to failure to control for age at arrival and period of arrival. Estimates from longitudinal analyses suggest that there is no systematic relationship between time in the U.S. and health insurance of Mexican immigrants, although imprecision in the fixed effects estimates makes it difficult to draw firm conclusions.
Keywords: Mexicans, Immigration, Health, Health insurance, Acculturation
Introduction
Previous research documents that upon arrival in the US immigrants are on average healthier than comparable US-born persons but their health advantage declines over time.1 The common explanation for their health trajectory is that immigrants are positively selected on health and that assimilation is unhealthy (Jasso et al. 2004, Kaestner et al. 2009,Vega and Amaro 1994). Assimilation often exposes immigrants to incidents of prejudice and discrimination which are stressful. Migration itself could be stressful and may adversely affect health. Furthermore, stress may cause immigrants to engage in unhealthy behaviors (Kaplan and Marks 1990). With assimilation, immigrants also adopt host country cultural norms including behaviors that are less healthy while losing certain protective aspects of their native cultures (e.g. healthy eating) and support networks tied to native cultures (Vega and Amaro 1994).
A potentially important factor affecting immigrant health trajectories is health insurance. Health insurance improves access to and use of health care services (Newhouse 1993). Health insurance may also change with time in the US as immigrants’ earnings rise and they integrate with the US civic system. Thus, it is possible that health insurance, and the increased use of health care associated with it, may offset adverse health shocks.2 If, on the other hand, there is no corresponding increase in health insurance coverage, the declining health of immigrants may affect their productivity and impose a burden on state and local governments who bear a significant responsibility for the health care costs of the uninsured. Despite the policy significance of this issue, surprisingly few studies have systematically investigated it.
In this paper, we study whether health insurance changes with time in the U.S. among Mexican immigrants. We focus on Mexican immigrants because they are the largest immigrant group in the country and are relatively disadvantaged compared to other immigrants in terms of education, earnings, visa status, and health insurance (Borjas and Katz 2007, Cho et al. 2004, Duncan et al. 2006, Kaushal 2008, Passel and Cohn 2009, Ramirez 2004, Rumbaut 2006). As of 2008, a third of all foreign-born persons and 23% of the working age population without a high-school degree in the US were born in Mexico and almost two thirds of the new arrivals ((in the US for less than 5 years) did not have health insurance. Mexican immigrants differ from other immigrants, including other Hispanics, in civic and socioeconomic incorporation, geographic location, return migration and health-behavioral norms. Thus, their health insurance trajectories may differ from those of other immigrants and a study of broader immigrant groups may be uninformative about the experience of this largely uninsured immigrant population.
Our paper makes three contributions. We provide the first systematic study of changes in health insurance coverage of Mexican immigrants with time since immigration using cross-sectional and longitudinal data. Secondly, we draw inferences about the likely pathways through which health insurance of Mexican immigrants’ changes with time in the US. Finally, ours is the first study of changes in dependence on public health insurance with time in the US.
Previous Literature
Two previous studies examined changes in health insurance with time in the U.S. for broader groups of immigrants and found a positive association between insurance coverage and years since immigration. LeClere et al. (1994) used data from the National Health Interview Survey (NHIS) for 1990 and Thamer et al. (1997) used data from the NHIS for 1989 and 1990. Neither of these papers examined Mexican immigrants separately. More importantly, they used cross-sectional data and did not control for confounding factors such as age at arrival and year of arrival. A cross-sectional analysis may yield biased estimates if the immigrant population exhibits selective return migration because those who plan to return may prefer relatively high wage jobs with no health insurance over relatively low wage jobs with insurance. In the presence of selective return migration, these studies will estimate improvement in insurance coverage over time even when there is no change. We address several of these limitations by applying appropriate models and cross-sectional and longitudinal data.
Conceptual Model and Empirical Strategy
There are a number of reasons why the health insurance of immigrants may change with the length of their stay the U.S. Immigrant earnings generally grow with the duration of stay in the U.S. Higher incomes improve ability to obtain health insurance either directly or through employer-provided insurance. Changes in legal status may also enhance the ability to obtain health insurance because of access to jobs that provide health insurance, or in the case of women, access to publicly provided insurance such as Medicaid. Insufficient information about the US healthcare system upon arrival and cultural barriers may also affect insurance coverage. These barriers decline with time in the U.S. (Wong and Espinoza 2006). Finally, changes in health may also affect immigrants’ demand for health insurance.
Our empirical approach, consistent with these theoretical considerations, is to first obtain estimates of the association between time in the U.S. and health insurance. To identify potential causes underlying the association we sequentially add determinants of health insurance, or proxy variables for these determinants, to the regression models. We focus on labor market outcomes such as hours and weeks of work, citizenship, and health status.3 Changes in associations between time in the US and health insurance, before and after the inclusion of these variables, will provide evidence of the importance of these underlying factors. Our analysis also controls for age at arrival and year of arrival – variables that may mediate the association between time in the US and health insurance. Year of arrival may proxy for economic conditions in Mexico and the U.S., and U.S. immigration policy that influence migration decisions (i.e., the types of immigrants) and thus may influence the insurance coverage of immigrants because of differences in preferences and other unmeasured determinants of insurance. Age at arrival may affect information of, or eligibility for, public health insurance. Notably, previous research has not accounted for these potentially confounding factors.
We use the following baseline model on a sample of Mexican immigrants from the March Current Population Survey (CPS):4
| (1) |
In equation (1), the health insurance status (HI – equals to 1 if the respondent lacks health insurance, otherwise 0) of Mexican immigrant (i) of age (j) in year (t) is a function of individual characteristics (X) namely education, marital status, number of children under 18 in the household, and state of residence in the US; state characteristics (Z) namely the unemployment rate, per-capita income, and rate of health insurance coverage among US-born non-Hispanic whites of same age, sex and education; and a set of dummy variables indicating each year of age (δj), years since immigration (YSIit), and each year of observation (ηt). YSI is measured in intervals: 0–5, 6–10,11–15,16–20, and 21–38 years. The parameters of interest are given by αm, which provide estimates of the association between health insurance and YSI. Because health insurance determinants are likely to differ by gender, all analyses are done separately by gender.
Equation (1) will yield estimates of the association between years in the US and health insurance that is due to changes in underlying determinants of health insurance such as changes in earnings and citizenship. Accordingly, we assess whether associations between health insurance and time in the U.S. are mediated by factors known to change with time since immigration, specifically, labor market outcomes and citizenship. Models similar to equation (1) are estimated by sequentially adding other variables that capture these mediating factors. The construction and specification of these variables are fully described in the data section.
Equation (1) does not control for year of arrival or age at arrival -variables that are likely to be correlated with years since immigration and health insurance status. They may also be correlated with labor market variables and citizenship, as well as other variables. Therefore, we estimate a third specification that includes these variables. We address the collinearity between year of observation, year of arrival, and years since immigration (years since immigration = year of observation – year of arrival) by grouping observations by years since immigration and year of arrival. Similarly, there is perfect collinearity between age, age at arrival, and years since immigration [age at arrival = age − (year of observation −year of arrival)]. So here too, we group one of the variables into categories, in this case, age at arrival (Mason et al. 1973).
Cross-sectional analysis may be biased if return migration is selective. We address this issue by using longitudinal data from the CPS that follow the same persons over time, eliminating return migrants and others who cannot be followed in the data). Years-since-arrival in the CPS is measured in categories because of the data reporting. These categories are sometimes quite large, and if we estimate equation (2) with person fixed effects, variation would come from only switching categories. But only a small proportion of persons switch categories even though every person adds another year of time in the US. To exploit more of the variation in time since arrival in the U.S., we estimate a slightly modified specification, described as:
| (2) |
There are two things to note about equation (3). First, the value of years-since-arrival in the U.S. is fixed at year t-1 values. Each person is in the sample for two periods: t-1 and t. Second, we allow the effect of years-since-immigration to differ by whether the observation is from year t-1 or year t. Here this choice is reflected by the interaction term (YSIij(t−1)m *YEAR_T). The parameters of interest are ᾶm, which measure differences in the health-insurance in year t versus year t-1 at various points of time since arrival in the US. Note that the main effect of years since arrival in the US drops out of the model because it is time invariant for each individual.
The inclusion of person fixed effects is quite important because unmeasured, person-specific factors may be correlated with time in the U.S. and health insurance. For example, those more likely to return to Mexico may also choose jobs with high wages but no insurance. If so, the association between time in the U.S. and health insurance would be positive, all else equal, even if health insurance did not improve over time. By including the person-fixed effect, we eliminate this type of bias. Note that being conditioned on person fixed effects, these estimates are not representative of a random sample of immigrants.
Consider estimates of the change in health insurance status with an additional year in the U.S. for two groups: those in the US for 0 to 5 years and those in the US for 11 to 15 years. The types of immigrants in these two groups are likely to differ, for example, because of selective return migration with respect to health or earnings. Inclusion of person-specific fixed effects controls for these differences. Conditional on these fixed effects, we measure how health insurance changes with an additional year spent in the U.S. This approach yields estimates for the sample of immigrants who are present (i.e., have not exited sample) throughout the distribution of years since immigration. Theoretically, we cannot observe a difference in health insurance over longer periods, for example 10 years, without observing changes in health insurance between two years. Thus, the issue is not whether observing a person one additional year is a sufficiently long time, which it is, but whether there is sufficient statistical power to detect potentially small changes.
Estimates of the association between years since immigration and health insurance using the longitudinal data may differ from cross-sectional estimates due to: (i) differences in method (inclusion of person fixed effects); or (ii) differences in samples (matched longitudinal sample versus the entire cross-sectional sample). If cross-sectional estimates are approximately the same between the two samples then differences in estimates between the cross-sectional and longitudinal analyses will identify how compositional changes in the sample that are embedded in the cross sectional analysis, for example because of return migration, bias estimates of the association between time since arrival in the US and health insurance. We assess this by estimating cross-sectional models with both samples.5
To further investigate the potential bias due to return migration, we conduct the above analysis on a sample of immigrants born from outside of the Americas, who are known to have much lower return migration (Borjas and Bratsberg 1996, Van Hook et al. 2006). Because of low return migration estimates from longitudinal and cross-sectional analyses for this group should be relatively similar, and will help identify the significance of return migration bias in the Mexican sample. Immigrants born outside the Americas differ from Mexican immigrants in many ways, including educational attainment and labor market characteristics. To improve comparability we restrict the sample of immigrants born outside the Americas to those with a high-school or less education. In the longitudinal analysis we restrict samples to persons with a high-school or less education in year t-1.
Data
We used the March Current Population Survey from 1996 to 2008 and selected a sample of adults, aged 18–60, born in Mexico. The analysis is restricted to persons who arrived in 1970 or later because sample sizes are small for the pre-1970 arrivals. The sample size for the cross-sectional analysis is 64,250 men and women born in Mexico.
The March CPS provides information on the health insurance status last year of all persons including whether the person was covered by Medicaid, private insurance, employer-sponsored insurance in their own name, or some other type of public insurance.6 Information on individual characteristics such as age, gender, educational attainment, country of birth, and labor market outcomes including employment status, usual hours worked per week last year, and weeks worked last year, industry and occupation of employment last year, earnings last year, other family income last year (excluding own earnings), and self-reported health status are also included. Data on usual hours worked last year per week and weeks worked last year are used to compute a categorical variable indicating the following values: 0 hours and 0 weeks, 1–34 hours/week and 1–24 weeks, more than 34 hours/week and 25–47 weeks, and more than 34 hours/week and 48 or more weeks.
The CPS provides data on period of arrival at two to three years intervals for those who arrived in 1980 or later. For those who arrived during the 1970s, the period of arrival is provided in two categories: 1970–1974 and 1975–1979. As a result, it is not possible to calculate exact year of arrival for most immigrants. Using this information, we assign immigrants to the following years since arrival categories: 0–5 years, 6–10 years, 11–15 years, 16–20 years and 21–38 years. The state unemployment rate from the Bureau of Labor Statistics and per capita income from the Bureau of Economic Analysis are merged with the CPS data by state and year. The proportion of non-Hispanic U.S.-born whites lacking health insurance is calculated by age (18–32, 33–48, and 49–64 years categories), education (high-school or less and some college or higher), gender, state and year and merged with the sample of Mexican immigrants by the demographic categories noted.
The CPS interviews persons living within the same housing unit for four consecutive months, drops them from the survey for the next eight months, and re-enters them into the survey for the following four months. The data contains identifiers that can be used to match individuals in two consecutive years. Because the CPS sampling frame is residences and not people, we use additional characteristics such as age, sex, race/ethnicity, nativity, state of residence, whether the individual changed residence in the last one year, and period of arrival in the US to match individuals across years. We are able to match approximately 47% percent of the Mexican immigrant sample and the longitudinal analysis is based on 15,752 observations.7 The matching rate is somewhat higher for women than men.
The CPS has a few limitations that may affect our analyses. The data on year of arrival are based on the question: “In which year did the respondent move to the U.S. permanently.” Repeat migrants may interpret it variously: some may provide the year of first entry and others the year of last entry (Jasso, Rosensweig and Smith 2000). Arguably, the ideal measure would be one that counts only the time in the U.S., which for those that move back and forth is neither captured by the first reported date nor the last report date of arrival. Arguably it is the cumulative number of years in the U.S. and perhaps whether the years have been consecutive or interspersed that matters. Little can be done to address this problem in our data. Our findings have to be interpreted in light of it. The CPS also undercounts the Mexican population in the U.S. Passel (2005) has estimated that the CPS misses approximately 10 percent of the undocumented. This limitation afflicts most publicly available datasets and is perhaps less severe in the CPS that tries to cover the entire civilian non-institutional US population.
Results
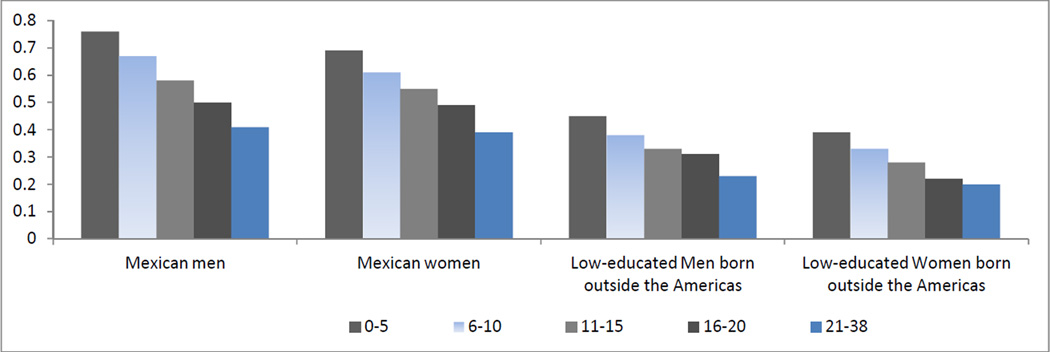
The proportion of uninsured Mexicans declines with years since immigration (Figure 1). For Mexican men, there is an18 percentage point (24%) decline in the proportion uninsured by 11 to 15 years after immigration and a 35 percentage point (46%) decline by 21 to 38 years after immigration. For Mexican women, the decline is 16 percentage points (23%) by 11 to 15 years after immigration and 30 percentage points (43%) by 21 to38 years after immigration. Immigrants born outside the Americas have a much lower proportion of uninsured, but they too experience an improvement in health insurance with time in the U.S.
Figure 1.
Association between Years since Immigration and Proportion Uninsured of Immigrants March CPS, 1996–2008
Table 1 presents estimates of the association between time in the U.S. and whether the respondent is without health insurance from regression analyses that adjust for several covariates. Model 1 controls for age, educational attainment, whether married, number of children under 18 in the household, state unemployment rate, state per capita income, and the proportion of US-born non-Hispanic white persons who are uninsured by age, education, sex, and state of residence and year of observation fixed effects. Model 2 includes additional controls for a number of labor market factors namely, hours worked and weeks worked last year and their interactions, industry and occupation of work last year, personal earnings, and family income (other than personal earnings) last year. Model 3 further adjusts for the citizenship status of the immigrant, and Model 4 includes additional controls for period of immigration (dummy variables indicating arrived during 1970–1979, 1980–1989, 1990–1999, and 2000–2008) and age at immigration (dummy variables indicating age at immigration intervals: <15, 15–22, 23–30,31–40 and >40 years). Finally, Model 5 adds controls for the health status of the respondent.
Table 1.
Estimates of the Association between Lack of Health Insurance and Years since Arrival in the US Mexican Immigrants, 1996−2008
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model/ | (1) | (2) | (3) | (4) | (5) | (1) | (2) | (3) | (4) | (5) |
| Panel 1: Cross-sectional sample |
||||||||||
| Years Since Arrival, 6−10 | −0.055*** (0.008) |
−0.045*** (0.007) |
−0.043*** (0.007) |
−0.033*** (0.009) |
−0.034*** (0.009) |
−0.062*** (0.009) |
−0.050*** (0.009) |
−0.048*** (0.009) |
−0.026*** (0.010) |
−0.027*** (0.010) |
| Years Since Arrival, 11−15 | −0.125*** (0.008) |
−0.105*** (0.008) |
−0.098*** (0.008) |
−0.078*** (0.012) |
−0.078*** (0.012) |
−0.111*** (0.009) |
−0.089*** (0.009) |
−0.083*** (0.009) |
−0.038*** (0.013) |
−0.039*** (0.013) |
| Years Since Arrival, 16−20 | −0.185*** (0.009) |
−0.159*** (0.009) |
−0.144*** (0.009) |
−0.111*** (0.016) |
−0.112*** (0.016) |
−0.173*** (0.010) |
−0.138*** (0.010) |
−0.124*** (0.010) |
−0.053*** (0.017) |
−0.055*** (0.017) |
| Years Since Arrival, 21−38 | −0.263*** (0.009) |
−0.218*** (0.009) |
−0.189*** (0.009) |
−0.124*** (0.020) |
−0.124*** (0.020) |
−0.261*** (0.009) |
−0.204*** (0.010) |
−0.172*** (0.010) |
−0.063*** (0.022) |
−0.064*** (0.022) |
| Number of Observations | 34688 | 34688 | 34688 | 34688 | 34688 | 29562 | 29562 | 29562 | 29562 | 29562 |
| Mean Uninsured for Reference Group (0−5 Years in US) |
0.76 | 0.76 | 0.76 | 0.76 | 0.76 | 0.69 | 0.69 | 0.69 | 0.69 | 0.69 |
| Panel 2:Matched sample | ||||||||||
| Years Since Arrival, 6−10 | −0.058*** (0.019) |
−0.050*** (0.019) |
−0.048** (0.019) |
−0.018 (0.022) |
−0.018 (0.022) |
−0.023 (0.019) |
−0.011 (0.019) |
−0.011 (0.019) |
0.011 (0.021) |
0.010 (0.021) |
| Years Since Arrival, 11−15 | −0.118*** (0.020) |
−0.095*** (0.019) |
−0.089*** (0.019) |
−0.032 (0.026) |
−0.033 (0.026) |
−0.086*** (0.020) |
−0.064*** (0.020) |
−0.061*** (0.019) |
−0.015 (0.026) |
−0.014 (0.026) |
| Years Since Arrival, 16−20 | −0.191*** (0.021) |
−0.171*** (0.021) |
−0.155*** (0.021) |
−0.070** (0.033) |
−0.071** (0.033) |
−0.145*** (0.021) |
−0.112*** (0.021) |
−0.096*** (0.021) |
−0.026 (0.033) |
−0.026 (0.033) |
| Years Since Arrival, 21−38 | −0.259*** (0.020) |
−0.215*** (0.020) |
−0.183*** (0.020) |
−0.049 (0.040) |
−0.049 (0.040) |
−0.240*** (0.020) |
−0.189*** (0.020) |
−0.151*** (0.020) |
−0.047 (0.041) |
−0.046 (0.041) |
| Number of Observations | 8044 | 8044 | 8044 | 8044 | 8044 | 7708 | 7708 | 7708 | 7708 | 7708 |
| Mean Uninsured for Reference Group (0−5 Years in US) |
0.71 | 0.71 | 0.71 | 0.71 | 0.71 | 0.63 | 0.63 | 0.63 | 0.63 | 0.63 |
| Model controls for: | ||||||||||
| Labor Market Factors | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Citizenship | No | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Period of and age at arrival | No | No | No | Yes | Yes | No | No | No | Yes | Yes |
| Health Status | No | No | No | No | Yes | No | No | No | No | Yes |
Notes: Figures in each column of panels 1 and 2 are based on a separate regression with whether uninsured as the dependent variable. In addition to the controls listed above, all models control for age (a dummy variable for each year of age), educational attainment (4 dummy variables indicating less than high-school, high-school, some college, and BA or higher education), whether married, number of children under 18 in the household, state of residence and year of observation fixed effects, state unemployment rate, per capita income, and the proportion of US-born non-Hispanic white persons who are uninsured by age, education, sex, state of residence, and year of observation. Heteroscedasticity adjusted standard errors are in parenthesis.
0.05 <p ≤ 0.1,
0.01 <p ≤ 0.05,
p ≤ 0.01.
For both men and women estimates from Model 1, panel 1, are similar to those indicated in Figure 1, but the decline in proportion uninsured over time is somewhat slower. Inclusion of labor market factors in Model 2 reduces (in absolute terms) the coefficients on the years-since-immigration categories suggesting that labor market assimilation has a mediating effect on the health insurance coverage and point estimates indicate the effect to be somewhat higher for women than men. Controlling for citizenship status (Model 3) further flattens the gradient. Overall, between 26 to 35 percent of the gain in health insurance by 21–38 years since immigration is attributable to economic and civic incorporation of Mexican immigrants.
Adding controls for the period of immigration and age at immigration variables (Model 4) dampens the gradient between years in US and the probability of being uninsured by a third for men and almost two thirds for women relative to estimates in Model 3. The strong mediating effect of age at arrival and period of arrival indicates that recent cohorts of Mexicans are more likely to be uninsured than earlier cohorts, and those who arrived at young ages are more likely to have health insurance than those who arrived at older ages. Indeed, estimated coefficients (not presented) in both men’s and women’s analyses show that compared to the 1970s arrival cohort, the 1980s, 1990s and 2000–2008 arrival cohorts had lower insurance rates. Mexican men and women who arrived at a young age (<15 years) were also more likely to be insured than those who arrived at older ages. The sensitivity of associations between time in the U.S. and proportion uninsured to the inclusion of controls for period and age of arrival is notable, and suggests that previous analyses that did not include these variables may have obtained substantially biased estimates. Interestingly, however, the inclusion of self-reported health (Model 5) has virtually no effect on the association between time in the U.S. and health insurance of Mexicans.8
Cross-sectional estimates (top panel) may be biased if return migration is selective on health insurance (or omitted factors that affect health insurance such as health, employment). To partly address this bias, we used longitudinal data consisting of a sample of Mexican immigrants observed in two consecutive years. But first, we assessed whether estimates from cross-sectional models are similar for the matched and larger samples (Panel 2). Cross-sectional estimates using the matched data were similar to those using the full sample for Models 1–3, but for Models 4–5, particularly in men’s analysis, estimates for the matched sample indicated a flatter gradient between years in US and probability of being uninsured. Overall, cross-sectional estimates for the matched and full samples are relatively similar.
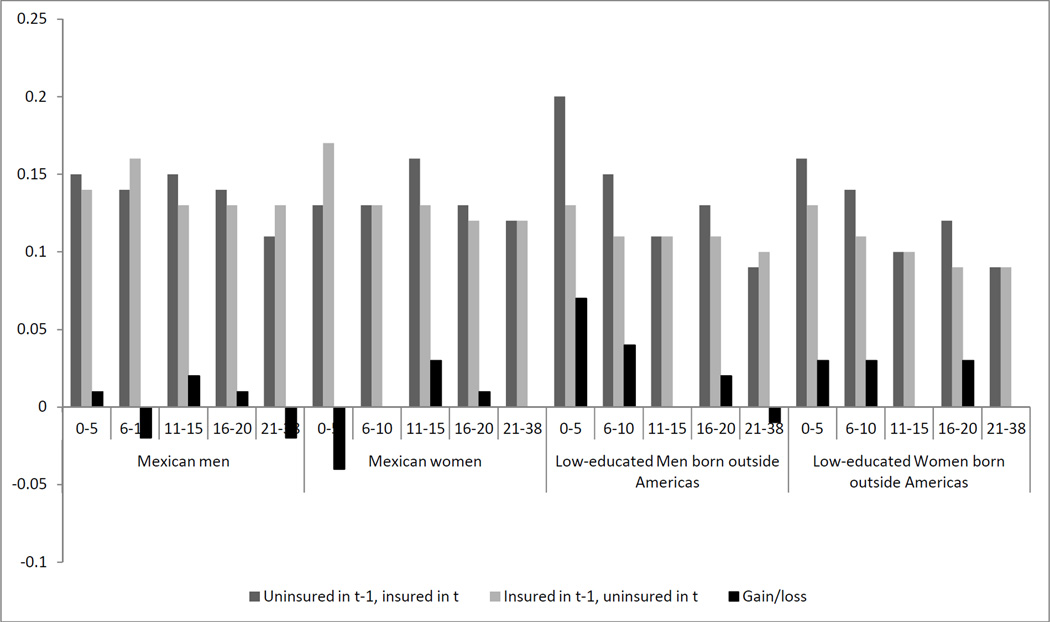
Descriptive evidence from the longitudinal data of changes in health insurance coverage between t-1 and t by years in the U.S. is presented in Figure 2. Among Mexican immigrant men, between 11 and 16 percent of the sample gains or loses health insurance each year, and the change does not differ by time in the U.S. Moreover, there is little evidence of a net gain in insurance coverage with increasing time since arrival. Instead, the pattern seems to be one of alternating (net) gains and losses. This descriptive evidence of no decline in probability of being uninsured with time in the US is at odds with the cross sectional evidence presented earlier. Approximately 12 to 17 percent of Mexican women also either gain or lose health insurance coverage each year. Here too, the descriptive evidence is inconsistent with the cross sectional estimates: year-to-year changes in health insurance coverage show a 5 percentage point decrease during the first 5 years in the U.S., followed by small increases or no net change in health insurance coverage over the next 33 years.
Figure 2.
Proportion Insured in Year t-1and Year t, by Years since Immigration (Based on matched CPS data)
Table 2 reports fixed effects regression estimates.9 The reported coefficients pertain to the interactions between years since immigration and whether the observation is taken from year t. None of the estimates is significant, although most estimates are negative indicating that another year spent in the US is associated with a decrease in the probability of being uninsured. The magnitudes of the fixed effects estimates are somewhat large relative to the cross sectional estimates, but not if measured relative to the year-to-year changes shown in Figure 2. There is a substantial amount of variation in year-to-year changes in health insurance and this variation makes it difficult to obtain precise estimates using the fixed effects method. Therefore, it is difficult to draw firm conclusions.
Table 2.
Estimates of the Association between Lack of Health Insurance Coverage and Years since Arrival in the US Matched Sample of Mexican Immigrants, 1996−2008 Fixed Effects Models
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (1) | (2) | (3) | (4) | |
| Years Since Arrival, 0−5 | −0.029 (0.037) | −0.026 (0.037) | −0.026 (0.037) | −0.029 (0.037) | 0.017 (0.036) | 0.022 (0.036) | 0.022 (0.036) | 0.017 (0.036) |
| Years Since Arrival, 6−10 | −0.002 (0.036) | −0.007 (0.036) | −0.007 (0.036) | −0.008 (0.036) | −0.010 (0.033) | −0.008 (0.033) | −0.008 (0.033) | −0.013 (0.033) |
| Years Since Arrival, 11−15 | −0.033 (0.035) | −0.035 (0.035) | −0.035 (0.035) | −0.036 (0.035) | −0.046 (0.035) | −0.044 (0.035) | −0.043 (0.035) | −0.049 (0.035) |
| Years Since Arrival, 16−20 | −0.025 (0.036) | −0.024 (0.036) | −0.025 (0.036) | −0.024 (0.036) | −0.034 (0.035) | −0.032 (0.035) | −0.031 (0.035) | −0.036 (0.035) |
| Years Since Arrival, 21−38 | −0.006 (0.032) | −0.007 (0.032) | −0.007 (0.032) | −0.010 (0.032) | −0.024 (0.032) | −0.023 (0.032) | −0.021 (0.032) | −0.025 (0.032) |
| Number of Observations | 8044 | 8037 | 8037 | 8037 | 7708 | 7699 | 7699 | 7699 |
| Mean Uninsured for 0−5 Years in US group | 0.71 | 0.71 | 0.71 | 0.71 | 0.63 | 0.63 | 0.63 | 0.63 |
| Labor Market Factors | No | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Citizenship | No | No | Yes | Yes | No | No | Yes | Yes |
| Health Status | No | No | No | Yes | No | No | No | Yes |
Note: Figures in each columnare based onseparate regressions with whether uninsured as dependent variable. The reported coefficients are interactions of years since arrival and whether the observation is from year t. All models include person-specific fixed effects. The variable years-since-arrival is measured in year t−1. In addition to the controls specified above, all models control for age (a dummy variable for each year of age), educational attainment, (4 dummy variables indicating less than high-school, high-school, some college, and BA or higher education), whether married, number of children under 18, year of observation fixed effects, state unemployment rate, per capita income, and the proportion of uninsured US-born non-Hispanic white persons by age, education, sex, state of residence, and year of observation. Heteroscedasticity adjusted standard errors are in parenthesis.
0.05 <p ≤ 0.1,
0.01 <p ≤ 0.05,
p ≤ 0.01.
Next, we study whether Mexican immigrant women’s participation in public health insurance increases with time in the US (Table 3). We study this outcome only for women because men are mostly ineligible for Medicaid. Cross-sectional analysis suggests a modest two percentage point increase in proportion with public health insurance in the first two to three decades after migration (Model 1). Adding controls for labor market factors (Model 2) steepens the gradient indicating that labor market advancement lowers the probability of receiving publicly financed health insurance. Citizenship status appears to have no effect on receipt of public health insurance (Model 3). Finally, inclusion of age at arrival and period of arrival controls results in almost flat public health insurance trajectories (Model 4). Further controlling for health status has no effect on the public health insurance trajectories of Mexican women (Model 5). Fixed effects estimates are statistically insignificant with no consistent pattern to the sign of the estimates. These results, largely consistent with the cross-sectional estimates, suggest little change in the receipt of public health insurance with time in US.
Table 3.
Estimates of the Association between Public Health Insurance Coverage and Years since Arrival in the US Cross-sectional Sample of Mexican Women Immigrants, 1996−2008
| Cross-sectional Model | Fixed effects Model | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (1) | (2) | (3) | (4) | |
| Years Since Arrival, 0−5 | Comparison category | −0.022 (0.024) | −0.022 (0.024) | −0.022 (0.024) | −0.020 (0.024) | ||||
| Years Since Arrival, 6−10 | 0.012** (0.006) | 0.019*** (0.006) | 0.019*** (0.006) | 0.014** (0.007) | 0.013* (0.007) | −0.009 (0.022) | −0.009 (0.022) | −0.009 (0.022) | −0.008 (0.022) |
| Years Since Arrival, 11−15 | 0.010 (0.006) | 0.023*** (0.006) | 0.022*** (0.006) | 0.010 (0.009) | 0.008 (0.009) | 0.033 (0.023) | 0.032 (0.023) | 0.032 (0.023) | 0.034 (0.023) |
| Years Since Arrival, 16−20 | 0.020*** (0.007) | 0.039*** (0.007) | 0.037*** (0.007) | 0.015 (0.012) | 0.013 (0.012) | 0.016 (0.023) | 0.016 (0.023) | 0.016 (0.023) | 0.018 (0.023) |
| Years Since Arrival, 21−38 | 0.021*** (0.006) | 0.050*** (0.007) | 0.046*** (0.007) | 0.004 (0.015) | 0.001 (0.015) | −0.022 (0.022) | −0.023 (0.022) | −0.023 (0.022) | −0.022 (0.022) |
| Number of Observations | 29562 | 29562 | 29562 | 29562 | 29562 | 7708 | 7699 | 7699 | 7699 |
| Mean Uninsured for those in the US for 0−5 Years | 0.10 | 0.10 | 0.10 | 0.10 | 0.10 | 0.12 | 0.12 | 0.12 | 0.12 |
| Labor Market Factors | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Citizenship | No | No | Yes | Yes | Yes | No | No | Yes | Yes |
| Age of Arrival, Period of Arrival | No | No | No | Yes | Yes | -- | -- | -- | -- |
| Health Status | No | No | No | No | Yes | No | No | No | Yes |
Analysis of Immigrants from Outside of Americas
To further assess the issue of return migration, we repeat some of the analyses using a sample of immigrants from outside of the Americas who have high-school or lower education. These immigrants have much lower rates of return migration and thus, the difference between cross-sectional and longitudinal (fixed effects) estimates should be smaller for this sample.
Cross sectional estimates (Table 4, Panels 1 and 2), based on the full and the matched samples, for both men and women, show a steady decline in proportion uninsured with time in the US. Labor market factors and citizenship status explain about a third of the gain in insurance. Inclusion of age at arrival and period of arrival flattens the health insurance trajectory considerably. Finally, health status has no effect on the health insurance trajectories of low-educated immigrants born outside the Americas.
Table 4.
Estimates of the Association between Lack of Health Insurance and Years since Arrival in the US Sample of Immigrants with high-school or lower education Born outside the Americas, 1996−2008
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model/ | (1) | (2) | (3) | (4) | (5) | (1) | (2) | (3) | (4) | (5) |
| Panel 1: Cross-sectional sample | ||||||||||
| Years Since Arrival, 6−10 | −0.059*** (0.015) |
−0.048*** (0.014) |
−0.043*** (0.015) |
−0.033* (0.017) |
−0.029* (0.017) |
−0.056*** (0.013) |
−0.048*** (0.013) |
−0.041*** (0.013) |
−0.033** (0.015) |
−0.031** (0.015) |
| Years Since Arrival, 11−15 | −0.090*** (0.015) |
−0.070*** (0.015) |
−0.058*** (0.015) |
−0.044** (0.021) |
−0.040* (0.021) |
−0.105*** (0.014) |
−0.089*** (0.014) |
−0.070*** (0.014) |
−0.060*** (0.020) |
−0.060*** (0.020) |
| Years Since Arrival, 16−20 | −0.107*** (0.016) |
−0.085*** (0.016) |
−0.069*** (0.016) |
−0.057** (0.027) |
−0.053* (0.027) |
−0.153*** (0.014) |
−0.133*** (0.014) |
−0.109*** (0.015) |
−0.102*** (0.025) |
−0.102*** (0.024) |
| Years Since Arrival, 21−38 | −0.162*** (0.014) |
−0.135*** (0.014) |
−0.114*** (0.015) |
−0.082** (0.034) |
−0.077** (0.034) |
−0.171*** (0.013) |
−0.145*** (0.013) |
−0.113*** (0.014) |
−0.092*** (0.031) |
−0.091*** (0.031) |
| Number of Observations | 10901 | 10901 | 10901 | 10901 | 10901 | 13030 | 13030 | 13030 | 13030 | 13030 |
| Mean Uninsured for Reference Group (0−5 Years in US) |
0.45 | 0.45 | 0.45 | 0.45 | 0.45 | 0.39 | 0.39 | 0.39 | 0.39 | 0.39 |
| Panel 2: Matched sample, OLS model | ||||||||||
| Years Since Arrival, 6−10 | −0.050* (0.026) |
−0.050* (0.026) |
−0.048* (0.026) |
−0.049* (0.029) |
−0.047 (0.029) |
−0.078*** (0.023) |
−0.071*** (0.022) |
−0.067*** (0.023) |
−0.050** (0.025) |
−0.047* (0.025) |
| Years Since Arrival, 11−15 | −0.105*** (0.026) |
−0.101*** (0.026) |
−0.096*** (0.027) |
−0.097*** (0.035) |
−0.095*** (0.035) |
−0.124*** (0.023) |
−0.113*** (0.023) |
−0.102*** (0.023) |
−0.082*** (0.030) |
−0.081*** (0.030) |
| Years Since Arrival, 16−20 | −0.129*** (0.027) |
−0.116*** (0.027) |
−0.108*** (0.028) |
−0.109** (0.044) |
−0.105** (0.044) |
−0.155*** (0.023) |
−0.137*** (0.023) |
−0.123*** (0.024) |
−0.113*** (0.037) |
−0.112*** (0.036) |
| Years Since Arrival, 21−38 | −0.170*** (0.024) |
−0.155*** (0.024) |
−0.144*** (0.026) |
−0.118** (0.054) |
−0.114** (0.054) |
−0.171*** (0.021) |
−0.150*** (0.021) |
−0.132*** (0.023) |
−0.076* (0.045) |
−0.074 (0.045) |
| Panel 3: Matched sample, fixed effects model | ||||||||||
| Years Since Arrival, 0−5 | −0.072 (0.047) |
−0.068 (0.047) |
−0.068 (0.047) |
−0.068 (0.047) |
-- | −0.001 (0.038) |
−0.000 (0.038) |
−0.000 (0.038) |
−0.001 (0.038) |
-- |
| Years Since Arrival, 6−10 | −0.040 (0.042) |
−0.029 (0.043) |
−0.030 (0.043) |
−0.030 (0.043) |
-- | −0.010 (0.035) |
−0.015 (0.035) |
−0.015 (0.035) |
−0.016 (0.035) |
-- |
| Years Since Arrival, 11−15 | −0.008 (0.045) |
0.001 (0.046) |
0.000 (0.046) |
0.003 (0.046) |
-- | 0.023 (0.036) |
0.019 (0.036) |
0.018 (0.036) |
0.018 (0.036) |
-- |
| Years Since Arrival, 16−20 | −0.027 (0.045) |
−0.030 (0.046) |
−0.032 (0.046) |
−0.031 (0.046) |
-- | 0.007 (0.037) |
0.005 (0.037) |
0.004 (0.037) |
0.003 (0.037) |
-- |
| Years Since Arrival, >20 | 0.013 (0.040) |
0.013 (0.041) |
0.012 (0.041) |
0.014 (0.041) |
-- | 0.021 (0.034) |
0.021 (0.034) |
0.021 (0.034) |
0.021 (0.034) |
-- |
| Number of Observations | 4026 | 4008 | 4008 | 4008 | 4008 | 5093 | 5093 | 5093 | 5093 | 5093 |
| Mean Uninsured for Reference Group (0−5 Years in US) |
0.35 | 0.35 | 0.35 | 0.35 | 0.35 | 0.35 | 0.35 | 0.35 | 0.35 | 0.35 |
Descriptive evidence on year-to-year changes in insurance status for the sample of immigrants from outside the Americas in Figure 2 shows that a 9 to 20 percent of the sample gains insurance and another 9–13 percent loses insurance each year. Overall, in the first 10 years after arrival on average five percent of men and three percent of women gained insurance each year; subsequent changes were modest. This descriptive evidence is consistent with the cross-sectional analyses in Table 4, particularly for men, and suggests a decline in the probability of being uninsured, although in Figure 2, the decline seems concentrated in the earlier years of arrival. Estimates from fixed effects models (Table 4, Panel 3) for the sample of immigrants from outside the Americas are statistically insignificant. However, the pattern is consistent with the descriptive evidence in Figure 2, specifically for men. Here too, the imprecision of the estimates makes it difficult to draw conclusions.
Conclusion
We examined how the health insurance coverage of Mexican immigrants changes with time in the U.S. Unadjusted cross-sectional trajectories show that about three decades of residency in the US is associated with a 35 percentage point gain in health insurance for Mexican men and a 30 percentage point gain in health insurance for Mexican women. Adjusting for age, marital status, and education, the gain in insurance over three decades is about 26 percentage points for both men and women. About a third (26% to 35%) of the gain could be attributed to civic and labor market incorporation of Mexican immigrants. However, much of the remaining relationship between time in the U.S. and health insurance coverage, after adjusting for demographic and labor market factors, is due to variation in age at arrival and period of arrival. Health status appears to be unrelated to gains in health insurance with time in the US.
Estimates from longitudinal analyses show virtually no systematic relationship between time in the U.S. and health insurance of Mexican immigrants, although the imprecision of the estimates makes it difficult to draw firm conclusions. We find that Mexican women’s propensity to get public health insurance rises modestly between 0–5 to 6–10 years of US residency, however, there is no further change in dependence on public health insurance with time in the US, refuting the commonly held belief that immigrant women become increasingly dependent on public health insurance with time in the US, and we find some evidence that Mexican immigrant women who do well in the labor market are less likely to use public health insurance.
The policy implication of these finding is that the labor market integration of Mexicans, a vast majority of whom are undocumented, is likely to improve their health insurance coverage and minimize their future dependence on public health insurance. The difference in our longitudinal and cross-sectional analyses affirms the presence of selective return migration of those who do not do well in the labor market. These results thus suggest that policies that restrict mobility of Mexicans, e.g. border controls, are likely to limit the labor market opportunities of those who do not do well in the US, which may in the long run create conditions for state dependence.
Acknowledgments
The authors thank Ce Shang for her excellent research assistance.
Footnotes
See Antecol and Bedard (2006), Cho et al. (2006), Dey and Lucas (2006), Harker (2001), Kandula et al. (2004), Landale et al. (1999), Lara et al. (2005), Palloni and Arias (2004), Rubacalva et al. (2008), Singh and Hiatt (2006), Singh and Siapush (2002), Stephen et al. (1994).
Health insurance may also exacerbate adoption of poor health behaviors because it lowers the cost of medical care that can treat behavioral-related changes in health (ex-ante moral hazard).
Economic theory suggests that health determines health insurance and health insurance may affect health via access to health care. Inclusion of health status rules out the later.
Our primary interest is in measuring changes in health insurance of Mexican immigrants, and not a comparison between Mexican immigrants and natives. Therefore, the native-born are not included. To check if their inclusion increased the precision of estimates, we estimated models including U.S.-born of Mexican origin, but the standard errors were not substantially smaller.
A comparison of cross-sectional and fixed effects estimates for the matched sample provides evidence of the importance of return migration, but only for this subsample of persons.
There is some question as to whether respondents are referring to last year or the current week/month when providing information about health insurance coverage.
The Hispanic oversample and SCHIP oversample are not included in matching. We were able to match 56% of the Mexican born sample for 1996–2000 and 43% for 2001–2007. Madrian and Lefgren (1999) reported matching 65 percent (native-born and foreign-born combined) persons in the 1980–1999 CPS. We were able to match 70 percent of the entire sample for 1996–2000, but matching declines from 2001 onwards. Van Hook et al. (2006) also found difficulties in matching immigrants across surveys in the post-2000 period.
Analyses with Logit models yielded similar results. For brevity and to facilitate comparison with fixed effects models we present only the OLS results.
The Breusch and Pagan Lagrangian multiplier test for random effects rejected the hypothesis that individual effects are uncorrelated with independent variables (Breusch and Pagan, 1979).
Contributor Information
Neeraj Kaushal, Columbia University School of Social Work, nk464@columbia.edu.
Robert Kaestner, Institute of Government and Public Affairs, University of Illinois at Chicago, kaestner@uic.edu.
References
- Antecol H, Bedard K. Unhealthy Assimilation: Do Immigrants Converge to American Health Status Levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Borjas G, Bratsberg B. Who Leaves? The Outmigration of the Foreign-born. The Review of Economics and Statistics. 1996;78(1):165–176. [Google Scholar]
- Borjas G, Katz S. The Evolution of Mexican-Born Workforce in the United States. In: Borjas G, editor. Mexican Immigration to the United States. Chicago: University of Chicago Press; 2007. [Google Scholar]
- Breusch TS, Pagan AR. Simple test for heteroscedasticity and random coefficient variation. Econometrica (The Econometric Society) 1979;47(5):1287–1294. [Google Scholar]
- Cho Y, Frisbie W, Hummer R, Rogers R. Nativity, Duration of Residence and the Health of Hispanic Adults in the United States. International Migration Review. 2006;38:184–211. [Google Scholar]
- Dey A, Lucas J. Physical and Mental Health Characteristics of U.S. Foreign-Born Adults: United States, 1998–2003. Advance Data. 2006 No.369. [PubMed] [Google Scholar]
- Duncan BV, Hotz J, Trejo SJ. Hispanics in the US Labor Market. In: Marta Tienda, Mitchell Faith., editors. Hispanics and the Future of America. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- Harker K. Immigrant Generation, Assimilation, and Adolescent Psychological Wellbeing. Social Forces. 2001;79(3):969–1004. [Google Scholar]
- Jasso G, Rosenzweig M, Smith JP. The Changing Skill of New Immigrants to the United States: Recent Trends and their Determinants. In: Borjas George., editor. Issues in the Economics of Immigration; A National Bureau of Economic Research Conference Report. The University of Chicago Press; 2000. [DOI] [PubMed] [Google Scholar]
- Jasso G, Massey D, Rosenzweig M, Smith J. Immigrant Health: Selectivity and Acculturation. In: Anderson Norman B, Bulatao Randy A, Cohen Barney., editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Kaestner R, Pearsonb J, Keene D, Geronimus A. Stress, Allostatic Load and Health of Mexican Immigrants. Social Science Quarterly. 2009;90(5):1089–1111. doi: 10.1111/j.1540-6237.2009.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandula NR, Kersey M, Lurie N. Assuring the Health of Immigrants: What the Leading Health Indicators Tell Us. Annual Review of Public Health. 2004;25:357–376. doi: 10.1146/annurev.publhealth.25.101802.123107. [DOI] [PubMed] [Google Scholar]
- Kaplan M, Marks G. Adverse Effects of Acculturation: Psychological Distress among Mexican American Young Adults. Social Science and Medicine. 1990;31:1313–1319. doi: 10.1016/0277-9536(90)90070-9. [DOI] [PubMed] [Google Scholar]
- Kaushal N. In-state Tuition for the Undocumented: Education Effects on Mexican Young Adults. Journal of Policy Analysis and Management. 2008;27(4):771–792. [Google Scholar]
- Landale NS, Oropesa RS, Llanes D, Gorman BK. Does Americanization Have Adverse Effects on Health? Stress, Health Habits, and Infant Health Outcomes Among Puerto Ricans. Social Forces. 1999;78:613–642. [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes D. Acculturation and Latino health in the United States: A Review of the Literature and its Sociopolitical Context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeClere Felicia B, Jensen Leif, Biddlecom Ann E. Health Care Utilization, Family Context, and Adaptation among Immigrants to the US. Journal of Health and Social Behavior. 1994;35(4):370–384. [PubMed] [Google Scholar]
- Madrian B, Lefgren LJ. NBER Technical Working Papers 0247. NBER.Inc.; 1999. A Note on Longitudinally Matching Current Population Survey Respondents. [Google Scholar]
- Mason KO, Mason WM, Winsborough HH, Poole WK. Some methodological issues in cohort analysis of archival data. American Sociological Review. 1973;38(2):242–258. [Google Scholar]
- Newhouse JP. Free for All? Lessons from the RAND Health Experiment. Cambridge, Mass: Harvard University Press; 1993. [Google Scholar]
- Palloni A, Arias E. Paradox Lost: Explaining the Hispanic Adult Mortality Advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Passel J, Cohn D. Mexican Immigrants: How Many Come? How Many Leave? Washington DC: Report, Pew Hispanic Center; 2009. [Google Scholar]
- Ramirez Roberto R. Census 2000 Special Report. U.S. Department of Commerce Economics and Statistics Administration, U.S. Census Bureau; 2004. We the People: Hispanics in the United States. [Google Scholar]
- Rubalcava LN, Teruel GM, Thomas D, Goldman N. Do healthier Mexicans migrate to the United States? New findings from the Mexican Family Life Survey. American Journal of Public Health. 2008;98:78–84. doi: 10.2105/AJPH.2006.098418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumbaut Ruben G. The Making of a People. In: Marta Tienda, Mitchell Faith., editors. Hispanics and the Future of America. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- Singh GK, Hiatt RA. Trends and Disparities in Socioeconomic and Behavioral Characteristics, Life Expectancy, and Cause-Specific Mortality of Native-Born and Foreign-Born Populations in the United States, 1979–2003. International Journal of Epidemiology. 2006;35(4):903–919. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M. Ethnic-Immigrant Differentials in Health Behaviors, Morbidity, and Cause-Specific Mortality in the United States: An Analysis of Two National Data Bases. Human Biology. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- Stephen E, Foote K, Hendershot G, Schoenborn C. Health of the Foreign-Born Population: United States, 1989–1990. Advance Data. 1994 No. 241. [PubMed] [Google Scholar]
- Thamer Mae Richard, Casebeer Christian, Waldman Adrianne, Nancy Fox Ray. Health insurance coverage among foreign-born US residents: The impact of race, ethnicity and length of residence. American Journal of Public Health. 1997;87:96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hook J, Passel J, Bean FD, Zhang W. Foreign-born Emigration: A New Approach and Estimates Based on Matched CPS Files. Demography. 2006;43(2):361–382. doi: 10.1353/dem.2006.0013. [DOI] [PubMed] [Google Scholar]
- Vega W, Amaro H. Latino outlook: Good health, uncertain prognosis. Annual Review of Public Health. 1994;15:39–67. doi: 10.1146/annurev.pu.15.050194.000351. [DOI] [PubMed] [Google Scholar]
- Wong R, Diaz JJ, Espinoza M. Health Care Use among Elderly Mexicans in the U.S. in Mexico: the role of health insurance. Research on Aging. 2006;28(3):393–408. doi: 10.1177/0164027505285922. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]