abstract
A vaccine against herpes zoster (HZ) and its complications has already proven safe and effective against infection and pain and against the related deterioration of quality of life in the elderly. In order to inform the vaccination decision-making process regarding inclusion of this vaccine in the French immunization schedule, we assessed the cost-effectiveness of several vaccination scenarios, compared to no vaccination. We chose to use a previously published Markov model. Starting vaccination in elderly individuals aged 65, 70 and 75 y old appears more cost-effective than vaccination for those aged 60 y old, with a cost-effectiveness ratio between 30,000 and 35,000 euros per quality-adjusted-life year (QALY) gained for the first 3 age groups versus 54,500 €; for the latter group. These results largely contributed to the recommendation to include the HZ vaccination in the French immunization schedule for people aged between 65 and 74 y old in France.
Keywords: cost-effectiveness, epidemiology, Herpes zoster, infectious disease, mathematical modeling, postherpetic neuralgia, vaccination, vaccine, vaccinology, viral
Introduction
Herpes zoster (HZ) is caused by a delayed painful local reactivation of infection by the virus causing chickenpox during childhood. The varicella-zoster-virus can remain dormant in the dorsal root ganglion.1 The main complication of HZ is post- herpetic neuralgia (PHN) defined as pain persisting over 90 d after rash onset.2 Severe pain and paresthesia are responsible for an important negative impact on patients’ quality of life at the onset of the acute phase and throughout the virus's evolution.3 Vaccination against HZ and PHN has proven effective against the disease (reduction of HZ and reduction of the severity if the disease does occur) and appears safe among the elderly.4 In order to inform the decision-making process regarding the introduction of systematic HZ vaccination for elderly French people, a study was conducted by the French Institute for public health surveillance (InVS) to determine whether vaccination was cost-effective and if so which age group(s) would be most appropriate to target. We chose to use a previously published Markov model.5
Results
Table 1 summarizes the main findings of our modeling study. Between 10,000 and 13,000 HZ cases were avoided through vaccination at 60, 65 and 70 y and fewer than 6,000 cases by vaccination at 75 y old. The number of PHN cases avoided by vaccination varied between 1,217 cases when vaccinating at 65 y and 2,366 cases when vaccinating at 70 y. Net estimated costs of the vaccination strategies were comparable for the 65 y old and older cohorts, varying between 35,090 and 38,883 k€. The vaccination strategy at 60 y old was more expensive costing 54,257 k€. The estimated cost-effectiveness (CE) ratio were relatively similar for the 65 y old and older cohorts, varying between 30,687 and 33,937 € per QALY (quality-adjusted life year) gained. The CE ratio was higher for the 60 y old vaccination strategy, costing 54,450 € per QALY gained (Table 2).
Table 1.
Base case results related to net costs and impact of vaccination in cohorts of French adults vaccinated at different age groups.
| Age groups (years) | 60-64* | 65-69** | 70-74** | 75-79** |
|---|---|---|---|---|
| Avoided HZ cases | 13,142 | 11,079 | 10,856 | 5,734 |
| Avoided PHN cases | 1,612 | 1,217 | 2,366 | 1,684 |
| Vaccination costs (€) | 54,256,596 | 35,090,691 | 38,883,296 | 37,683,737 |
| Net cost of vaccination per case of HZ avoided (€) | 4,128 | 3,167 | 3,582 | 6,572 |
* vaccine coverage: 50%,
**vaccine coverage: 60%
Table 2.
Base case incremental cost-effectiveness ratio of vaccination at different age groups compared with no vaccination, France.
| Age groups (years) | 60-64 | 65-69 | 70-74 | 75-79 |
|---|---|---|---|---|
| Cost per QALY gained (€) | 54,450 | 33,937 | 30,687 | 32,815 |
Figure 1 shows the results of the deterministic sensitivity analysis for the vaccination at 70 y of age. The most influential parameters were the duration of vaccination protection, and, to a lesser extent, the costs of vaccination, the utility estimates and HZ incidence. Similar conclusions were reached for the other cohorts considered.
Figure 1.
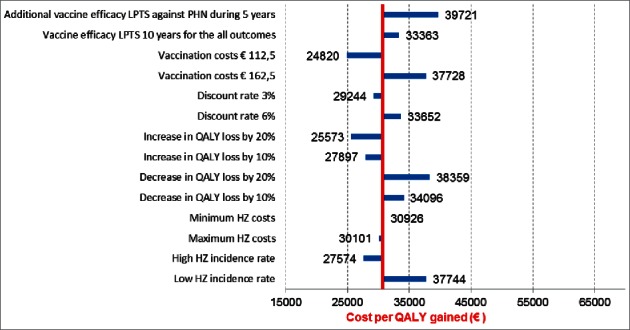
Deterministic sensitivity analysis: Herpes Zoster vaccination at 70 y old.
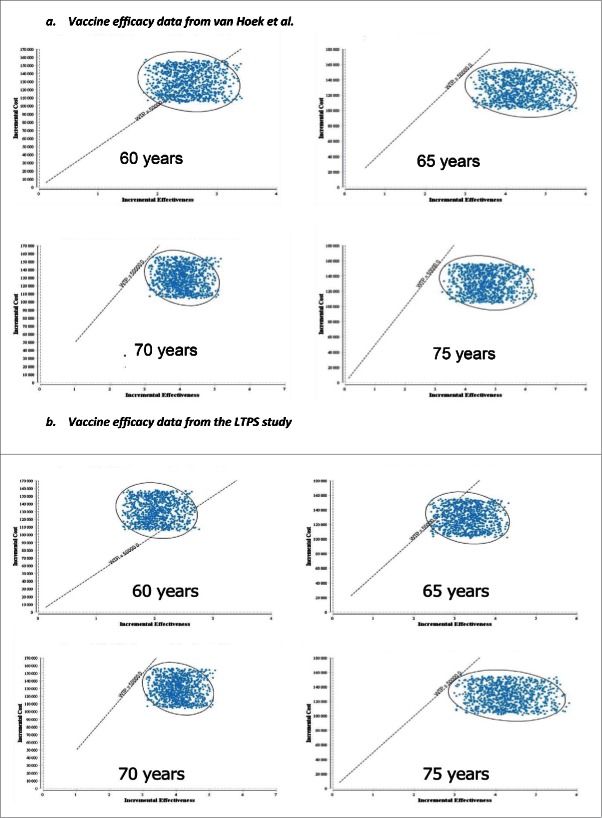
The probabilistic sensitivity analyses showed that respectively 66%, 100%, 100% and 100% of the CE ratio simulations were under the threshold of 50,000 € per QALY gained when vaccinating at age 60, 65, 70 and 75 y. When using the Long-Term Persistence Substudy (LTPS) duration of efficacy data,6 respectively 19%, 92%, 100% and 100% of the CE ratio simulations were under this threshold value (Fig. 2a and b). The corresponding results for a threshold of 30,000 € per QALY gained were respectively 0%, 57%, 50% and 64% (base case efficacy data) and 0%, 10%, 30% and 49% (LTPS efficacy data).
Figure 2.
Probabilistic sensitivity analysis: cost effectiveness for HZ vaccination at 60, 65, 70 and 75 y compared with no vaccination using vaccination efficacy.
Discussion
In the base case analysis, the CE ratio ranged from 30,687 € to 54,450 € per QALY gained. HZ vaccination in France appears more cost-effective when administered at 65, 70 and 75 y of age than when administered at 60 y of age.
The cost-effectiveness of HZ vaccination is most sensitive to duration of protection estimates. In the base case analysis, we assumed an average duration of protection of 9.5 y. This assumption of a persistent protection beyond 10 y post-vaccination is likely to have overestimated the real duration of protection, according to the recently published LTPS data. However, even in the alternative LTPS-data based probabilistic sensitivity analysis assuming no protection beyond 10 y after vaccination, the CE ratio remained below the threshold of 50,000 € per QALY gained in almost all simulations performed as part of the sensitivity analysis, when vaccination occurred at 65 y of age or beyond. Although there is no official CE ratio threshold for health interventions in France, as in most European countries, based on our results, HZ vaccination was considered reasonably cost-effective at 65 y of age or above.
We used the model built for the English/Welsh context but we re-parameterized it with French data. One of the limitations of our study is the absence of French data on QALY loss related to HZ. However we used the values estimated by Van Hoek et al., based on an extensive literature review.5 Another limitation is related to the estimation of the hospitalization rate. On the one hand it may have been overestimated as some patients may have been admitted several times for the same episode. On the other hand, it may have been underestimated by only considering ICD-10 code in the main diagnosis but not in other associated codes.
Bresse et al. in 20137also found that HZ vaccination in France was cost-effective for those vaccinated at 70 y old and over. They arrived at a lower CE ratio than ours (14,198 € per QALY gained vs. our 30,687 € per QALY gained from a societal perspective). Given that we essentially used the same French epidemiological data sources as Bresse et al.,8-10 this difference could be explained by the slightly different model structures and by different assumptions or parameters values for costs and vaccine effectiveness data. A recent article on the French burden of herpes zoster found hospital costs similar to those in our study.11
Our results are also consistent with those from other studies. A recent systematic review was conducted to assess the cost-effectiveness of routine varicella and herpes zoster vaccination in high-income countries by modeling studies. The majority of studies reviewed CE ratio or ICER (incremental cost-effectiveness ratio) from 10,000 to 40,000 € per QALY and concluded that HZ vaccination would indeed represent a cost-effective strategy.12
In those studies, when considering both a payer and a societal perspective, the differences in results between the 2 perspectives decreased with increasing age at vaccination, since indirect costs due to sick leave become less relevant with population aging.
The authors of the systematic review concluded that most results suggested that the optimal age for HZ vaccination is between 60 and 70 y or approximately 70 y. Conclusions about the cost-effectiveness of HZ vaccination depended mainly on the price of the vaccine, the duration of protection and the assumed cost-effectiveness threshold. Indeed, diverging results were essentially due to different choices regarding the duration of vaccine protection, HZ incidence and costs of vaccination.12,13
To our knowledge this is the first study to have used LTPS data. Interestingly, although LTPS results were less favorable than estimates used in previous studies in terms of duration of protection, vaccination against HZ for those 65-75 y old remains, in our study, reasonably cost-effective.
The results of this study were presented to the “Haut Conseil de la Santé Publique” (HCSP) which is responsible for making recommendations to the Ministry of Health when new vaccines are granted a licensing authorization. Taking into consideration our results as well as data on safety and effectiveness, in October 2013 the HCSP recommended zoster vaccination in people aged between 65 and 74 y old. Lack of data on vaccine effectiveness when administered above 75 y or older prevented us from estimating the cost-effectiveness for those age groups. However, the adopted vaccination strategy also included a one-year catch-up program for those aged 75 to 79 y,14 which was not based on an economical assessment.
This recommendation was endorsed by the Ministry of Health in 2015 and zoster vaccination has been included in the 2016 national immunization schedule for all individuals aged 65 to 74 y old, with a one-year catch-up for those aged 75-79 y old.
Methods (see Appendix)
A Markov cohort model already published by van Hoek et al.5 was reproduced to estimate the cost-effectiveness (CE) ratio of HZ vaccination in France compared to no vaccination. We used TreeAge Pro software to reproduce the Markov model developed by van Hoek et al. in which the patients are initially distributed in 4 health states no pain, mild pain, clinically relevant pain (CRP) divided in 2 groups acute herpes zoster (short term) and PHN which was defined as a CRP after 90 d. Different parameters were estimated for the initial distribution of the patients in the 4 health states and for the transition rate between these different health states. (Fig. A1).
The CE ratio of vaccination at different ages (60, 65, 70 or 75 years) were estimated and compared with the no-vaccination reference strategy. For each scenario defined by age at vaccination, the number of HZ and PHN cases prevented, as well as the net costs and the quality-adjusted life year (QALY) gained were calculated. According to the French guidelines, futures cost and effects were discounted at a 4% rate.15 We only considered a societal perspective (i.e. not the payer's perspective). Productivity costs were not included in the analysis.
Quality-adjusted life year (QALY)
In the absence of French data, we used the QALY loss estimates published by Hoek et al. They estimated the quality of life weight for each pain state from the literature by fitting a model to the data from the different published studies and combined those results with data on the duration of each state. Values used are shown in Fig. A2.
Model adaptation
Since the publication of van Hoek's article, several studies including 2 French studies9,10 have been published regarding the incidence of PHN. We have therefore adapted the van Hoek's model in order to fit the initial distribution of patients the 4 initial states: no pain, pain, short CRP, long CRP (PHN) to the results of the above mentioned French studies (Fig. A3 and Table A3). All individuals were followed in the model up to death or 104 y old, whatever event comes first. Zoster-specific mortality was neglected.
Vaccine efficacy
In the base-case analysis, we used the vaccine efficacy and waning rate as estimated by van Hoek et al. by fitting a model to clinical trial data. Efficacy was assumed to decline at a constant rate with time since vaccination. However, the likelihood function obtained was fairly flat in the region of the maximum, therefore several combinations of efficacy and waning rate were supported by the data. We chose in the base case analysis the values provided in Table A1, corresponding to an average duration of protection of 9.5 years, as they were those with the best graphical fit with the year by year Long term Prevention Study (LTPS) data (Fig. A4). Indeed, during our analysis, data on long-term (10 years) vaccine efficacy yielded by the LTPS were made available to us through the French Regulatory Agency, prior to their publication in 2015.6 Based on the result of the pivotal clinical trial, we also assumed an additional vaccine efficacy against PHN in the 70 y and over age groups (corresponding to a reduction of the morbidity associated with HZ infection in the vaccinated). We used data from the LTPS study for the immediate and annual decrease of the additional efficacy of the vaccine against PHN (Table A2).
Incidence data
French demographic data and mortality rates were obtained from the National Institute for Statistics and Economics studies (Insee). Age specific incidence rates of HZ (cases per 100,000 inhabitants) were obtained from the General Practitioners (GP) sentinel network surveillance system.8 Hospitalization data were computed from the national hospital discharge database (“Programme de médicalisation des systems d’information” (PMSI)) using ICD-10 codes B020-29 as the main diagnosis (Table A3).
Cost data
Hospitalization costs were obtained by multiplying daily inpatients costs for an HZ and a PHN episode by the average number of days spent in hospital, calculated from the PMSI data. Costs of an HZ and a PHN episode in primary care were derived from the French study EPIZOD.8 All costs were presented in 2012 Euros (€). Costs from the previous year were inflated to their 2012 value (Table A3).
Vaccination costs (137.5 €) included the cost of one dose (125 € in the base case analysis) and half the cost of one GP visit (12.5 €) as we assumed that only half of the vaccinations would require an extra medical consultation. In the sensitivity analysis, alternative costs were used for the vaccine, varying between 112.5 and 162.5 €. Costs and utilities were discounted by 4% per year in line with official French guidelines.15
Sensitivity analyses
Deterministic sensitivity analyses were performed on vaccine costs, disease costs, utilities, HZ incidence, discount rate, vaccine effectiveness and duration of protection as these were the parameters with the greatest impact on the results. Hypothesis made for the efficacy and duration of protection and ranges considered for the various parameters are given in Fig. 1 and Table A3. Probabilistic sensitivity analyses were also performed on those same parameters using uniform distributions. The same ranges as considered in deterministic sensitivity analysis were used. We run the probabilistic sensitivity analysis separately for 2 scenarios regarding duration of protection: one with data on the duration of protection from the base case analysis, one with data derived from the LTPS study for all outcomes (efficacy against HZ and additional efficacy against PHN) (Table A2). One thousand simulations were run for each of the 2 scenarios.
Supplementary Material
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
We would like to thank Dr. AJ van Hoek who kindly replied to all our questions about his model.
References
- [1]. Hope-Simpson RE. The nature of herpes zoster: a long-term study and a new hypothesis. Proc R Soc Med 1965; 58:9-20; PMID:14267505 [PMC free article] [PubMed] [Google Scholar]
- [2]. Hope-Simpson RE. Postherpetic neuralgia. J R Coll Gen Pract 1975; 25(157):571-5; PMID:1195231 [PMC free article] [PubMed] [Google Scholar]
- [3]. Dworkin RH, Portenoy RK. Pain and its persistence in herpes zoster. Pain 1996; 67(2-3):241-51; PMID:8951917; http://dx.doi.org/ 10.1016/0304-3959(96)03122-3 [DOI] [PubMed] [Google Scholar]
- [4]. Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, Arbeit RD, Simberkoff MS, Gershon AA, Davis LE, et al. . A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 2005; 352(22):2271-84; PMID:15930418; http://dx.doi.org/ 10.1056/NEJMoa051016 [DOI] [PubMed] [Google Scholar]
- [5]. van Hoek AJ, Gay N, Melegaro A, Opstelten W, Edmunds WJ. Estimating the cost-effectiveness of vaccination against herpes zoster in England and Wales. Vaccine 2009; 27(9):1454-67; PMID:19135492; http://dx.doi.org/ 10.1016/j.vaccine.2008.12.024 [DOI] [PubMed] [Google Scholar]
- [6]. Morrison VA, Johnson GR, Schmader KE, Levin MJ, Zhang JH, Looney DJ, Betts R, Gelb L, Guatelli JC, Harbecke R, et al. . Long-term persistence of zoster vaccine efficacy. Clin Infect Dis 2015; 60(6):900-9; PMID:25416754; http://dx.doi.org/ 10.1093/cid/ciu918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Bresse X, Annemans L, Preaud E, Bloch K, Duru G, Gauthier A. Vaccination against herpes zoster and postherpetic neuralgia in France: a cost-effectiveness analysis. Expert Rev Pharmacoecon Outcomes Res 2013; 13(3):393-406; PMID:23537397; http://dx.doi.org/ 10.1586/erp.13.19 [DOI] [PubMed] [Google Scholar]
- [8]. Gonzalez Chiappe S, Sarazin M, Turbelin C, Lasserre A, Pelat C, Bonmarin I, Chosidow O, Blanchon T, Hanslik T. Herpes zoster: burden of disease in France. Vaccine 2010; 28(50):7933-8; PMID:20946861; http://dx.doi.org/ 10.1016/j.vaccine.2010.09.074 [DOI] [PubMed] [Google Scholar]
- [9]. Mick G, Gallais JL, Simon F, Pinchinat S, Bloch K, Beillat M, Serradell L, Derrough T. [Burden of herpes zoster and postherpetic neuralgia: Incidence, proportion, and associated costs in the French population aged 50 or over]. Rev Epidemiol Sante Publique 2010; 58(6):393-401; PMID:21094001; http://dx.doi.org/ 10.1016/j.respe.2010.06.166 [DOI] [PubMed] [Google Scholar]
- [10]. Bouhassira D, Chassany O, Gaillat J, Hanslik T, Launay O, Mann C, Rabaud C, Rogeaux O, Strady C. Patient perspective on herpes zoster and its complications: an observational prospective study in patients aged over 50 years in general practice. Pain 2012; 153(2):342-9; PMID:22138256; http://dx.doi.org/ 10.1016/j.pain.2011.10.026 [DOI] [PubMed] [Google Scholar]
- [11]. Blein C, Gavazzi G, Paccalin M, Baptiste C, Berrut G, Vainchtock A. Burden of herpes zoster: the direct and comorbidity costs of herpes zoster events in hospitalized patients over 50 years in France. BMC Infect Dis 2015; 15(1):350; PMID:26286598; http://dx.doi.org/ 10.1186/s12879-015-1059-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Damm O, Ultsch B, Horn J, Mikolajczyk RT, Greiner W, Wichmann O. Systematic review of models assessing the economic value of routine varicella and herpes zoster vaccination in high-income countries. BMC Public Health 2015; 15:533; PMID:26041469; http://dx.doi.org/ 10.1186/s12889-015-1861-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Kawai K, Preaud E, Baron-Papillon F, Largeron N, Acosta CJ. Cost-effectiveness of vaccination against herpes zoster and postherpetic neuralgia: a critical review. Vaccine 2014; 32(15):1645-53; PMID:24534737; http://dx.doi.org/ 10.1016/j.vaccine.2014.01.058 [DOI] [PubMed] [Google Scholar]
- [14]. Haut Conseil de la Santé Publique Vaccination des adultes contre le zona: place du vaccin Zostavax® [Internet]. Paris: Haut Conseil de la Santé Publique, 2013. 10/25/2013. [Google Scholar]
- [15]. Haute Autorité de Santé Choix méthodologiques pour l’évaluation économique à la HAS. Saint-Denis La Plaine: Haute Autorité de Santé, 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.