Abstract
Objective:
To determine incidence, risk factors, and outcome of acute kidney injury (AKI) in Pediatric Intensive Care Unit (PICU).
Materials and Methods:
This is a prospective, observational study conducted in PICU of Department of Paediatrics, S.P. Medical College, Bikaner, from October 2013 to May 2014. In this study, 536 patients of aged 29 days to 16 years were screened for AKI according to the Pediatric Risk, Injury, Failure, Loss, End-stage Renal Disease (pRIFLE) criteria. Their clinical and biochemical data were recorded and followed up to their discharge/death.
Results:
During the study period, 230 (42.9%) out of 536 patients developed AKI. Younger age (<5 years) and females (P ≤ 0.013) were more prone to develop AKI. Most common etiologies were septicemia, multiple organ dysfunction syndrome (MODS), gastroenteritis, and severe malaria (P ≤ 0.05). The maximal stage of AKI was stage “R” (49.1%), followed by “I” (29.5%) and “F” (21.3%). Major PICU-related risk factors were use of vasoactive drug (VD) and nephrotoxic drug (ND) and need of mechanical ventilation (MV) (P ≤ 0.05). Length of stay was significantly longer than non-AKI patients (P ≤ 0.05). Mortality in AKI (47.5%) was higher (P ≤ 0.05%) in comparison to non-AKI (25.56%).
Conclusion:
AKI is common in critically sick children, especially in younger age and in females with septicemia and MODS. Use of VD and ND and need of MV are common risk factors. AKI is associated with longer hospital stay and higher mortality. pRIFLE is better diagnostic criteria in early detection of AKI and reduction of their morbidity and mortality.
Keywords: Acute kidney injury, critically ill children, Pediatric Intensive Care Unit, pRIFLE
Introduction
Acute kidney injury (AKI) is one of the most common conditions seen in the Pediatric Intensive Care Unit (PICU) setup. We come across AKI in patients on admission to the PICU initially or as a complication during the course. Studies show that AKI is independently associated with poor outcome.[1] Much of the available data on clinical course of patients with AKI is from western literature. Compared to that, reports from our country are scanty.[2] However, incidence and risk factors of AKI in our country may be different from western countries, so there is a need to study the most common diseases/conditions causing AKI which can help in detecting the AKI at the earliest and in developing strategies for prevention and treatment of AKI.
0by25, a global initiative with a strong emphasis on developing countries in Africa, Asia, aims to eliminate preventable deaths from AKI worldwide by 2025. To achieve this ambitious goal, the mission is to call for globally applicable strategies that permit timely diagnosis and treatment of AKI for patients with potentially reversible diseases. AKI is often preventable and treatable with few, if any, long-term health consequences. However, the lack of early identification and treatment in many countries means that patients often do not receive essential care before it is too late. We need to identify people who are at risk, monitor them appropriately, diagnose the problem early, and provide reliable and consistent treatment to everyone.
Most studies were based on retrospective analysis of records,[3,4] which may distort the results, so we aimed to prospectively determine the incidence, risk factors, and outcome of AKI in children admitted to the PICU.
Materials and Methods
The prospective, observational study was carried out on consecutive patients between the age of 29 days to 16 years, of either sex, admitted to the PICU between October 2013 to May 2014 and staying for >24 h.
The study was approved by the Institutional Ethical Committee. Following informed parental consent, data regarding baseline characteristics, admission diagnosis, degree of kidney injury, length of stay, and outcome were noted.
Serum creatinine was analyzed daily with Jaffe method and estimated creatinine clearance (eCC) was calculated according to Schwartz formula. The patients, who were admitted with missing baseline renal function data, normal renal clearance value of 100 ml/min/1.73 m2 was considered as reference, as proposed by Akcan-Arikan et al.
Patients were classified as AKI cases if AKI was diagnosed based on Pediatric Risk, Injury, Failure, Loss, End-stage Renal Disease (pRIFLE) criteria either at admission or subsequently during the hospital stay; patients who did not develop AKI were served as controls. We used both urine output and eCC criteria of pRIFLE, and maximum pRIFLE stage reached during PICU stay was recorded.
Exclusion criteria
patients with previous renal diseases and staying for <24 h were excluded from the study.
Statistics
Incidence of AKI cases was determined as the number of AKI cases per 100 patients. SPSS version 22 (Armonk NY, IBM Company) was used for statistical calculation. Risk factors of AKI were examined using Cox proportional hazard analysis and reported as hazard ratio (95% confidence interval). Results were considered significant if two-sided P < 0.05.
Results
Of 603 patients screened, 67 were excluded (19–CKD, 48–<24 h stay). Of remaining 536 patients, 230 patients (42.9%) patients developed AKI (as defined by modified pRIFLE criteria).
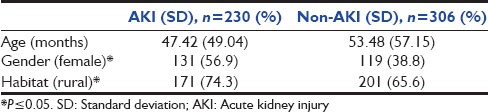
Patients were classified into two groups: AKI and non-AKI, and baseline characteristics in both groups are compared as shown in Table 1.
Table 1.
Comparison of baseline characteristics of patients in the acute kidney injury and nonacute kidney injury groups
Onset of acute kidney injury
Out of 230 AKI patients, 115 (50%) patients had AKI at admission while 40.4% developed within 72 h.
Clinical course of acute kidney injury
Of the 230 patients classified as AKI by modified pRIFLE criteria, 113 (49.1%) patients reached pRIFLE max of risk, 68 (29.5%) patients reached injury, and 49 (21.3%) patients had failure.
Clinical features
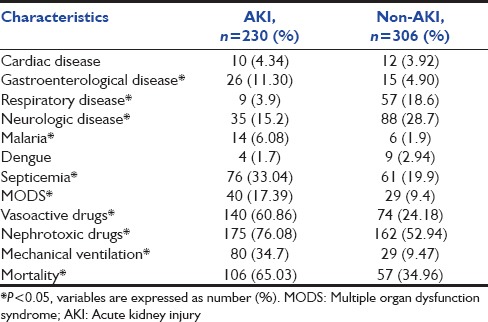
Septicemia, multiple organ dysfunction syndrome (MODS), nephrotoxic drugs (NDs) usage, vasopressor support, and mechanical ventilation (MV) were significantly associated with development of AKI [Table 2].
Table 2.
Characteristics of patients with and without acute kidney injury
Risk factors of acute kidney injury
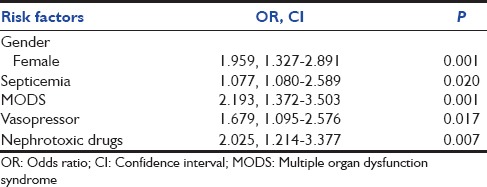
In multivariate analysis, only gender, septicemia, MODS, NDs usage, and vasopressor support were found to be independent risk factors of AKI [Table 3].
Table 3.
Independent risk factors of acute kidney injury (multivariate regression analysis)
Pediatric Intensive Care Unit and hospital stay
The median duration of PICU and hospital stay was 4.75 ± 1.99, 9.15 ± 3.11 and 3.75 ± 2.06, 6.63 ± 2.38 in AKI and non-AKI groups, respectively (P < 0.001).
Outcome
The overall mortality in studied patients was 30.41% (163/536). Crude mortality in AKI patients was 46.03% (106/230) whereas that in the non-AKI group was 18.62% (57/306), which was significantly higher (P < 0.0001). When mortality was compared between different classes, there was progressive and significant increase in the mortality rate associated with increasing pRIFLE class, i.e., 31.19% for risk, 53.03% for injury, and 77.08% for failure patients (P = 0.00001).
Discussion
AKI in intensive care setup in children is a significant complication which further aggravates the already high case fatality rate and adds another dimension to the clinical profile and management. Our study was single-center, prospective, observational study with the objective to determine the incidence and risk factors of AKI and classify patients with AKI using pRIFLE criteria. We found that female gender, septicemia, MODS, vasopressor support, and exposure to NDs were the independent risk factors. Patients with AKI also associated with longer PICU and hospital stay and poor outcome in terms of mortality.
Several studies from India and abroad showed variable incidence ranging from 25.1% to 82% depending on various inclusion criteria and profile of patients admitted to the PICU.[2,5,6,7,8,9] A study conducted by Mehta et al. showed 38.1% incidence of AKI in PICU while Krishnamurthy et al. and Soler et al. found incidence of 25.1% and 27.4%, respectively, which is somewhat lower than our study.[2,9,10] Plötz et al. and Akcan-Arikan et al. showed very high incidence of 58% and 82%, respectively.[1,6] The reported difference in incidence of AKI in different studies could be due to different study population and/or PICU environment.
In our study, 90% of patients developed AKI within 72 h of PICU stay. Keniamachado and Plötz et al. identified 36.2% and 45% of AKI on day first of admission, respectively, in comparison to our study in which 50% had AKI on admission.[1,8] Akcan-Arikan also identified that AKI was either present on admission or does develop early in the course of intensive care emphasizing the importance of early diagnosis of AKI.[6]
Severity grading of AKI cases according to pRIFLE criteria showed that 49.1%, 29.5%, and 21.3% patients were in “R” category, “I” category, and “F” category, respectively, in this study. In a study by Mehta et al., maximum cases of AKI had Stage 1 (65.8%), followed by Stage 2 (17.8%) and Stage 3 (16.4%).[2] Similar pattern of AKI level (R, I, F) was reported by Akcan-Arikan et al., i.e., 48.8%, 26%, 25.2%, and Plötz et al., i.e., 52%, 37%, 11%, respectively.[1,6] Recently, Naik et al. described 37.9% patients had risk, followed by 35.9% and 26.2% had injury and failure categories, respectively.[11]
Various studies have identified risk factors of AKI. Mehta et al. found that younger age, shock, sepsis, and need for MV were independent risk factors for AKI in their study.[2] Krishnamurthy et al. described that regarding factors such as MV, vasoactive drugs requirement, and exposure to NDs, exposed patients had increased risk of renal injury.[9] Naik et al. identified lower age, cardiac diseases, and shock as most important risk factors of AKI.[11]
Keniamachado et al., Mehta et al., and Akcan-Arikan et al. also reported longer PICU and hospital stay in AKI patients.[2,6,8]
Regarding mortality, several studies have clearly shown that any degree of AKI is a poor prognosis indicator for critically all patients. According to Mehta et al. and Krishnamurthy et al., mortality in AKI was 37% and 46.3%, respectively.[2,9] Mehta et al. found that AKI was not independent predictor of mortality in multivariate analysis.[2] Increased mortality in AKI is because patients with AKI are more sick with multiorgan failure.
The present study has some limitations. First, it is a single-center study, so it would be necessary to confirm the incidence from other centers also. Neonates were not included in this study since their susceptibility to AKI is different and risk factors were also different. The predictors for mortality were not identified in this study. Long-term follow-up was not done. Further studies are required to compare AKIN and pRIFLE criteria, in order to determine which is better for early identification and outcome prediction.
Conclusion
This prospective study is to address the current lack of data over burden of AKI in sick children. Higher incidence of AKI was seen in female gender, and patients with septicemia, with MODS, require MV, on vasopressor support, and exposed to NDs. These risk factors support in early identification of AKI. The presence of AKI is associated with longer PICU and hospital stay, with higher mortality imposing the significant burden to healthcare system. AKI should no longer be a death sentence for these people. Nobody should die of preventable and treatable AKI by 2025 (as per the 0by25 initiative). We should raise awareness of AKI across the global health-care community including health-care professionals, among public health institutions and the private sector.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Plötz FB, Hulst HE, Twisk JW, Bökenkamp A, Markhorst DG, van Wijk JA. Effect of acute renal failure on outcome in children with severe septic shock. Pediatr Nephrol. 2005;20:1177–81. doi: 10.1007/s00467-005-1946-1. [DOI] [PubMed] [Google Scholar]
- 2.Mehta P, Sinha A, Sami A, Hari P, Kalaivani M, Gulati A, et al. Incidence of acute kidney injury in hospitalized children. Indian Pediatr. 2012;49:537–42. doi: 10.1007/s13312-012-0121-6. [DOI] [PubMed] [Google Scholar]
- 3.Palmieri T, Lavrentieva A, Greenhalgh D. An assessment of acute kidney injury with modified RIFLE criteria in pediatric patients with severe burns. Intensive Care Med. 2009;35:2125–9. doi: 10.1007/s00134-009-1638-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schneider J, Khemani R, Grushkin C, Bart R. Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med. 2010;38:933–9. doi: 10.1097/CCM.0b013e3181cd12e1. [DOI] [PubMed] [Google Scholar]
- 5.Ostermann M, Chang RW. Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med. 2007;35:1837–43. doi: 10.1097/01.CCM.0000277041.13090.0A. [DOI] [PubMed] [Google Scholar]
- 6.Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71:1028–35. doi: 10.1038/sj.ki.5002231. [DOI] [PubMed] [Google Scholar]
- 7.Bagshaw SM, George C, Dinu I, Bellomo R. A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23:1203–10. doi: 10.1093/ndt/gfm744. [DOI] [PubMed] [Google Scholar]
- 8.Freire KM, Bresolin NL, Farah AC, Carvalho FL, Góes JE. Acute kidney injury in children: Incidence and prognostic factors in critical ill patients. Rev Bras Ter Intensiva. 2010;22:166–74. [PubMed] [Google Scholar]
- 9.Krishnamurthy S, Mondal N, Narayanan P, Biswal N, Srinivasan S, Soundravally R. Incidence and etiology of acute kidney injury in Southern India. Indian J Pediatr. 2013;80:183–9. doi: 10.1007/s12098-012-0791-z. [DOI] [PubMed] [Google Scholar]
- 10.Soler YA, Nieves-Plaza M, Prieto M, García-De Jesús R, Suárez-Rivera M. Pediatric risk, injury, failure, loss, end-stage renal disease score identifies acute kidney injury and predicts mortality in critically ill children: A prospective study. Pediatr Crit Care Med. 2013;14:e189–95. doi: 10.1097/PCC.0b013e3182745675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naik S, Sharma J, Yengkom R, Kalrao V, Mulay A. Acute kidney injury in critically ill children: Risk factors and outcomes. Indian J Crit Care Med. 2014;18:129–33. doi: 10.4103/0972-5229.128701. [DOI] [PMC free article] [PubMed] [Google Scholar]


