Abstract
Hantavirus infection, a rare disease diagnosed in India and carries a very high mortality. There are no reports of this infection in association with pregnancy or postpartum period in our country. We present a case of a 30-year-old female diagnosed to have hantavirus pulmonary syndrome in the postpartum period. We intend to create awareness about this infection and consider it in the differential diagnosis of patients presenting with acute respiratory distress syndrome and multiorgan dysfunction in association with pregnancy and postpartum period.
Keywords: Acute respiratory distress syndrome, hantavirus pulmonary syndrome, postpartum
Introduction
Hantaviruses are described as emerging pathogens as newer serotypes are being discovered in many areas nonendemic to hantaviruses.[1] Hantaviruses are the most widely distributed zoonotic rodent-borne viruses and can cause two important clinical syndromes: hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary syndrome (HPS) in Asia and America, respectively.[2]
Humans are accidental hosts and get infected by aerosols generated from contaminated urine, feces, and saliva of infected rodents. Rodents are the natural hosts of these viruses and develop persistent infection. Human-to-human infections are rare, and the evolution of the virus depends largely on that of the rodent host. HPS is characterized by severe noncardiogenic pulmonary edema resulting in respiratory compromise often resembling acute respiratory distress syndrome (ARDS). The case fatality rate of HPS is about 45%.[3]
Very few cases of HPS have been reported in association with pregnancy in the world, none in India; we present a case of HPS in the postpartum period.
Case Report
A 30-year-old female developed severe pain in abdomen, fever, and giddiness 8 days, following full-term normal vaginal delivery. Her antepartum and peripartum course were uneventful. She was admitted to a private nursing home for the above symptoms. They noted gaping of her episiotomy wound and resuturing was done. She was also evaluated for fever and was found to have a platelet count of 50,000/cumm. The next day, she had a worsening fever, started developing breathlessness, and was found to be hypotensive. She was conservatively managed and was shifted to our hospital in view of worsening of above-mentioned symptoms.
On admission to our hospital, she was found to be severely tachypneic, had severe hypotension needing inotropic supports. She was intubated and mechanically ventilated. On evaluation, she had a platelet count of 40,000/cumm, deranged liver function tests, and a creatinine of 4.1 mg/dl. She also had coagulopathy with international normalized ratio of 4.3. Her chest X-ray showed bilateral chest infiltrates [Figure 1], arterial blood gas showed a PaO2/FiO2 of <100 suggesting severe ARDS [Table 1]. Ultrasonography abdomen and pelvis and two-dimensional echocardiography were normal. With a provisional diagnosis of acute febrile illness with severe sepsis and septic shock, further evaluation to find out the etiology was done. Polymerase chain reaction for leptospira and dengue IgM was negative; malaria smear showed no parasites. However, IgM antibodies for hantavirus were tested positive.
Figure 1.
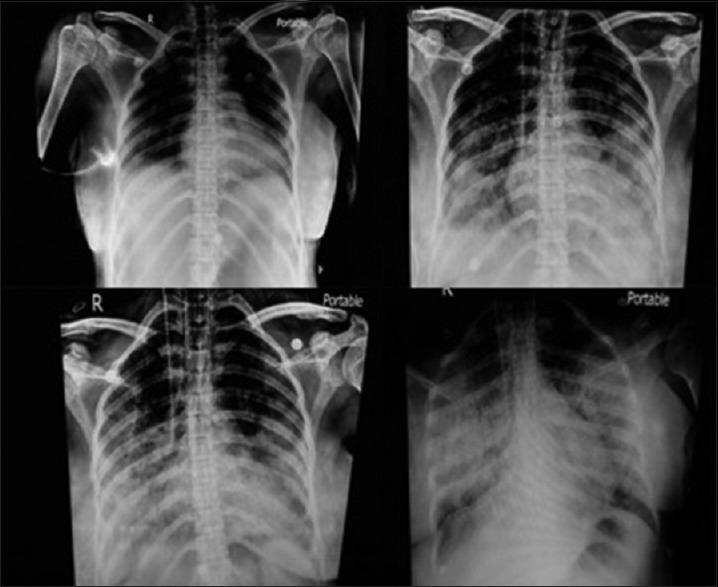
Serial X-rays showing progressive worsening of lung shadows
Table 1.
Serial laboratory values
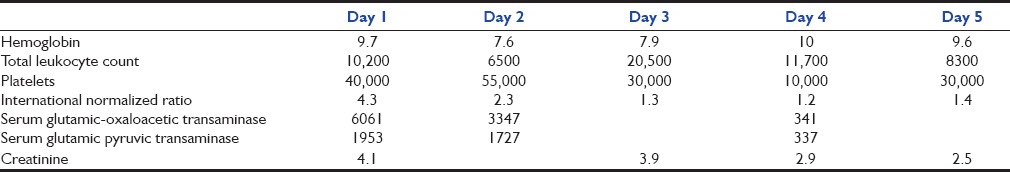
During her course in the Intensive Care Unit, she had a falling platelet count and coagulopathy needing blood component transfusion, severe ARDs needing lung protective ventilation, renal dysfunction needing renal replacement therapy, septic shock needing broad-spectrum antibiotics and inotropic support. She had progressively worsening chest X-ray [Figure 1], started developing alveolar hemorrhage, and worsening lung function. Along with hemodynamic support, renal replacement therapy, broad-spectrum antibiotics, ribavirin were also started as part of therapy. She had worsening lung function and expired with multiorgan dysfunction 10 days following the onset of symptoms.
Discussion
There are two types of hantavirus infection described: HFRS and HPS.
HFRS is a group of clinically similar illnesses caused by species of hantaviruses from the family Bunyaviridae. It is found in Europe, Asia, and Africa. The incubation period of HFRS is 7–36 days. Only 10%–15% of cases have a severe course, with lethality rates between 6% and 15%. HFRS is characterized by the systemic involvement of capillaries and venules. It induces various hemorrhagic manifestations and circulation disorders. Renal involvement is characterized by acute renal failure as a result of interstitial hemorrhage and interstitial infiltrates.[4,5]
HPS is found in North, Central, and South America. It is an often fatal pulmonary disease. It has a fatality rate of 36%–50%. The onset of HPS is characterized by flu-like symptoms such as high fever, myalgia, and headache. The patients develop acute noncardiac pulmonary edema and hypotension within 2–15 days. Bilateral infiltrates develop rapidly, sometimes associated with pleural effusions. Neutrophilic leukocytosis, hemoconcentration, thrombocytopenia, and circulating immunoblasts are observed. Severe courses of HPS are associated with increased lactate levels. The mortality rates of HPS are approximately 50%. Patients who survive the acute phase of the disease recover normally within 5–7 days without any sequelae. Acute renal failure is secondary as a result of shock and respiratory failure.[4]
Hantavirus pulmonary syndrome in association with pregnancy and postpartum
Gilson et al. have reported HPS association with pregnancy in the western world and have associated with increased mortality in mothers and fetal hypoxic damage.[6] Another case report on a pregnant woman in Europe was reported by Macé et al., mimicking acute fatty liver of pregnancy with renal failure.[7]
Indian data
Thottapalayam virus which has been shown to be genetically similar to hantavirus being isolated from India has been reported by Carey et al. in 1971.[8] Later, hantavirus infection, reported by Chandy et al. in Tamil Nadu, showed serological evidence of the existence of the disease.[9] There were no clinical data in association with pregnancy so far from India.
Therapy
Supportive therapy is the mainstay of care for patients with hantavirus infections. Care includes careful management of the patient's fluid and electrolytes, respiratory and hemodynamic parameters, and appropriate treatment of any secondary infection. Renal replacement therapy may be required to correct severe fluid overload. Intravenous ribavirin, an antiviral drug, has been shown to decrease illness and death associated with HFRS if used very early in the disease.[10] Ribavirin has not shown to be effective in HPS and needs further evaluation.[11]
Conclusion
Hantavirus infection, once thought to be rare in India, needs to be considered in the differential diagnosis of ARDS and especially in association with pregnancy and postpartum period.
Early diagnosis and supportive care are the mainstays of therapy. Ribavirin may be useful in HFRS and is still experimental in HPS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Morse SS, Schluederberg A. Emerging viruses: The evolution of viruses and viral diseases. J Infect Dis. 1990;162:1–7. doi: 10.1093/infdis/162.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Drebot MA, Jones S, Grolla A, Safronetz D, Strong JE, Kobinger G, et al. Hantavirus pulmonary syndrome in Canada: An overview of clinical features, diagnostics, epidemiology and prevention. Can Commun Dis Rep. 2015;41:6. doi: 10.14745/ccdr.v41i06a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krüger DH, Ulrich R, Lundkvist AA. Hantavirus infections and their prevention. Microbes Infect. 2001;3:1129–44. doi: 10.1016/s1286-4579(01)01474-5. [DOI] [PubMed] [Google Scholar]
- 4.Beers MH, Berkow R. The Merck Manual of Diagnosis and Therapy. 17th ed. Indianapolis: Wiley Publishers; 2005. Infectious diseases; viral diseases. [Google Scholar]
- 5.Sirotin BZ, Keiser NP. On the history of the study of haemorrhagic fever with renal syndrome in eastern Russia. Nephrol Dial Transplant. 2001;16:1288–90. doi: 10.1093/ndt/16.6.1288. [DOI] [PubMed] [Google Scholar]
- 6.Gilson GJ, Maciulla JA, Nevils BG, Izquierdo LE, Chatterjee MS, Curet LB. Hantavirus pulmonary syndrome complicating pregnancy. Am J Obstet Gynecol. 1994;171:550–4. doi: 10.1016/0002-9378(94)90298-4. [DOI] [PubMed] [Google Scholar]
- 7.Macé G, Feyeux C, Mollard N, Chantegret C, Audia S, Rebibou JM, et al. Severe seoul hantavirus infection in a pregnant woman, France, October 2012. Euro Surveill. 2013;18:20464. [PubMed] [Google Scholar]
- 8.Carey DE, Reuben R, Panicker KN, Shope RE, Myers RM. Thottapalayam virus: A presumptive arbovirus isolated from a shrew in India. Indian J Med Res. 1971;59:1758–60. [PubMed] [Google Scholar]
- 9.Chandy S, Boorugu H, Chrispal A, Thomas K, Abraham P, Sridharan G. Hantavirus infection: A case report from India. Indian J Med Microbiol. 2009;27:267–70. doi: 10.4103/0255-0857.53215. [DOI] [PubMed] [Google Scholar]
- 10.Huggins JW, Hsiang CM, Cosgriff TM, Guang MY, Smith JI, Wu ZO, et al. Prospective, double-blind, concurrent, placebo-controlled clinical trial of intravenous ribavirin therapy of hemorrhagic fever with renal syndrome. J Infect Dis. 1991;164:1119–27. doi: 10.1093/infdis/164.6.1119. [DOI] [PubMed] [Google Scholar]
- 11.Maes P, Clement J, Gavrilovskaya I, Van Ranst M. Hantaviruses: Immunology, treatment, and prevention. Viral Immunol. 2004;17:481–97. doi: 10.1089/vim.2004.17.481. [DOI] [PubMed] [Google Scholar]


