Abstract
Objective:
To determine the nationwide incidence of subarachnoid hemorrhage (SAH) and report nationwide changes in smoking rates between 1998 and 2012 in Finland.
Methods:
In this register-based study, we utilized the nationwide Causes of Death Register and Hospital Discharge Register in identifying SAH events between 1998 and 2012. Population statistics in Finland, which were obtained through a database of Statistics Finland, were used to calculate crude annual incidence rates of SAH. For the direct age standardization of crude incidence rates, we used the European Standard Population (ESP) 2013. Data on changes in nationwide smoking rates between 1998 and 2012 were extracted from a database of the National Institute for Health and Welfare.
Results:
For the total of 79,083,579 cumulative person-years, we identified 6,885 people with SAH. Sudden deaths from SAH away from hospitals or in emergency rooms accounted for 1,771 (26%) of the events. Crude nationwide annual incidence rates varied between 6.2 and 10.0 per 100,000 persons, and increased by age particularly in women. Among 70- to 75-year-old women, the incidence of SAH was highest (22.5 per 100,000 persons). The 3-year average of ESP standardized incidence decreased 24% from 11.7 in 1998–2000 to 8.9 per 100,000 persons in 2010–2012. Daily smoking decreased 30% between 1998 and 2012.
Conclusions:
The incidence of SAH seems to be decreasing. This tendency may be coupled with changes in smoking rates. The incidence of SAH in Finland is similar to other Nordic countries.
Subarachnoid hemorrhage (SAH) has a 1-year case-fatality of close to 50%.1 Because a substantial number of SAH patients die suddenly away from hospitals or in emergency rooms,1 and few countries have high autopsy rates for sudden deaths to confirm the diagnosis, reports of nationwide incidence rates of SAH are scarce.
The purpose of this study was to determine the nationwide incidence of SAH in Finland for the first time. As smoking, the most important lifestyle risk factor for SAH,2–4 is likely to contribute to the incidence of SAH, we also tried to report changes in smoking rates in Finland. Finally, since the incidence of SAH in Finland is reported to be exceptionally high,5–8 and this has led, for example, to the exclusion of Finnish studies from SAH risk prediction models,5 we compared Finnish incidence rates with those population-based or nationwide risk estimates, which have included sudden deaths away from hospitals in their analyses.
METHODS
Standard protocol approvals, registrations, and patient consents.
Approvals for this register-based study were obtained from Statistics Finland and the National Institute for Health and Welfare. The National Institute for Health and Welfare accomplished the linkage of the nationwide Hospital Discharge Register (HDR) and the nationwide Causes of Death Register (CDR). According to Finnish and European Union legislation, linkages of nationwide registries and subsequent register-based analyses do not require institutional review board approval. The combined register data did not contain personally identifiable information. The study person responsible for register-based data analyses (J.K.) signed a separate certificate of confidentiality.
Register-based identification of SAH patients.
Using the ICD-10, we retrieved data from the HDR, maintained by the National Institute for Health and Welfare, and from the nationwide CDR, maintained by Statistics Finland, on all persons listed with the primary diagnosis of SAH (ICD-10 codes I60.1-I60.9), like previously.1,2,9 With regard to the nationwide HDR, the cohort included all emergency admissions to any health care facilities due to SAH. People dying away from hospitals or in emergency rooms were classified as sudden deaths, not as hospital-admitted patients. In an attempt to decrease the likelihood of reporting inaccurate incidence rates for aneurysmal SAH, we excluded SAHs coded as undefined or nonaneurysmal SAHs (I60.7-I60.9). We also excluded patients with secondary diagnoses of arteriovenous malformations (Q28*) or intracranial injuries (S06*) from the final SAH cohort. Since the ICD-10 diagnostic codes were introduced in 1996 in Finland, we omitted the data of the first 2 years, as the possibility of diagnostic inaccuracies in the early years is theoretically higher. The final data were collected from the time period starting in January 1998 and ending in December 2012. The National Institute for Health and Welfare linked and anonymized the personal data on the HDR and CDR.
Accuracy of register-based diagnosis of SAH.
The accuracy of the register-based diagnosis of SAH has been reported previously, and the agreement rate and sensitivity are 89%–92%, respectively, in the HDR.4,10 The agreement rate of SAH diagnosis in the Finnish CDR is 95%.10,11
Incidence of SAH.
Incidence rates are expressed as cases per 100,000 persons. We calculated the nationwide crude annual incidence rates by dividing the total number of SAHs by the annual total population in Finland. The 5-year age group population numbers were retrieved from Statistics Finland. We calculated the European age-standardized (European Standard Population [ESP] 2013) annual incidence rates by first multiplying the age-specific rates of SAH by age-specific weights (the weights used in the age adjustment were the proportions of the ESP by each age group), and then we summed the weighted rates across the age groups to give the ESP-adjusted rates. Rates were computed overall and by sex. For estimating changes in incidence rates, we used 3-year average figures, like in a previous nationwide study.12 Since the presented incidence rates are nationwide rates, not based on selected subpopulations, we omitted reporting of confidence intervals. For estimating the statistical significance of changes in incidence rates, we used the Poisson regression analysis.
Data collection on smoking between 1998 and 2012.
We extracted data on smoking in Finland from open-access public Websites (thl.fi/en_US/web/en/statistics/topics/tobacco) of the National Institute for Health and Welfare.
Statistical analyses.
We used Stata statistical software (version 13.1; Stata Corp, College Station, TX) in analyses.
RESULTS
SAH patients in 1998–2012.
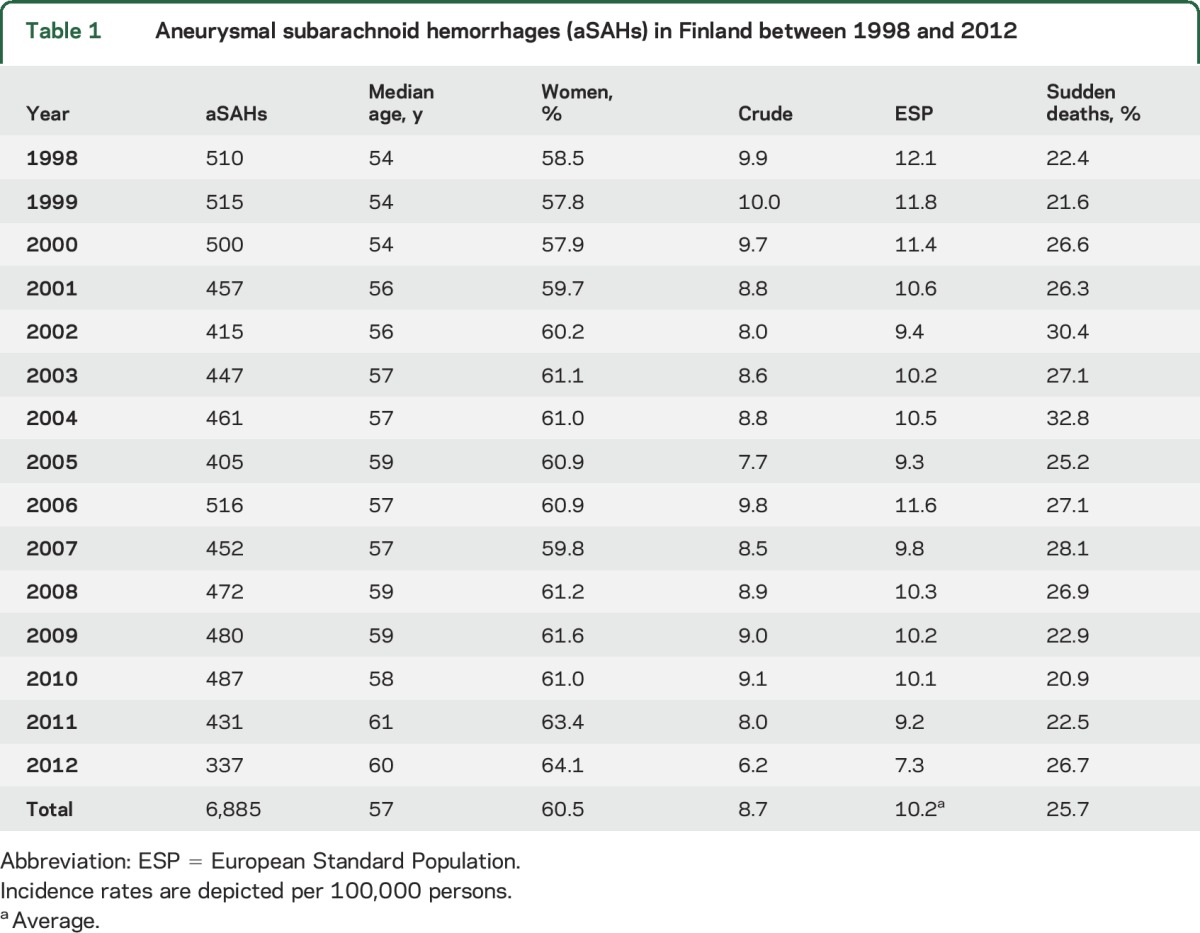
For the total of 79,083,579 cumulative person-years, the register-based search found data on 6,990 persons with a primary diagnosis of SAH (I60.0-I60.9). Of these, 6,912 (98.9%) had a primary diagnosis of aneurysmal SAH (I60.0-I60.6). When we excluded people with secondary diagnoses of arteriovenous malformations or intracranial injuries, the final cohort included 6,885 (98.5%) persons with SAH (table 1). Of these, one-fourth died suddenly (table 1). Of the 1,771 people dying suddenly, 54.9% were women. The median ages for women and men were 60 and 54 years at the time of SAH. The median age for all SAH cases increased during the study period (table 1).
Table 1.
Aneurysmal subarachnoid hemorrhages (aSAHs) in Finland between 1998 and 2012
Based on the ICD-10 codes, internal carotid artery and middle cerebral artery aneurysms accounted for 16.2% and 35.3% of aneurysmal SAHs. Anterior communicating artery and posterior communication artery aneurysms accounted for 23.5% and 6.0% of SAHs. Basilar artery and vertebral artery aneurysms caused SAH in 9.7% and 2.9% of the cases.
Incidence of SAH in 1998–2012.
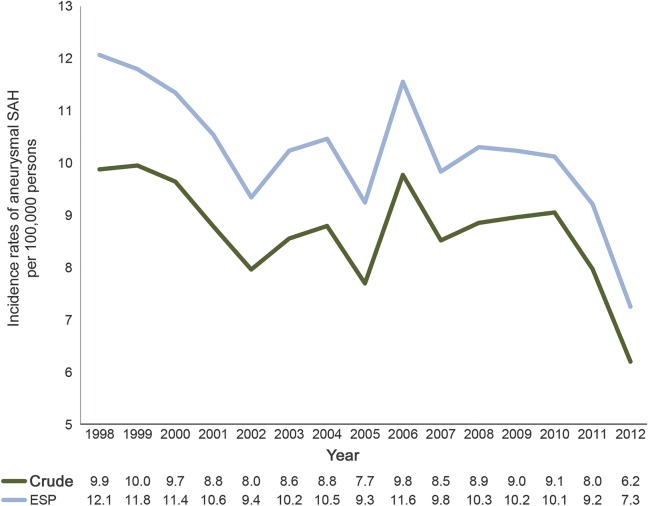
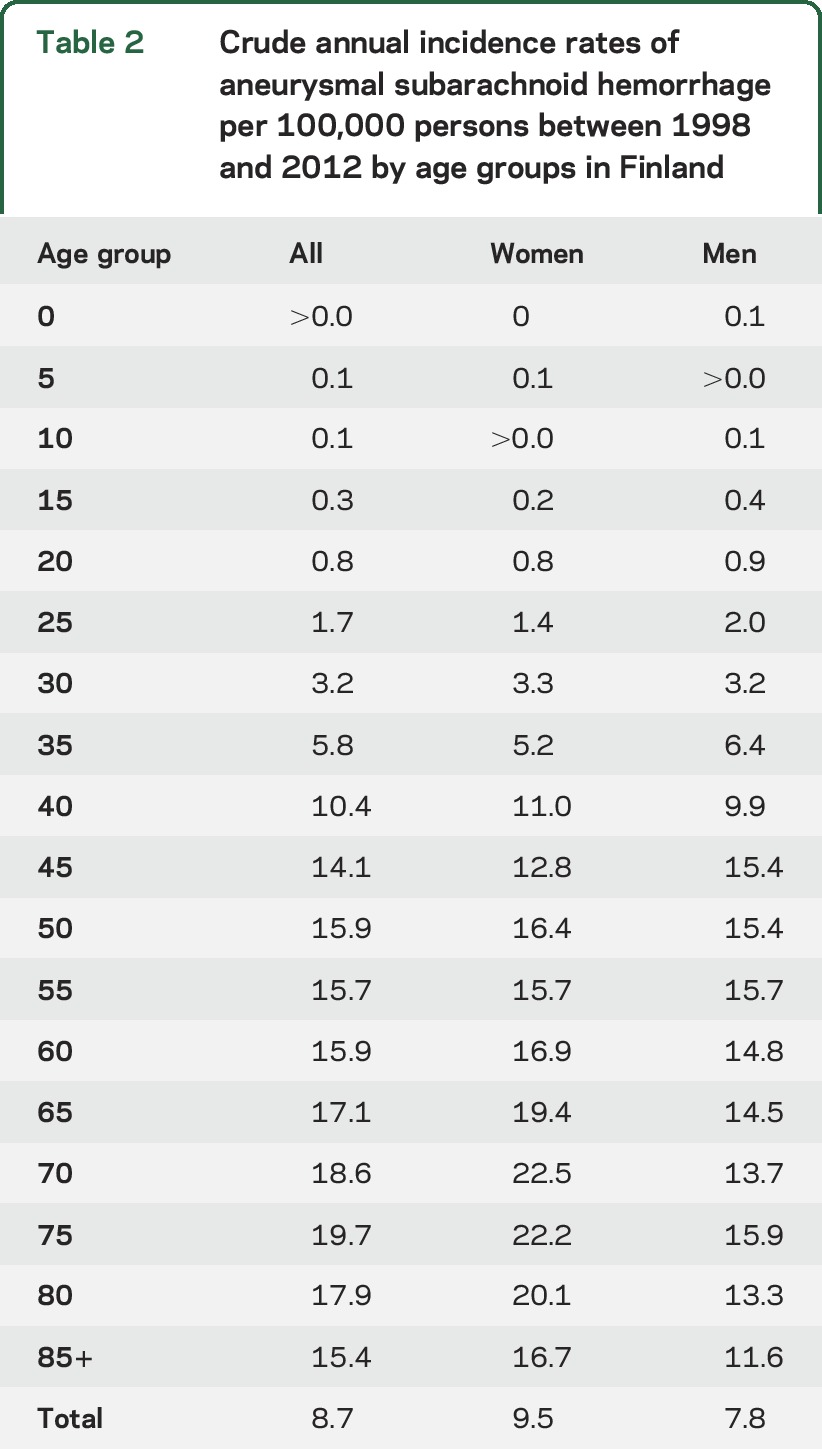
Table 1 and figure 1 depict the annual crude and ESP standardized incidences of SAH. The incidence decreased over time (table 1 and figure 1). According to the Poisson regression analysis, the average annual incidence decrease of 2.1% between 1998 and 2012 was significant (annual incidence rate ratio 0.979, 95% confidence interval 0.974–0.985). The 3-year average of the ESP incidence was 11.7 between 1998 and 2000, but decreased 24% to 8.9 per 100,000 persons in 2010–2012. The 3-year average of the crude incidence decreased by 45% in women younger than 50 years between the time periods 1998–2000 and 2010–2012, and by 38% in age-matched men. In the older age group, of 50 years and older, the 3-year average of the crude incidence decreased less (16% in women and 26% in men) between the same 2 time periods. In general, the crude incidence increased by age, being highest in the age group of 75–80 years (table 2). The female-to-male ratio remained relatively constant (close to 1:1) until age 65 years, after which the ratio increased with increasing age (table 2).
Figure 1. European Standard Population (ESP) 2013 standardized and crude incidence rates of aneurysmal subarachnoid hemorrhage (SAH) between 1998 and 2012 in Finland.
Table 2.
Crude annual incidence rates of aneurysmal subarachnoid hemorrhage per 100,000 persons between 1998 and 2012 by age groups in Finland
Smoking between 1998 and 2012.
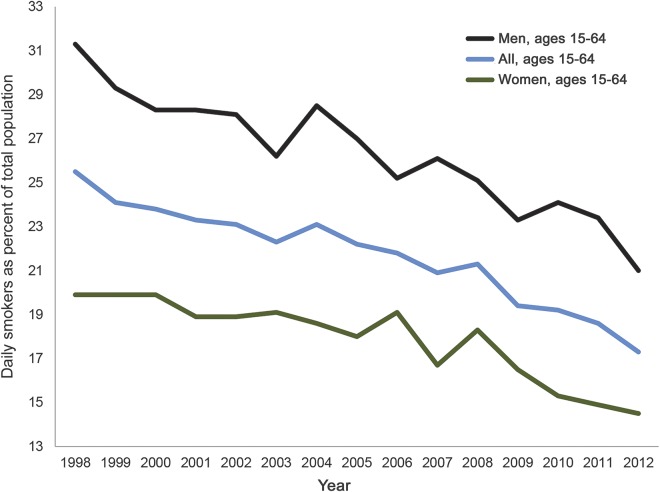
Since 1998, the number of daily smokers has gradually decreased (figure 2), and in 2012, 17% of Finns aged between 15 and 64 years smoked daily. Men used to smoke daily substantially more often than women (figure 2). The percentage of daily smokers among high school students aged 15–17 years decreased 44% from 19% in 2000 to 11% in 2011 among girls, and 41% from 18% to 10% among boys (sotkanet.fi/sotkanet/en/index?).
Figure 2. Daily smokers aged 15–64 years in Finland between 1998 and 2012.
DISCUSSION
Over a time period of 15 years, we observed a decrease in the annual ESP standardized nationwide incidence of SAH in Finland. The crude incidence rates decreased especially in women younger than 50 years. As the incidence of SAH decreased in the relatively short time period and especially in younger age groups, declining smoking rates may partly explain the observed changes. During the study period, the percentage of daily smokers (aged 15–64 years) decreased 30% in Finland, and the decrease was particularly evident among high school students. Between 1997 and 2007, however, blood pressure values decreased in Finland,13,14 as well.
Smoking rates and the prevalence of hypertension decreased already in the 1970s and 1980s, when these risk factor changes were estimated to account for 29% of a substantial drop in the overall stroke figures in Finland.15 At the same time with decreasing incidence rates, the median age at diagnosis of SAH increased by 6 years in the current study. Elimination of preventable risk factors in younger age groups may be coupled with a decrease in incidence rates in the same age groups, thus leading to an increase in the median age at diagnosis.
Studies that report the incidence of SAH need to include sudden deaths from SAH in incidence estimates. Depending on the study year, one-fifth to one-third of people with SAH died suddenly away from hospitals or in emergency rooms. Autopsy rates for sudden deaths are high in Finland,16 and higher than in other Nordic countries.17 The autopsy rate is the lowest in Norway,17 where the ESP standardized incidence rate of SAH is also the lowest (8.7 per 100,000 person-years between 1984 and 2007).18 With regard to the changes in Nordic nationwide incidence rates over time, the crude nationwide incidence of SAH declined ∼20% from 11.1 in 1999–2001 to 8.9 per 100,000 person-years in 2005–2007 in Norway.12 In Sweden, the crude nationwide incidence rates declined ∼11% from 12.7 in 1987–1994 to 11.3 per 100,000 person-years in 1995–2002.19 The nationwide ESP standardized incidence decreased from 13.8 in 1992 to 12.3 per 100,000 persons in 2002 in Denmark.20
The reported incidence rates in Finland have been somewhat inconsistent, depending on the study years, study areas, and study methods. For example, a Finnish study published in 1967 reported an incidence of 15.7 per 100,000 person-years in the capital area.21 In 1991, Sarti et al.22 reported an exceptionally high incidence rate of 29.8 per 100,000 person-years for 25- to 74-year-old Finnish people. This incidence rate was much higher than previously published figures between 1975 and 1986.23–26 Fogelholm27 suggested that the exclusion of nearly 40% of the population (<25-year-old and >74-year-old people) resulted in incomparable rates with earlier studies that included all age groups. This proved to be so, as after an adjustment to the Finnish population in 1986, the incidence rates of 5 previous studies21–24,26 varied from 14.4 to 19.6 per 100,000 person-years.27 Inconsistent incidence rates occur also in those previous studies, which report changes in the Finnish incidence of SAH over time. For example, according to a study covering only a few small geographical areas (<10% of population) in Finland, an age- and sex-adjusted incidence of SAH decreased from 29.9 in 1972–1973 to 13.7 per 100,000 person-years in 1989–1991 among people aged ≥15 years.28 Another small (<10% of population) Finnish study, which was based on a prospective stroke registry FINMONICA and its successor FINSTROKE, reported a steady ESP standardized incidence rate of ∼20 per 100,000 person-years for 25- to 74-year-old people between 1988 and 1997.29 When conducting meta-analyses, pooled studies, or systematic reviews, such inconsistences in Finnish population-based studies lead easily to inaccurate nationwide incidence estimates, as discussed recently.30
The current study has some strengths in comparison with previous population-based and nationwide epidemiologic studies on SAH. Since the incidence of SAH can vary between geographical areas,12,18,19 population-based incidence rates from a few hospitals or hospital districts may be misleading. The current study reports the first nationwide incidence of SAH in Finland. Furthermore, we limited the study to the time period when brain CT scans and ICD-10 classification were in routine use. By doing this, we presumed that the register-based study on the incidence rates of aneurysmal SAH is accurate. In 2010, 141 aneurysmal SAH patients were admitted to the Helsinki University Hospital (based on the hospital's own registry), which has a catchment area of ∼1.8 million people. Thus, the incidence of hospital-admitted aneurysmal SAH was ∼7.8 per 100,000 persons in 2010 in the Helsinki University Hospital area. Taking into account sudden deaths (21% of SAH cases in 2010), we can estimate that the incidence of SAH was ∼9.9 per 100,000 in 2010 in the Helsinki University Hospital area. The nationwide ESP standardized incidence of SAH was approximately the same, 10.1 per 100,000 in 2010 in the current study, suggesting that our register-based search strategy yielded reliable incidence figures. The most disappointing shortcoming in our study is that smoking habits and other risk factors could not be studied at the individual level. This is a shortcoming common to nationwide register-based epidemiologic studies, which can poorly identify causal associations.
The incidence of SAH seems to be decreasing in Finland. This decrease may be coupled with the changes in smoking. The findings indirectly suggest that primary prevention by means of health behavior changes may have a significant effect on the incidence of SAH in the future, and may therefore decrease the population-wide cardiovascular disease burden in many countries. Finally, the Finnish incidence rate of SAH is similar to other Nordic countries. Therefore, Finnish studies can provide important and generalizable data on the epidemiology of SAH, contrary to some previous beliefs.
Supplementary Material
GLOSSARY
- CDR
Causes of Death Register
- ESP
European Standard Population
- HDR
Hospital Discharge Register
- ICD-10
International Classification of Diseases–10
- SAH
subarachnoid hemorrhage
Footnotes
Editorial, page 1070
AUTHOR CONTRIBUTIONS
M.K. had the main responsibility for study design, conducted data analyses, and wrote the paper. H.L. contributed to acquisition and interpretation of data and revision of the paper. S.J. contributed to interpretation of data and critical revision of the paper. J.K. conducted data analyses, contributed to acquisition and interpretation of data, and contributed to critical revision of the paper.
STUDY FUNDING
This study was supported by a personal grant from the Paulo Foundation to M. Korja. J. Kaprio acknowledges the support of the Academy of Finland (grants 265240, 263278). The study sponsors did not have any role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
DISCLOSURE
M. Korja, H. Lehto, and S. Juvela report no disclosures relevant to the manuscript. J. Kaprio consulted for Pfizer on nicotine dependence in 2012–2014. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Korja M, Silventoinen K, Laatikainen T, Jousilahti P, Salomaa V, Kaprio J. Cause-specific mortality of 1-year survivors of subarachnoid hemorrhage. Neurology 2013;80:481–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Korja M, Silventoinen K, Laatikainen T, et al. Risk factors and their combined effects on the incidence rate of subarachnoid hemorrhage: a population-based cohort study. PLoS One 2013;8:e73760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sandvei MS, Romundstad PR, Muller TB, Vatten L, Vik A. Risk factors for aneurysmal subarachnoid hemorrhage in a prospective population study: the HUNT study in Norway. Stroke 2009;40:1958–1962. [DOI] [PubMed] [Google Scholar]
- 4.Knekt P, Reunanen A, Aho K, et al. Risk factors for subarachnoid hemorrhage in a longitudinal population study. J Clin Epidemiol 1991;44:933–939. [DOI] [PubMed] [Google Scholar]
- 5.Greving JP, Wermer MJ, Brown RD Jr, et al. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol 2014;13:59–66. [DOI] [PubMed] [Google Scholar]
- 6.Linn FH, Rinkel GJ, Algra A, van Gijn J. Incidence of subarachnoid hemorrhage: role of region, year, and rate of computed tomography: a meta-analysis. Stroke 1996;27:625–629. [DOI] [PubMed] [Google Scholar]
- 7.de Rooij NK, Linn FH, van der Plas JA, Algra A, Rinkel GJ. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry 2007;78:1365–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Gijn J, Kerr RS, Rinkel GJ. Subarachnoid haemorrhage. Lancet 2007;369:306–318. [DOI] [PubMed] [Google Scholar]
- 9.Korja M, Silventoinen K, McCarron P, et al. Genetic epidemiology of spontaneous subarachnoid hemorrhage: Nordic Twin Study. Stroke 2010;41:2458–2462. [DOI] [PubMed] [Google Scholar]
- 10.Tolonen H, Salomaa V, Torppa J, et al. The validation of the Finnish hospital discharge register and causes of death register data on stroke diagnoses. Eur J Cardiovasc Prev Rehabil 2007;14:380–385. [DOI] [PubMed] [Google Scholar]
- 11.Leppala JM, Virtamo J, Heinonen OP. Validation of stroke diagnosis in the national hospital discharge register and the register of causes of death in Finland. Eur J Epidemiol 1999;15:155–160. [DOI] [PubMed] [Google Scholar]
- 12.Lindekleiv HM, Njolstad I, Ingebrigtsen T, Mathiesen EB. Incidence of aneurysmal subarachnoid hemorrhage in Norway, 1999–2007. Acta Neurol Scand 2011;123:34–40. [DOI] [PubMed] [Google Scholar]
- 13.Kastarinen M, Antikainen R, Peltonen M, et al. Prevalence, awareness and treatment of hypertension in Finland during 1982–2007. J Hypertens 2009;27:1552–1559. [DOI] [PubMed] [Google Scholar]
- 14.Vartiainen E, Laatikainen T, Peltonen M, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol 2010;39:504–518. [DOI] [PubMed] [Google Scholar]
- 15.Tuomilehto J, Bonita R, Stewart A, Nissinen A, Salonen JT. Hypertension, cigarette smoking, and the decline in stroke incidence in eastern Finland. Stroke 1991;22:7–11. [DOI] [PubMed] [Google Scholar]
- 16.Lunetta P, Lounamaa A, Sihvonen S. Surveillance of injury-related deaths: medicolegal autopsy rates and trends in Finland. Inj Prev 2007;13:282–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Penttila A, Lahti RA, Lunetta P. Autopsies as a guarantee of legal protection and quality of patient care [in Finnish]. Duodecim 1999;115:1524–1530. [PubMed] [Google Scholar]
- 18.Sandvei MS, Mathiesen EB, Vatten LJ, et al. Incidence and mortality of aneurysmal subarachnoid hemorrhage in two Norwegian cohorts, 1984–2007. Neurology 2011;77:1833–1839. [DOI] [PubMed] [Google Scholar]
- 19.Koffijberg H, Buskens E, Granath F, et al. Subarachnoid haemorrhage in Sweden 1987–2002: regional incidence and case fatality rates. J Neurol Neurosurg Psychiatry 2008;79:294–299. [DOI] [PubMed] [Google Scholar]
- 20.Engberg AW, Teasdale TW. Epidemiology of non-traumatic brain injury of sudden onset in Denmark 1994–2002 [in Danish]. Ugeskr Laeger 2007;169:204–208. [PubMed] [Google Scholar]
- 21.Pakarinen S. Incidence, aetiology, and prognosis of primary subarachnoid haemorrhage: a study based on 589 cases diagnosed in a defined urban population during a defined period. Acta Neurol Scand 1967;43(suppl 29):1–128. [PubMed] [Google Scholar]
- 22.Sarti C, Tuomilehto J, Salomaa V, et al. Epidemiology of subarachnoid hemorrhage in Finland from 1983 to 1985. Stroke 1991;22:848–853. [DOI] [PubMed] [Google Scholar]
- 23.Fogelholm R. Subarachnoid hemorrhage in middle-Finland: incidence, early prognosis and indications for neurosurgical treatment. Stroke 1981;12:296–301. [DOI] [PubMed] [Google Scholar]
- 24.Sivenius J. Studies on the Rehabilitation, Epidemiology and Clinical Features of Stroke in East Central Finland [dissertation]. Kuopio: University of Kuopio; 1982. [Google Scholar]
- 25.Aho K. Incidence, Profile and Early Prognosis of Stroke: Epidemiological and Clinical Study of the 286 Persons with Onset of Stroke in 1972 and 1973 in a South-Finnish Urban Area [dissertation]. Helsinki: University of Helsinki; 1975. [Google Scholar]
- 26.Kotila M. Declining incidence and mortality of stroke? Stroke 1984;15:255–259. [DOI] [PubMed] [Google Scholar]
- 27.Fogelholm R. Subarachnoid hemorrhage in Finland. Stroke 1992;23:437. [PubMed] [Google Scholar]
- 28.Numminen H, Kotila M, Waltimo O, Aho K, Kaste M. Declining incidence and mortality rates of stroke in Finland from 1972 to 1991: results of three population-based stroke registers. Stroke 1996;27:1487–1491. [DOI] [PubMed] [Google Scholar]
- 29.Sivenius J, Tuomilehto J, Immonen-Raiha P, et al. Continuous 15-year decrease in incidence and mortality of stroke in Finland: the FINSTROKE study. Stroke 2004;35:420–425. [DOI] [PubMed] [Google Scholar]
- 30.Korja M, Kaprio J. Controversies in epidemiology of intracranial aneurysms and SAH. Nat Rev Neurol 2016;12:50–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.