Abstract
Background and purpose
Vaginal stenosis (VS) after pelvic radiotherapy can impair long-term quality of life. We prospectively assessed adherence and efficacy of VD use as the primary and secondary objectives, respectively.
Material and methods
Women with gastrointestinal (n=63) and gynecologic (n=46) cancers self-reported use and VD size in monthly diaries for 12 months after radiotherapy. Adherence was measured as actual VD use out of recommended times over 12 months (3×/week × 52 weeks = 156).
Results
Among 109 participants, aged 28–81 years (median, 58 years), mean percent adherence over 12 months was 42% (95% confidence interval [CI], 36%–48%). Adherence was highest in the first quarter (56%), but fell to 25% by the fourth. Disease type, treatment sequence, and chemotherapy were predictors of adherence (all P<.05). Eighty-two percent maintained pre-RT VD size at 12 months; of 49% with decrease in VD size at 1 month post-RT, 71% returned to pre-RT VD size at 12 months. Disease type, younger age, and increased adherence at 6 months were associated with maintaining or returning to pre-RT size at 12 months (all P≤.05).
Conclusions
VD use is effective in minimizing VS, but adherence at 12 months was poor. Studies evaluating methods of improving adherence and determining the optimal frequency and duration of use are needed.
Keywords: Pelvic radiotherapy, Sexual function, Late effects, Gastrointestinal cancers, Vaginal dilator
Pelvic radiotherapy (RT) plays an integral role in managing gynecologic and pelvic gastrointestinal (GI) malignancies. This has been shown to reduce local recurrence, but can lead to long-term side effects, particularly vaginal stenosis (VS), shortening and narrowing of the vagina. Prevalence of radiation-induced VS after pelvic RT for gynecologic malignancies varies widely [1–3]. However, impact of VS has been well documented, with increased rates of dyspareunia, leading to diminished frequency of, and satisfaction with, sexual intercourse [4, 5] and pain on vaginal examination, potentially impairing thorough and adequate pelvic assessment [3].
In a previous study [6] examining sexual intercourse compared with vaginal dilator (VDs) in minimizing VS, 57% of women relying on sexual intercourse alone developed VS versus 11% for VDs. Based on these data, the best practice guidelines from the National Forum of Gynecological Oncology Nurses in 2005 recommended patients use the dilator three times per week for 10 minutes. This regimen is to continue for the duration of the patients’ lives after pelvic radiation to decrease adhesions and minimize stenosis, regardless of sexual activity [7].
Studies have found low adherence with VD use [8–10], but were limited to endometrial and cervical cancers, and sample sizes were small, limiting generalizability. There are limited data confirming the efficacy of VD use in minimizing VS, or in establishing timing, frequency, and duration for gynecologic and GI malignancies. To collect evidence to establish best practices, we prospectively investigated adherence to use of a VD to determine effectiveness in minimizing VS after pelvic RT during a 12-month trial.
Patients and methods
This study was approved by the Memorial Sloan Kettering Cancer Center Institutional Review Board in November 2008.
Eligibility
Women ≥21 years, with histologically confirmed, nonmetastatic cervical, endometrial, rectal, or anal cancer treated with definitive or adjuvant pre- or postoperative external beam pelvic radiation or brachytherapy were eligible. Exclusion criteria included prior pelvic radiation and prior mental or physical handicap.
Patient recruitment
Eligible patients were identified and approached in radiation oncology clinics at the Memorial Sloan Kettering Cancer Center Manhattan campus and its four regional sites in New York and New Jersey. Between January 2009 and June 2012, 116 patients were recruited. All study participants gave written informed consent.
Study Intervention
Before starting radiation, participants were provided with dilator kits, containing 4 dilator tubes of increasing sizes and lubricating jelly. After the nurse demonstrated the equipment and supplies and reviewed the content of a uniform patient-education fact card, each patient was instructed to use the VD 3 times/week, regardless of sexual intercourse frequency. Patients were taught how to determine their baseline VD size, specifically the largest dilator that could be tolerably inserted and kept in place for 10 minutes without vaginal pain, tightness, and/or bleeding.
The start date for VD use was determined by participants’ RT treatment sequence:
Preoperative RT patients (rectal): 12–14 weeks post-RT (6–8 weeks after pelvic surgery)
Postoperative RT patients (cervical and endometrial) and those undergoing RT alone (anal): 4–6 weeks post- RT.
When initiating VD use, patients received additional instruction on when and how to increase the size of the VD for optimal benefit. Patients were also given a diary to record the date of each dilator use and the size of the dilator.
Data collection
During enrollment, patients completed a demographic questionnaire, including age, medical history, sexual history, and lifestyle factors. Patients are initially instructed in VD use prior to RT treatment to determine their VD size and record their baseline measurements in their diaries. One month (median, 31 days) after RT, patients again use the VD to determine a post-treatment baseline. During regular use, patients recorded dilator size (i.e., size 1–4) for each date of use in their weekly diary. The study team made scripted monthly phone calls to remind each participant to mail in their diaries. This was further facilitated by providing MSKCC stamped envelopes at the end of each month. In addition, the study primary investigator called participants at 3, 6, and 12 months to collect current VD size. Study duration was 12 months (Supplemental Fig. 1). The study was designed to determine the level of self-adherence of patients to VD use based on the weekly diary entries.
Study outcome/end points
Dilator Adherence
Patients’ adherence to weekly VD regimen was measured by 1) summarizing the number of times the VD was used per week based on the weekly diaries, 2) calculating overall percent adherence from the number of 156 possible times each patient used the VD during the 52 weeks on study (3×/week × 52 weeks = 156), and 3) calculating percent adherence from the number of times each patient used the VD each quarter (3×/week × 13 weeks = 39). Adherence was calculated for all patients eligible for the study. If a patient withdrew early from the study due to non-adherence or other non-medical reasons, the patient was assumed to have not used the dilator after withdrawal and the full denominator of 156 was used to calculate overall percent adherence. However, if a patient did not finish the study due to advanced disease, death, or medical reasons to discontinue VD use, the denominator for percent adherence was reduced to the total number of times the patient could have used the dilator while on the study (<156 times).
Vaginal Dilator Efficacy
The efficacy of VD use was defined as ability to maintain or return to pre-RT baseline size with the dilator in place for a full 10 minutes; this was evaluated in patients completing the 3-, 6-, and 12-month assessments. We also examined ability to return to pre-RT baseline VD size in patients with decreased dilator size at 1 month post-RT.
Data analysis
Group comparisons were evaluated using Fisher’s exact test for categorical variables and the Wilcoxon rank sum test or Kruskal-Wallis test for continuous variables. P<.05 was considered statistically significant. Computations were performed using SAS version 9.2 (SAS Institute, Cary, NC).
Results
Study sample
116 patients were enrolled; 7 were ineligible and removed due to distant metastases or medical condition incompatible with VD use. Data analysis was thus performed on 109 participants (Supplemental Fig. 2). There was only 1 cervical cancer patient. This patient was included in all analyses, except those examining the effect of disease diagnosis.
Patient characteristics
Table 1 describes patient characteristics. Median age was 58 years (range, 28–81 years); endometrial cancer patients were older (median age, 60 years) than rectal (54 years) or anal (55 years) cancer patients and had more comorbidities, in particular hypertension. History of tobacco use was more common in anal cancer patients. Rectal and anal cancer patients reported more sexual activity at baseline than endometrial cancer patients (64%, 69%, and 41%, respectively; P=.03). Most endometrial patients (84%) were post-menopausal compared with rectal (57%) and anal (71%). All endometrial patients had total hysterectomy pre-radiation.
Table 1.
Patient Characteristics
| Variable | Category | Total (n = 109) | Rectal (n = 28) | Anal (n = 35) | Endometrial (n = 45) | P |
|---|---|---|---|---|---|---|
| Age | Median (range) | 58 (28–81) | 54 (28–78) | 55 (44–77) | 60 (44–81) | 0.06 |
| Race | White | 82 (75%) | 18 (64%) | 26 (74%) | 37 (82%) | 0.14 |
| Asian | 9 (8%) | 5 (18%) | 1 (3%) | 3 (7%) | ||
| Black/African- American | 7 (6%) | 1 (4%) | 2 (6%) | 4 (9%) | ||
| Hispanic | 7 (6%) | 2 (7%) | 4 (11%) | 1 (2%) | ||
| Other | 4 (4%) | 2 (7%) | 2 (6%) | 0 | ||
| Education level | Post-graduate degree | 33 (31%) | 5 (18%) | 13 (37%) | 15 (34%) | 0.25 |
| College degree | 33 (31%) | 13 (46%) | 11 (31%) | 9 (21%) | ||
| Some college | 21 (19%) | 6 (21%) | 4 (11%) | 11 (25%) | ||
| High school or less | 21 (19%) | 4 (14%) | 7 (20%) | 9 (21%) | ||
| Missing | 1 | 0 | 0 | 1 | ||
| Marital status | Married | 75 (69%) | 22 (79%) | 25 (71%) | 27 (60%) | 0.06 |
| Divorced | 13 (12%) | 2 (7%) | 5 (14%) | 6 (13%) | ||
| Single | 9 (8%) | 1 (4%) | 5 (14%) | 3 (7%) | ||
| Widowed | 12 (11%) | 3 (11%) | 0 | 9 (20%) | ||
| Gravida | No children | 19 (17%) | 3 (11%) | 7 (20%) | 9 (20%) | 0.59 |
| Children | 90 (83%) | 25 (89%) | 28 (80%) | 36 (80%) | ||
| Menopausal status at diagnosis | Pre-menopausal | 18 (17%) | 8 (29%) | 5 (14%) | 5 (11%) | 0.10 |
| Post-menopausal | 80 (73%) | 16 (57%) | 25 (71%) | 38 (84%) | ||
| Peri-menopausal | 11 (10%) | 4 (14%) | 5 (14%) | 2 (4%) | ||
| Using topical estrogen | No | 105 (96%) | 28 (100%) | 32 (91%) | 44 (98%) | 0.22 |
| Yes | 4 (4%) | 0 | 3 (9%) | 1 (2%) | ||
| Sexually active (baseline) | No | 48 (44%) | 10 (36%) | 11 (31%) | 26 (59%) | 0.03 |
| Yes | 60 (56%) | 18 (64%) | 24 (69%) | 18 (41%) | ||
| Missing | 1 | 0 | 0 | 1 | ||
| Smoking History | No | 59 (54%) | 20 (71%) | 14 (40%) | 25 (56%) | 0.05 |
| Comorbidities | Yes | 50 (46%) | 8 (29%) | 21 (60%) | 20 (44%) | |
| 0 | 77 (71%) | 23 (82%) | 29 (83%) | 24 (53%) | 0.03 | |
| 1 | 24 (22%) | 4 (14%) | 5 (14%) | 15 (33%) | ||
| 2+ | 8 (7%) | 1 (3%) | 1 (3%) | 6 (13%) | ||
| Diabetes | No | 98 (90%) | 25 (89%) | 34 (97%) | 38 (84%) | 0.17 |
| Yes | 11 (10%) | 3 (11%) | 1 (3%) | 7 (16%) | ||
| Hypertension | No | 81 (74%) | 25 (89%) | 29 (83%) | 26 (58%) | 0.005 |
| Yes | 28 (26%) | 3 (11%) | 6 (17%) | 19 (42%) | ||
| Vascular Insufficiency | No | 107 (98%) | 28 (100%) | 35 (100%) | 43 (96%) | 0.51 |
| Yes | 2 (2%) | 0 | 0 | 2 (4%) |
Cancer treatment modality
Forty-six patients had gynecologic cancers. The 45 endometrial cancer patients were treated with total abdominal hysterectomy and bilateral salpingo-oophorectomy, followed by adjuvant RT [11]. Of these, 7 received external beam RT (EBRT) alone (median dose, 50.4 Gy) and 38 intravaginal RT (median dose, 21 Gy; range, 18–25 Gy, in 3–5 fractions), 2 of whom also received EBRT to 45 Gy. The target volume treated was one-half to two-thirds the vagina length. Treatment was delivered using a cylinder connected to an after-loading HDR 192Ir source. Cylinder diameter ranged from 2 to 3 cm (median, 3 cm). The dose was prescribed to a depth of 0.5 cm from the vaginal surface. The 1 cervical cancer patient was treated with EBRT alone to 50.4 Gy.
Anal cancer patients (n = 35) were treated with concurrent chemotherapy (5-fluorouracil and mitomycin C) and EBRT in 5–6 weeks with intensity-modulated radiation therapy to a total of 50–56 Gy (median dose, 56Gy) using a 1.8–2 Gy daily fraction) [12]. Rectal cancer patients (n = 28) were treated with concurrent 5-fluorouracil-based chemotherapy and EBRT for 5–6 weeks pre- or postoperatively with either a 3-field plan or intensity-modulated radiation to a median dose of 50Gy using a 1.8–2 Gy daily fraction; patients also received postoperative chemotherapy [13].
Table 2 displays treatment modality, total radiation dose, and vaginal dose. Median vaginal maximum dose and mean vaginal dose were significantly higher for anal cancer patients than rectal or endometrial cancer EBRT patients.
Table 2.
Treatment Modality and Radiation Doses
| Variable | Category | Total (n = 109) | Rectal (n = 28) | Anal (n = 35) | Endometrial (n = 45) |
|---|---|---|---|---|---|
| Surgery | No | 32 (29%) | 4 (14%) | 28 (80%) | 0 |
| Yes | 77 (71%) | 24 (86%) | 7 (20%) | 45 (100%) | |
| Radiation | Preoperative RT | 28 (26%) | 25 (89%) | 3 (9%) | 0 |
| Postoperative RT | 51 (47%) | 2 (7%) | 4 (11%) | 45 (100%) | |
| RT with no surgery | 30 (28%) | 1 (4%) | 28 (80%) | 0 | |
| RT modality | EBRT | 71 (65%) | 28 (100%) | 35 (100%) | 7 (16%) |
| Intravaginal | 38 (35%) | 0 | 0 | 38 (84%) | |
| Mean EBRT dose | Median (range) | 5000 | 5000 | 5400 | 5040 (4320–5040) |
| Mean IVRT dose | Mean IVRT dose | 2100 (1800–2500) | |||
| Chemotherapy | No | 32 (29%) | 0 | 0 | 32 (71%) |
| Yes | 77 (71%) | 28 (100%) | 35 (100%) | 13 (29%) |
Abbreviations: EBRT, external beam radiotherapy; IVRT, intravaginal radiotherapy; RT, radiotherapy.
Adherence to VD use
Percent adherence was calculated for all patients, regardless of whether they finished the study; however, we adjusted the total number of times the dilator could be used for five patients to account for these patients not finishing the study (due to advanced disease, death, or medical reasons to discontinue VD use). Weekly adherence rates using VD for 3×/week versus 1x/week were compared across groups (Fig. 1). At 4 weeks after initiation of use, the adherence rate for 3×/week was 45% (49/108), declining to 20% (21/106) at 35 weeks and 5% (5/104) at 52 weeks. Adherence to VD only once/week was 69% (74/108) at 4 weeks after initiation, 34% (35/104) by 48 weeks, and 12% (12/104) at 52 weeks.
Fig. 1.
Adherence of vaginal dilator at 3×/week versus 1×/week in all groups.
Mean percent adherence across all groups over the 1-year period was 42% (95% CI, 36%–48%). Mean percent adherence was also examined quarterly, and declined across all groups from 56% in the first quarter (95% CI, 49%–63%) to 46% in the second quarter (95% Cl, 39%–53%), 41% in the third quarter (95% CI, 34%–49%), and 25% in the fourth quarter (95% CI, 20%–31%).
Adherence was lowest among patients with rectal cancer, pre-op RT, and those receiving chemotherapy (all P<.05; Table 3).
Table 3.
Factors Associated with Mean Percent Adherence
| Variable | Category | N | Mean (std) | P value |
|---|---|---|---|---|
| Disease group | Rectal | 28 | 0.24 (0.30) | .002 |
| Anal | 35 | 0.51 (0.28) | ||
| Endometrial | 45 | 0.47 (0.34) | ||
| Age | <65 | 78 | 0.44 (0.33) | .34 |
| ≥65 | 31 | 0.37 (0.33) | ||
| Race | Non-white | 27 | 0.42 (0.27) | .84 |
| White | 82 | 0.42 (0.35) | ||
| Education | College degree or higher | 66 | 0.47 (0.32) | .10 |
| Less than college degree | 42 | 0.36 (0.33) | ||
| Marital status | Married | 75 | 0.43 (0.33) | .77 |
| Other | 34 | 0.4 (0.33) | ||
| Menopausal | Post | 80 | 0.43 (0.33) | .82 |
| Pre | 29 | 0.4 (0.31) | ||
| Sexually active (baseline) | No | 48 | 0.41 (0.33) | .75 |
| Yes | 60 | 0.43 (0.33) | ||
| Smoking history | No | 59 | 0.42 (0.34) | .95 |
| Yes | 50 | 0.42 (0.31) | ||
| Comorbidities | No | 77 | 0.4 (0.33) | .32 |
| Yes | 32 | 0.46 (0.32) | ||
| Radiation | Preop | 28 | 0.26 (0.29) | .004 |
| Postop | 51 | 0.45 (0.34) | ||
| RT with no surgery | 30 | 0.53 (0.29) | ||
| RT modality | EBRT | 71 | 0.39 (0.33) | .14 |
| Intravaginal | 38 | 0.48 (0.32) | ||
| Chemotherapy | No | 32 | 0.52 (0.33) | .04 |
| Yes | 77 | 0.38 (0.32) |
Abbreviations: EBRT, external beam radiotherapy; RT, radiotherapy.
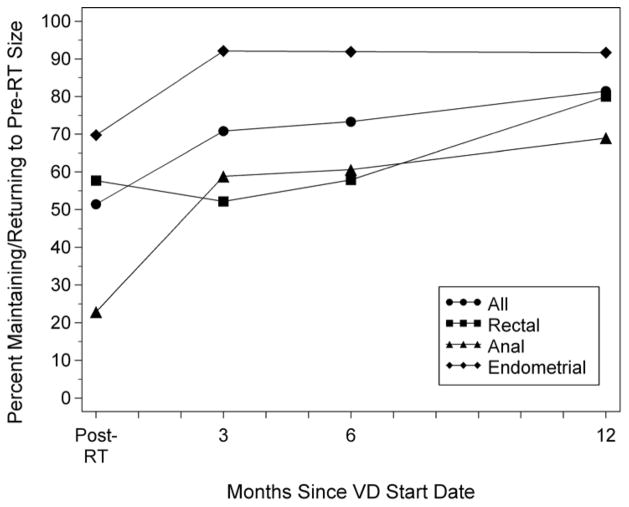
Effectiveness of VD use
Effectiveness of VD use was measured by maintaining or returning to pre-RT dilator size and was calculated in patients who provided measurements. Effectiveness for all groups at 6 and 12 months after VD start was 73% (66/90) and 82% (66/81), respectively (Fig. 2). At 1 month post-RT, 51 of 105 patients (49%) had a decrease in VD size from pre-RT; of these, 52% (24/46) reported return to baseline by 6 months and 71% (29/41) by 12 months after VD start. Of those who had a decrease in VD size at 1 month post-RT, 22% (2/9) and 63% (5/8) were able to return to pre-RT size at 6 and 12 months, respectively, in the rectal cancer group; 54% (14/26) and 68% (15/22), respectively, in the anal cancer group; and 73% (8/11) and 82% (9/11), respectively, in the endometrial group (Supplemental Table 1).
Fig. 2.
Effectiveness of vaginal dilator use.
There was a strong association between adherence to VD use by 6 and 12 months and maintaining or returning to pre-RT size at 12 months. Mean percent adherence by both 6 months (68% vs. 45%, respectively, P=.03) and 12 months (57% vs. 39%, respectively, P=.05) was higher in patients who maintained or returned to pre-RT dilator size at 12 months compared with those who did not. Baseline characteristics associated with maintaining or returning to pre-RT dilator size at 12 months include disease group (endometrial cancer; P=.05) and younger age (P=.05) (Table 4).
Table 4.
Factors Associated with Effectiveness by 12 Months
| Variable | Category | 12 month denominator | Do not maintain or return to pre-RT size at 12 months | Maintain or return to pre-RT size at 12 months | P value |
|---|---|---|---|---|---|
| Disease group | 1 Rectal | 15 | 3 (20%) | 12 (80%) | 0.05 |
| 2 Anal | 29 | 9 (31%) | 20 (69%) | ||
| 3 Endometrial | 36 | 3 (8%) | 33 (92%) | ||
| Age | <65 | 60 | 8 (13%) | 52 (87%) | 0.05 |
| ≥65 | 21 | 7 (33%) | 14 (67%) | ||
| Race | Non-white | 21 | 5 (24%) | 16 (76%) | 0.52 |
| White | 60 | 10 (17%) | 50 (83%) | ||
| Education | Less than college degree | 31 | 9 (29%) | 22 (71%) | 0.08 |
| College degree or higher | 50 | 6 (12%) | 44 (88%) | ||
| Marital status | Married | 56 | 7 (13%) | 49 (88%) | 0.06 |
| Other | 25 | 8 (32%) | 17 (68%) | ||
| Menopausal | Pre | 21 | 2 (10%) | 19 (90%) | 0.33 |
| Post | 60 | 13 (22%) | 47 (78%) | ||
| Topical estrogen | No | 79 | 15 (19%) | 64 (81%) | 1.0 |
| Yes | 2 | 0 | 2 (100%) | ||
| Sexually active (baseline) | No | 34 | 8 (24%) | 26 (76%) | 0.39 |
| Yes | 47 | 7 (15%) | 40 (85%) | ||
| Smoking history | No | 41 | 7 (17%) | 34 (83%) | 0.78 |
| Yes | 40 | 8 (20%) | 32 (80%) | ||
| Comorbidities | No | 55 | 11 (20%) | 44 (80%) | 0.76 |
| Yes | 26 | 4 (15%) | 22 (85%) | ||
| Radiation | Pre-operative | 15 | 3 (20%) | 12 (80%) | 0.28 |
| Post-operative | 41 | 5 (12%) | 36 (88%) | ||
| RT with no surgery | 25 | 7 (28%) | 18 (72%) | ||
| RT modality | EBRT | 49 | 12 (24%) | 37 (76%) | 0.14 |
| Intravaginal | 32 | 3 (9%) | 29 (91%) | ||
| No Chemotherapy | No | 54 | 14 (26%) | 40 (74%) | 0.02 |
| Yes | 27 | 1 (4%) | 26 (96%) | ||
| Vaginal moisturizer (3 months) | No | 62 | 13 (21%) | 49 (79%) | 0.50 |
| Yes | 19 | 2 (11%) | 17 (89%) | ||
| Vaginal moisturizer (6 months) | No | 60 | 15 (25%) | 45 (75%) | 0.009 |
| Yes | 21 | 0 | 21 (100%) | ||
| Vaginal moisturizer (12 months) | No | 58 | 12 (21%) | 46 (79%) | 0.54 |
| Yes | 23 | 3 (13%) | 20 (87%) | ||
| Compliance rate by 6 months | Mean (std) | - | 45% (34%) | 68% (28%) | 0.03 |
| Compliance rate by 12 months | Mean (std) | - | 39% (31%) | 57% (27%) | 0.05 |
Abbreviations: EBRT, external beam radiotherapy; RT, radiotherapy.
Study attrition and nonadherence
Of the 109 participants, 24% (n = 26) requested to withdraw over the course of 12 months due to (a) nonadherence with VD use (n = 10); (b) progression of disease (n = 3); (c) personal reasons (n = 8); and (d) treatment-related side effects (n = 5). The most common reasons for nonadherence were lack of understanding of VD utility (not enough time, not in the mood, sexually active or inactive, vacation); vaginal symptoms associated with VD use (primarily bleeding and discomfort), and medical reasons (postchemotherapy fatigue, rehospitalization, and urinary tract infection).
Discussion
Vaginal stenosis is a significant long-term effect of pelvic RT in patients with gynecologic and GI cancers. Our prospective study of VD use suggests that adherence results in maintaining or returning to baseline VD size in 82% overall. In those who had a decrease in VD at 1 month post-RT, 71% returned to baseline (endometrial, 82%; anal, 68%; rectal, 63%).
This is the first prospective study to report on the incidence of VS in women treated for GI malignancies. However, in women with gynecologic malignancies, prevalence has been reported from 1.6% to 88% [1–3, 14–17]. Factors accounting for the wide variation may include RT techniques, treatment planning differences, sequence and combination of modalities, over- or underreporting, and lack of valid measurement tools [1, 4, 15, 16, 18–20]. Onset of VS was evident as early as 1 month post-RT in 77%, 42%, and 30% of anal, rectal, and endometrial patients, respectively, in this sample. Our findings were consistent with studies showing that VS develops early, even during the course of intracavitary RT and within 1 month after EBRT in cervical and endometrial cancers [20, 21]. Development of VS has also been attributed to the cumulative effect of radiation, which produces adhesions and circumferential fibrosis in vaginal epithelium. This could significantly diminish blood flow to the vaginal tissues, causing loss of elasticity and sensation [5, 21, 22]. Our study demonstrated adherence to VD use at 6 months was important for recovery to pre-RT vaginal size; thus, early intervention may reduce long-term consequences.
To date, no studies have prospectively evaluated adherence with VD use in women with GI cancers. Unfortunately, mean percent adherence for dilator use 3×/week for the 12 months on study was only 42%. The subgroup of patients with rectal cancer and those undergoing pre-operative RT had the lowest adherence to VD use, likely due the subsequent surgical resection, either a low anterior resection or abdominal perineal resection with construction of permanent colostomy. In addition, patients receiving chemotherapy were less adherent with VD use, likely related to the on-going symptoms from their therapy that may prevent patients from focusing on long-term preventative measures.
Some studies [4, 8] report adherence rates of only 6% at 12 months for endometrial or cervical cancers. A recent study of gynecologic cancer patients who received an educational intervention reported adherence to 2–3×/week VD use of 35% at 12 months, using patient recall [3]. Our findings are based on real-time documentation at time of VD use. Measurement of adherence over a certain timespan may better represent overall adherence since there were various reported practices for VD use.
In our study age was less of a factor than in previous studies, which found higher adherence in older women [3, 8, 23]. We found that the main predictors of low adherence were disease type, treatment sequence, and chemotherapy. Patients with rectal cancer who needed postoperative chemotherapy were less likely to adhere, most likely due to treatment-related side effects, such as bowel dysfunction, fatigue, and neutropenia related to surgery and adjuvant chemotherapy. Their longer treatment course [24] with more acute side effects may have lessened the priority of long-term health maintenance.
Adherence is a complex phenomenon, and ensuring regular VD use may require more than education. Additional psychoeducational interventions to ameliorate fears about sexuality following RT led to better adherence than basic instruction alone in one study (44% versus 5.6%, respectively) [8]. However, there is a lack of evidence on the optimal timing, frequency, and duration of VD use.
Duration of VD use is a significant question. At 12 months, 82% of patients maintained their pre-RT size, with persistent VS in 18%. Previous studies indicated that VS was present 2 years post-RT, with decreased vaginal length >1–2 cm in endometrial cancer patients [25] without VD use. We believe that the positive effects from VD use to minimize VS should be available to patients for as long as necessary, especially beyond 1 year.
Our results highlight the need for methods to improve adherence. Recent studies offer some ideas: women tend to be more motivated to use VDs if they believe pelvic exams will be more comfortable [10].
Limitations
Our 24% attrition rate at 12 months fell within the 16%–45% range of similar prospective studies [3, 4, 9]. To maintain data integrity and avoid overestimating adherence, all patients were included in the calculation of adherence rates.
Although psychological barriers to VD use exist, we studied only physical factors. We did not explore positive influences, or “facilitators,” to adherence. One qualitative study of 15 participants [26] originally identified barriers and facilitators of VD use. The lack of standardized VS measures and methods of addressing VS makes it difficult to correlate results from different studies. In addition, due to the different disease types included in the study, there was not a uniform start time for VD use. Also complicating the assessment is the inability to obtain consistent vaginal length and caliber due to patients’ varying ages and physical characteristics, which alter the anatomic structure of vaginal tissues [27]. Shortening of the apex and decreased caliber can contribute to the inability to insert the dilator beyond the distal vagina. Further, we realize that without randomizing participants to 2x/week, 1x/week, and <1x/week, differing thresholds for pain tolerance, variations in vaginal symptoms, and effectiveness with varying frequent use of VD would not be accounted for. Thus, we obtained the pre-RT VD sizes, allowing us to compare and measure effectiveness post-RT. We consider our pre-RT measurement effort to be a strength of the study, and we believe the use of self-report to be the best method of collecting data without standardized measurement instruments. Our study was not designed to attempt to impute effectiveness of VD use but to assess patients’ pattern of adherence and secondarily to evaluate the effectiveness of VD use.
The study was designed to include patients who were either sexually active or not There were not any preconceived expectations or attempts to predict outcomes, only to learn whether patients adhered to VD use. The inconsistent sexual activity of our patients made it impossible to ascertain whether sexual activity was a determining factor.
Future implications
A goal for future studies is to improve the patient self-reporting tools. Informal conversations with patients indicated that over- and under-recording resulted from the desire to avoid embarrassment or fear of rejection from her caregiver. Future studies should examine whether sexual activity is a predictor of adherence of VD use. Finally, randomized controlled trials in a homogeneous patient population are needed to determine if timing and frequency of VD use affect efficacy.
Conclusions
Our study reported on the adherence and effectiveness of VD use in reducing the effects of VS for patients receiving pelvic radiation for anal and rectal cancers not previously studied prospectively, and included gynecologic cancers. We demonstrated benefit of VD adherence, specifically by minimizing VS following pelvic RT. These results will serve as a significant foundation for future studies determining the optimal frequency and duration of VD use and for improving quality of life post-RT.
Supplementary Material
Acknowledgments
Supported by Geri and ME Nursing Research Fund. The study sponsors had no role in the study design, in the collection, analysis and interpretation of data; in the writing of the manuscript or in the decision to submit the manuscript for publication.
This research team wishes to express its thanks and profound appreciation to Nancy Kline, PhD, RN, CPNP, FAAN, Dennis Graham, PhD, RN, ANP-BC, MaryEllen Coglianese, BSN, RN, Marisol Hernandez, MLS, MA, and Lawrence A. Herman, editor.
Footnotes
Presented as a poster discussion, 2013 ASCO Annual Meeting, McCormick Place, Chicago, Illinois, May 31–June 4, 2013.
Conflict of Interest Statement
The authors have no potential conflicts of interest.
References
- 1.Nori D, Merimsky O, Batata M, Caputo T. Postoperative high dose-rate intravaginal brachytherapy combined with external irradiation for early stage endometrial cancer: a long-term follow-up. Int J Radiat Oncol Biol Phys. 1994;30:831–7. doi: 10.1016/0360-3016(94)90357-3. [DOI] [PubMed] [Google Scholar]
- 2.White ID, Faithfull S. Vaginal dilation associated with pelvic radiotherapy: a UK survey of current practice. Int J Gynecol Cancer. 2006;16:1140–6. doi: 10.1111/j.1525-1438.2006.00452.x. [DOI] [PubMed] [Google Scholar]
- 3.Brand AH, Do V, Stenlake A. Can an educational intervention improve compliance with vaginal dilator use in patients treated with radiation for a gynecological malignancy? Int J Gynecol Cancer. 2012;22:897–904. doi: 10.1097/IGC.0b013e31824d7243. [DOI] [PubMed] [Google Scholar]
- 4.Schover LR, Fife M, Gershenson DM. Sexual dysfunction and treatment for early stage cervical cancer. Cancer. 1989;63:204–12. doi: 10.1002/1097-0142(19890101)63:1<204::aid-cncr2820630133>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 5.Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med. 1999;340:1383–9. doi: 10.1056/NEJM199905063401802. [DOI] [PubMed] [Google Scholar]
- 6.Decruze SB, Guthrie D, Magnani R. Prevention of vaginal stenosis in patients following vaginal brachytherapy. Clin Oncol (R Coll Radiol) 1999;11:46–8. doi: 10.1053/clon.1999.9008. [DOI] [PubMed] [Google Scholar]
- 7.National Forum of Gynaecological Oncology Nurses. [Accessed November 18, 2014];Best practice guidelines on the use of vaginal dilators in women receiving pelvic radiotherapy. http://www.nfgon.org.uk/international-guidelines-on-vaginal-dilation-after-pelvic-radiotherapy/
- 8.Robinson JW, Faris PD, Scott CB. Psychoeducational group increases vaginal dilation for younger women and reduces sexual fears for women of all ages with gynecological carcinoma treated with radiotherapy. Int J Radiat Oncol Biol Phys. 1999;44:497–506. doi: 10.1016/s0360-3016(99)00048-6. [DOI] [PubMed] [Google Scholar]
- 9.Jeffries SA, Robinson JW, Craighead PS, Keats MR. An effective group psychoeducational intervention for improving compliance with vaginal dilation: a randomized controlled trial. Int J Radiat Oncol Biol Phys. 2006;65:404–11. doi: 10.1016/j.ijrobp.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Friedman LC, Abdallah R, Schluchter M, Panneerselvam A, Kunos CA. Adherence to vaginal dilation following high dose rate brachytherapy for endometrial cancer. Int J Radiat Oncol Biol Phys. 2011;80:751–7. doi: 10.1016/j.ijrobp.2010.02.058. [DOI] [PubMed] [Google Scholar]
- 11.Alektiar KM, Venkatraman E, Chi DS, Barakat RR. Intravaginal brachytherapy alone for intermediate-risk endometrial cancer. Int J Radiat Oncol Biol Phys. 2005;62:111–7. doi: 10.1016/j.ijrobp.2004.09.054. [DOI] [PubMed] [Google Scholar]
- 12.Dasgupta T, Rothenstein D, Chou JF, et al. Intensity-modulated radiotherapy vs. conventional radiotherapy in the treatment of anal squamous cell carcinoma: a propensity score analysis. Radiother Oncol. 2013;107:189–94. doi: 10.1016/j.radonc.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Yang TJ, Oh JH, Son CH, et al. Predictors of acute gastrointestinal toxicity during pelvic chemoradiotherapy in patients with rectal cancer. Gastrointest Cancer Res. 2013;6:129–36. [PMC free article] [PubMed] [Google Scholar]
- 14.Pitkin RM, VanVoorhis LW. Postirradiation vaginitis. An evaluation of prophylaxis with topical estrogen. Radiology. 1971;99:417–21. doi: 10.1148/99.2.417. [DOI] [PubMed] [Google Scholar]
- 15.Noyes WR, Bastin K, Edwards SA, et al. Postoperative vaginal cuff irradiation using high dose rate remote afterloading: a phase II clinical protocol. Int J Radiat Oncol Biol Phys. 1995;32:1439–43. doi: 10.1016/0360-3016(95)00097-I. [DOI] [PubMed] [Google Scholar]
- 16.Nunns D, Williamson K, Swaney L, Davy M. The morbidity of surgery and adjuvant radiotherapy in the management of endometrial carcinoma. Int J Gynecol Cancer. 2000;10:233–8. doi: 10.1046/j.1525-1438.2000.010003233.x. [DOI] [PubMed] [Google Scholar]
- 17.Saibishkumar EP, Patel FD, Sharma SC. Evaluation of late toxicities of patients with carcinoma of the cervix treated with radical radiotherapy: an audit from India. Clin Oncol (R Coll Radiol) 2006;18:30–7. doi: 10.1016/j.clon.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 18.Hartman P, Diddle AW. Vaginal stenosis following irradiation therapy for carcinoma of the cervix uteri. Cancer. 1972;30:426–9. doi: 10.1002/1097-0142(197208)30:2<426::aid-cncr2820300219>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 19.Flay LD, Matthews JH. The effects of radiotherapy and surgery on the sexual function of women treated for cervical cancer. Int J Radiat Oncol Biol Phys. 1995;31:399–404. doi: 10.1016/0360-3016(94)E0139-B. [DOI] [PubMed] [Google Scholar]
- 20.Brand AH, Bull CA, Cakir B. Vaginal stenosis in patients treated with radiotherapy for carcinoma of the cervix. Int J Gynecol Cancer. 2006;16:288–93. doi: 10.1111/j.1525-1438.2006.00348.x. [DOI] [PubMed] [Google Scholar]
- 21.Katz A, Njuguna E, Rakowsky E, Sulkes A, Sulkes J, Fenig E. Early development of vaginal shortening during radiation therapy for endometrial or cervical cancer. Int J Gynecol Cancer. 2001;11:234–5. doi: 10.1046/j.1525-1438.2001.01019.x. [DOI] [PubMed] [Google Scholar]
- 22.Hintz BL, Kagan AR, Chan P, et al. Radiation tolerance of the vaginal mucosa. Int J Radiat Oncol Biol Phys. 1980;6:711–6. doi: 10.1016/0360-3016(80)90227-8. [DOI] [PubMed] [Google Scholar]
- 23.Bahng AY, Dagan A, Bruner DW, Lin LL. Determination of prognostic factors for vaginal mucosal toxicity associated with intravaginal high-dose rate brachytherapy in patients with endometrial cancer. Int J Radiat Oncol Biol Phys. 2012;82:667–73. doi: 10.1016/j.ijrobp.2010.10.071. [DOI] [PubMed] [Google Scholar]
- 24.Quick AM, Seamon LG, Abdel-Rasoul M, Salani R, Martin D. Sexual function after intracavitary vaginal brachytherapy for early-stage endometrial carcinoma. Int J Gynecol Cancer. 2012;22:703–8. doi: 10.1097/IGC.0b013e3182481611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruner DW, Lanciano R, Keegan M, Corn B, Martin E, Hanks GE. Vaginal stenosis and sexual function following intracavitary radiation for the treatment of cervical and endometrial carcinoma. Int J Radiat Oncol Biol Phys. 1993;27:825–30. doi: 10.1016/0360-3016(93)90455-5. [DOI] [PubMed] [Google Scholar]
- 26.Bonner C, Nattress K, Anderson C, et al. Chore or priority? Barriers and facilitators affecting dilator use after pelvic radiotherapy for gynaecological cancer. Support Care Cancer. 2012;20:2305–13. doi: 10.1007/s00520-011-1337-z. [DOI] [PubMed] [Google Scholar]
- 27.Barnhart KT, Izquierdo A, Pretorius ES, Shera DM, Shabbout M, Shaunik A. Baseline dimensions of the human vagina. Hum Reprod. 2006;21:1618–22. doi: 10.1093/humrep/del022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.