Abstract
Introduction:
Adult idiopathic hydrocele is a common benign disorder that merits surgical correction when symptomatic. The most popular techniques for repair are plication (Lord’s procedure) or excision and eversion of the tunica vaginalis (Jaboulay procedure). Established complications from these traditional repairs include hematoma, recurrence, and infection. These procedures are performed through a scrotal incision. We describe a novel technique of hydrocele repair with gubernaculum preservation through a subinguinal incision.
Methods:
The novel technique is described in detail. A retrospective review was performed of those patients treated by a single surgeon with the subinguinal technique. Demographic information, indication for treatment, success rate, and details regarding complications were collected.
Results:
We term the technique the “Snip, Stitch & Tug” repair. Through a small subinguinal incision, the tunica is everted posterior to the spermatic cord and testis without resection of the hydrocele sac or division of the gubernaculum. Twelve patients with postoperative followup were identified. Eleven patients (92%) treated with the novel technique were cured. There was only one complication (superficial wound infection) recorded after this technique.
Conclusions:
Idiopathic hydrocele repair with gubernaculum preservation can be easily and safely performed through a small subinguinal incision.
Introduction
Idiopathic hydrocele is a common cause of increased scrotal size in adult males. Despite being a benign condition, patients often seek treatment due to local discomfort, cosmetic appearance, and limitations with intercourse and physical activity. The mainstay of treatment continues to be traditional repairs via a scrotal incision, such as the Jaboulay technique1 or Lord’s procedure.2
There are multiple known complications following scrotal surgery for hydroceles, including infection, abscess formation, hematoma, orchalgia, and treatment failures.3 Contemporary large series from the literature suggest the overall complication rate is as high as 20%.3,4 In an effort to minimize complications while maintaining comparable treatment success rates, we developed a novel subinguinal hydrocelectomy with gubernacular sparing. We hypothesize that with minimal tissue dissection and avoiding a scrotal incision, complications can be minimized, while maintaining efficacy in hydrocele repair.
Methods
Patients
A total of 12 individual patients (13 hydroceles) were included in the study. Mean patient age was 61 years and the mean followup was 8.3 months. All hydrocelectomy procedures were performed in the outpatient setting.
Surgical technique
We term the technique the “Snip, Stitch & Tug” repair to reflect the simple and minimally invasive approach to a common urologic condition. A 2–3 cm incision is made over the subinguinal spermatic cord (Fig. 1). The spermatic cord is isolated and elevated through the wound using a penrose drain (Fig. 2). Gentle pressure on the scrotum is used to mobilize the hydrocele sac cephalad so that the superior aspect is visible in the wound (Fig. 3). The tunica vaginalis is opened anteriorly and the hydrocele fluid is drained (Fig. 4). The gubernaculum is preserved. The hydrocele sac is everted, bringing the free edges posterior to the spermatic cord and testis. These edges are fixed in place with a single figure-of-eight suture (Fig. 5). Gentle traction on the scrotum pulls the testis back into orthotopic position (Fig. 6). Scarpas fascia and skin are reapproximated using absorbable sutures.
Fig. 1.
A 2–3 cm incision is made over the subinguinal spermatic cord.
Fig. 2.

Spermatic cord is isolated and elevated in the wound.
Fig. 3.

Gentle pressure on the scrotum mobilizes the hydrocele sac into the wound.
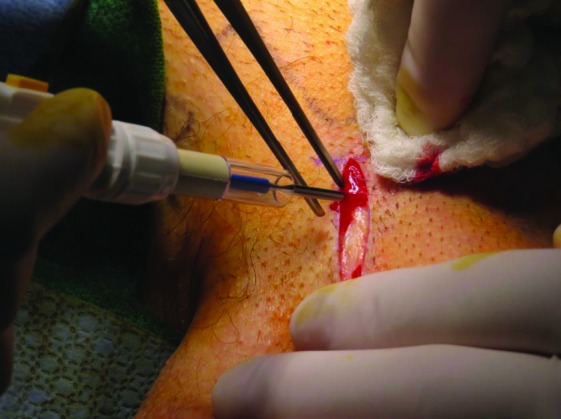
Fig. 4.

The tunica vaginalis is opened anteriorly while maintaining preservation of the gubernacular attachments.
Fig. 5.

A single figure-of-eight suture approximates the everted tunica vaginalis posterior to the spermatic cord and testis.
Fig. 6.

Gentle traction on the scrotum pulls the testis back into orthotopic position.
Results
A total of 13 hydroceles in 12 patients were treated using the novel technique. Indications for surgery included pain/discomfort (n=7) and cosmesis (n=5). Mean operating room time was 35 minutes (range 23–57 min) for the procedure. All patients were followed up in the outpatient clinic at 3–5 weeks (Fig. 7) and again at three months. One patient developed a superficial wound infection (Clavien Grade II) and one patient demonstrated some fluid accumulation (Clavien Grade I) that did not require further intervention. No patients experienced a scrotal hematoma. Importantly, there was a complete absence of scrotal edema and wound discharge in all patients. As well, none of the 12 patients required repeat hydrocelectomy.
Fig. 7.
Results at the three-week postoperative visit.
Discussion
Hydrocelectomy is a commonly performed urologic procedure and is typically performed via a trans-scrotal approach. Trans-scrotal repairs have been widely accepted as the standard of care. Despite this, large series have identified a 20% complication rate —including abscess/infection, hematoma, and recurrence of hydrocele — in the management of this benign condition.3–4 Anecdotally, these procedures are commonly associated with weeks to months of persistent scrotal swelling and serous incisional drainage.
Other, minimally invasive approaches to hydrocele management have been described. Aspiration and sclerotherapy seems to have minimal complications, but limited efficacy (∼75% success rate).5 Other small incision techniques tend to use a trans-scrotal approach and be susceptible to scrotal complications (scrotal edema, scrotal hardness, wound infection, hematoma).6,7
We are pleased to report our initial experience with a novel, minimally invasive technique. By using a 2–3 cm subinguinal incision, hydroceles can be managed without a scrotal incision and without extensive tissue dissection. As a consequence, incisional drainage and scrotal swelling, normally associated with the trans-scrotal approach, can be avoided. We also believe that the minimal dissection associated with this technique was responsible for the low complication rate in our small series. Furthermore, unlike other novel minimally invasive techniques, the “Snip, Stitch & Tug” technique is easy to perform, requires no special equipment, and can be performed in a rapid, safe manner. While replication of our findings is needed prior to wide adoption of this technique, our data support that this is a simple, practical, and safe approach to hydrocelectomy.
The “Snip, Stitch & Tug” hydrocelectomy is associated with a small incision, minimal swelling, and a low complication/recurrence rate.
Footnotes
Competing interests: Dr. Martin has been an Advisory Board member for Janssen and has received grants/honoraria from Astellas, Paladin Labs, and Pfizer. The remaining authors report no competing personal or financial interests.
This paper has been peer-reviewed.
References
- 1.Jaboulay M. Chirurgie des centres nerveux des viscères et des membres. Lyon; Paris: Storck: 1902. p. 192. [Google Scholar]
- 2.Lord PH. A bloodless operation for the radical cure of idiopathic hydrocele. Brit J Surg. 1964;51:914–6. doi: 10.1002/bjs.1800511212. [DOI] [PubMed] [Google Scholar]
- 3.Swartz MA, Todd MM, Krieger JN. Complications of scrotal surgery for benign conditions. Urology. 2007;69:616–9. doi: 10.1016/j.urology.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Kiddoo DA, Wollin TA, Mador DR. A population-based assessment of complications following outpatient hydrocelectomy and spermatocelectomy. J Urol. 2004;171:746–8. doi: 10.1097/01.ju.0000103636.61790.43. [DOI] [PubMed] [Google Scholar]
- 5.Beiko DT, Kim D, Morales A. Aspiration and sclerotherapy vs. hydrocelectomy for treatment of hydroceles. Urology. 2003;61:708–12. doi: 10.1016/S0090-4295(02)02430-5. [DOI] [PubMed] [Google Scholar]
- 6.Onol SY, Ilbey YO, Onol FF, et al. A novel pull-through technique for the surgical management of idiopathic hydrocele. J Urol. 2009;181:1201–5. doi: 10.1016/j.juro.2008.10.166. [DOI] [PubMed] [Google Scholar]
- 7.Saber A. New minimally access hydrocelectomy. Urology. 2011;77:487–90. doi: 10.1016/j.urology.2010.02.048. [DOI] [PubMed] [Google Scholar]



