Abstract
Background
According to Self-Determination Theory, the extent to which the motivation underlying behavior is self-determined or controlled influences its sustainability. This is particularly relevant for behaviors that must be repeated, such as completion of the human papillomavirus (HPV) vaccine series. To date, no measures of motivation for HPV vaccination have been developed.
Methods
As part of a larger study, parents (N=223) whose adolescents receive care at safety-net clinics completed a telephone questionnaire about HPV and the vaccine. We modified the Treatment Self-Regulation Questionnaire to assess parents’ motivation for HPV vaccination in both Spanish and English. We used confirmatory factor analysis to test a three-factor measurement model.
Results
The three-factor model fit the data well (RMSEA=.04, CFI=.98, TLI=.96), and the scales’ reliabilities were adequate (autonomous: α=.87; introjected: α=.72; external: α=.72). The factor loading strength for one item was stronger for Spanish- than English-speaking participants (p<.05); all others were equivalent. The intercorrelations among the scales ranged from −.17 to .32, suggesting discriminant factors. The scales displayed the expected pattern of correlations with other psychosocial determinants of behavior. Vaccination intentions showed a strong correlation with autonomous motivation (r= .52), but no correlation with external motivation (r=.02), suggesting autonomous motivation may be particularly important in vaccine decision-making.
Conclusion
Findings support the use of three subscales to measure motivation in HPV vaccination and suggest possible cultural differences in motivation.
Keywords: Validity, Self-Determination Theory, Motivation, HPV vaccine
Motivation is a key determinant for initiation and maintenance of health behaviors [1,2] but has not been examined in HPV vaccination. According to Self-Determination Theory (SDT), motivation occurs along a continuum ranging from self-determined (performed for internal reasons) to controlled (performed due to external pressures) to amotivation (the absence of motivation). Behaviors are more likely to be maintained if the behavior is autonomously motivated [3]. Since 2007 guidelines recommending routine administration of the 3-dose HPV vaccine series to adolescent girls aged 11–12 (boys added in 2011), national data shows suboptimal vaccine uptake [4]. Parents, the primary decision-makers, are often hesitant and delay vaccination for a number of reasons [5,6]. Theoretically, facilitating autonomous motivation in parents should improve HPV vaccine initiation and completion. However, the lack of valid motivation measures impedes its application to HPV vaccine decision-making.
Autonomously motivated behaviors are those for which people experience a true sense of volition and are performed because of a personal sense of the behavior’s importance [7]. Autonomous motivation facilitates behaviors that are in line with a person’s values and have been integrated into the person’s sense of self. There are two forms of ‘controlled’ motivation: behaviors performed to avoid feeling guilty (introjected motivation), and behaviors performed for a reward or to avoid a negative consequence (external motivation). Practically speaking, an autonomously motivated parent decides to vaccinate their child because they believe in its value and benefit, whereas a parent operating under controlled motivation decides to vaccinate their child to meet others’ expectations (e.g., their child’s doctor). For the 3-dose HPV vaccine series, autonomous motivation may be important in influencing two aspects of parental decisions: 1) timing of the first dose - initiating at the recommended ages (11–12) versus later in adolescence, and 2) timely completion - obtaining the second and third doses on-schedule (i.e., 2 and 6 months after the first dose). Psychometrically sound measures of parental motivation for HPV vaccination are needed in order to examine if it is a determinant of vaccine initiation and series completion and the pathways linking it to other theory-based determinants (e.g., intention, subjective norms).
Validated across a wide range of behaviors [8], the original Treatment Self-Regulation Questionnaire (TSRQ) includes items assessing the different types of motivation, but has only been evaluated in English-speaking populations. A valid Spanish TSRQ HPV vaccine version is needed because many patients in U.S. safety-net healthcare settings prefer to communicate in Spanish and they are at high risk for HPV-related cancers.
This study adapted and gathered evidence on the validity of a TSRQ measuring autonomous, introjected, and external motivation with English- and Spanish-speaking parents. We excluded amotivation items because previous studies demonstrated poor factor loadings compared to items measuring the other motivation types [8]. We assessed construct validity in two ways. First, we examined the scale’s factor structure and tested for factorial equivalence by language. Evidence of factorial invariance is necessary to assess potential group differences in motivation (past studies have shown the influence of other HPV vaccine determinants vary by race/ethnicity and language [9]). Second, we tested discriminant validity. Based on SDT, we hypothesized that factors closer along the continuum of self-determination would show stronger correlations with each other than those factors that are farther apart (e.g., autonomous motivation should correlate more strongly with introjected motivation than with controlled motivation). We also hypothesized that the magnitude of the correlations between the three motivation subscales and other determinants (self-efficacy, perceived benefits, intentions, and subjective norms) would differ. Specifically, (a) autonomous motivation would have stronger, positive correlations with self-efficacy, perceived benefits, and intentions than with subjective norms; (b) the magnitude of the correlations between introjected motivation and the other determinants would be weaker than for autonomous motivation and stronger than those shown with external motivation; and (c) external motivation would have stronger correlations with subjective norms than with self-efficacy, perceived benefits, and intentions.
Methods
This study was part of a multi-stage project to develop, refine, and test a tablet-based self-persuasion intervention to promote HPV vaccination among parents who are undecided about the vaccine (for additional details, see [10]). The analyses reported here used baseline survey data from the first stage of the project that characterized parents’ thoughts and reasons for the HPV vaccine and patient-provider HPV vaccine discussions.
Participants and Setting
Study participants (N=223) were parents or guardians of unvaccinated adolescents (11–17 year old girls and boys) attending Parkland Health & Hospital System pediatric clinics. Parkland is an integrated safety-net system and serves a diverse population of over 14,000 low-income, under- and uninsured adolescents living in Dallas County, TX. Parkland participates in the Vaccines for Children (VFC) program providing vaccines at free or reduced cost and their providers document parental decisions and vaccine administration in their comprehensive electronic health record (EHR).
Recruitment
Potential participants were identified through weekly EHR reports identifying unvaccinated adolescents ages 11–17 with upcoming scheduled clinic visits. Parents of eligible patients were mailed a letter inviting them to participate and provided with a toll-free number to ask questions or refuse participation. Invitation letters were sent in English or Spanish based on preferred language listed in the EHR. Bilingual research assistants (RAs) called parents of eligible patients, explained the project, and asked them to report their decision stage about the vaccine (i.e., never thought about the HPV vaccine, undecided about the vaccine, do not want the vaccine, or do want the vaccine). Parents in the first two stages (never thought about the vaccine, undecided) were invited and consented. Then, the RA administered the baseline survey over the telephone. In addition to the adapted TSRQ items, the survey included additional items assessing perceived benefits, subjective norms, self-efficacy, intentions, and parental demographics [11–13]. We called and verified contact information for a total of 540 parents of eligible adolescents; 260 (48%) were not interested in participating, 57 (11%) consented but did not complete the survey, and 233 (41%) completed the survey.
Adaptation process of the TSRQ
Due to evidence suggesting the amotivation items display poor factor loadings [8] we chose not to include them in our measure. Other adaptations of the TSRQ have also elected not to include these items [8]. Given concerns about participant burden, we also had the goal to identify a shorter TSRQ (i.e., 8 items instead of the typical 15 or 19 items) to assess autonomous, introjected, and external motivation. The lead-in for the eight items was “The reason you would get [child’s name] the [HPV] vaccine is because…”. Content and language experts were consulted to examine the items for face validity and comprehension. A Spanish language translation committee (8 members representing several Latin American countries) translated items into Spanish. During the administration of the survey items, participants responded to each item on a 1 to 5 scale with anchors that ranged from strongly agree to strongly disagree. We averaged responses within the three subscales to create mean scores for each.
Measures to Establish Discriminant Validity
Self-efficacy was assessed with two items reflecting participants’ confidence in their ability to get their child the vaccine in spite of barriers (e.g. “You are confident that you can get the HPV vaccine for your child”; adapted from [12]) and demonstrated adequate reliability (α= .732). Intentions to vaccinate were assessed with three items asking about the likelihood of parents vaccinating their children (e.g. “In the next year, how likely is it that you will get the HPV vaccine for your child?”; adapted from [12]) and demonstrated good reliability (α= .88). Subjective norms were assessed with two items that reflected the influence of friends and family in decision-making about the HPV vaccine (e.g. “Your family influences your decision about getting your child the vaccine”; adapted from [12,14]) and these items displayed good reliability (α= .82). Perceived benefits were assessed with six items that assessed parents’ beliefs regarding the positive nature of HPV vaccination for their adolescents (e.g. “Getting my child the HPV vaccine will be good for my child’s health”; adapted from [11,13]) and demonstrated good reliability (α= .83).
Analysis
Of the 223 parents in the dataset, 215 (96.4%) had complete responses on the motivation items. Analyses were limited to these parents to allow for the examination of modification indices and best estimates of model fit.
Confirmatory Factor Analysis
To examine whether the a priori, three-factor structure of the TSRQ fit parental motivation for adolescent HPV vaccination, we conducted a series of confirmatory factor analyses (CFAs) using full-information maximum likelihood (FIML) estimation in AMOS [15]. FIML uses iterative simultaneous equations to estimate model parameters with missing data by computing a likelihood function for each case based on all available data [16]. Use of FIML leads to more accurate fit indices and parameter estimates than more typical analyses using listwise or pairwise deletion strategies with missing data [17]. We examined three indices (RMSEA, CFI, and TLI) to assess overall adequacy of fit.
Factorial Invariance
To test invariance of the model (i.e., structurally equivalent) across language (Spanish- vs. English-speakers), we followed procedures previously described [18]. We conducted 2-group CFAs that compared constrained and unconstrained models. Constrained models assume that factor loadings are equivalent between Spanish and English groups, whereas unconstrained models allow factor loadings to vary between groups. We expected the TSRQ would provide similar factor loadings across language. This would be demonstrated by strong overall fit indices and a non-significant global test of equality of covariance structures, which follows a χ2 distribution [18].
Discriminant Validity
To determine the discriminant validity of the three-factor TSRQ structure, we examined the pattern of correlations between the three subscales and other psychosocial determinants of HPV vaccination. Due to the lack of other existing measures of motivation in this domain, we were unable to examine convergent validity.
Results
Characteristics of parent/guardian respondents stratified by language are in Table 1. The majority of the sample was Spanish-speaking (59.6%), Hispanic Whites (64.1%). Most participants were women (99.5%) with ages ranging from 22 to 75 (M= 39.8). Spanish- and English speakers differed on education, with English speakers reporting higher levels of education (χ2= .435, p < .05). In terms of adolescent sex, the sample was evenly split (52.5% of parents answered questions for their son). There were no differences of adolescent sex or age by language. Adolescent patients ranged in age from 11 to 17 (M= 13.69).
Table 1.
Characteristics of parent/guardian respondents and their child, Dallas, TX, 2014–2015 (N = 223)
| Spanish | English | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Adolescent Age, years | 11.07 | 2.01 | 11.06 | 2.08 |
| N | % | N | % | |
| Adolescent Race/Ethnicity | ||||
| Hispanic | 129 | 57.9 | 22 | 9.8 |
| Non-Hispanic White | 2 | .9 | 3 | 1.4 |
| Non-Hispanic Black | 60 | 26.9 | ||
| Unknown race/ethnicity | 2 | .8 | 5 | 2.3 |
| Adolescent Sex | ||||
| Male | 67 | 30.1 | 50 | 22.4 |
| Female | 66 | 29.6 | 40 | 17.9 |
| Parent Education | ||||
| Less than high school | 52 | 23.4 | 3 | 1.4 |
| Some high school | 37 | 16.6 | 14 | 6.3 |
| High school/Vocational degree | 34 | 15.2 | 35 | 15.7 |
| Some college/College graduate | 10 | 4.4 | 38 | 17 |
Confirmatory Factor Analysis
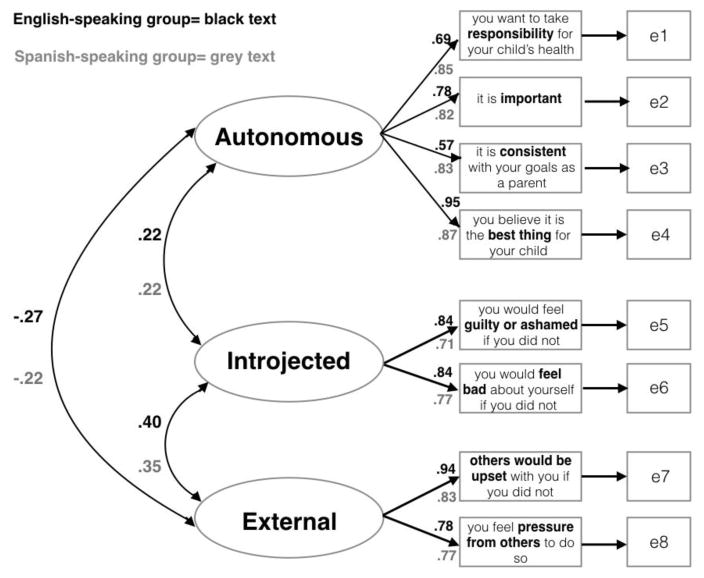
The three-factor model provided good fit to the data as demonstrated by strong fit indices, TLI= .963, CFI= .983, RMSEA= .040 [90% CI: .022, .057]. Each item loaded significantly onto its designated factor (see Figure 1) and the scales’ reliability were adequate (autonomous: α=.87; introjected: α=.72; external: α=.72). Bivariate correlations among the three factors were moderate, ranging from −.17 (autonomous and external) to .32 (introjected and external), suggesting that the three factors were discriminant from each other (Table 2).
Figure 1.
Two-group, 3-factor confirmatory factor analysis model and factor loadings for English and Spanish-speaking groups (latter in grey text)
Table 2.
Correlations among TSRQ subscales and other psychosocial determinants of HPV vaccine behavior
| Autonomous Motivation | Introjected Motivation | External Motivation | Self-Efficacy | Benefits | Intentions | Subjective Norms | |
|---|---|---|---|---|---|---|---|
| Autonomous Motivation | 1 | ||||||
| Introjected Motivation | .265** | 1 | |||||
| External Motivation | −.166* | .315** | 1 | ||||
| Self-Efficacy | .309** | .085 | −.031 | 1 | |||
| Benefits | .660** | .287** | −.046 | .302** | 1 | ||
| Intentions | .523** | .239** | .020 | .182** | .456** | 1 | |
| Subjective Norms | .125 | .251** | .344** | .145* | .115 | .090 | 1 |
p < .01;
p < .05
Factorial Invariance
We compared Model 1 (unconstrained allowing all factors, variances, and covariances to vary freely between English and Spanish language groups) to Model 2 (constrained factor loadings to be equal across groups). The χ2 difference test was statistically significant (p = .002; see Table 3), suggesting some items loaded differently between the groups. To determine which factor loadings were not equivalent, we tested sequential nested models with cumulatively constrained parameters (i.e., the unconstrained Model 1 is tested against models with constraints cumulatively added to individual parameters in each test) and found that Responsibility item (“…you want to take responsibility for your child’s health), on the autonomous factor, loaded more strongly for Spanish-compared to English-speakers (Δχ2 = 11.093, Δ df= 3, p= .01; see Figure 1). By allowing the model to freely estimate the Responsibility item factor, we achieved an equivalent measurement model across groups (Model 1 versus 3; see Table 3).
Table 3.
Confirmatory factor analyses testing the invariance of the three-factor model as applied to Spanish- and English-speaking participants
| Model | χ2 | df | CFI | RMSEA (90% CI) |
|---|---|---|---|---|
| 1. Unconstrained | 46.907** | 34 | .979 | .046 (.011, .072) |
| 2. Equality of Factor Loadings | 66.585** | 39 | .955 | .058 (.036, .079) |
| 3. Equality of Factor Loadings with Responsibility freely estimated | 49.875 | 38 | .984 | .038 (.000, .065) |
| Model Comparisons | χ2 difference | Difference df | p-value |
|---|---|---|---|
| Model 1 vs. Model 2 | 19.678 | 5 | .001 |
| Model 1 vs. Model 3 | 2.968 | 4 | .563 |
Discriminant Validity
To examine discriminant validity of the measure, we examined correlations between the various subscales and other measures related to motivation. Figure 1 shows the correlations between TSRQ subscales for both the Spanish- and English-speaking groups, and Table 2 shows correlations between the subscales, perceived benefits, subjective norms, self-efficacy and intentions for the overall sample. The direction and magnitude of correlations between the TSRQ subscales and other constructs followed our hypotheses. As expected, autonomous motivation had stronger correlations with perceived benefits, self-efficacy, and intentions to vaccinate than with subjective norms. In contrast, external motivation showed weaker correlations with perceived benefits, self-efficacy, and intentions to vaccinate than with subjective norms (see Table 2). Of note, the magnitude of the correlations between introjected motivation (which falls between autonomous and external motivation on the continuum) and the other psychosocial factors fell between the magnitude of the correlations of the psychosocial factors with autonomous and external motivation. Importantly, the expected pattern of correlations between more closely related subscales was demonstrated such that autonomous motivation was more highly correlated with introjected motivation than was external motivation (see Figure 1).
Discussion
The findings support the validity of the TSRQ as a measure to assess motivation to engage in HPV vaccination. CFAs replicated the underlying factor structure of the TSRQ demonstrated in previous work [8] across two different language groups. Results of the factorial invariance analyses support an equivalent structure across Spanish- and English-speaking populations. Only one item (“…because you want to take responsibility for your child’s health”) had a stronger factor loading for Spanish- than English-speakers. The scale will be useful in assessing motivation for HPV vaccination among clinical and research populations, and will allow researchers to examine it as a potential determinant of decision-making about the vaccine.
The results provide evidence for the validity of the TSRQ to assess parental motivation for HPV vaccination among adolescents through discriminant validity with other psychosocial determinants of vaccination, confirmatory factor analysis, and factorial invariance. Further, the pattern of correlations between the different types of motivation supports the hypothesized pattern of self-determination and is consistent with patterns seen in adaptations of the TSRQ to assess motivation for other health behaviors [8]. This modified, abbreviated version of the TSRQ to assess motivation in HPV vaccine may be beneficial in understanding the role of motivation in decision-making about the vaccine – an important factor to target in interventions and clinical interactions. For example, providers could tailor their recommendation style based on parental motivation (e.g., use a presumptive style with externally motivated parents) and/or facilitate parental autonomous motivation. Tailoring communication to parental motivation, however, presumes clinics and providers can screen parents on this construct. Feasibility of this screen and tailor approach is unknown. Facilitating parental autonomous motivation may be more feasible and effective because SDT-based clinical approaches such as motivational interviewing have increased autonomous motivation and changed behavior [19]. Further, SDT hypothesizes that increasing autonomous motivation leads to greater behavioral maintenance [20]. Thus, future research should examine whether intervention effects on HPV vaccine completion are larger when the intervention’s goal is to increase parental autonomous motivation versus encourage providers to tailor their recommendation style to parental motivation.
Consistent with SDT, autonomous motivation had a strong correlation with vaccination intentions (r = 0.52), whereas introjected motivation had a more moderate correlation (r = 0.24) and external motivation had no correlation (r = 0.02). These findings illustrate the importance of distinguishing between motivation types to better understand vaccine decisions. In addition, autonomous motivation in particular may be an important construct to integrate into theoretical models of health behavior, most of which focus on expectancy value-based beliefs (e.g., attitudes, perceived benefits [21,22]). Currently, SDT [20] is the only health behavior theory where autonomous motivation is a central construct. In terms of public health and clinical practice, the findings suggest that facilitating autonomous motivation is important in interventions and clinical encounters. However, future work comparing the effects of autonomous motivation and other factors on vaccine initiation and completion, and interventions designed to change autonomous motivation, are needed before clear conclusions can be drawn.
Past HPV vaccine studies have shown differences in vaccination rates and attitudes toward vaccination between non-Hispanics, Spanish-speaking Hispanics, and English-speaking Hispanics [9,23–25]. Thus, establishing an equivalent underlying structure between language groups was necessary. Our findings did not provide evidence to support different factorial structures between groups. The stronger loading of the responsibility item for Spanish-speakers suggests this item may more strongly capture what drives autonomous motivation for Spanish-speaking parents. Thus, responsibility for their children’s health may play the largest role in driving motivation to vaccinate for Spanish-speaking parents. Previous work on acculturation and vaccination demonstrated that more highly acculturated Hispanic individuals were less likely to vaccinate [26] due to decreases in parental sense of responsibility and attitudes toward vaccination [27]. In light of these previous findings, our measure demonstrating a strong sense of responsibility for their children’s health among the Spanish-speaking parents may indicate lower acculturation levels among the parents in our study.
One limitation of this study is the small number of items on each factor (e.g. two each for introjected and external motivation), as factors with fewer than three items are generally considered weak and unstable [28]. Despite this, we found good fit for the three-factor model. In addition, although the sample size was relatively small, it was adequate to conduct the factor analyses and invariance analyses needed to examine construct validity of the scales. Recruitment was also limited to individuals seen in safety-net clinics in one metropolitan area, thus caution is warranted in generalizing findings. Researchers could use our English and Spanish versions of the HPV vaccine TSRQ to examine if our findings replicate. Finally, the data were collected in a cross-sectional survey and did not examine predictive validity. However, the primary purpose of the study was to examine construct and concurrent validity of the motivation measures, and for these purposes, a cross-sectional design is sufficient.
Conclusions
In summary, analyses of the factor structure of the TSRQ to assess motivation for HPV vaccination provide evidence for the validity of the measure in this context and invariance across language. Our study provides health behavior researchers a useful measure to examine the role of motivation in HPV vaccination decision-making. Future research should examine the role of different types of motivation in initiation delay and poor completion of the three-dose vaccine series.
Highlights.
Motivation is a key determinant of initiation and maintenance of health behaviors, but lack of valid measures of motivation impedes its application to HPV vaccine decision-making.
The current study adapted the Treatment Self Regulation Questionnaire (TSRQ) to measure parental motivation for adolescent HPV vaccination among English- and Spanish-speaking parents.
Analyses of the factor structure of the TSRQ to assess motivation for HPV vaccination and its discriminant validity from other measures provide evidence for its validity in this context.
Acknowledgments
All phases of this study were supported by a grant funded by the National Cancer Institute (PIs: Tiro & Baldwin; 1R01CA178414). Additional support provided to Deanna Denman by a supplement to the parent grant (Denman; 3R01CA178414-02S1), the UTSW Center for Translational Medicine, through the NIH/National Center for Advancing Translational Sciences (UL1TR001105) and the Simmons Comprehensive Cancer Center (1P30 CA142543). The authors would like to acknowledge the support and cooperation received from the following individuals at Parkland Health and Hospital System, Dallas, TX, USA: Jonson Cha (data extraction); Susan Partridge, RN, Anna Barden, RN, Aletheia Miller, (administrative support for conducting research); Eden Pineda, RN, Kerrie Roberts Watterson, Eric Walker, Jane Hunley, Cesar Termulo, MD, Barbara Durso, MD, Trayce Robinson, MD, Susan Spalding, MD, Terri Jackson, PA, LaVonda McLennan, NP, April Campbell, PA, Teresa Garry, RN, Rhonda Anderson, RN, Levet Hamilton, RN, Cassandra Williams-Emanuel RN, Tammiko Jones (clinic site administrators, lead physicians/providers, and lead nurses). We also acknowledge Juan Mijares, Claudia Chavez, Sujehy Arredondo, Joanna Garcia, Meghan McKellar, and Caroline Mejias (UTSW) for recruitment, survey administration, and database development.
Footnotes
Conflict of Interest: All authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kennedy S, Goggin K, Nollen N. Adherence to HIV medications: Utility of the theory of self-determination. Cogn Ther Res. 2004;28:611–28. [Google Scholar]
- 2.Williams GC, McGregor HA, Zeldman A, Freedman ZR, Deci EL. Testing a self-determination theory process model for promoting glycemic control through diabetes self-management. Health Psychol. 2004;23:58. doi: 10.1037/0278-6133.23.1.58. [DOI] [PubMed] [Google Scholar]
- 3.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 4.Reagan-Steiner S, Yankey D, Jeyarajah J, Elam-Evans LD, Singleton JA, Curtis CR, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years–United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:784–92. doi: 10.15585/mmwr.mm6429a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dempsey AF, Abraham LM, Dalton V, Ruffin M. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human papillomavirus. Ann Epidemiol. 2009;19:531–8. doi: 10.1016/j.annepidem.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darden PM, Thompson DM, Roberts JR, Hale JJ, Pope C, Naifeh M, et al. Reasons for not vaccinating adolescents: National Immunization Survey of Teens, 2008–2010. Pediatrics. 2013;131:645–51. doi: 10.1542/peds.2012-2384. [DOI] [PubMed] [Google Scholar]
- 7.Williams GC, Minicucci DS, Kouides RW, Levesque CS, Chirkov VI, Ryan RM, et al. Self-determination, smoking, diet and health. Health Educ Res. 2002;17:512–21. doi: 10.1093/her/17.5.512. [DOI] [PubMed] [Google Scholar]
- 8.Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Educ Res. 2007;22:691–702. doi: 10.1093/her/cyl148. [DOI] [PubMed] [Google Scholar]
- 9.Watts LA, Joseph N, Wallace M, Rauh-Hain JA, Muzikansky A, Growdon WB, et al. HPV vaccine: A comparison of attitudes and behavioral perspectives between Latino and non-Latino women. Gynecol Oncol. 2009;112:577–82. doi: 10.1016/j.ygyno.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Tiro JA, Lee SC, Marks EG, Persaud D, Skinner CS, Street RL, et al. Developing a Tablet-Based Self-Persuasion Intervention Promoting Adolescent HPV Vaccination: Protocol for a Three-Stage Mixed-Methods Study. JMIR Res Protoc. 2016:5. doi: 10.2196/resprot.5092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bynum SA, Wigfall LT, Brandt HM, Richter DL, Glover SH, Hébert JR. Assessing the influence of health literacy on HIV-positive women’s cervical cancer prevention knowledge and behaviors. J Cancer Educ. 2013;28:352–6. doi: 10.1007/s13187-013-0470-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012;44:171–80. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerend MA, Barley J. Human papillomavirus vaccine acceptability among young adult men. Sex Transm Dis. 2009;36:58–62. doi: 10.1097/OLQ.0b013e31818606fc. [DOI] [PubMed] [Google Scholar]
- 14.Allen JD, Mohllajee AP, Shelton RC, Othus MK, Fontenot HB, Hanna R. Stage of adoption of the human papillomavirus vaccine among college women. Prev Med. 2009;48:420–5. doi: 10.1016/j.ypmed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Arbuckle J. AMOS 22. Users Guide. Chic IL: SmallWaters Corp; 2013. [Google Scholar]
- 16.Arbuckle JL. IBM SPSS Amos 19 user’s guide. Crawfordville FL: Amos Dev Corp; 2010. p. 635. [Google Scholar]
- 17.Wothke W, Arbuckle JL. Full-information missing data analysis with Amos. SPSS White Pap. 1996 [Google Scholar]
- 18.Byrne BM. Testing for multigroup invariance using AMOS graphics: A road less traveled. Struct Equ Model. 2004;11:272–300. [Google Scholar]
- 19.Ng JYY, Ntoumanis N, Thogersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, et al. Self-Determination Theory Applied to Health Contexts: A Meta-Analysis. Perspect Psychol Sci. 2012;7:325–40. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- 20.Ryan RM, Patrick H, Deci EL, Williams GC. Facilitating health behaviour change and its maintenance: Interventions based on self-determination theory. Eur Health Psychol. 2008;10:2–5. [Google Scholar]
- 21.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 22.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2:328–35. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 23.Baldwin AS, Bruce CM, Tiro JA. Understanding how mothers of adolescent girls obtain information about the human papillomavirus vaccine: Associations between mothers’ health beliefs, information seeking, and vaccination intentions in an ethnically diverse sample. J Health Psychol. 2013;18:926–38. doi: 10.1177/1359105312445078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chando S, Tiro JA, Harris TR, Kobrin S, Breen N. Effects of socioeconomic status and health care access on low levels of human papillomavirus vaccination among Spanish-speaking Hispanics in California. Am J Public Health. 2013;103:270–2. doi: 10.2105/AJPH.2012.300920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stevens CF, Caughy MO, Lee SC, Bishop WP, Tiro JA. Does language moderate the influence of information scanning and seeking on HPV knowledge and vaccine awareness and initiation among Hispanics? Ethn Dis. 2013;23:95–102. [PMC free article] [PubMed] [Google Scholar]
- 26.Anderson LM, Wood DL, Sherbourne CD. Maternal acculturation and childhood immunization levels among children in Latino families in Los Angeles. Am J Public Health. 1997;87:2018–21. doi: 10.2105/ajph.87.12.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prislin R, Suarez L, Simpson DM, Dyer JA. When acculturation hurts: the case of immunization. Soc Sci Med. 1998;47:1947–56. doi: 10.1016/s0277-9536(98)00336-0. [DOI] [PubMed] [Google Scholar]
- 28.Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10:7. [Google Scholar]