Abstract
AIM
To evaluate the effects of posterior corneal surface measurements on the accuracy of total estimated corneal astigmatism.
METHODS
Fifty-seven patients with toric intraocular lens (IOL) implantation and posterior corneal astigmatism exceeding 0.5 diopter were enrolled in this retrospective study. The keratometric astigmatism (KA) and total corneal astigmatism (TA) were measured using a Pentacam rotating Scheimpflug camera to assess the outcomes of AcrySof IOL implantation. Toric IOLs were evaluated in 26 eyes using KA measurements and in 31 eyes using TA measurements. Preoperative corneal astigmatism and postoperative refractive astigmatism were recorded for statistical analysis. The cylindrical power of toric IOLs was estimated in all eyes.
RESULTS
In all cases, the difference of toric IOL astigmatism magnitude between KA and TA measurements for the estimation of preoperative corneal astigmatism was statistically significant. Of a total of 57 cases, the 50.88% decreased from Tn to Tn-1, and 10.53% decreased from Tn to Tn-2. In all cases, 5.26% increased from Tn to Tn+1. The mean postoperative astigmatism within the TA group was significantly lower than that in the KA group.
CONCLUSION
The accuracy of total corneal astigmatism calculations and the efficacy of toric IOL correction can be enhanced by measuring both the anterior and posterior corneal surfaces using a Pentacam rotating Scheimpflug camera.
Keywords: cornea, astigmatism, cataract, intraocular lenses, refractive errors, rotating Scheimpflug camera
INTRODUCTION
Corneal astigmatism is one of the most common optical aberrations of the cornea. It has been reported that between 15% and 50% of cataract patients exhibit 1 diopter (D) to 2 D corneal astigmatism[1]–[3]. Corneal astigmatism is commonly attributed to postoperative uncorrected visual acuity after cataract extraction. Toric intraocular lens (IOL) implantation can correct pre-existing corneal astigmatism in patients undergoing cataract surgery[4]–[5]. The key requirement in IOL implantation is accurate calculations of cylinder power and toric IOLs and correct alignment in order to neutralize astigmatism in the cornea. Misalignment by 1̊ reduces the efficacy of astigmatism correction by 3.3%[5]–[7]. Keratometric astigmatism (KA) can be measured by a variety of techniques such as the utilization of a manual keratometer or automatic keratometer, corneal topography, and IOLMaster[8]–[10]. KA is the most commonly used method and is based solely on measurement of the anterior corneal curvature, through the assessment of the reflection of keratometric mires from the anterior corneal surface. However, the power of KA does not represent the power of total corneal astigmatism (TA) in which both the anterior and posterior corneal surfaces are be taken into account. Furthermore, obtaining measurements of the posterior corneal surface has been previously shown to be very difficult in clinical settings[11]–[12].
Recently, an anterior corneal measurement method was developed using the keratometric index (1.3375) that omits the posterior corneal surface measurement[13]. Both the anterior and posterior corneal surfaces contribute to TA; omitting the posterior corneal surface would lead to a significant deviation from the actual corneal power estimation prior to surgery[13]–[16]. Cheng et al[15] and Ho et al[16] recently reported that neglecting the posterior corneal surface measurement in the calculation of the TA would lead to significant inaccuracies during the estimation of the TA magnitude or axis in some eyes.
The placido-optical coherence tomography device and motion-corrected optical coherence tomography drastically shortens measurement time owing to a faster scan rate and a significantly reduced influence of motion artifacts[17]–[19]. The Pentacam rotating Scheimpflug camera (Oculus, Wetzlar, Germany) can provide biometric information on the anterior and posterior corneal surfaces and the anterior chamber[20]–[23]. In this study, we used both anterior and posterior corneal surface measurements, derived from Pentacam scanning, to estimate corneal astigmatism. The accuracy of calculating AcrySof toric IOL type by TA and KA measurements was also evaluated. The main objective of this study was to evaluate the outcome of astigmatism correction with toric IOL implantation. Therefore, visual acuity and refraction were not the main outcomes.
SUBJECTS AND METHODS
Patients who had undergone ArcySof toric IOL (Alcon, Fort Worth, TX, USA) implantation and phacoemulsification, with the astigmatism of the posterior corneal surface exceeding 0.5 D, in the Second Hospital of Hebei Medical University were enrolled in the study. This study was conducted in accordance with the Declaration of Helsinki and with approval from the Ethics Committee of the Second Hospital of Hebei Medical University. Written informed consent was obtained from all participants. Patients with corneal irregular astigmatism, retinal disease, intraoperative complications, posterior capsule opacification, or toric IOL misalignment were excluded. Poor quality Pentacam scans was also an exclusion criterion.
Prior to cataract extraction, patients underwent a variety of ophthalmologic examinations including slit lamp microscope examination, applanation tonometry, indirect ophthalmoscopy, keratometry, and Pentacam scanning. The axial length was measured by an optical biometer (IOLMaster) or by ultrasonic immersion biometry (for patients with dense cataracts). Keratometry data were derived from the Pentacam rotating Scheimpflug camera. The flat and steep central radius and meridian in the 3 mm zone on the anterior and posterior corneal surfaces, and the central corneal thickness were measured. Residual astigmatism results were obtained with subjective and objective refraction at 3mo postoperatively.
Astigmatism and Spherical Equivalent Measurements Omitting the Posterior Corneal Surface
The anterior corneal surface acts as a positive lens, while the posterior corneal surface acts as a negative lens due to the reduction of refractive indices (n) from the cornea to aqueous humour. The corneal refractive index (nc) and aqueous humor refractive index (na) was 1.376 and 1.336, respectively. The flat meridian was used for vector addition since a positive magnitude was required for defining the posterior corneal astigmatism. Astigmatism and the spherical equivalent (SE) were measured by KA, omitting the posterior corneal surface.
The refractive index was n = 1.3375:
KA = [(nc−1)/ Rs,front− (nc−1)/ Rf,front] ×1000@As,front;
SE = 1/2[(n−1)/ Rs,front+ (n−1)/ Rf,front] ×1000.
Where, Rs,front, is the steep meridian radius of the anterior corneal; Rf,front, is the flat meridian radius of the anterior corneal.
Total Corneal Astigmatism Measurements Incorporating the Posterior Corneal Surface
Ho's formula[16] was used to calculate the refractive power of the anterior and posterior corneal surfaces. The powers of the steep and flat meridian on the anterior corneal surface were calculated by (nc−1)/ Rs,front and (nc−1)/Rf,front. The powers of the posterior corneal surface were calculated by (na−nc)/Rs,back and (na−nc)/Rf,back. The SE of the anterior and posterior corneal surfaces were determined as follows:
SEfront = 1/2[(nc−1)/ Rs,front + (nc−1)/ Rf,front] ×1000;
SEback = 1/2[(na−nc)/ Rs,back + (na−nc)/ Rf,back] ×1000.
Where, nc is the refractive index of the cornea (nc=1.376); na is the refractive index of the aqueous humor (na=1.336)[24]; Rs,back is the steep meridian radius of the posterior corneal; Rf,back is the flat meridian radius of the posterior corneal.
The SE of the total cornea (SEtotal) was calculated by the thick lens formula as follows, where d is the central corneal thickness:
The cylinder powers of astigmatism on the anterior corneal surface and posterior corneal surface were described as follows:
Cfront = [(nc−1)/Rs,front − (nc−1)/ Rf,front]*1000;
Cback = [(na−nc)/Rf,back − (na−nc)/ Rs,back]*1000.
The vector summation was used to calculate the TA, including the posterior corneal measurement. The combined effect of two obliquely crossed cylinders on the anterior and posterior corneal surface was analyzed by the Holladay-Cravy-Koch formula. The formula was used for calculating the crossed cylinders in contact with a theoretical plane. However, according to the vertex distance formula, below, since only a small change in focus was caused by an average corneal thickness of 0.5 mm, this variable could be disregarded.
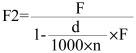 |
We calculated the vertex of both surfaces on the anterior corneal plane without conversion, according to Holladay-Cravy-Koch formula[25]:
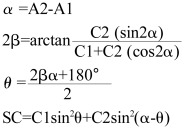 |
The TA was described as C3@A3
Magnitude of the Astigmatic Power Vector[16],[26]
The residual astigmatism data were described by two cylinder J0 and J45 [16],[26]. The following formulae were used where C was residual cylinder power and α was the axis:
J0=−(Ccos2α)/2, J45=−(Csin2α)/2
The vector from the origin to J0and J45 was termed the astigmatic power vector. The magnitude of the power was derived using the formulae:
Astigmatic power vector=(J02+J452)1/2
The magnitude of the power vector were used to compare the difference of the magnitude of residual cylinder between two groups.
Toric Intraocular Lens Calculations
The intended target of the postoperative D was emmetropia. The SE of the IOLs was calculated using the SRK/T formula. An online toric IOL calculator was utilized for calculating the cylinder power and alignment axis (available at: http://www.acrysoftoriccalculator.com).
Surgical Procedures
Prior to surgery, meridians at 0° and 180° were marked on the corneal limbus when the patients were sitting up straight and looking ahead. The targeted implantation axis was marked during the operation. The same operation was performed in all cataract extractions with a standard two-plane 3 mm incision created 110° above the clear cornea. Following a divide-and-conquer nucleofractis and cortex removal, the AcrySof toric IOL was injected through the incision using a Monarch II injector (Alcon Laboratories Inc.). Subsequently, the cylindrical axis of the IOL aligned with the limbal axis marks by rotating the IOL. Examinations including uncorrected visual acuity and best spherical corrected visual acuity, slit lamp microscope examination, applanation tonometry, Pentacam scans, and automated and manifest refraction were performed at the 1 and 3mo postoperative visits. The postoperative axis of the toric IOL was measured using the slit lamp when the patient was sitting straight.
Statistical Analysis
Mean astigmatism was compared between the TA and KA groups using the paired t-test. Preoperative and postoperative astigmatism was compared between the TA and KA groups using the independent sample t-test.
RESULTS
Demographics and Preoperative Data
The mean±standard deviation (SD) patient age was 62.7±12.9y (range: 28-86y). The mean SE±SD of the total corneal powers and keratometric corneal powers was 42.7±3.7 D (range: 38.2 D-48.0 D) and 44.0±3.4 D (range: 39.7 D-48.2 D), respectively.
Keratometric Corneal Astigmatism and Total Corneal Astigmatism Magnitude and Meridian
TA and KA were measured for each of the 57 cases. The mean±SD astigmatism of the TA and KA was 1.57±0.56 D×90.92° (range: 0.9 D-3.7 D) and 2.01±0.61 D×85.55° (range: 1.3 D-4.3 D), respectively. There was a statistically significant difference between TA and KA magnitude (P<0.0001, paired t-test).
Posterior Corneal Astigmatism Magnitude and Meridian
The mean±SD posterior corneal astigmatism of the 57 cases was 0.61±0.14 D×15.71° (range: 0.5 D-1.2 D).
Functions of Total Corneal Astigmatism Posterior and Anterior Magnitude
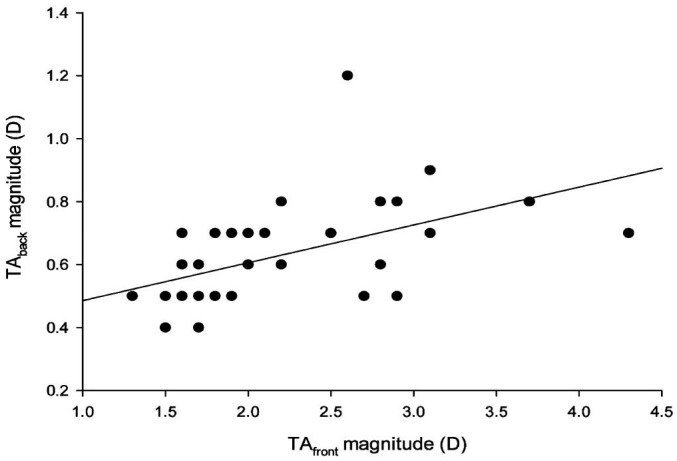
Figure 1 presents a scattergram illustrating the functions of TAback magnitude and TAfront magnitude. The regression formula comprised: (TAback magnitude)=0.107×(TAfront magnitude)+0.365 (r=0.531, P<0.0001).
Figure 1. Scattergram of the TAback magnitude as a function of the TAfront magnitude.
The regression formula was (TAback magnitude)= 0.107×(TAfront magnitude) +0.365 (r=0.531, P<0.0001).
The posterior corneal astigmatism measurement resulted in a mean reduction of 0.44±0.26 D (range:−0.3 D to1 D) and a mean percentage reduction of 21.86%±13.59% (range: 20%-38.89%) in the anterior corneal astigmatism magnitude.
Estimation of Total Corneal Astigmatism and Keratometric Corneal Astigmatism Magnitude and Angle Measurements
The estimation results of the TA and KA measurements in all of the 57 enrolled eyes were summarized. The mean arithmetic error of the magnitude between KA and TA was 0.44±0.26 D (range: −0.3D to 1D). Among the 57 eyes, 8 (14.04%) and 40 (70.18%) had a KA magnitude that was within ±0.25 D and±0.50 D of the TA magnitude, respectively. Seventeen eyes (29.8%) had a KA magnitude greater than ±0.50 D of the TA magnitude. The mean arithmetic errors of the KA angle for the TA angle was 0.94°±10.06° (range: −42.8° to 18°). There was no significant difference between the TA and KA angle (P=0.919, paired t-test). Twenty-five eyes (43.86%) and 44 eyes (77.19%) had a KA angle that was within ±5° and ±10° of the TA angle, respectively.
Change of Toric Intraocular Lens Type Calculated with Total Corneal Astigmatism and Keratometric Corneal Astigmatism
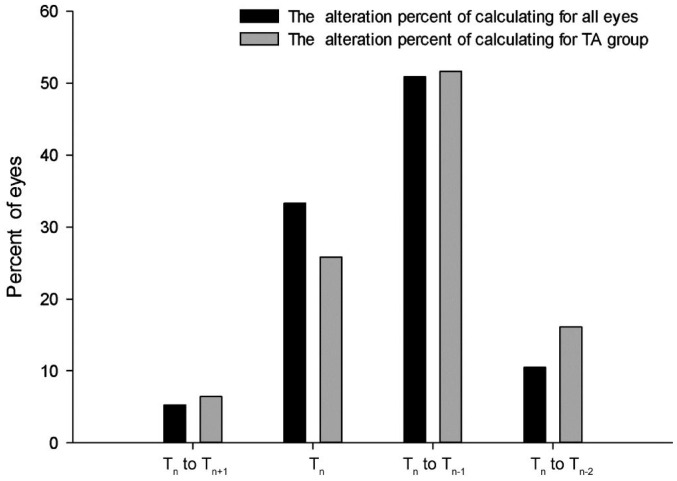
We classified all of the 57 cases according to toric IOL type with TA and KA. Table 1 shows that three eyes (5.26%) increased from Tn to Tn+1, 19 eyes (33.33%) remained the same, 29 eyes (50.88%) decreased from Tn to Tn−1, and 6 eyes (10.53%) decreased from Tn to Tn−2. Toric IOL implantation became unnecessary for seven eyes according to the reduction in astigmatism magnitude.
Table 1. The types of AcrySof toric IOL calculated retrospectively and preoperatively.
| Parameters | No. of eyes | Non-Toric | T3 | T4 | T5 | T6 | T7 | T8 |
| Calculated with KA retrospectively | 57 | 0 | 17 | 14 | 16 | 4 | 5 | 1 |
| Calculated with TA retrospectively | 57 | 7 | 17 | 22 | 5 | 5 | 1 | 0 |
Non-Toric: The toric IOL was unnecessary according to the result of a Web-based AcrySof toric IOL calculator; KA: Keratometric astigmatism; TA: Total corneal astigmatism.
Toric Intraocular Lens Implantation Surgical Outcomes
Among the 57 eyes that underwent toric IOL implantation for astigmatism correction, 26 cases were assessed with KA and 31 cases were assessed with TA. The mean astigmatism of the TA and KA groups was 1.65 D±0.67 D × 86.58° and 1.91±0.39 D × 95.91°, respectively. There was no significant difference in magnitude between the two groups preoperatively (P=0.08887, t-test).
For the TA group, we also calculated the type of ArySof toric IOLs with KA. The type of toric IOL for two eyes (6.45%) changed from Tn to Tn+1, eight eyes (25.81%) remained the same, 16 eyes (51.62%) changed from Tn to Tn−1, and five eyes (16.13%) changed from Tn to Tn−2. According to KA calculations, toric IOL implantation became unnecessary for five eyes in the TA group. Figure 2 shows the percentage alteration in all 57 summarized eyes and in the TA group. Out of 57 eyes, three eyes (5.26%) increased from Tn to Tn+1, 19 eyes (33.33%) remained the same, 29 eyes (50.88%) decreased from Tn to Tn−1, and 6 eyes (10.53%) decreased from Tn to Tn−2. For the TA group, the type of toric IOL for 2 eyes changed (6.45%) from Tn to Tn+1, 8 eyes (25.81%) remained the same, 16 eyes (51.62%) changed from Tn to Tn−1, and five eyes (16.13%) changed from Tn to Tn−2.
Figure 2. The alteration percent of calculating in theory for all eyes and TA group.
The cases of 29 eyes (50.88%) decreased from Tn to Tn−1, 19 eyes (33.33%) remained the same, 6 (10.53%) decreased from Tn to Tn−2, and 3 eyes (5.26%) in all cases increased from Tn to Tn+1. According to the decreased magnitude of astigmatism, 7 eyes became unnecessary for toric IOL.
Residual Astigmatism Postoperative Outcomes
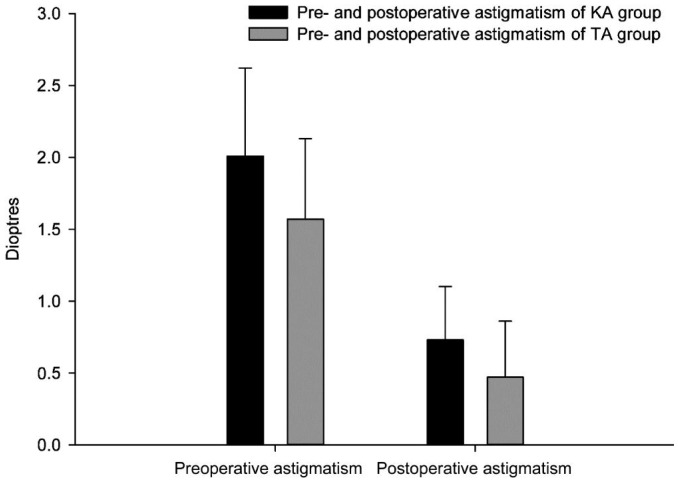
We measured the residual astigmatism of the TA and KA groups at 3mo postoperatively. The residual astigmatism of TA was 0.47±0.39 D×75.45° (range: 0 D-1.5 D). The residual astigmatism of KA was 0.73±0.37 D×96.32° (range: 0.25 D-1.5 D). Figure 3 summarizes the preoperative and postoperative astigmatism results according to the two different groups. In the TA group, the magnitude of the residual astigmatic power vector was 0.21±0.19 D. In the KA group, the magnitude of the residual astigmatic power vector was 0.38±0.18 D. There was a significant difference in the magnitude of astigmatism between the TA and KA group (P=0.022, t-test).
Figure 3. The preoperative and postoprative astigmatism of between TA and KA group.
There is no statistical significance between the two groups for the preoperative astigmatism magnitude. The postoperative astigmatic power vector is significantly lower in the TA group compared with the KA group (P=0.022, t-test).
We performed a correlation analysis between the posterior corneal surface astigmatism (Aback) and postoperative astigmatic shift (Ashift) for the TA and KA groups. The postoperative astigmatic shift comprised the deviation of residual postoperative astigmatism from the toric IOL calculator. In the TA group, the posterior corneal surface astigmatism was 0.71±0.19 D (range: 0.5 D-1.2 D) and the postoperative astigmatic shift was 0.38±0.26 D (range: 0 D-0.8 D). There was no significant correlation between posterior corneal surface astigmatism and postoperative astigmatic shift (r=0.2145, P>0.05). In the KA group, the posterior corneal surface astigmatism was 0.66±0.29 D (range: 0.5 D-1.2 D) and the postoperative astigmatic shift was 0.61±0.33 D (range: 0.4 D-1.1 D). There was a significant correlation between posterior corneal surface astigmatism and postoperative astigmatic shift (r=0.642, P<0.05). The regression formula was (Ashift)=0.712×Aback +0.214 (r=0.642, P<0.05).
DISCUSSION
The main finding of this study is that determination of the AcrySof toric IOLs through TA measurements significantly reduces postoperative keratometric-associated astigmatism (that is frequently the result of omitting astigmatism measurements on the posterior corneal surface). It is very important to accurately measure the magnitude and axis of corneal astigmatism when determining the AcrySof toric IOL type. However, both the anterior and posterior corneal surfaces contribute to the TA. Conventionally, the corneal astigmatism is obtained from measuring the curvature of the anterior cornea whilst omitting the curvature of the posterior corneal. This may be due to the difficulty in measuring the posterior corneal curvature based on the Purkinje images in a clinical setting[11],[27]–[28]. Another potential reason may be that the posterior corneal astigmatism is so small that it could be easily be overlooked. The difference in the refractive indices from the posterior corneal surface to the aqueous humor (1.336−1.376= −0.04) was relatively small compared with that from the air to the anterior corneal surface (1.376−1=0.376).
Dunne et al[29] found that the toricity anterior to posterior ratio was significantly lower in the vertical direction than in the horizontal direction. This indicated that the posterior corneal surface exhibits greater toricity than the anterior surface on some radii. Therefore, astigmatism of the posterior surface on some radii may be elevated compared with the anterior surface[30]. The ratio of posterior to anterior surface astigmatism was 0.33 in Mas et al's[31] study, while Oshika et al[32] obtained a mean ratio of 0.35. In our study, the regression formula comprised TAback magnitude=0.107× (TAfront magnitude) +0.365; this is very similar to Ho's finding of PAback magnitude = 0.0998×(PAfront magnitude)+0.3073[16]. The convergence induced by the anterior corneal surface could be partially neutralized by the negative dioptric power of the posterior surface due to the reduction of the refractive indices across the corneal stroma to the aqueous humor (1.376−1.336= −0.04). Previous studies have shown that in 77.1% to 81.7% of eyes, posterior corneal surface astigmatism resulted in a reduction of TA and an average reduction in the astigmatism of the anterior corneal surface by 12.9% to 31.0%[33]. Koch et al[34] analyzed 715 corneas using ray tracing and found that the mean magnitude of posterior corneal astigmatism was −0.30 D. The posterior corneal surface astigmatism exceeded 0.50 D in 9% of eyes.
Astigmatism correction outcomes were affected by regular corneal astigmatism, the accuracy of toric IOL types, and rotational stability. Surgically induced astigmatism (SIA) is an important factor for the accurate correction of corneal astigmatism. The IOL calculator program calculated the type of toric IOL to be implanted by taking both the preoperative corneal astigmatism magnitude and the SIA (which in our cases was 0.5 D) into account. The vector calculation of SIA will slightly increase or reduce the difference when the direction of astigmatism for a given eye varies from either against the rule astigmatism (ART) or with the rule astigmatism (WRT). Karunaratne [10] and Ahmed et al[35] found that 51% eyes with preoperative WTR astigmatism changed in ATR astigmatism, and 34.1% of ATR changed in WTR after the toric IOL implantation. With regards to the direction of the preoperative corneal astigmatism, there was no significant effect when the toric IOL was implanted. It appears that toric IOLs can sufficiently correct large astigmatism, while any relative SIA included in the calculation program can induce a low amount of astigmatism but does not affect the final outcome.
In this study, we found that the inclusion of posterior corneal surface astigmatism reduced astigmatism in 21.86% cases. Out of the 57 eyes, 70.18% had a KA magnitude within ±0.50 D of the TA magnitude and 77.19% had a KA angle within ±10° of the TA angle. The alteration of the toric IOL type was calculated with TA and KA; 50.88% decreased from Tn to Tn−1 and 10.53% decreased from Tn to Tn−2, retrospectively. Toric IOL implantation could be avoided in seven eyes according to the reduction in pre-existing astigmatism after the posterior corneal measurement was considered. This finding may explain some of the unpredictable results associated with toric IOL implantation when omitting the posterior corneal surface measurement.
The surgical prognosis related to the reduction of the postoperative residual refractive cylinder is influenced by the accurate estimation of the TA and its axis. The efficacy of astigmatism correction can be reduced by 3.3% due to 1° of misalignment[5]–[7]. Posterior corneal surface astigmatism has been reported to cause between 2.63° to 7.40° of change in the axis[24]. In our study, the mean arithmetic estimation error was 0.94±10.06° (range: −42.8° to 18°) and the mean absolute estimation error was 7.24±7.00° (range: 0.1°-42.8°); however, there was no significant difference between the TA and KA angle.
Eyes with a posterior corneal astigmatism exceeding 0.5 D were enrolled in this study. The AcrySof toric IOL offers different cylinder powers at 0.5 D intervals. Therefore, posterior corneal surface astigmatism less than 0.5 D may be too weak to affect the determination of AcrySof toric IOLs. In our study, the residual refractive cylinder was smaller in the TA group (0.47±0.39 D) than in the KA group (0.72±0.53 D). However, there was a significant difference in the magnitude of astigmatism between the TA and KA groups. In summary, we found that omitting the posterior corneal surface measurement leads to inaccuracy in the estimation of the magnitude of the TA in some eyes that have received toric IOL implantation. When a Pentacam rotating Scheimpflug camera is used to measure anterior and posterior corneal surfaces simultaneously, calculation of TA will improve the prediction of the corneal astigmatism, and therefore enhance the efficacy of astigmatism correction with toric IOLs.
In conclusion, the accuracy of TA, with a posterior surface astigmatism exceeding 0.5 D, and the efficacy of toric IOL correction can be enhanced by measuring both anterior and posterior corneal surfaces with a Pentacam rotating Scheimpflug camera.
Acknowledgments
Conflicts of Interest: Zhang B, None; Ma JX, None; Liu DY, None; Guo CR, None; Du YH, None; Guo XJ, None; Cui YX, None.
REFERENCES
- 1.Mashige KP, Jaggernath J, Ramson P, Martin C, Chinanayi FS, Naidoo KS. Prevalence of refractive errors in the INK area, Durban, South Africa. Optom Vis Sci. 2016;93(3):243–250. doi: 10.1097/OPX.0000000000000771. [DOI] [PubMed] [Google Scholar]
- 2.De Bernardo M, Zeppa L, Cennamo M, Iaccarino S, Zeppa L, Rosa N. Prevalence of corneal astigmatism before cataract surgery in Caucasian patients. Eur J Ophthalmol. 2014;24(4):494–500. doi: 10.5301/ejo.5000415. [DOI] [PubMed] [Google Scholar]
- 3.Yuan X, Song H, Peng G, Hua X, Tang X. Prevalence of corneal astigmatism in patients before cataract surgery in Northern China. J Ophthalmol. 2014;2014:536412. doi: 10.1155/2014/536412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iovieno A, Yeung SN, Lichtinger A, Alangh M, Slomovic AR, Rootman DS. Cataract surgery with toric intraocular lens for correction of high corneal astigmatism. Can J Ophthalmol. 2013;48(4):246–250. doi: 10.1016/j.jcjo.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg. 2008;34(10):1631–1636. doi: 10.1016/j.jcrs.2008.04.041. [DOI] [PubMed] [Google Scholar]
- 6.Eom Y, Rhim JW, Kang SY, Kim SW, Song JS, Kim HM. Toric intraocular lens calculations using ratio of anterior to posterior corneal cylinder power. Am J Ophthalmol. 2015;160(4):717–724.e2. doi: 10.1016/j.ajo.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Novis C. Astigmatism and toric intraocular lenses. Curr Opin Ophthalmol. 2000;11(1):47–50. doi: 10.1097/00055735-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Chang M, Kang SY, Kim HM. Which keratometer is most reliable for correcting astigmatism with toric intraocular lenses? Korean J Ophthalmol. 2012;26(1):10–14. doi: 10.3341/kjo.2012.26.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hashemi H, Asgari S, Miraftab M, Emamian MH, Shariati M, Fotouhi A. Agreement study of keratometric values measured by Biograph/LENSTAR, auto-kerato-refractometer and Pentacam: decision for IOL calculation. Clin Exp Optom. 2014;97(5):450–455. doi: 10.1111/cxo.12186. [DOI] [PubMed] [Google Scholar]
- 10.Karunaratne N. Comparison of the Pentacam equivalent keratometry reading and IOL Master keratometry measurement in intraocular lens power calculations. Clin Experiment Ophthalmol. 2013;41(9):825–834. doi: 10.1111/ceo.12124. [DOI] [PubMed] [Google Scholar]
- 11.Lam AK, Douthwaite WA. A pilot study on the measurement of central posterior corneal radius in Hong Kong Chinese using Purkinje image technique. Ophthalmic Physiol Opt. 1997;17(1):68–74. [PubMed] [Google Scholar]
- 12.Leyland M. Validation of Orbscan II posterior corneal curvature measurement for intraocular lens power calculation. Eye(Lond) 2004;18(4):357–360. doi: 10.1038/sj.eye.6700659. [DOI] [PubMed] [Google Scholar]
- 13.Wang L, Booth MA, Koch DD. Comparison of intraocular lens power calculation methods in eyes that have undergone LASIK. Ophthalmology. 2004;111(10):1825–1831. doi: 10.1016/j.ophtha.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 14.Kamiya K, Shimizu K, Igarashi A, Miyake T. Assessment of anterior, posterior, and total central corneal astigmatism in eyes with keratoconus. Am J Ophthalmol. 2015;160(5):851–857.e1. doi: 10.1016/j.ajo.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Cheng LS, Tsai CY, Tsai RJ, Liou SW, Ho JD. Estimation accuracy of surgically induced astigmatism on the cornea when neglecting the posterior corneal surface measurement. Acta Ophthalmol. 2011;89(5):417–422. doi: 10.1111/j.1755-3768.2009.01732.x. [DOI] [PubMed] [Google Scholar]
- 16.Ho JD, Tsai CY, Liou SW. Accuracy of corneal astigmatism estimation by neglecting the posterior corneal surface measurement. Am J Ophthalmol. 2009;147(5) doi: 10.1016/j.ajo.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 17.Viswanathan D, Kumar NL, Males JJ, Graham SL. Comparative analysis of corneal measurements obtained from a Scheimpflug camera and an integrated Placido-optical coherence tomography device in normal and keratoconic eyes. Acta Ophthalmol. 2015;93(6):e488–494. doi: 10.1111/aos.12622. [DOI] [PubMed] [Google Scholar]
- 18.McNabb RP, Farsiu S, Stinnett SS, Izatt JA, Kuo AN. Optical Coherence Tomography Accurately Measures Corneal Power Change from Laser Refractive Surgery. Ophthalmology. 2015;122(4):677–686. doi: 10.1016/j.ophtha.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ueno Y, Hiraoka T, Miyazaki M, Ito M, Oshika T. Corneal thickness profile and posterior corneal astigmatism in normal corneas. Ophthalmology. 2015;122(6):1072–1078. doi: 10.1016/j.ophtha.2015.01.021. [DOI] [PubMed] [Google Scholar]
- 20.Kovács I, Miháltz K, Ecsedy M, Németh J, Nagy ZZ. The role of reference body selection in calculating posterior corneal elevation and prediction of keratoconus using rotating Scheimpflug camera. Acta Ophthalmol. 2011;89(3):e251–256. doi: 10.1111/j.1755-3768.2010.02053.x. [DOI] [PubMed] [Google Scholar]
- 21.Fukuda S, Beheregaray S, Hoshi S, Yamanari M, Lim Y, Hiraoka T, Yasuno Y, Oshika T. Comparison of three-dimensional optical coherence tomography and combining a rotating Scheimpflug camera with a Placido topography system for forme fruste keratoconus diagnosis. Br J Ophthalmol. 2013;97(12):1554–1559. doi: 10.1136/bjophthalmol-2013-303477. [DOI] [PubMed] [Google Scholar]
- 22.Huang J, Lu W, Savini G, Hu L, Pan C, Wang J, Tan W, Chen J, Wang Q. Evaluation of corneal thickness using a Scheimpflug-Placido disk corneal analyzer and comparison with ultrasound pachymetry in eyes after laser in situ keratomileusis. J Cataract Refract Surg. 2013;39(7):1074–1080. doi: 10.1016/j.jcrs.2013.01.038. [DOI] [PubMed] [Google Scholar]
- 23.Ho JD, Tsai CY, Tsai RJ, Kuo LL, Tsai IL, Liou SW. Validity of the keratometric index: evaluation by the Pentacam rotating Scheimpflug camera. J Cataract Refract Surg. 2008;34(1):137–145. doi: 10.1016/j.jcrs.2007.09.033. [DOI] [PubMed] [Google Scholar]
- 24.Speicher L. Intra-ocular lens calculation after corneal refractive surgery. Curr Opin Ophthalmol. 2001;12(1):17–29. doi: 10.1097/00055735-200102000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Holladay JT, Cravy TV, Koch DD. Calculating the surgically induced refractive change following ocular surgery. J Cataract Refract Surg. 1992;18(5):429–443. doi: 10.1016/s0886-3350(13)80095-8. [DOI] [PubMed] [Google Scholar]
- 26.Statham M, Apel A, Stephensen D. Comparison of the AcrySof SA60 spherical intraocular lens and the AcrySof Toric SN60T3 intraocular lens outcomes in patients with low amounts of corneal astigmatism. Clin Experiment Ophthalmol. 2009;37(8):775–779. doi: 10.1111/j.1442-9071.2009.02154.x. [DOI] [PubMed] [Google Scholar]
- 27.Turuwhenua J, Henderson J. The recovery of posterior cornea and anterior lens radii by a novel ray-tracing method. Optom Vis Sci. 2004;81(11):884–894. doi: 10.1097/01.opx.0000145025.65160.78. [DOI] [PubMed] [Google Scholar]
- 28.Garner LF, Owens H, Yap MK, Frith MJ, Kinnear RF. Radius of curvature of the posterior surface of the cornea. Optom Vis Sci. 1997;74(7):496–498. doi: 10.1097/00006324-199707000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Dunne MC, Royston JM, Barnes DA. Posterior corneal surface toricity and total corneal astigmatism. Optom Vis Sci. 1991;68(9):708–710. doi: 10.1097/00006324-199109000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Nemeth G, Berta A, Lipecz A, Hassan Z, Szalai E, Modis L., Jr Evaluation of posterior astigmatism measured with Scheimpflug imaging. Cornea. 2014;33(11):1214–1218. doi: 10.1097/ICO.0000000000000238. [DOI] [PubMed] [Google Scholar]
- 31.Mas D, Espinosa J, Domenech B, Perez J, Kasprzak H, Illueca C. Correlation between the dioptric power, astigmatism and surface shape of the anterior and posterior corneal surfaces. Ophthalmic Physiol Opt. 2009;29(3):219–226. doi: 10.1111/j.1475-1313.2008.00632.x. [DOI] [PubMed] [Google Scholar]
- 32.Oshika T, Tomidokoro A, Tsuji H. Regular and irregular refractive powers of the front and back surfaces of the cornea. Exp Eye Res. 1998;67(4):443–447. doi: 10.1006/exer.1998.0558. [DOI] [PubMed] [Google Scholar]
- 33.Giessler S, Duncker GI. Orbscan pachymetry after LASIK is not reliable. J Refract Surg. 2001;17(3):385–387. doi: 10.3928/1081-597X-20010501-12. [DOI] [PubMed] [Google Scholar]
- 34.Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080–2087. doi: 10.1016/j.jcrs.2012.08.036. [DOI] [PubMed] [Google Scholar]
- 35.Ahmed II, Rocha G, Slomovic AR, Climenhaga H, Gohill J, Grégoire A, Ma J, Canadian Toric Study Group Visual function and patient experience after bilateral implantation of toric intraocular lenses. J Cataract Refract Surg. 2010;36(4):609–616. doi: 10.1016/j.jcrs.2009.10.044. [DOI] [PubMed] [Google Scholar]