Abstract
AIM
To assess the effects of upper lid blepharoplasty on visual quality.
METHODS
Seventy-three eyelids of 39 patients were subjected to upper lid blepharoplasty. Pre- and post-operative contrast sensitivity, visual acuity, vertical palpebral aperture and the degree of lash ptosis were measured.
RESULTS
The mean log contrast sensitivities under photopic (P=0.017) and scotopic conditions (P=0.009) were improved after surgery, and these differences were significant. The degree of lash ptosis was also decreased after blepharoplasty (P<0.001).
CONCLUSION
In our study, a significant increase in contrast sensitivity was found after surgery. These results suggest that upper lid blepharoplasty can be helpful for improving visual quality.
Keywords: blepharoplasty, visual quality, contrast sensitivity
INTRODUCTION
The aging eye undergoes many changes during each decade of life, including the onset of presbyopia, the loss of accommodative ability and many changes that encompass all aspects of the adnexa and eyeball[1]–[2]. Dermatochalasis is a common disorder, and its frequency increases with age. Dermatochalasis is atrophy of the elastic tissue (elastosis) of the eyelids, and it results in excess lid skin with fine wrinkles[2]–[3]. It is a common age-related involutional change characterized by excessive redundant skin folds that are sometimes associated with fat prolapsing through the orbital septum[4]–[5]. Periorbital changes associated with aging such as laxity of the supporting ligaments, thinning of the levator muscle aponeurosis, descent of the midface, and inferoforward movement of orbital fat also induce dermatochalasis[6]–[8].
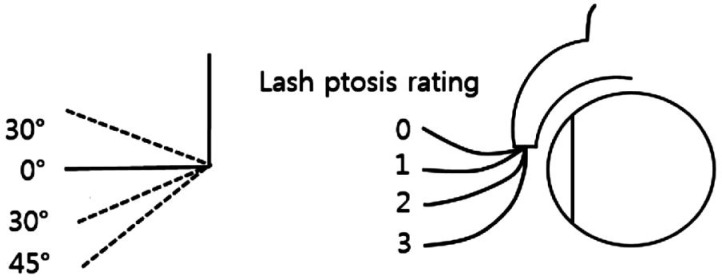
This condition could cause functional and cosmetic problems[9]. Functional problems include superior visual field defects that are caused by overhanging redundant skin, lateral skin erosion due to tear collection, and lash ptosis caused by the gravitational pull of excess skin. Lash ptosis, also known as eyelash ptosis, refers to a global declination of lash follicles of the upper eyelid[10]–[12] (Figure 1) and might coexist with dermatochalasis. Some patients may be concerned about a sleepy-looking facial appearance caused by drooping eyelids and may look far older than their actual age[13]–[14].
Figure 1. A 4-point LPR scale enumerates variations in the degree of lash ptosis[12].
An LPR of 0 indicates no lash ptosis, while 1 indicates minimal, 2 indicates moderate, and 3 indicates significant lash ptosis.
If the upper lid and eyelashes droop to the extent that they interfere with the line of sight, upper lid blepharoplasty might be indicated. Blepharoplasty usually involves removing excess skin, muscle and protruding fat from the eyelids, thus restoring vision and relieving superior visual field loss. Improvements in the superior visual field after blepharoplasty have been well documented[15]–[16]. Visual field testing is often used preoperatively in functional disability cases to justify surgery. The Center for Medicare Services in the United States has established a standard for functional upper blepharoplasty. According to the standard guidelines, the measurement of the upper margin reflex distance should be less than 2.5 mm with a visual field showing improvement of more than 30% between untaped and taped eyelids[13]. Although blepharoplasty has been shown to improve objective visual fields, changes in patients' visual quality and subjective perception of visual function have also been demonstrated to occur after blepharoptosis surgery.
In this study, we performed contrast sensitivity tests to measure changes in visual quality after blepharoplasty. Contrast sensitivity is the ability to detect luminance contrast and to perceive differences between an object and its background[17]. Contrast sensitivity testing has become an important clinical tool in the battery of tests used to characterize the vision of patients[17]. Recently, Rogers et al[13] reported significant improvement in contrast sensitivity after upper eyelid blepharoplasty.
Although most upper eyelid blepharoplasties include levator aponeurosis advancement procedures, we only removed excess skin that overshadowed patients' sight. Thus, we aimed to explore whether visual quality improves after the removal of only remnant skin in dermatochalasis and lash ptosis patients.
SUBJECTS AND METHODS
This study included prospectively enrolled east Asian patients with dermatochalasis and lash ptosis who visited the Dong-A Medical Center from June 2013 to March 2014. The study was approved by the Institutional Review Board of Dong-A University. The research protocol adhered to the tenets of the Declaration of Helsinki for clinical research. Written informed consent was obtained from all participants after the purpose and possible consequences of the study were explained. One oculoplastic surgeon (Ahn HB) performed incisional upper eyelid blepharoplasty on 73 eyelids of 39 patients. Patients who had undergone previous upper eyelid surgery, those with brow ptosis, those with abnormal neurosensory patterns of the face, those with marked active ocular abnormalities, and those with a history of trauma or congenital blepharoptosis were excluded. All patients underwent full oculoplastic assessments and measurements of visual acuity, the degree of lash ptosis, vertical palpebral fissure aperture, levator function and contrast sensitivity. Visual acuity was measured using a Snellen chart, and all visual acuity results were converted into LogMAR values for analysis. The degree of lash ptosis was assessed using a 4-point rating scale for lash ptosis and was assigned a lash ptosis rating (LPR). An LPR of 0 indicates no lash ptosis, while 1 indicates minimal, 2 indicates moderate, and 3 indicates severe lash ptosis. An LPR of 0 represents the natural position of the eyelashes relative to the eyelid margin (0° to 30° above the horizontal meridian). Eyelashes oriented nearly parallel to the horizontal meridian relative to the eyelid margin (0° to 30° below the horizontal meridian) are assigned an LPR of 1. An LPR of 2 represents eyelashes with an orientation that is 31° to 45° below the horizontal meridian. Eyelashes oriented at more than 45° below the horizontal meridian have an LPR of 3[12] (Figure 1). The vertical dimension of the palpebral fissure aperture was assessed by measuring the vertical distance between the upper and lower lids, as measured with the pupil centered and the eyes in the primary position. Contrast sensitivity was measured using a Vector Vision CSV-1000 (Greenville, OH, USA) chart, which is a translucent chart that is rear-illuminated by a tungsten bulb. The unit self-calibrates to produce a mean luminance of 85 cd/m2. All patients were tested at the recommended distance of 8 feet under photopic (85 cd/m2) and scotopic (<2 cd/m2) conditions. The CSV-1000 comprises a series of circular achromatic sine-wave patches measuring 1.5 inches in diameter. Vertical pairs of circles are present across each row; one circle contains the sine-wave patch, and the other circle is blank, with the same space-averaged luminance as the test patch. There are four rows, each of which corresponds to one of the following four spatial frequencies: 3, 6, 12, and 18 cycles per degree (cpd). When selected, a given spatial frequency is rear-illuminated, and the subject is shown a suprathreshold example of the test pattern. Each spatial frequency is presented at eight different contrast levels that systematically decrease from 0.20 to 0.08 from left to right in eight columns. The first patch on the far left side of the row presents high-contrast grating (sample patch). The remaining 16 patches are situated in eight columns distributed across the row. In each column, one patch presents a grating, and the other is blank. The patches that present gratings decrease in contrast moving from left to right across the row. The patient is directed to observe the first sample patch and is told to look for the grating pattern in each column. While reading across the row, the patient indicates whether the grating appears in the top patch or the bottom patch for each column. Patients must be informed that there are three possible responses: the sine wave pattern is in the top circle, the bottom circle, or neither, the latter indicating that the patient cannot see a pattern in either patch. The contrast threshold is defined as the contrast of the last column in which the patient could correctly identify the location of the sine-wave patch. The contrast sensitivity levels in each row range from 0.70 to 2.08, 0.91 to 2.29, 0.61 to 1.99, and 0.17 to 1.55 log units for 3, 6, 12, and 18 cpd, respectively. The contrast levels diminish in a uniform logarithmic fashion in increments of 0.15 log units for contrast levels 3 through 8 and 0.17 log units for steps 1 through 3. The contrast change between the sample patch and level 1 is 0.3 log units[18]–[19].
One evaluator (An SH) conducted the levator function test (LFT), determined the vertical palpebral fissure aperture, LPR and contrast sensitivity in each eye in primary gaze and took pictures of the primary gaze and side views of each eye to the measure the angular displacement of the anterior projection of the eyelashes.
All patients underwent routine upper eyelid blepharoplasty surgery under local anesthesia. The aim of the surgery was to remove the maximal amount of redundant skin. After marking the skin crease, the amount of excess skin was assessed. A caliper was used to measure from the base of the eyebrow hairs to the eyelid skin, and a mark was placed on the skin. The upper limit of the skin incision was then marked, and the redundant skin and some bulging fat were removed. Supratarsal fixation sutures were placed (three to four) to create a lid crease. The wounds were closed with continuous or interrupted 6-0 nylon sutures. Levator aponeurosis advancement was not performed for any of the patients. Postoperative visual acuity, vertical palpebral fissure aperture, LPR and contrast sensitivity assessments and the LFT were performed. Postoperative follow-up visits were scheduled at 1wk, 1 and 3mo.
A paired t-test was used to analyze changes in all parameters, and P<0.05 was considered statistically significant. All statistical analyses were performed using SPSS software (SPSS for Windows, version 12.0; SPSS, Inc., Chicago, IL, USA).
RESULTS
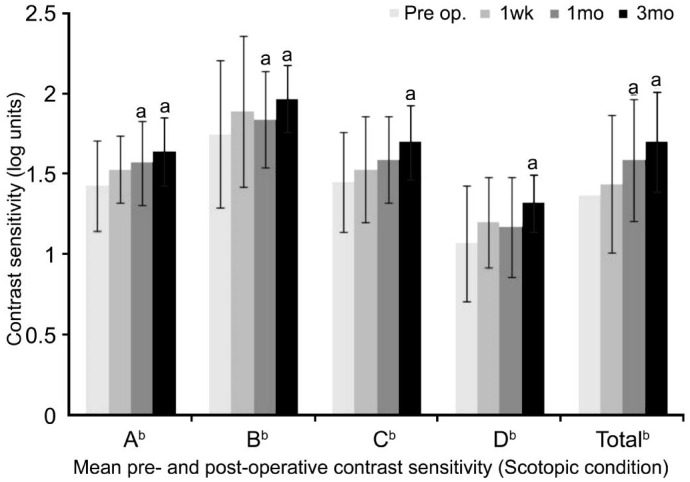
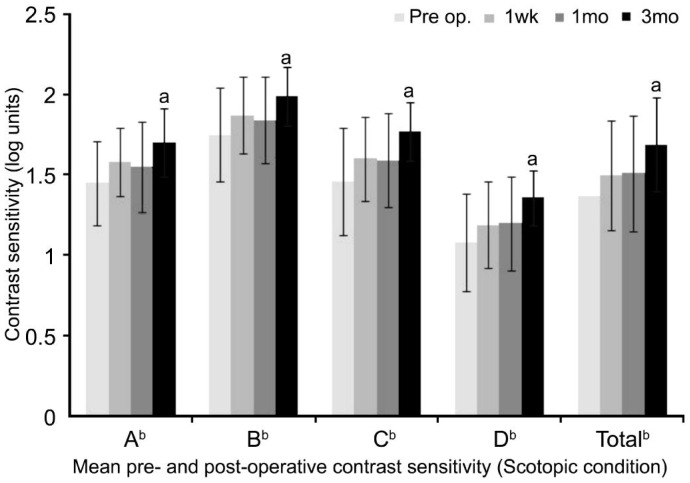
Seventy-three eyelids of 39 patients were included in the study. The age range was 54-71y, with an average age of 62.6y. The preoperative and postoperative contrast sensitivity values are shown in Figures 2 and 3. Contrast sensitivity was significantly increased after surgery at each spatial frequency under photopic and scotopic conditions. Under photopic conditions, the average contrast sensitivity values gradually increased at all spatial frequencies after surgery, and a significant improvement was observed after 1mo (P=0.017) (Figure 2). Under scotopic conditions, the average postoperative contrast sensitivity values also increased at all spatial frequencies. Three months after surgery, the mean increase in contrast sensitivity was significantly enhanced (P=0.009) (Figure 3). Slight changes in the mean logMAR visual acuity and LFT results were found, but these differences were not significant.
Figure 2. Mean pre- and postoperative contrast sensitivity (under photopic conditions).
Significant increases in contrast sensitivity were found at spatial frequencies A and B at 1 post-operative month and at each spatial frequency at 3 postoperative months (A: From 1.43±0.28 log units to 1.64±0.21 log units; B: From 1.75±0.46 log units to 1.97±0.21 log units; C: From 1.45±0.31 log units to 1.70±0.23 log units; D: From 1.07±0.36 log units to 1.32±0.18 log units; Total: From 1.37±0.40 log units to 1.70±0.31 log units). aThe correlation is significant at P<0.05 (paired t-test); bA: 3 cpd; B: 6 cpd; C: 12 cpd; D: 18 cpd; Total: Sum of A-D cpd contrast sensitivity values.
Figure 3. Mean pre- and postoperative contrast sensitivity (under scotopic conditions).
A significant increase in contrast sensitivity was found at every spatial frequency at 3 postoperative months (A: From 1.45±0.26 log units to 1.70±0.21 log units; B: From 1.75±0.29 log units to 1.99±0.18 log units; C: From 1.46±0.33 log units to 1.77±0.18 log units; D: From 1.08±0.30 log units to 1.36±0.17 log units; Total: From 1.37±0.37 log units to 1.69±0.29 log units). aThe correlation is significant at P<0.05 (paired t-test). bA: 3 cpd; B: 6 cpd; C, 12 cpd; D, 18 cpd; Total: Sum of A-D cpd contrast sensitivity values.
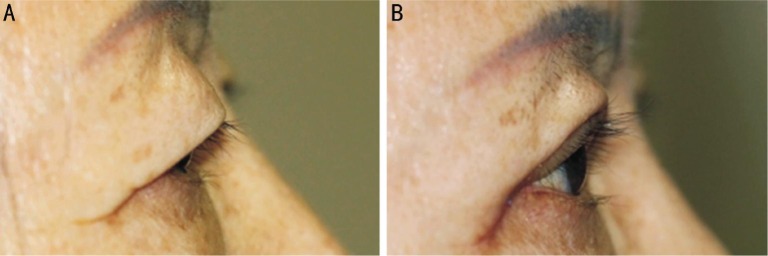
The patients had an average LPR of 2.60±0.49 before surgery and 0.49±0.51 after 3mo. Thus, the LPR significantly decreased (P<0.001), confirming that the lash ptosis was improved after upper eyelid blepharoplasty (Figure 4). The change in vertical palpebral fissure aperture was significant beginning at 1wk after surgery, with values of 4.84±1.54 mm to 7.18±0.97 mm after 1wk and of 7.63±0.87 mm after 3mo (P<0.001) (Figure 5).
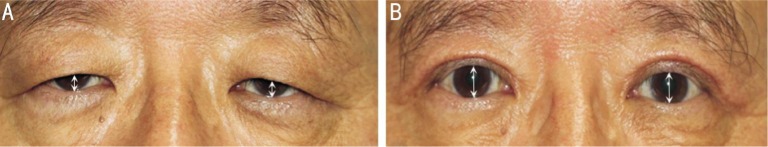
Figure 4. Lash ptosis before and after upper eyelid blepharoplasty.
A: Moderate LP (LPR 2); B: No LP (LPR 0)
Figure 5. The height of the palpebral aperture at the midpupil point before and after upper eyelid blepharoplasty.
A: The height of the vertical palpebral aperture was decreased due to excessive redundant skin folds; B: After the redundant skin folds were removed, the height of the vertical palpebral aperture at the midpupil was increased.
DISCUSSION
Dermatochalasis is an aging process aided by gravity and characterized by grossly redundant or loose eyelid skin that causes the upper lid to begin to obstruct the superior visual field, potentially affecting the visual axis[2]–[3]. The loss of elastic tissue, weakening of the connective tissue, thinning of the epidermis, and redundancy of the skin cause dermatochalasis[2]. Aponeurotic ptosis is involutional. Gradual drooping of the eyelid occurs, with weakness and stretching of the levator aponeurosis[20]–[21]. The lid might droop to the extent that it causes artificial visual field loss, which is usually superior and temporal. Age-related dermatochalasis frequently presents along with upper eyelid ptosis. Dermatochalasis is known to cause the protrusion of redundant skin. Drooped fat pads cover the eyes, causing discomfort and obstructing vision. This condition also limits the superior visual field in many patients[22]. Inexperienced surgeons often evaluate and surgically manage patients' ptotic eyelids, believing that the abnormal eyelid positioning is merely caused by dermatochalasis[23]–[26]. Postoperatively, these patients experience minimal or no change in their actual upper eyelid level and no improvement in their visual field, despite the apparently excellent removal of the upper eyelid skin[24]–[25]. This lack of vision improvement occurs because ptosis is a condition that involves the position of the eyelid margin as it relates to the visual axis, in contrast with dermatochalasis, which is an involutional change entirely confined to the eyelid skin and its subcutaneous attachments[22]–[24]. Thus, the successful management of eyelid ptosis requires addressing the underlying aponeurotic pathologic condition[22]–[27].
However, many patients who undergo upper blepharoplasty often report that their vision spontaneously brightens following surgery. Although blepharoplasty has been shown to improve the objective visual field, changes in the visual quality of patients after blepharoplasty have not been well studied. In this study, we focused on patients' subjective perceptions of visual function and investigated the possibility that upper eyelid blepharoplasty affects contrast sensitivity. Contrast sensitivity is defined as the ability to distinguish individual objects from objects in the background[14]. Reduced contrast sensitivity causes objects to appear to blend into the background and may lead to difficulty in completing many common tasks, such as driving at night and reading. Rogers et al [13] evaluated contrast sensitivity in dermatochalasis patients. Visual function could be characterized by spatial contrast sensitivity, which is separate from visual acuity[17]. The results of this study showed that 28 eyelids of 14 patients exhibited improvements in a contrast sensitivity test after upper eyelid blepharoplasty, a consequence of the effects of brighter vision. This study also showed a significant increase in contrast sensitivity following upper eyelid blepharoplasty. These results suggest that upper eyelid blepharoplasty has significant effects on vision quality.
To explain the effects of upper blepharoplasty on vision quality, Rogers et al[13] suggested several hypotheses. One hypothesis is the existence of a blinker effect caused by excess overhanging skin. Another hypothesis is that excess skin has a diffractive effect, which disperses incoming light. This skin is anterior to the path of light and obscures the image[13]. In our study, the majority of patients had lash ptosis accompanied by dermatochalasis. Dermatochalasis can affect the structure of the upper eyelid and cause deformation of other anatomical structures, leading to lash ptosis. Loose and redundant eyelid skin pushes the lashes downward, thus obstructing an individual's field of vision. However, no studies in the literature have examined the effect of lash ptosis on visual function. Deviated lashes might cause scattering or blocking of incoming light; both scenarios could affect contrast sensitivity.
Evidence indicates that upper eyelid blepharoplasty affects corneal topography. In the current study, upper eyelid blepharoplasty likely had an overall beneficial effect on postoperative corneal topography, which might have resulted in increased contrast sensitivity; however, these suggestions are purely theoretical. Although changes in astigmatism have been reported in other studies[9],[28]–[29], no significant changes in astigmatism were detected in our study. This lack of change occurred because we only removed redundant skin folds, which do not influence astigmatism. Further examination of these hypotheses is needed to determine the exact cause of the increase in contrast sensitivity.
The actual practical visual benefit of this increased contrast sensitivity is difficult to quantify. A simple comparison could be made with cataract surgery. In a series of cataract extractions performed on 80 eyes from the same population assessed in this study, an average increase in contrast sensitivity of 0.28 was achieved[9]. In this study, the authors showed that upper eyelid blepharoplasty resulted in an average increase in contrast sensitivity of 0.14. Therefore, these data suggest that upper eyelid blepharoplasty effectively improves contrast sensitivity, similar to the effect of cataract surgery. Thus, blepharoplasty should be considered for functional improvements in vision.
In this study, upper eyelid surgery involving the removal of only redundant skin folds increased contrast sensitivity and improved functional visual acuity in patients with dermatochalasis and lash ptosis. This surgical process enhanced visual quality by eradicating the shield effect of the overhanging eyelid and eyelashes. Although contrast sensitivity was improved in our study, long-term follow-up is necessary to evaluate these changes in contrast sensitivity.
Aging is unavoidable and naturally occurs with the progression of time, and it can negatively affect cosmetic and functional aspects of life. Drooping eyelids and eyelashes caused by aging can be easily corrected with varying degrees of intervention and surgery. In blepharoplasty for aging, the correction of sagging upper eyelid skin might be achieved by excising redundant skin. As demonstrated in our study, this procedure results in significant improvements in aspects of visual quality such as contrast sensitivity, lash ptosis, and vertical palpebral fissure aperture. After upper eyelid blepharoplasty, patients may experience brightening of vision. Thus, upper lid blepharoplasty could help to improve visual quality. The information obtained in our study might be useful for justifying age-related blepharoplasty surgery in the future.
Acknowledgments
The study was presented as poster in AAO 2014.
Foundation: Supported by Dong-A University Research Fund.
Conflicts of Interest: An SH, None; Jin SW, None; Kwon YH, None; Ryu WY, None; Jeong WJ, None; Ahn HB, None.
REFERENCES
- 1.Lambros V. Observations on periorbital and midface aging. Plast Reconstr Surg. 2007;120(5):1367–1376. doi: 10.1097/01.prs.0000279348.09156.c3. [DOI] [PubMed] [Google Scholar]
- 2.Nagi KS, Carlson JA, Wladis EJ. Histologic assessment of dermatochalasis: elastolysis and lymphostasis are fundamental and interrelated findings. Ophthalmology. 2011;118(6):1205–1210. doi: 10.1016/j.ophtha.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 3.Shirado M. Dyslipidaemia and age-related involutional blepharoptosis. J Plast Reconstr Aesthet Surg. 2012;65(6):e146–150. doi: 10.1016/j.bjps.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 4.Hacker HD, Hollsten DA. Investigation of automated perimetry in the evaluation of patients for upper lid blepharoplasty. Ophthal Plast Reconstr Surg. 1992;8(4):250–255. doi: 10.1097/00002341-199212000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Ho SF, Morawski A, Sampath R, Burns J. Modified visual field test for ptosis surgery(Leicester Peripheral Field Test) Eye(Lond) 2011;25(3):365–369. doi: 10.1038/eye.2010.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fea A, Damato D, Actis AG, De Sanctis U, Actis G, Grignolo FM. Blepharoplastic: essential review. Minerva Chir. 2013;68(6 Suppl 1):49–56. [PubMed] [Google Scholar]
- 7.Kane MA. Nonsurgical periorbital and brow rejuvenation. Plast Reconstr Surg. 2015;135(1):63–71. doi: 10.1097/PRS.0000000000000831. [DOI] [PubMed] [Google Scholar]
- 8.Nuhoglu F, Ozdemir FE, Karademir Z, Eltutar K. Levator function in blepharoptosis surgery. Facial Plast Surg. 2013;29(1):71–75. doi: 10.1055/s-0033-1333835. [DOI] [PubMed] [Google Scholar]
- 9.Brown MS, Siegel IM, Lisman RD. Prospective analysis of changes in corneal topography after upper eyelid surgery. Ophthal Plast and Reconstr Surg. 1999;15(6):378–383. doi: 10.1097/00002341-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Langford JD, Linberg JV. A new physical finding in floppy eyelid syndrome. Ophthalmology. 1998;105(1):165–169. doi: 10.1016/s0161-6420(98)91960-1. [DOI] [PubMed] [Google Scholar]
- 11.Hwang K. Surgical anatomy of the upper eyelid relating to upper blepharoplasty or blepharoptosis surgery. Anat Cell Biol. 2013;46(2):93–100. doi: 10.5115/acb.2013.46.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malik KJ, Lee MS, Park DJ, Harrison AR. Lash ptosis in congenital and acquired blepharoptosis. Arch Ophthalmol. 2007;125(12):1613–1615. doi: 10.1001/archopht.125.12.1613. [DOI] [PubMed] [Google Scholar]
- 13.Rogers SA, Khan-Lim D, Manners RM. Does upper lid blepharoplasty improve contrast sensitivity? Ophthal Plast Reconstr Surg. 2012;28(3):163–165. doi: 10.1097/IOP.0b013e31823d2125. [DOI] [PubMed] [Google Scholar]
- 14.Kim JW, Lee H, Chang M, Park M, Lee TS, Baek S. What causes increased contrast sensitivity and improved functional visual acuity after upper eyelid blepharoplasty? J Craniofac Surg. 2013;24(5):1582–1585. doi: 10.1097/SCS.0b013e318292c5ac. [DOI] [PubMed] [Google Scholar]
- 15.Battu VK, Meyer DR, Wobig JL. Improvement in subjective visual function and quality of life outcome measures after blepharoptosis surgery. Am J Ophthalmol. 1996;121(6):677–686. doi: 10.1016/s0002-9394(14)70634-8. [DOI] [PubMed] [Google Scholar]
- 16.Mellington F, Khooshabeh R. Brow ptosis: are we measuring the right thing? The impact of surgery and the correlation of objective and subjective measures with postoperative improvement in quality-of-life. Eye (Lond) 2012;26(7):997–1003. doi: 10.1038/eye.2012.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shoshani YZ, Harris A, Rusia D, Spaeth GL, Siesky B, Pollack A, Wirostko B. Contrast sensitivity, ocular blood flow and their potential role in assessing ischaemic retinal disease. Acta Ophthalmol. 2011;89(5):e382–395. doi: 10.1111/j.1755-3768.2011.02130.x. [DOI] [PubMed] [Google Scholar]
- 18.Kelly SA, Pang Y, Klemencic S. Reliability of the CSV-1000 in adults and children. Optom Vis Sci. 2012;89(8):1172–1181. doi: 10.1097/OPX.0b013e318264097b. [DOI] [PubMed] [Google Scholar]
- 19.Koefoed VF, Baste V, Roumes C, Høvding G. Contrast sensitivity measured by two different test methods in healthy, young adults with normal visual acuity. Acta Ophthalmol. 2015;93(2):154–161. doi: 10.1111/aos.12487. [DOI] [PubMed] [Google Scholar]
- 20.Yabe T, Tsuda T, Hirose S, Ozawa T. Intraoperative adjustment of eyelid level in aponeurotic blepharoptosis surgery. Ann Plast Surg. 2015;74(5):520–523. doi: 10.1097/SAP.0b013e3182978885. [DOI] [PubMed] [Google Scholar]
- 21.Baroody M, Holds JB, Vick VL. Advances in the diagnosis and treatment of ptosis. Curr Opin Ophthalmol. 2005;16(6):351–355. doi: 10.1097/01.icu.0000186647.00413.21. [DOI] [PubMed] [Google Scholar]
- 22.Maegawa J, Kobayashi S, Yabuki Y, Hirotomi K, Yasumura K, Iwai T. Blepharoplasty in senile blepharoptosis: preoperative measurements and design for skin excision. Aesthet Surg J. 2012;32(4):441–446. doi: 10.1177/1090820X12442681. [DOI] [PubMed] [Google Scholar]
- 23.Cho I. Aging blepharoplasty. Arch Plast Surg. 2013;40(5):486–491. doi: 10.5999/aps.2013.40.5.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee TE, Lee JM, Lee H, Park M, Kim KH, Baek S. Lash ptosis and associated factors in Asians. Ann Plast Surg. 2010;65(4):407–410. doi: 10.1097/SAP.0b013e3181d3f006. [DOI] [PubMed] [Google Scholar]
- 25.Martin JJ., Jr Ptosis repair in aesthetic blepharoplasty. Clin Plast Surg. 2013;40(1):201–212. doi: 10.1016/j.cps.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 26.Lee IJ, Park MC, Lim H, Kim JH, Lee SH. Blepharoptosis correction: repositioning the levator aponeurosis. J Craniofac Surg. 2011;22(6):2284–2287. doi: 10.1097/SCS.0b013e31823278a6. [DOI] [PubMed] [Google Scholar]
- 27.Clauser L, Tieghi R, Galiè M. Palpebral ptosis: clinical classification, differential diagnosis, and surgical guidelines: an overview. J Craniofac Surg. 2006;17(2):246–254. doi: 10.1097/00001665-200603000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Zinkernagel MS, Ebneter A, Ammann-Rauch D. Effect of upper eyelid surgery on corneal topography. Arch Ophthalmol. 2007;125(12):1610–1612. doi: 10.1001/archopht.125.12.1610. [DOI] [PubMed] [Google Scholar]
- 29.Thiagarajan M, McClenaghan R, Anderson DF. Comparison of visual performance with an aspheric intraocular lens and a spherical intraocular lens. J Cataract Refract Surg. 2011;37(11):1993–2000. doi: 10.1016/j.jcrs.2011.05.046. [DOI] [PubMed] [Google Scholar]