Abstract
Objective
To investigate the sex- and age-specific incidence of healthcare-register-recorded anorexia nervosa (AN) and other eating disorders (OED) in a complete birth cohort, and assess whether incidence varies by diagnostic period and (sub-) birth cohort.
Method
We used the actuarial method and Poisson models to examine the incidence of AN and OED from 1987–2009 (when individuals were 8–30 years) for a cohort of 2.3 million individuals (48.7% female) born from 1979–2001 in Sweden, identified using Swedish registers.
Results
For both sexes, incidences of AN and OED increased considerably for diagnostic periods after 2000, but differed little by birth cohort. In 2009, AN incidence in the peak age category was 205.9 cases/100,000 persons (95% CI: 178.2, 233.5) for females (14–15 years), versus 12.8 cases/100,000 (95% CI: 5.6, 20.1) for males (12–13 years). OED incidence in the peak age category was 372.1 cases/100,000 (95% CI: 336.4, 407.9) for females (16–17 years), versus 22.2 cases/100,000 (95% CI: 13.3, 31.1) for males (14–15 years).
Discussion
Our finding of an increase in healthcare register-recorded eating disorders for diagnostic periods after 2000 likely reflects improved detection and expanded register coverage in Sweden. The peak of eating disorder incidence in adolescence, which began unexpectedly early for AN in males, suggests the importance of vigilance for signs of AN in young boys and early primary prevention efforts. Waiting until later could miss critical windows for intervention that could prevent disorders from taking root.
Keywords: eating disorders, anorexia nervosa, men, incidence, epidemiology, Sweden
Eating disorders have substantial morbidity, elevated mortality,1 and significant economic and societal costs.2,3 Incidence, a measure of new cases of a disorder for a given population, provides essential data for service planning.4 In addition, information on how incidence varies with respect to age, sex, and birth cohort can provide valuable insight into the etiology of the disorder.4 Most studies of eating disorder incidence have been based on small samples, narrow age ranges, subgroups (e.g., females, hospitalized or primary care patients only), limited diagnostic periods, or only focus on a single eating disorder.5 However, these limitations can be overcome by combining data from population and healthcare registers to estimate incidence in a large cohort followed over time, as demonstrated by a recent study of treated mental disorders in Denmark.6 In particular, Swedish population and healthcare registers, the latter of which presently capture nearly all healthcare-detected eating disorders in Sweden,7 can be used to estimate the incidence of healthcare detected and recorded eating disorders in a complete birth cohort over time in an efficient and cost-effective way.
Thus, we used the Swedish registers to conduct a nationwide cohort study of 2.3 million individuals born 1979–2001 to: 1) estimate the age- and sex-specific incidence of healthcare-register-recorded cases of any eating disorder (AED), anorexia nervosa (AN), or any other eating disorder (OED) between 1987 and 2009 (when individuals were 8–30 years old); and 2) determine whether changes in the incidence of AED, AN, and OED over calendar time are attributable to (birth) cohort effects and/or to (diagnostic) period effects, given that changes in diagnostic practices or completeness of registration between diagnostic periods can result in substantial differences in incidence over calendar time, even in the absence of cohort effects.8
Methods
Study Sample and Information Resources
We linked information from Swedish population and healthcare registers via a unique personal identification number assigned to all Swedish residents at birth.9 Our cohort includes all individuals who were born in Sweden between January 1, 1979 and December 31, 2001 and survived to at least age 8 years without emigrating (N = 2,269,280; 1,104,074 females), identified using the Total Population (TP),10 Migration,11 and Cause of Death (COD; data access through December 31, 2008)12 registers, which also provided demographic data (e.g., sex). For individuals in our cohort, we identified all eating disorders detected by the Swedish healthcare system and recorded in the Swedish healthcare registers between January 1, 1987 and December 31, 2009 using the National Patient Register (NPR),13 Riksät-National Quality Register for Specialized Treatment for Eating Disorders,7 and Stepwise-regional quality assurance system for eating disorders.14 The NPR13 provides national coverage of all Swedish public and private hospital inpatient admissions beginning in 1973 and outpatient specialist care beginning in 2001.15 At the time of data extraction, Riksät7 and Stepwise14 (longitudinal registers that first entered patient information in 1999 and 2005, respectively) provided quality assurance of over 35 specialist treatment centers capturing nearly all individuals receiving inpatient, day treatment, or outpatient specialized eating disorders treatment in Sweden (for detailed information see Birgegård et al.,14). Using the COD, we also identified all individuals with cause of death listed as an eating disorder (n = 6), but all of these individuals had previously received at least one eating disorder diagnosis through the healthcare system. The University of North Carolina Biomedical Institutional Review Board approved this study, which was also approved by the Regional Ethics Committee of Karolinska Institutet.
Eating Disorder Outcome
We restricted our focus to eating disorder diagnoses occurring at age 8 or older to avoid diagnostic misclassification (e.g., feeding difficulties of childhood). Diagnoses were made by physicians based on WHO International Classification of Diseases, Ninth Revision (ICD-9; 1987–1996)16 and ICD-Tenth Revision (ICD-10; 1997-present)17 at hospital discharge (data from NPR) or by specially-trained clinicians based on DSM-IV criteria18 once intent to treat was established (data from Riksät and Stepwise). The specially-trained clinicians used semi-structured clinical interviews (Structured Clinical Interview for DSM-IV Axis I Disorders, SCID-I19 for adults or Mini International Neuropsychiatric Interview, M.I.N.I.Kid20,21 for children prior to February 2008, or Structured Eating Disorder Interview, SEDI22 for all ages beginning February 2008) to determine diagnosis. ICD-9 eating disorders include AN (307B) and “other eating disorders” (307F). ICD-10 eating disorders include AN (F50.0), atypical AN (F50.1), bulimia nervosa (BN; F50.2), atypical BN (F50.3), and “eating disorder, unspecified” (F50.9). DSM-IV18 diagnoses include AN, BN, and EDNOS (eating disorder not otherwise specified).
We collapsed diagnoses into two primary categories: AN and OED. For AN, we used two definitions: 1) “narrow AN,” which includes only full-criteria AN (i.e., ICD-9 307B, ICD-10 F50.0, and DSM-IV AN) cases and 2) “broad AN,” which includes both full-criteria AN and atypical AN (e.g., ICD-10 F50.1) cases. In Sweden, atypical AN is usually diagnosed in individuals who meet all but the amenorrhea criterion, which has been dropped as a diagnostic criterion for AN in the newest edition of the DSM (i.e., DSM-5) due to poor clinical utility and prognostic value.23 In this report, we only present “broad AN” results because sensitivity analyses using the “narrow AN” definition yielded the same outcome. For OED, we included all other eating disorder diagnoses (excluding full-criteria AN and atypical AN). We were unable to examine sub-categories of OED (e.g., BN or BED) separately in analyses because the ICD-9 only includes the heterogeneous category of OED.
In addition to AN and OED, we also examined AED as an outcome. Consistent with previous reports regarding diagnostic crossover between eating disorders,24,25 numerous individuals in our dataset had both AN and OED diagnoses (at different dates). These individuals are included as incident cases for both the AN and OED outcomes. Thus, the number of incident cases of AN and/or OED is greater than the number of incident cases of AED, where each individual can be an incident case only once. Analyses of AED are included to provide information on the overall incidence of eating disorders without inflation due to crossover.
Statistical Analyses
Data management was conducted using SAS® version 9.3,26 and data analysis was conducted using R version 3.1.27 Descriptive statistics and graphics were used to screen data for implausible values, outliers, and potential influential observations.
First, for each outcome (AED, AN, or OED), we used the actuarial method28 to calculate the age-specific annual incidence (per person) and accompanying confidence intervals (CIs) of first recorded contact with the healthcare system due to the respective outcome, by sex. For visual simplicity, incidence estimates and accompanying 95% CIs were calculated (and plotted) for age categories defined by grouping together developmentally similar ages (8–11, 12–13, 14–15, 16–17, 18–19, 20–23, 24–30), with a wider range of ages included in the youngest and older age groups due to lower incidence rates. We plotted the annual incidence estimates (and CIs) by age category to depict how incidence changes across age categories and from 1987 to 2009. In addition, we examined the incidence estimates (and CIs) for age categories with peak incidence during 2009 (the last calendar year included in the present study) to illustrate the magnitude of eating disorder incidence in Sweden in recent years.
Second, for each outcome, we fitted age-period-cohort Poisson models to estimate the age-specific incidence rate (per person-year) and to determine whether the incidence rates differed by diagnostic period or birth cohort, again by sex.8,29,30 Age refers to the age at which an eating disorder could have been detected and recorded (here, from 8 to 30 years old), and (diagnostic) period refers to the date on which the eating disorder could have been detected and recorded (here, from January 1, 1987 to December 31, 2009). (Birth) cohort refers to the date on which individuals were born (here, from January 1, 1979 to December 31, 2001). Finally, drift (used below) refers to a regular trend in incidence over calendar time that can be equally attributed to period or to cohort.8 To determine whether incidence rates differed by period and cohort, we fitted a series of six models to the data and compared their fit:8,29,31 (I) Age; (II) Age + Period (drift); (III) Age + Period; (IV) Age + Cohort; (V) Age + Period (drift) + Cohort; (VI) Age + Period + Cohort. After determining the best-fitting model for each outcome and sex, we used diagnostic plots and formal test of overdispersion32,33 to assess the appropriateness of model assumptions, and we then examined the estimates and CIs for the model coefficients.
In the Poisson models, age, period, and cohort were each grouped into categories, as is customary in age-period-cohort modeling.8,29 We used one-year age categories for females and roughly two-year age categories for males; finer age categories were necessary to improve model fit (and reduce overdispersion) in females, but could not be used in males due to sparser outcomes. (Models fit well in males even with coarser age categories). For the same reason, we used roughly two-year period categories for females, but combined the earlier period categories (i.e., 1987–1989 and 1990–1991; 1992–1993, 1994–1995, and 1996–1997) for males. We used approximately ten-year cohort categories (1979–1990 and 1991–2001) for each sex. Before fitting the Poisson models, we calculated the number of person-years at risk and number of first AED, AN, and OED diagnoses for each combination of the age, period, and cohort categories, with individuals treated as censored at the date of first emigration from Sweden (based on the Migration Register), the date of death (based on the COD Register), or the end of the follow-up period (December 31, 2009). In all models except those with a drift term, no constraints were placed on the coefficients for the ordinal age, period, or cohort categories, aside from constraining the coefficients for one period category (2008–2009) and one cohort category (1979–1990) to zero for purposes of identifiability. (We chose 2008–2009 as the reference period category because, as described in more detail in the Results, coefficients for the age categories would then represent (transformations of) incidence rates during the most recent period included in the study). In models with a Period (drift) term, it was assumed that coefficients for period categories were determined by δc, where c indexes the C period categories (c = 0, …, C − 1) and δ refers to the linear effect of period categories on log(incidence).
Results
Out of the initial cohort (n = 2,269,280 at 8 years old), there were 16,403 incident cases of AED (0.7%). For females (n = 1,104,074), there were 15,433 incident cases of AED (1.4%), 7,715 incident cases of AN, and 11,038 incident cases of OED. For males (n = 1,165,206), there were 970 incident cases of AED (0.08%), 459 incident cases of AN, and 680 incident cases of OED.
Annual Incidence
Figure 1 presents estimates and 95% CIs for annual incidence, by age category, for each outcome and sex. (See Supplemental Tables 1–6 for the numbers of incident cases and persons at risk used to calculate the estimates and CIs for each age category and year.) The plots for females (left-hand column) reveal a peak incidence of AED (top plot) in the 16–17 year old category, with incidence for AN (middle plot) highest in the 14–15 and 16–17 year old age categories and incidence for OED (bottom plot) highest in the 16–17 and 18–19 year old age categories. The plots also reveal that the incidence of all three outcomes increased considerably after 2000. By 2009, incidence of AN was 205.9 cases per 100,000 persons (95% CI: 178.2, 233.5) in the peak 14–15 year old age category, and incidence of OED was 372.1 cases per 100,000 persons (95% CI: 336.4, 407.9) in the peak 16–17 year old age category. Incidence of AED was 457.4 cases per 100,000 persons (95% CI: 417.7, 497.1) in the peak 16–17 year old age category in 2009.
Figure 1. Annual age-category-specific incidences.
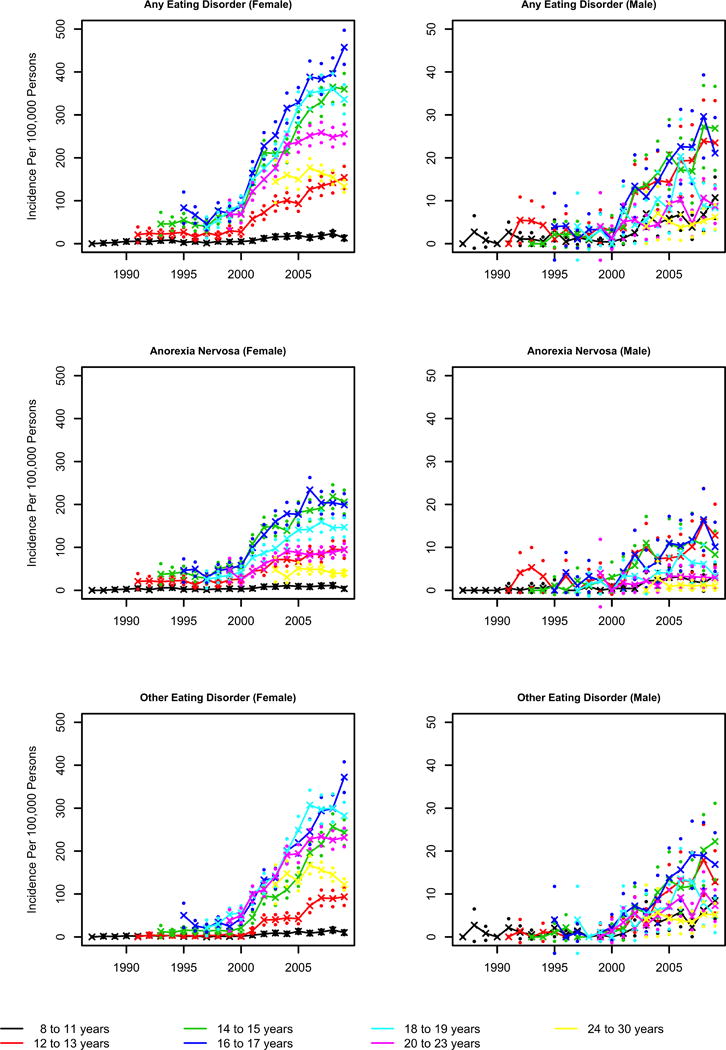
Each plot represents a different sex and outcome. Within a plot, Xs refer to estimates and dots refer to bounds of 95% confidence intervals (all calculated using the actuarial method), with different colors representing different age categories.
The plots for males (right-hand column) reveal that incidences were considerably lower, by more than a factor of 10, than for females. In males, peak incidence of AED (top plot) was in the 12–13, 14–15, and 16–17 year old age categories, with incidence for AN (middle plot) highest in the 12–13, 14–15, and 16–17 year old age categories, and incidence for OED (bottom plot) highest for the 14–15 and 16–17 year old age categories. The plots also reveal that incidences of all three outcomes increased after 2000. By 2009, incidence of AN was 12.8 cases per 100,000 persons (95% CI: 5.6, 20.1) in the peak 12–13 year old age category, and incidence of OED was 22.2 cases per 100,000 persons (95% CI: 13.3, 31.1) in the peak 14–15 year old age category. Incidence of AED was 26.9 cases per 100,000 persons (95% CI: 17.1, 36.6) in the peak 14–15 year old age category in 2009.
Age-Period-Cohort Modeling of Incidence Rates
Tables 1 and 2 present the residual deviance and degrees of freedom for the six models, as well as results from model comparisons and the overdispersion test in the best-fitting model, for each outcome in females and males, respectively. Figures 2 and 3, as well as Tables 3 and 4, present the estimates and accompanying CIs for the age coefficients (transformed as recommended in Clayton et al.8) from the best-fitting model for each outcome in females and males, respectively. The estimated coefficient for each age category represents the model-based estimate of the incidence rate (per 100,000 person-years) for that age category during the 2008–2009 period (and, in models with cohort effects, for the 1979–1990 birth cohort). Tables 3 and 4 also present the estimates and accompanying CIs for the period and cohort coefficients (transformed as recommended in Clayton et al.8) from the best-fitting model for each outcome in females and males, respectively. In those tables, the estimated coefficient for each period category represents the model-based estimate of that category’s multiplicative effect (relative to the 2008–2009 period) on incidence rates. Likewise, in models with cohort effects, the estimated coefficient for the 1991–2001 cohort category represents the model-based estimate of that category’s multiplicative effect (relative to the 1979–1990 birth cohort) on incidence rates.
Table 1.
Poisson model comparisons for females
| Any Eating Disorder
|
Anorexia Nervosa
|
Other Eating Disorder
|
||||
|---|---|---|---|---|---|---|
| Deviance | DF | Deviance | DF | Deviance | DF | |
| Model I. Agea | 4270.3 | 131 | 1971.3 | 131 | 4379.6 | 131 |
| Model II. Agea + Period (drift)b | 631.0 | 130 | 405.9 | 130 | 673.0 | 130 |
| Model III. Agea + Periodc | 144.2 | 121 | 147.2 | 121 | 231.6 | 121 |
| Model IV. Agea + Cohortd | 2929.9 | 130 | 1412.5 | 130 | 2908.0 | 130 |
| Model V. Agea + Period (drift)b + Cohortd | 624.5 | 129 | 389.4 | 129 | 668.4 | 129 |
| Model VI. Agea + Periodc + Cohortd | 143.1 | 120 | 146.5 | 120 | 204.1 | 120 |
| Model II vs. Model Ie | p < 0.001 | p < 0.001 | p < 0.001 | |||
| Model III vs. Model IIe | p < 0.001 | p < 0.001 | p < 0.001 | |||
| Model VI vs. Model IIIe | p = 0.31 | p = 0.42 | p < 0.001 | |||
| Best-Fitting Model (overdispersion test results)f | Model III (p = 0.80) | Model III (p = 0.83) | Model VI (p = 0.06) | |||
Abbreviations: DF = Degrees of Freedom
Age treated as categorical variable with levels for every year between 8 and 30 (inclusive). There is no reference level because model excludes an intercept term.
Period treated as an interval variable with the levels described in footnote c assigned integer values 0 – 10.
Period treated as categorical variable with levels [1987–1989] (reference level), [1990–1991], [1992–1993], [1994–1995], [1996–1997], [1998–1999], [2000–2001], [2002–2003], [2004–2005], [2006–2007], [2008–2009].
(Birth) Cohort treated as categorical variable with levels [1979–1990] (reference level), [1991–2001].
p-value based on chi-squared test comparing (residual) deviance and DF for Model A (less reduced model) versus Model B (more reduced model).
p-value based on (one-sided) test of H1. Poisson model mean < variance (overdispersion) versus H0. mean = variance (no overdispersion).
Table 2.
Poisson model comparisons for males
| Any Eating Disorder
|
Anorexia Nervosa
|
Other Eating Disorder
|
||||
|---|---|---|---|---|---|---|
| Deviance | DF | Deviance | DF | Deviance | DF | |
| Model I. Agea | 501.3 | 65 | 231.7 | 65 | 455.1 | 65 |
| Model II. Agea + Period (drift)b | 105.8 | 64 | 69.0 | 64 | 98.0 | 64 |
| Model III. Agea + Periodc | 67.6 | 58 | 47.9 | 58 | 58.6 | 58 |
| Model IV. Agea + Cohortd | 299.0 | 64 | 146.9 | 64 | 271.1 | 64 |
| Model V. Agea + Period (drift)b + Cohortd | 105.4 | 63 | 68.9 | 63 | 98.0 | 63 |
| Model VI. Agea + Periodc + Cohortd | 67.5 | 57 | 47.9 | 57 | 58.6 | 57 |
| Model II vs. Model Ie | p < 0.001 | p < 0.001 | p < 0.001 | |||
| Model III vs. Model IIe | p < 0.001 | p = 0.002 | p < 0.001 | |||
| Model VI vs. Model IIIe | p = 0.84 | p = 0.92 | p = 0.85 | |||
| Best-Fitting Model (overdispersion test)f | Model III (p = 0.70) | Model III (p = 0.99) | Model III (p = 0.99) | |||
Abbreviations: DF = Degrees of Freedom
Age treated as categorical variable with levels for every year between 8 and 30 (inclusive). There is no reference level because model excludes an intercept term.
Period treated as an interval variable with the levels described in footnote c assigned integer values 0 – 10.
Period treated as categorical variable with levels [1987–1991] (reference level), [1992–1997], [1998–1999], [2000–2001], [2002–2003], [2004–2005], [2006–2007], [2008–2009].
(Birth) Cohort treated as categorical variable with levels [1979–1990] (reference level), [1991–2001].
p-value based on chi-squared test comparing (residual) deviance and DF for Model A (less reduced model) versus Model B (more reduced model).
p-value based on (one-sided) test of H1. Poisson model mean < variance (overdispersion) versus H0. mean = variance (no overdispersion).
Figure 2. Age coefficients (estimates and confidence intervals, CIs) from best-fitting Poisson models for females.
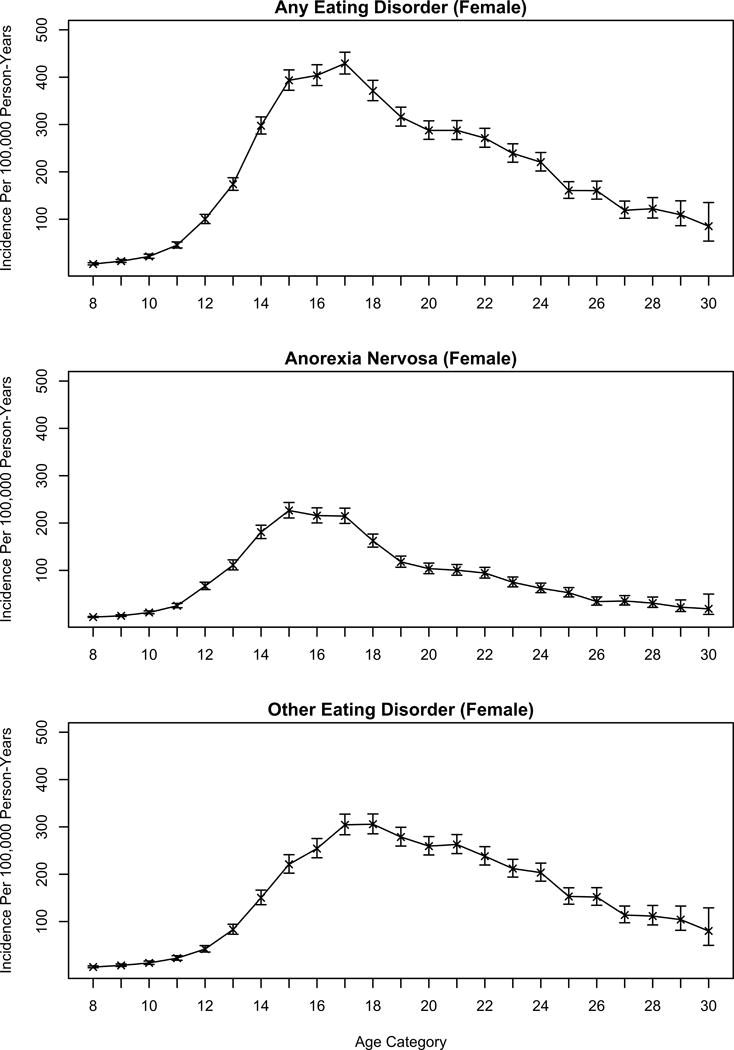
Each plot represents a different outcome (Any Eating Disorders; Anorexia Nervosa; Other Eating Disorders). Within a plot, Xs refer to estimates; bars refer to bounds of 95% CIs. Estimates (and lower and upper bounds of CIs) for age are transformed by exp(x)*100000, and represent model-based estimates of the incidence (per 100,000 person-years) for the age in question during the 2008–2009 period (and, for the Other Eating Disorder outcome only, for the 1979–1990 birth cohort).
Figure 3. Age coefficients (estimates and confidence intervals, CIs) from best-fitting Poisson models for males.
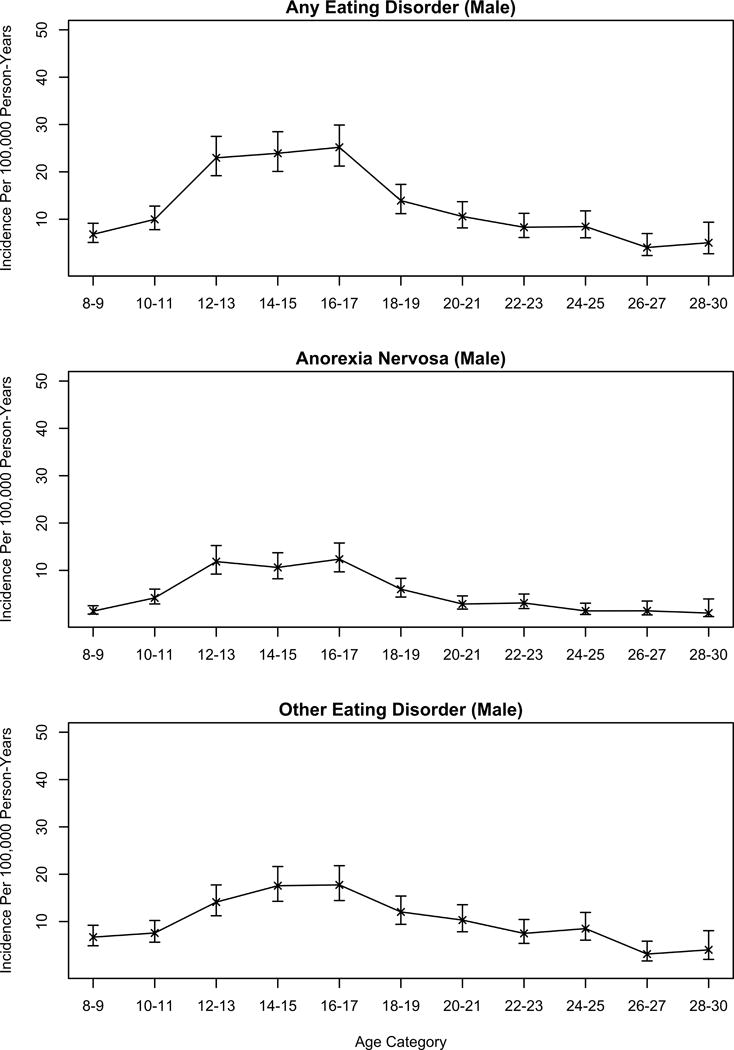
Each plot represents a different outcome (Any Eating Disorders; Anorexia Nervosa; Other Eating Disorders). Within a plot, Xs refer to estimates; bars refer to bounds of 95% CIs. Estimates (and lower and upper bounds of CIs) for age are transformed by exp(x)*100000, and represent model-based estimates of the incidence (per 100,000 person-years) for the age in question during the 2008–2009 period.
Table 3.
Coefficients (estimates and confidence intervals) from best-fitting Poisson models for females
| Any Eating Disordera
|
Anorexia Nervosab
|
Other Eating Disorderc
|
||||
|---|---|---|---|---|---|---|
| Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | |
| Age (in years)d | ||||||
| [8] | 5.3 | 3.5, 8.0 | 1.4 | 0.6, 2.9 | 4.0 | 2.5, 6.4 |
| [9] | 11.3 | 8.6, 15.0 | 4.1 | 2.7, 6.4 | 7.3 | 5.1, 10.5 |
| [10] | 21.4 | 17.4, 26.2 | 11.0 | 8.4, 14.4 | 12.6 | 9.6, 16.6 |
| [11] | 45.2 | 39.2, 52 | 25.2 | 21.0, 30.2 | 22.7 | 18.3, 28.0 |
| [12] | 100.0 | 90.7, 110.3 | 66.9 | 59.5, 75.1 | 41.9 | 35.6, 49.3 |
| [13] | 173.9 | 161.1, 187.6 | 111.1 | 101.1, 122.1 | 83.1 | 73.3, 94.3 |
| [14] | 297.5 | 279.9, 316.1 | 180.8 | 167.2, 195.5 | 150.3 | 135.7, 166.4 |
| [15] | 393.4 | 372.4, 415.5 | 226.5 | 210.7, 243.5 | 220.9 | 202.3, 241.2 |
| [16] | 403.8 | 382.4, 426.4 | 215.7 | 200.3, 232.3 | 254.3 | 234.8, 275.4 |
| [17] | 429.1 | 406.6, 452.8 | 214.7 | 199.2, 231.4 | 304.4 | 283.4, 326.9 |
| [18] | 371.2 | 350.3, 393.3 | 162.4 | 149.2, 176.8 | 305.7 | 285.4, 327.3 |
| [19] | 316.0 | 296.6, 336.6 | 117.9 | 106.8, 130.2 | 278.6 | 259.5, 299.2 |
| [20] | 287.6 | 268.8, 307.7 | 103.6 | 93.1, 115.4 | 259.4 | 240.7, 279.6 |
| [21] | 287.7 | 268.3, 308.4 | 100.5 | 89.8, 112.5 | 262.9 | 243.6, 283.7 |
| [22] | 271.4 | 252.1, 292.1 | 94.5 | 83.8, 106.5 | 238.1 | 219.4, 258.3 |
| [23] | 239.0 | 220.5, 259.2 | 74.9 | 65.2, 86.0 | 212.0 | 194.0, 231.6 |
| [24] | 220.5 | 201.9, 240.9 | 62.3 | 53.0, 73.1 | 203.5 | 185.3, 223.6 |
| [25] | 160.7 | 144.0, 179.2 | 52.9 | 43.9, 63.7 | 153.0 | 136.7, 171.3 |
| [26] | 160.3 | 142.4, 180.5 | 34.1 | 26.6, 43.9 | 151.9 | 134.5, 171.6 |
| [27] | 118.8 | 102.0, 138.3 | 35.4 | 26.9, 46.7 | 113.8 | 97.4, 132.9 |
| [28] | 122.3 | 102.6, 145.7 | 30.9 | 21.8, 43.7 | 111.6 | 92.9, 134.0 |
| [29] | 109.4 | 86.3, 138.8 | 22.3 | 13.2, 37.7 | 104.2 | 81.7, 132.8 |
| [30] | 85.2 | 53.7, 135.3 | 18.7 | 7.0, 49.9 | 80.2 | 49.8, 129.0 |
| Periode | ||||||
| [1987–1989] | 0.2 | 0.1, 0.6 | 0.3 | 0.1, 1.2 | 0.2 | 0.0, 0.6 |
| [1990–1991] | 0.3 | 0.2, 0.4 | 0.4 | 0.2, 0.6 | 0.2 | 0.1, 0.3 |
| [1992–1993] | 0.2 | 0.2, 0.3 | 0.3 | 0.2, 0.3 | 0.1 | 0.1, 0.2 |
| [1994–1995] | 0.2 | 0.2, 0.2 | 0.2 | 0.2, 0.3 | 0.1 | 0.1, 0.1 |
| [1996–1997] | 0.1 | 0.1, 0.2 | 0.2 | 0.1, 0.2 | 0.1 | 0.1, 0.1 |
| [1998–1999] | 0.2 | 0.2, 0.2 | 0.2 | 0.2, 0.3 | 0.1 | 0.1, 0.1 |
| [2000–2001] | 0.3 | 0.3, 0.4 | 0.4 | 0.4, 0.4 | 0.2 | 0.2, 0.3 |
| [2002–2003] | 0.6 | 0.6, 0.6 | 0.7 | 0.7, 0.8 | 0.5 | 0.5, 0.5 |
| [2004–2005] | 0.8 | 0.8, 0.8 | 0.9 | 0.8, 0.9 | 0.7 | 0.7, 0.8 |
| [2006–2007] | 1.0 | 0.9, 1.0 | 1.0 | 0.9, 1.0 | 1.0 | 0.9, 1.0 |
| [2008–2009] | Reference | Reference | Reference | |||
| Cohortf | ||||||
| [1979–1990] | NA | NA | NA | NA | Reference | |
| [1991–2001] | NA | NA | NA | NA | 1.2 | 1.1, 1.3 |
Abbreviations: CI = Confidence Interval; NA = Not Applicable
Best-fitting model for any eating disorder (AED) outcome is Model III (Age + Period).
Best-fitting model for anorexia nervosa (AN) outcome is Model III (Age + Period).
Best-fitting model for other eating disorder (OED) outcome is Model VI (Age + Period + Cohort).
Coefficients (and lower and upper bounds of CIs) for age are transformed by exp(x)*100000, and represent model-based estimates of the incidence rate (per 100,000 person-years) for the age in question during the 2008–2009 period (and, in models with cohort effects, for the 1979–1990 birth cohort).
Coefficients (and lower and upper bounds of CIs) for period are transformed by exp(x), and represent model-based estimates of the multiplicative effect on incidence rates for the period in question relative to the 2008–2009 period.
Coefficients (and lower and upper bounds of CIs) for cohort are transformed by exp(x), and represent model-based estimates of the multiplicative effect on incidence rates for the cohort in question relative to the 1979–1990 birth cohort.
Table 4.
Coefficients (estimates and confidence intervals) from best-fitting Poisson models for males
| Any Eating Disordera
|
Anorexia Nervosab
|
Other Eating Disorderc
|
||||
|---|---|---|---|---|---|---|
| Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | |
| Age (in years)d | ||||||
| [8–9] | 6.8 | 5.1, 9.1 | 1.4 | 0.8, 2.5 | 6.7 | 4.9, 9.2 |
| [10–11] | 10.0 | 7.8, 12.8 | 4.2 | 2.9, 6.0 | 7.6 | 5.6, 10.2 |
| [12–13] | 23.0 | 19.2, 27.5 | 11.9 | 9.2, 15.3 | 14.1 | 11.2, 17.7 |
| [14–15] | 23.9 | 20.1, 28.5 | 10.6 | 8.2, 13.7 | 17.6 | 14.3, 21.6 |
| [16–17] | 25.2 | 21.2, 29.9 | 12.4 | 9.7, 15.8 | 17.7 | 14.4, 21.8 |
| [18–19] | 13.9 | 11.2, 17.3 | 6.0 | 4.4, 8.3 | 12.0 | 9.4, 15.4 |
| [20–21] | 10.6 | 8.2, 13.7 | 2.9 | 1.8, 4.6 | 10.3 | 7.8, 13.6 |
| [22–23] | 8.3 | 6.1, 11.2 | 3.1 | 1.9, 5.0 | 7.5 | 5.4, 10.4 |
| [24–25] | 8.4 | 6.1, 11.8 | 1.4 | 0.7, 3.1 | 8.5 | 6.1, 11.9 |
| [26–27] | 4.0 | 2.3, 7.0 | 1.5 | 0.6, 3.5 | 3.1 | 1.7, 5.9 |
| [28–30] | 5.0 | 2.7, 9.4 | 1.0 | 0.2, 4.0 | 4.0 | 2.0, 8.1 |
| Periode | ||||||
| [1987–1991] | 0.2 | 0.1, 0.4 | 0.1 | 0.0, 0.4 | 0.2 | 0.1, 0.4 |
| [1992–1997] | 0.1 | 0.1, 0.2 | 0.2 | 0.1, 0.2 | 0.1 | 0.1, 0.1 |
| [1998–1999] | 0.1 | 0.1, 0.2 | 0.2 | 0.1, 0.4 | 0.0 | 0.0, 0.1 |
| [2000–2001] | 0.2 | 0.1, 0.3 | 0.2 | 0.1, 0.3 | 0.2 | 0.1, 0.2 |
| [2002–2003] | 0.5 | 0.4, 0.6 | 0.6 | 0.5, 0.9 | 0.4 | 0.3, 0.5 |
| [2004–2005] | 0.7 | 0.6, 0.8 | 0.8 | 0.6, 1.0 | 0.6 | 0.5, 0.8 |
| [2006–2007] | 0.8 | 0.7, 1.0 | 0.9 | 0.7, 1.2 | 0.8 | 0.7, 1.0 |
| [2008–2009] | Reference | Reference | Reference | |||
| Cohort | ||||||
| [1979–1990] | NA | NA | NA | NA | NA | NA |
| [1991–2001] | NA | NA | NA | NA | NA | NA |
Abbreviations: CI = Confidence Interval; NA = Not Applicable
Best-fitting model for any eating disorder (AED) outcome is Model III (Age + Period).
Best-fitting model for anorexia nervosa (AN) outcome is Model III (Age + Period).
Best-fitting model for other eating disorder (OED) outcome is Model III (Age + Period).
Coefficients (and lower and upper bounds of CIs) for age are transformed by exp(x)*100000, and represent model-based estimates of the incidence rate (per 100,000 person-years) for the ages in question during the 2008–2009.
Coefficients (and lower and upper bounds of CIs) for period are transformed by exp(x), and represent model-based estimates of the multiplicative effect on incidence rates for the period in question relative to the 2008–2009 period.
For females, Model III (Age + Period) fit the AN data best, suggesting that AN incidence differed by age and period, but not by cohort once the effects of age and period were accounted for. In Model III, the incidence of AN (per person-year) peaked at the 15 year old age category, with incidence for 15 year olds estimated to be 226.5 cases per 100,000 person-years (95% CI: 210.7, 243.5) in 2008–2009. Further, the incidence of AN increased throughout the study period, with incidence being significantly lower (than in the 2008–2009 reference period) for all periods between 1990–1991 and 2004–2005. For the OED outcome, Model VI (Age + Period + Cohort) fit the data best, suggesting that OED incidence differed by age, period, and cohort. In Model VI, the incidence of OED peaked at the 17 and 18 year old age categories, with incidence for 18 year olds estimated to be 305.7 cases per 100,000 person-years (95% CI: 285.4, 327.3) in 2008–2009. Further, the incidence of OED increased throughout the study period, with incidence being significantly lower (than in 2008–2009) for all periods up through 2004–2005. Finally, the incidence of OED was slightly, but significantly, higher for the 1991–2001 cohort relative to the 1979–1990 cohort.
For males, Model III (Age + Period) fit the AN data best. In Model III, the incidence of AN (per person-year) peaked at the 12–13, 14–15, and 16–17 year old age categories, with incidence for 16–17 year olds estimated to be 12.4 cases per 100,000 person-years (95% CI: 9.7, 15.8) in 2008–2009. Further, the incidence of AN increased throughout the study period, with incidence being significantly lower (than in 2008–2009) for all periods up through 2002–2003. For the OED outcome, Model III (Age + Period) again fit the data best. In Model III, the incidence of OED peaked at the 14–15 and 16–17 year old age categories, with incidence for 16–17 year olds estimated to be 17.7 cases per 100,000 person-years (95% CI: 14.4, 21.8) in 2008–2009. Further, the incidence of OED increased throughout the study period, with incidence being significantly lower (than in 2008–2009) for all periods up through 2004–2005.
Discussion
Our study is one of the largest and most rigorous studies to date to identify age- and sex-specific patterns in the incidence of healthcare-register-recorded eating disorders over time. Swedish population and healthcare registers comprising 2.3 million individuals aged 8 to 30 years captured 16,403 eating disorder cases (0.7% of the initial birth cohort) detected and recorded between the years of 1987 and 2009. The finding that detection of AN begins to peak at an unexpectedly early age in boys is novel and has important implications for healthcare service and primary prevention planning and direction for future research.
The sex differences in healthcare-register-recorded eating disorder incidence were dramatic. Similar to other register-based study findings in the UK (primary care detected cases only)34 and Denmark,6,35 incidence was more than 10 times higher in females than males. For example, in 2009, incidence of AN was 205.9 cases per 100,000 persons (95% CI: 178.2, 233.5) at peak age of detection in females and 12.8 cases per 100,000 persons (95% CI: 5.6, 20.1) at peak age of detection in males. Similarly, incidence of OED was 372.1 cases per 100,000 persons (95% CI: 336.4, 407.9) at peak age of detection in females and 22.2 cases per 100,000 persons (95% CI: 13.3, 31.1) at peak age of detection in males. This discrepancy may be due to actual sex differences in the incidence of eating disorders, sex differences in treatment seeking, or providers’ failure to detect eating disorders in men. Regarding the last two hypotheses, studies suggest that males may be less likely than females to seek treatment for an eating disorder36 and that healthcare providers may fail to detect eating disorders in men because they do not include eating disorders among differential diagnoses, they use assessments that are normed on females, or fail to use male-specific measures.37 Although nationally-representative community studies in the United States38 and Canada39 have documented a less extreme male:female ratio of eating disorders, supporting either of the above-two hypotheses, females were still disproportionally affected.
Early to late adolescence is a high-risk period for the development of an eating disorder. Our findings of peak detection in the teenage years is consistent with other register-based studies6,35 and community studies of self-reported eating disorder onset.25,38 Existing literature identifies the adolescent period, especially puberty,38 as a high risk time for the onset of eating disorders owing to genetic, biological, and sociocultural factors and their interplay during this period.40–42 Similar to other register-based studies,35 the peak-detection age in our study was earlier for AN than OED, reflecting either actual earlier age at onset of AN or earlier detection of the disorder.
In our study, incidence of AN and OED began peaking at a younger age (about 3 years earlier) for males than females. For AN, incidence (per person-year) peaked at 12–17 years for males versus 15 years for females. For OED, incidence peaked at 14–17 years for males versus 17–18 years for females. Our analytic approach did not allow us to test formally whether the sex differences in peak age of first diagnosis captured in the registers were statistically significant. However, the findings of sex differences are consistent with other similar (though not directly comparable) register studies,35,43 albeit not with one other study that found no sex differences in age at admission to a specialized eating disorder unit.44 In contrast, the somewhat contradictory literature on retrospectively-reported age of eating disorder onset (not examined here)43–45 generally supports younger onset in females than males, suggesting our findings may indicate earlier age at detection, but not onset, of eating disorders in males. Additional studies are needed to test this hypothesis by examining sex differences in age of onset versus detection in large samples with wide age ranges. In general, our findings suggest that primary prevention programs should be implemented prior to or early in adolescence and should ensure that parents and providers are aware of sex-specific signs of emerging eating pathology.
The incidence of both AN and OED was substantially lower in calendar years prior to 2000, with age-period-cohort modeling indicating that this decrease was primarily attributable to diagnostic period effects rather than birth cohort effects. Regarding diagnostic period effects, the incidence of detected eating disorders was significantly lower in earlier periods than in the final 2008–2009 period. Given that the NPR achieved complete coverage of outpatient clinics and the quality assurance registers (Riksät and Stepwise) came online during the 2000s, it is likely that the observed increase in incidence for diagnostic periods after 2000 is at least partly due to expansion in the coverage of the healthcare registers. Regarding birth cohort effects, the incidence rate for the 1980s versus 1990s birth cohorts did not differ, except for OED where incidence was slightly higher in females born in the 1990s, suggesting a general lack of birth cohort effects in recent decades. Comparing the above results to other studies of eating disorder incidence5,34 is not straightforward due to methodological differences and because the referenced studies do not decompose calendar time trends into period and cohort effects. Generally, it is difficult for researchers to determine whether the incidence of eating disorders is truly increasing over time given that epidemiological studies with long follow-up periods, such as the one reported here, are sensitive to methodological changes (e.g., variations in disorder criteria, register policy, detection methods, and availability of services) and changes in population composition.5 Regardless, our findings indicate that it is essential to adjust for diagnostic period when using Swedish registers to examine risk factors for eating disorders, especially for risk factors whose levels change systematically over time.
Limitations
Our study has considerable strengths and overcomes many of the limitations common to previous studies of incidence (small sample size, failure to consider period and cohort effects, use of limited diagnostic periods). However, our study does have some limitations, and it is important to address those limitations and their implications systematically.
First, because age, period, and cohort are confounded in continuous time (i.e., knowing two determines the third), their effects can only be separated by making assumptions.46 In our analyses, the manner in which we categorized age, period, and cohort implied certain assumptions regarding the functional form of the relationship between incidence and those variables, which may or may not be valid. Second, because the Swedish healthcare registers did not include standard eating disorder diagnoses prior to the introduction of ICD-9 in 1987, we could not include individuals born prior to 1979 in our cohort since it was not possible to ensure that any eating disorder diagnosis they received during the study period (1987–2009) was actually their first instance of a healthcare-detected eating disorder (from 8 years on). As a result, the data did not contain information on incidence for the older age categories during the earlier period categories, limiting the precision of estimates for those age categories. Further, by the end of the study period (2009), the oldest individuals included in our cohort were only 30 years old, which precluded investigation of incidence in older age categories. Third, because BN and BED could not be differentiated from other eating disorders prior to 1997, we were unable to determine the incidence of these disorders separately (from OED) without compromising power. Fourth, the registers did not achieve near-complete ascertainment of healthcare-detected eating disorder cases until recently.7,14 However, we addressed this limitation by highlighting age- and sex-specific incidence for 2009 (the most recent diagnostic year included in the study).
When considering results, it is also important to emphasize that registers capture detected and recorded eating disorders only, and not non-treatment-seeking or non-medically-detected cases. Also, registers in this study did not include cases that were detected only in primary care. In Sweden, nearly all individuals with a potential eating disorder diagnosis detected in primary care are referred to specialist care for a thorough diagnostic evaluation and treatment, but there may be some individuals who end up in another type of care or do not follow-up with referrals and, thus, are not captured in this study—to our knowledge, these cases are the exception. Thus, estimates of incidence for (healthcare detected and recorded) eating disorders likely underestimate the incidence of all eating disorder cases. Also of note, studies validating ICD-9 eating disorder diagnoses in the NPR were not performed; encouragingly, however, validation studies of schizophrenia show good results, and positive predictive values (PPV) between 85% and 95% have been recorded for a range of inpatient diagnoses.15
In addition, differences in the incidence of (healthcare detected and recorded) eating disorders with respect to sex, age, cohort or diagnoses can reflect differences in detection, as well as differences in actual incidence, with respect to these factors, as noted above in our discussion of sex differences. Relatedly, registers capture information only on age at diagnosis, not age of onset. A substantial gap between eating disorder onset and treatment exists,47,48 and any interpretation of our results should bear this in mind, especially because the quality registers do not include diagnoses made in primary care, which may occur closer to eating disorder onset if first presentation is in primary care.
However, despite being limited to detected and recorded cases, register-based cohort studies provide vital information that complements information derived from community-based studies that use historical interviews.38,49–51 Community-based studies capture non-medically-detected cases, but they are subject to recall and reporting bias and are limited to surviving individuals.6 The latter point is a particular limitation for AN given its elevated mortality rate.1 In contrast, register-based studies do not rely on participant report and can include all members of a particular birth cohort, not only survivors. Finally, register-based studies are especially rich resources for documenting recent healthcare utilization, which is essential for healthcare planning.
Conclusions
Incidence of healthcare-register-recorded eating disorders in Sweden is higher in females than males. Adolescence is the most likely time for eating disorders to emerge, and, unexpectedly, the peak age of detection is somewhat younger in males. Our data suggest that detection and primary prevention efforts should begin in late childhood or early adolescence and that vigilance for signs of impending AN in young males (e.g., falling off the growth curve, dramatic changes in eating habits, body shape or weight preoccupation, or driven exercise) is warranted. Waiting until later could miss critical windows for intervention that could prevent disorders from taking root or increasing in severity or duration.
Supplementary Material
Acknowledgments
This research was supported by the American Foundation for Suicide Prevention (PI: Bulik) and the Anorexia Nervosa Genetics Initiative (ANGI) an initiative of the Klarman Family Foundation (L.M.T., C.M.B.). C.D.R. was supported by the Global Foundation for Eating Disorders (PIs: Bulik and Baucom; www.gfed.org) and K.J. was supported by the National Institutes of Mental Health (PI: Bulik; T32MH076694). Riksät is financially supported by the Swedish Association of Local Authorities and Regions. The Stepwise database is financially supported by Stockholm County Council.
Footnotes
Conflict of Interest
Dr. Bulik is a consultant for Shire. No other authors have a declaration of interest to disclose.
References
- 1.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13:153–60. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 3.Crow S. The economics of eating disorder treatment. Curr Psychiatry Rep. 2014;16:454. doi: 10.1007/s11920-014-0454-z. [DOI] [PubMed] [Google Scholar]
- 4.Rothman KJ, Greenland S, Lash TJ. Modern Epidemiology. Third. Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 5.Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence, and mortality rates. Curr Psychiatry Rep. 2012;14:406–14. doi: 10.1007/s11920-012-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71:573–81. doi: 10.1001/jamapsychiatry.2014.16. [DOI] [PubMed] [Google Scholar]
- 7.Swedish Association of Local Authorities and Regions. National Healthcare Quality Registeries in Sweden 2007. Stockholm: Swedish Association of Local Authorities and Regions; 2007. [Google Scholar]
- 8.Clayton D, Schifflers E. Models for temporal variation in cancer rates. I: age–period and age–cohort models. Stat Med. 1987;6:449–67. doi: 10.1002/sim.4780060405. [DOI] [PubMed] [Google Scholar]
- 9.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24:659–67. doi: 10.1007/s10654-009-9350-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Statistics Sweden. Background facts, to measure and monitor internal migration based on national population register: IAOS Conference; Ottawa, Canada. Stockholm, Sweden: Statistics Sweden; 2006. [Google Scholar]
- 11.Statistics Sweden. Folk- och bostadsräkningar, FoB. http://www.scb.se/Pages/List____257507.aspx. Accessed 11/25/2011.
- 12.National Board of Health and Welfare, NBHW. Causes of Death. National Board of Health and Welfare; 2010. [Google Scholar]
- 13.Center for Epidemiology at the National Board of Health and Welfare, NBHW. The National Patient Register. http://www.socialstyrelsen.se/register/halsodataregister/patientregistret/inenglish. Accessed May 10 2012.
- 14.Birgegård A, Björck C, Clinton D. Quality assurance of specialised treatment of eating disorders using large-scale internet-based collection systems: methods, results and lessons learned from desiging the Stepwise database. Eur Eat Disord Rev. 2010;18:251–9. doi: 10.1002/erv.1003. [DOI] [PubMed] [Google Scholar]
- 15.Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450–66. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO, World Health Organization. International Classification of Diseases. 9th. Geneva: 1978. revised. [Google Scholar]
- 17.WHO, World Health Organization. International Classification of Diseases. 10th. Geneva: 1992. revised. [Google Scholar]
- 18.APA. American Psychiatric Association. (DSM-IV-TR) Diagnostic and statistical manual of mental disorders, 4th edition, text revision. Washington, DC: American Psychiatric Press, Inc; 2000. [Google Scholar]
- 19.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for the DSM-IV Axis I Disorders–Patient Edition (SCID-I/P, Verson 2.0) New York: Biometrics Research Department: New York State Psychiatric Institute; 1996. [Google Scholar]
- 20.Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavas J, Weiller E, et al. The Mini International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 21.von Knorring L, von Knorring AL, Björck C. MINI International neuropsychiatric interview for children and adolescents: Swedish version 2.1. Uppsala/Stockholm: Uppsala University/Karolinsak Institutet; 2003. [In Swedish] [Google Scholar]
- 22.de Man Lapidoth J, Birgegård A. Validation of the Structured Eating Disorder Interview (SEDI) against the Eating Disorder Examination (EDE) Stockholm: Karolinska Institutet; 2010. [Google Scholar]
- 23.Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? Int J Eat Disord. 2009;42:581–9. doi: 10.1002/eat.20720. [DOI] [PubMed] [Google Scholar]
- 24.Allen KL, Byrne SM, Oddy WH, Crosby RD. DSM-IV-TR and DSM-5 eating disorders in adolescents: prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. J Abnorm Psychol. 2013;122:720–32. doi: 10.1037/a0034004. [DOI] [PubMed] [Google Scholar]
- 25.Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Psychol. 2013;122:445–57. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.SAS/SAT 9.3 User’s Guide. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- 27.R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2014. http://www.R-project.org/. [Google Scholar]
- 28.Szklo M, Nieto FJ. Epidemiology: beyond the basics. Burlington, MA: Jones & Bartlett Learning; 2014. [Google Scholar]
- 29.Clayton D, Schifflers E. Models for temporal variation in cancer rates. II: age–period–cohort models. Stat Med. 1987;6:469–81. doi: 10.1002/sim.4780060406. [DOI] [PubMed] [Google Scholar]
- 30.Laird N, Olivier D. Covariance analysis of censored survival data using log-linear analysis techniques. J Amer Stat Assoc. 1981;76:231–40. [Google Scholar]
- 31.Hemminki K, Li X, Mutanen P. Age-incidence relationships and time trends in cervical cancer in Sweden. Eur J Epid. 2001;17:323–8. doi: 10.1023/a:1012761717028. [DOI] [PubMed] [Google Scholar]
- 32.Cameron AC, Trivedi PK. Microeconometrics: Methods and Applications. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- 33.Cameron AC, Trivedi PK. Regression-based tests for overdispersion in the Poisson model. J Econometrics. 1990;46:347–364. [Google Scholar]
- 34.Micali N, Hagberg KW, Petersen I, Treasure JL. The incidence of eating disorders in the UK in 2000–2009: findings from the General Practice Research Database. BMJ Open. 2013;3:1–7. doi: 10.1136/bmjopen-2013-002646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zerwas S, Larsen JT, Petersen L, Thornton LM, Mortensen PB, Bulik CM. The incidence of eating disorders in a Danish register study: associations with suicide risk and mortality. J Psychiatr Res. 2015;65:16–22. doi: 10.1016/j.jpsychires.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carlat DJ, Carmago CA. Review of bulimia nervosa in males. Am J Psychiatry. 1991;148:831–43. doi: 10.1176/ajp.148.7.831. [DOI] [PubMed] [Google Scholar]
- 37.Darcy AM, Lin IH. Are we asking the right questions? A review of assessment of males with eating disorders. Eat Disord. 2012;20:416–26. doi: 10.1080/10640266.2012.715521. [DOI] [PubMed] [Google Scholar]
- 38.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–58. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pinhas L, Morris A, Crosby RD, Katzman DK. Incidence and age-specific presentation of restrictive eating disorders in children: a Canadian Paediatric Surveillance Program study. Arch Pediatr Adolesc Med. 2011;165:895–9. doi: 10.1001/archpediatrics.2011.145. [DOI] [PubMed] [Google Scholar]
- 40.Klump KL. Puberty as a critical risk period for eating disorders: a review of human and animal studies. Hormones and Behavior. 2013;64:399–410. doi: 10.1016/j.yhbeh.2013.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Klump KL, Burt SA, McGue M, Iacono WG. Changes in genetic and environmental influences on disordered eating across adolescence: a longitudinal twin study. Arch Gen Psychiatry. 2007;64:1409–15. doi: 10.1001/archpsyc.64.12.1409. [DOI] [PubMed] [Google Scholar]
- 42.Keel PK, Forney KJ. Psychosocial risk factors for eating disorders. Int J Eat Disord. 2013;46:433–9. doi: 10.1002/eat.22094. [DOI] [PubMed] [Google Scholar]
- 43.Støving RK, Andries A, Brixen K, Bilenberg N, Hørder K. Gender differences in outcome of eating disorders: a retrospective cohort study. Psychiatry Research. 2011;186:362–6. doi: 10.1016/j.psychres.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 44.Braun DL, Sunday SR, Huang A, Halmi KA. More males seek treatment for eating disorders. Int J Eat Disord. 1999;25:415–24. doi: 10.1002/(sici)1098-108x(199905)25:4<415::aid-eat6>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 45.Gueguen J, Godart N, Chambry J, Brun-Eberentz A, Foulon C, Divac SM, et al. Severe anorexia nervosa in men: comparison with severe AN in women and analysis of mortality. Int J Eat Disod. 2012;45:537–45. doi: 10.1002/eat.20987. [DOI] [PubMed] [Google Scholar]
- 46.Osmond C, Gardner MJ. Age, period, and cohort models non-overlapping cohorts don’t resolve the identification problem. Am J of Epidemiology. 1989;129:31–5. doi: 10.1093/oxfordjournals.aje.a115121. [DOI] [PubMed] [Google Scholar]
- 47.Nicholls DE, Lynn R, Viner RM. Childhood eating disorders: British national surveillance study. Brit J Psychiatry. 2011;198:295–301. doi: 10.1192/bjp.bp.110.081356. [DOI] [PubMed] [Google Scholar]
- 48.de la Rie S, Noordenbos G, Donker M, Van Furth EF. Evaluating the treatment of eating disorders from the patient’s perspective. Int J Eat Disord. 2006;39:667–76. doi: 10.1002/eat.20317. [DOI] [PubMed] [Google Scholar]
- 49.Keski-Rahkonen A, Hoek HW, Linna MS, Raevuori A, Sihvola E, Bulik CM, et al. Incidence and outcomes of bulimia nervosa: a nationwide population-based study. Psychol Med. 2009;39:823–31. doi: 10.1017/S0033291708003942. [DOI] [PubMed] [Google Scholar]
- 50.Keski-Rahkonen A, Hoek HW, Susser ES, Linna MS, Sihvola E, Raevuori A, et al. Epidemiology and course of anorexia nervosa in the community. Am J Psychiatry. 2007;164:1259–65. doi: 10.1176/appi.ajp.2007.06081388. [DOI] [PubMed] [Google Scholar]
- 51.Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization mental health surveys. Biol Psychiatry. 2013;73:904–14. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


