Abstract
Y1 receptor (Y1R)-signalling pathway plays a pivotal role in the regulation of bone metabolism. The lack of Y1R-signalling stimulates bone mass accretion that has been mainly attributed to Y1R disruption from bone-forming cells. Still, the involvement of Y1R-signalling in the control of bone-resorbing cells remained to be explored. Therefore, in this study we assessed the role of Y1R deficiency in osteoclast formation and resorption activity. Here we demonstrate that Y1R germline deletion (Y1R−/−) led to increased formation of highly multinucleated (n > 8) osteoclasts and enhanced surface area, possibly due to monocyte chemoattractant protein-1 (MCP-1) overexpression regulated by RANKL-signalling. Interestingly, functional studies revealed that these giant Y1R−/− multinucleated cells produce poorly demineralized eroded pits, which were associated to reduce expression of osteoclast matrix degradation markers, such as tartrate-resistant acid phosphatase-5b (TRAcP5b), matrix metalloproteinase-9 (MMP-9) and cathepsin-K (CTSK). Tridimensional (3D) morphologic analyses of resorption pits, using an in-house developed quantitative computational tool (BonePit), showed that Y1R−/− resorption pits displayed a marked reduction in surface area, volume and depth. Together, these data demonstrates that the lack of Y1Rs stimulates the formation of larger multinucleated osteoclasts in vitro with reduced bone-resorbing activity, unveiling a novel therapeutic option for osteoclastic bone diseases based on Y1R-signalling ablation.
Osteoclasts are highly specialized multinucleated cells involved in bone resorption that derive from precursor cells of the hematopoietic lineage1. Bone-resorbing osteoclasts act in a concerted manner with bone-forming osteoblasts to accomplish bone remodelling, where old and damaged bone is resorbed followed by the formation of new bone2. The exacerbation of osteoclast-resorbing activity observed in cases of metabolic bone diseases (e.g. osteoporosis, Paget’s disease)3, metastatic bone disease4 and rheumatoid arthritis5, results in the formation of fragile bones, increased risk of fracture and disability, leading to serious pathological conditions and possibly to death. Hence, uncovering putative signalling pathways that control osteoclast activity is of vital importance and might unfold new promising treatment options.
Traditionally, bone remodelling is viewed as a complex process regulated by hormonal, autocrine/paracrine and mechanical signals. However, growing evidence has shown that signalling molecules supplied by skeletal sympathetic and sensorial nerve fibbers might also be directly involved in the control of bone turnover through neurotransmitter receptors expressed by bone cells6. Among the neurotransmitters expressed in bone microenvironment, described to modulate bone mass, emerges the neuropeptide Y (NPY) system through Y1R signalling pathway7,8,9.
Several findings supported a generalized and powerful peripheral action of Y1R signalling in the regulation of bone mass. Both germ line and osteoblast-specific Y1R deletion resulted in significantly greater cancellous and cortical bone volume in femoral, tibia, and vertebrae bones in mice7,8. Previous work from our group have also shown that the systemic blockade of Y1R signalling stimulates pronounced increments on bone mass10. These anabolic effects have been exclusively attributed to increased osteoblast activity, given that Y1Rs are expressed in differentiated osteoblasts11 and that the specific deletion of receptors from mature osteoblasts augmented osteoblast differentiation and activity12. Nonetheless, the involvement of Y1R signalling in bone turnover via osteoclast activity remains to be fully addressed. Y1R has been shown to be robustly expressed by immune cells (e.g. T-cells, monocytes and macrophages)13 and to play a pivotal role in macrophage function14. Since both osteoclasts and macrophages share a common progenitor lineage, these studies suggest a direct role for Y1Rs in osteoclast progenitors activity. Moreover, tartrate-resistant acid phosphatase (TRAP)-stained bone histological sections revealed an increase in osteoclast surface upon disruption of Y1R signalling in mice7,10.
In the light of these indications, we hypothesize that Y1R signalling pathway might also be involved in the regulation of osteoclast activity and function, thus acting in both arms of bone remodelling. Hence, the aim of this study was to investigate the functional role of Y1R signalling in osteoclastogenesis and bone matrix resorption, using bone marrow-derived osteoclasts retrieved from wild-type (WT) and Y1R germ line knockout (Y1R−/−) mice. Moreover, we have also developed a novel computational tool – BonePit – that allowed to perform a detailed morphologic analysis of the resorption pits produced by osteoclasts in a 3D space.
Results
Y1R gene expression is upregulated during osteoclastogenesis
Previous studies have demonstrated that Y1−/− mice retain a high-bone mass phenotype7. This feature has been associated with increased osteoblast activity and bone formation. Nevertheless little is known regarding the involvement of Y1R signalling in osteoclast function. Hence, we have first assessed the expression profile of Y1R during all stages of osteoclast differentiation15, using bone marrow retrieved from WT mice. The Y1R mRNA expression was demonstrated to be substantially upregulated throughout osteoclast differentiation (osteoclast fusion and maturation) by quantitative real-time PCR (qPCR) analysis (Fig. 1). As depicted in Fig. 1, Y1R gene expression increased considerably upon the differentiation of bone marrow-derived monocytes into small round mononucleated TRAP-positive cells (pre-osteoclasts) and the formation of multinucleated TRAP-positive cells (mature osteoclasts). These results provided the first indication that Y1Rs might play a regulatory function in osteoclast activity.
Figure 1. Y1R gene expression profile during osteoclastogenesis.
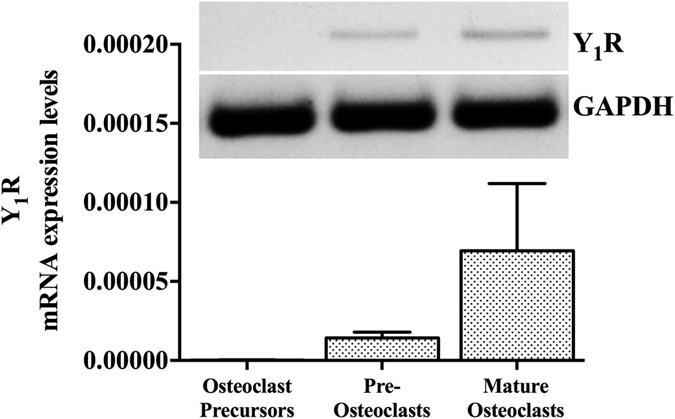
The expression of Y1R is upregulated during osteoclast differentiation, as determined by qRT-PCR analysis. Values are normalized to GADPH levels (housekeeping gene). Data is expressed as mean ± SEM.
It is widely accepted that RANKL signalling pathway plays a role in osteoclast formation and differentiation16. Accordingly, the expression of RANKL and decoy receptor osteoprotegerin (OPG) was quantified by qRT-PCR analysis, using WT and Y1−/− osteoblast cultures (Supplementary Information Fig. S1). Quantitative analysis revealed that RANKL gene expression is elevated in Y1R−/− osteoblast cultures (p < 0.05), while no differences were detected for OPG when compared to WT cultures. Importantly, the RANKL/OPG ratio was significantly elevated in Y1R−/− cultures (p < 0.001). These data confirmed our previous hypotheses involving the Y1R signalling pathway on osteoclastogenesis.
Y1R signalling deficiency stimulates the formation of larger osteoclasts
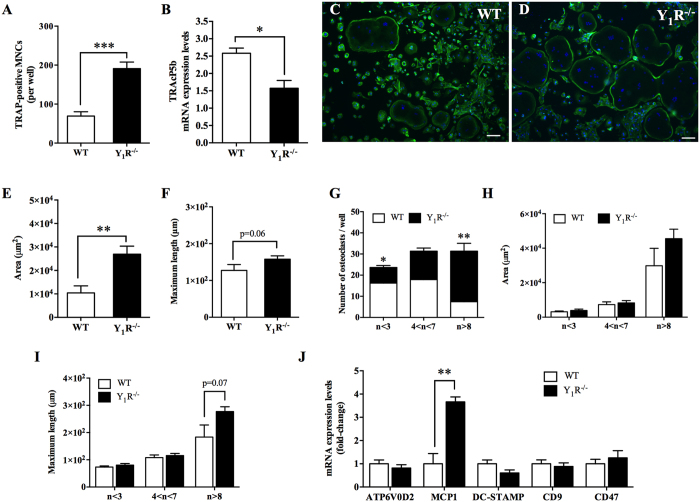
To evaluate the specific role of Y1R in osteoclast differentiation, osteoclast precursors retrieved from WT and Y1R−/− mice were stimulated in the presence of M-CSF and RANKL. As a first measure outcome, the number of TRAP-positive multinucleated cells (MNCs) with more than 3 nuclei was quantified. Y1R−/− cultures showed a 2-fold increase in the number of TRAP-positive MNCs (with more than 3 nuclei) when compared to their WT counterparts (Fig. 2A; p < 0.001). Interestingly, although the number of TRAP-positive MNCs with more than 3 nuclei is increased in Y1R−/− cultures, a trend towards decreased TRAcP5b activity (a marker of osteoclast activity) has been observed when compared to WT cultures (Fig. 2B; p = 0.1). Moreover, qRT-PCR analysis demonstrated that TRAcP5b expression levels were also reduced in Y1R−/− osteoclasts (Fig. 2C; p < 0.05), suggesting Y1R−/− osteoclast activity might be impaired.
Figure 2. Y1R modulates osteoclast precursors fusion and osteoclast formation.
The lack of Y1R signalling promoted an increase in the number of TRAP-positive multinucleated (MNCs) cells with more than 3 nuclei (A), while TRAcP5b mRNA expression levels (B) are decreased. The formation of podosome belts was observed in both WT (C) and Y1R−/− (D) conditions. Quantitative analysis showed that Y1R−/− osteoclasts have an elevated surface area (E) and a trend towards increased maximum length (F). Moreover, the number of osteoclasts with more than 8 nuclei is also elevated in Y1R−/− cultures (G). Nevertheless, there were no differences between genotypes on osteoclast area (H) and in maximum length (I) per each category. The gene expression of key markers of migration and fusion revealed that MCP-1 is significantly upregulated, as determined by qRT-PCR analysis (J). Data is expressed as mean ± SEM. *p < 0.05, **p < 0.01, ***p < 0.001 different from WT. Scale bar = 100 μm.
The morphology of the WT and Y1R−/− osteoclasts was then analysed by F-actin immunostaining (Fig. 2D,E). The formation of a characteristic podosome belt by the multinucleated cells was detected in both genotypes (WT versus Y1R−/−) in plastic plates. As shown in Fig. 2F,G, quantification analysis revealed a significant increase in the Y1R−/− osteoclast surface area (p < 0.01) and a trend towards increased maximum length (p = 0.06), when compared to WT osteoclasts. These pieces of evidence indicate an increase in the size of osteoclasts in Y1R−/− mice.
To characterize in more detailed the differences observed, multinucleated osteoclasts were grouped into three categories based on the number of nuclei per cell: a) n < 3; b) 4 < n < 7; and c) n > 8. As depicted in Fig. 2H, 53% of Y1R−/− osteoclasts have more than 8 nuclei (n > 8) when compared to the 18% of WT osteoclasts (p < 0.01), and only 17% of Y1R−/− osteoclasts have less than 3 nuclei (n < 3), when compared to 39% of WT osteoclasts (p < 0.05). Moreover, similar percentages were observed at the category 4 < n < 7 between the two groups. Nevertheless, no statistical differences between genotypes could be observed regarding the osteoclast area (Fig. 2I) and maximum length (p = 0.07; Fig. 2J) for each category, suggesting that the increase in Y1R−/− osteoclast surface area and diameter is independent of the number of nuclei.
Taking into account that Y1R seems to stimulate the formation of larger multinucleated cells, we have then proposed to evaluate the expression of key markers of osteoclast precursors migration and fusion17 that might be upregulated in Y1R−/− mice (Fig. 2K). Among the osteoclast fusion markers studied, quantitative analysis revealed that the expression of MCP-1 (also known as CCL2), known to be involved in osteoclast differentiation in a RANKL dependent manner18, was significantly elevated in Y1R−/− osteoclasts (Fig. 2K; p < 0.01). Interestingly, no statistical differences were found in the gene expression of Atp6v0d2 (a component of the v-ATPase involved in osteoclast fusion that exerts its function through direct cell-cell contact), DC-STAMP (a RANKL-dependent transmembrane protein that is fundamental in osteoclast fusion), CD9 and CD47 (membrane proteins involved in cell fusion and cell recognition, respectively)17.
Y1R deletion impairs matrix demineralization
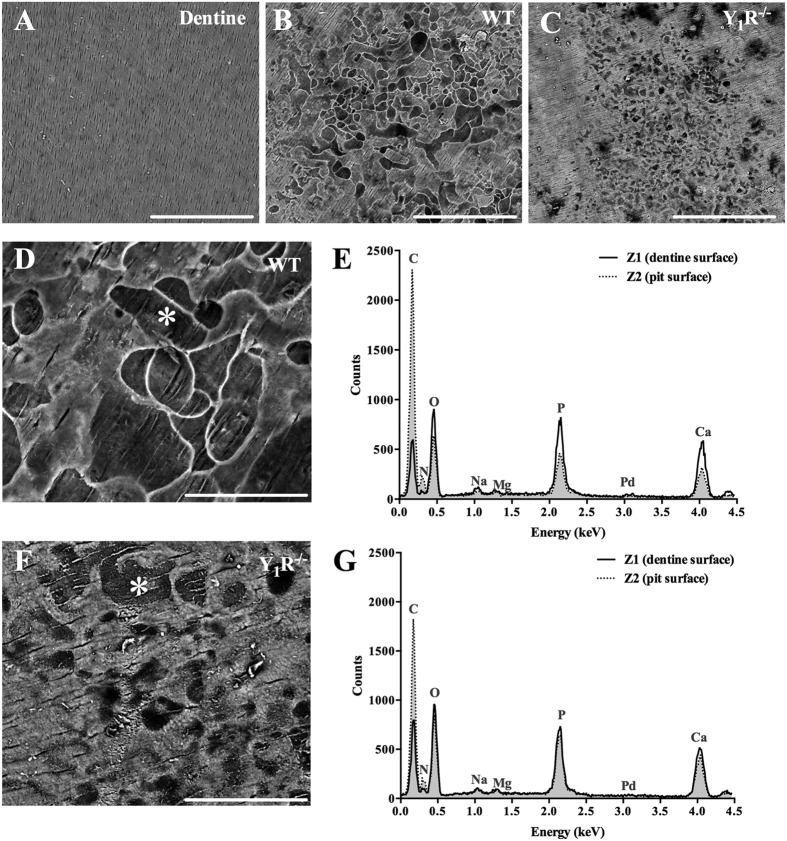
To date, there are no published data reporting the specific effects of Y1R in osteoclast-resorbing capacity. In order to clarify this, osteoclast precursors were cultured on top of dentine substrate discs (untreated discs are displayed in Fig. 3A) in the presence of M-CSF and RANKL, to evaluate the resorbing activity of osteoclasts. These dentine discs are mainly constituted by a mineralized collagen matrix (collagen filaments covered by a hydroxyapatite layer) and are used in in vitro studies as bone resorption substrates19.
Figure 3. Y1R deficiency impairs the resorption of the mineralized surface.
Osteoclast matrix resorptive activity was evaluated using dentine discs as substrates (A). Osteoclast precursors were seeded on top of dentine substrates. SEM analysis demonstrated that the lack of Y1R modulated the resorptive activity of osteoclasts resulting in a diminished eroded area, as depicted by representative micrographs of WT (B) and Y1R−/− (C) dentine discs. EDS analysis of the dentine and pit (*) surfaces revealed a significant decrease in phosphate and calcium in WT eroded surfaces (D,E). These differences were not so prominent when comparing non-eroded and eroded Y1R−/− surfaces (F,G). Scale bar (A–C) = 200 μm; Scale bar (D,F) = 50 μm.
After culture, dentine substrates were scanned by electron microscopy (SEM). As shown by representative microphotographs in Fig. 3, Y1R−/−-cultured dentine substrates comprise a smaller region of resorptive area, and the resorption pits appear to be smaller and narrower (Fig. 3C,F), when compared to WT-cultured dentine substrates (Fig. 3B,D). Additionally, considering that darker regions correspond to exposed collagen, Y1R−/− resorption pits are less deep than WT (as represented by brighter regions). To confirm these observations, the surface of the dentine discs was analysed by Energy dispersive X-ray spectroscopy (EDS) analysis (Fig. 3E,G), where the discrete energy of the backscattered electrons is used to roughly obtain the surface atomic composition up to few nanometers deep20. In both conditions, the dentine surface has been compared to the resorption pit surface (*), as illustrated in Fig. 3D–G. As expected, in WT dentine discs the phosphate and calcium peaks are elevated at the surface of the dentine, while the carbon peak is higher in the pit surface than in dentine surface (dashed line), most likely due to the exposure of collagen fibres each is mainly constituted by carbon (Fig. 3E). Interestingly, in Y1R−/− dentine discs the differences observed in calcium and phosphate peaks in dentine and pit (dashed line) surfaces are not as steeper as for WT (Fig. 3G), suggesting an inferior exposure of collagen fibres and reduced matrix demineralization in dentin discs cultured with Y1R−/− osteoclast precursors.
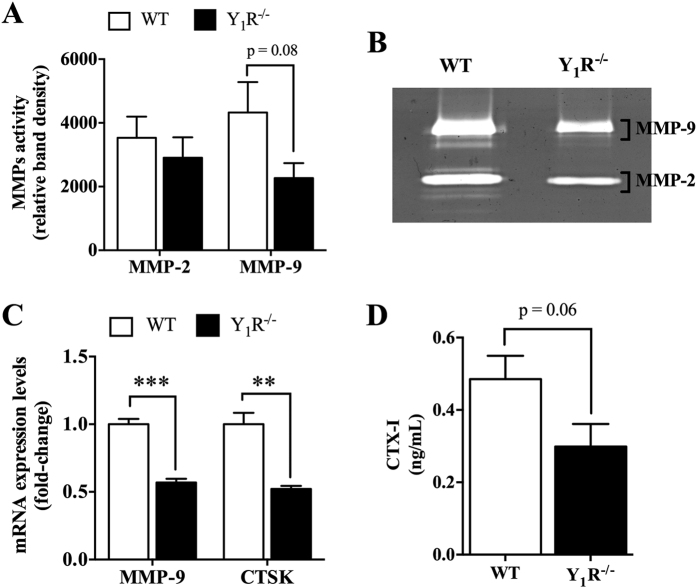
Subsequently, we have then explored the expression profile of key factors critical for the resorption of mineralized matrices, such as matrix metalloproteinases (MMPs) and CTSK, expressed by osteoclasts to degrade the organic components of bone matrix21,22. The quantitative analysis of gelatin zymography allowed us to demonstrate that there is a trend towards decreased MMP-9 activity in Y1R−/− cultures when compared to WT (p = 0.08), while the proteolytic activity of MMP-2 was not different between groups (Fig. 4A,B). This was further confirmed by qRT-PCR analysis, where the MMP-9 mRNA expression levels were shown to be significantly downregulated in Y1R−/− cultures (Fig. 4C; p < 0.001). In addition, the mRNA expression of CTSK was also diminished (Fig. 4C; p < 0.01). Furthermore, the quantification of degradation products from collagen I, such as C-terminal telopeptide (CTX-I) levels, revealed to be diminished in Y1R−/− cultures when compared to WT (p = 0.06; Fig. 4D). Overall, the attenuation of collagen degradation correlates well with decreased matrix degradation, suggesting that bone matrix resorption might be impaired in Y1R−/− cultures.
Figure 4. Y1R deficiency inhibits the expression of essential bone-resorbing factors.
The proteolytic activity of MMP-9 in Y1R−/− osteoclasts was slightly diminished, as determined by gelatin zymography (A,B). In agreement, the mRNA expression levels of MMP-9 and CSTK were also downregulated in Y1R−/− cultures (C), which resulted in a trend towards decreased levels of released CTX-I (D). Data is expressed as mean ± SEM. **p < 0.01, ***p < 0.001 different from WT.
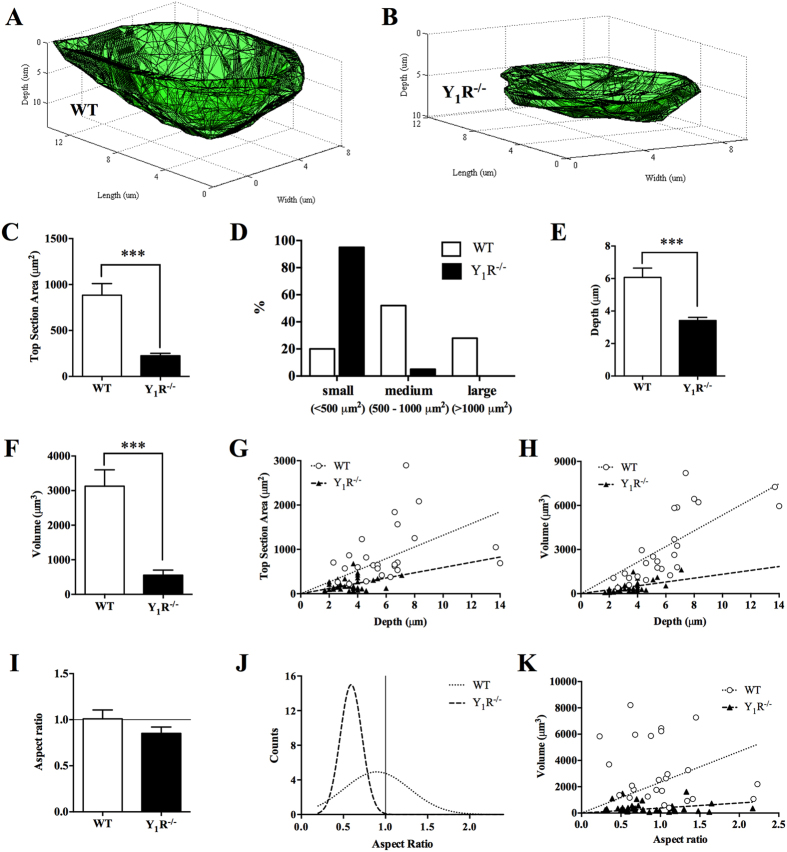
Y1R deletion leads to the formation of small resorption pits
In order to better appreciate the differences observed in eroded surfaces between WT and Y1R−/− cultures, we have developed a computational tool (BonePit algorithm) that enabled us to quantify in detail relevant pit morphologic features in a 3D space, such as pit top section area, volume, depth and aspect ratio. The 3D reconstruction of the resorption pits revealed striking morphological differences in the pits produced by WT (Fig. 5A) and Y1R−/− osteoclasts (Fig. 5B). Quantitative analysis demonstrated that Y1R−/− resorptive pits have a significantly smaller top section surface area (Fig. 5C; p < 0.001). To analyse these differences in detail, resorption pits were divided into three categories accordingly with their surface area: (a) small (<500 μm2); b) medium (500–1000 μm2) and (c) large (>1000 μm2). The percentage of resorption pits calculated per each category revealed that Y1R−/− resorption pits are significantly small and medium sized, whereas WT pits are evenly distributed throughout all categories (Fig. 5D; p < 0.0001, Fisher’s exact test). In addition, based on a previously published scoring method by Caselli et al.23, the pit area index was estimated. Briefly, the number of pits of each category was multiplied by a factor: (a) small (x0.5), (b) medium (x1) and (c) large (x10). The sum of the three scores resulted in the pit area index. The Y1R−/− samples presented a pit area index of 21, in comparison to a much elevated pit area index of 86 for WT resorption pits.
Figure 5. Y1R deletion impairs osteoclast resorption activity.
The generation of 3D reconstructions of WT (A) and Y1R−/− (B) resorption pits revealed striking morphological differences. The analysis of these 3D reconstructions demonstrated that Y1R−/− resorption pits exhibit a decreased top section area (C), pit size (D), depth (E) and volume (F). Moreover, an increase on Y1R−/− pit depth is not accompanied by augmented top section area (G) or volume (H). Although the mean aspect ratio of Y1R−/− resorption pits was not different from WT (I), the frequency distribution of Y1R−/− resorption pits revealed a shift towards less circular pits than WT (J), which did not alter with increases in pit volume (K). Data is expressed as mean ± SEM. ***p < 0.001 different from WT.
Furthermore, 3D analysis demonstrated that Y1R−/− resorptive pits displayed a drastic reduction in volume (Fig. 5E) and in depth (Fig. 5F), when compared to WT resorption pits (p < 0.001). These marked results are consistent with the results obtained previously by SEM analysis (Fig. 3). Interestingly, by plotting the top section area versus pit depth, it is clear that the depth increase is not accompanied by an increase in the surface area in Y1R−/− resorptive pits, resulting in a shift towards the bottom (Fig. 5G). A similar distribution can be observed in volume versus depth scatter (Fig. 5H), where a homogenous distribution is only visible for WT resorptive pits.
As an attempt to measure the circularity of the resorption pit, the maximum length of the pit was divided into the maximum perpendicular size, allowing conveying the “aspect ratio” of the resorption pits. An aspect ratio of 1 corresponds to an approximately circular section area. As shown in Fig. 5I,J, although there were no significant differences in resorption pits aspect ratio for both genotypes, it is clear that Y1R−/− resorption pits are distributed far from the 1 value, in opposition to WT resorption pits. Moreover, increases in Y1R−/− resorption pit volume are not associated with a circular aspect ratio (Fig. 5K). Together, these results suggest that osteoclast-resorbing capacity is impaired in Y1R−/− mice.
To confirm that the inhibitory effects in osteoclastic resorption activity are Y1R-specific, osteoclast precursors were cultured in dentine substrate discs in the presence of increasing doses of a highly selective Y1R antagonist BIBP 3226 (0, 60, 1000 nM). Backscattered electron SEM analysis demonstrated that both doses of BIBP 3226 inhibit the formation of resorption pits, when compared to untreated osteoclasts (Supplementary Information Fig. S2). The resorption in 60 nM BIBP 3226-treated dentine discs appears to be more evenly distributed throughout the dentine surface but at a shallow depth, while in 1000 nM BIBP 3226-treated dentine discs suffered resorption within a smaller area, although resorption pits appear wider than at the lowest dose (Fig. S2). EDS spectra analysis comparing the dentine surface and pit surface confirmed that the peaks of phosphate and calcium remained reasonably unchanged at both treatment-conditions, when compared to untreated-dentine discs (Fig. S2).
Furthermore, resorption pit reconstructions revealed that BIBP 3226-treated dentine discs present a higher percentage of smaller resorption pits (p < 0.0001, Fisher’s exact test), regardless the concentration tested. Top section area, volume and depth (Fig. S2) of the resorption pits were also significantly diminished upon treatment. These results demonstrate that the Y1R antagonism recapitulates the effects of Y1R deletion in osteoclastic resorption activity, which suggests that the decrease in bone matrix resorption is Y1R-dependent.
Discussion
It is known that Y1R−/− mice exhibit a high-bone mass phenotype7, mainly due to elevated osteoblast activity8,12. Herein we demonstrate that the lack of Y1R promotes the formation of larger TRAP-positive multinucleated osteoclasts. Interestingly, these features were associated with diminished resorbing capacity, which was further confirmed by antagonizing Y1Rs using a highly selective antagonist BIBP 3226. Overall, these results suggest that the increase in bone mass observed in Y1R−/− mice resulted from a deficiency on resorbing activity allied to augmented osteoblast activity.
Osteoclast differentiation and maturation have long been demonstrated to be regulated by RANKL/RANK/OPG signalling pathway24. RANKL stimulation leads to the formation and fusion of TRAP-positive MNCs25. NPY signalling pathway has been demonstrated to inhibit RANKL expression by MC3T3-E1 cells and osteoblast-derived bone marrow stromal cells11. Moreover, NPY has also been shown to inhibit RANKL isoprenaline-induced osteoclastogenesis, possibly through Y1R signaling26. In this study, we show that the lack of Y1R results in increased RANKL expression and RANKL/OPG ratio by osteoblasts. Therefore, we hypothesize that the presence of RANKL boosts the formation of larger multinucleated osteoclasts in Y1R−/− cultures.
TRAcP5b is an acidic phosphatase highly expressed by the osteoclasts that is crucial for bone resorption. TRAcP5b is released into the resorptive-sealing zone and is partially responsible for bone demineralization process. The deletion of TRAP resulted in bone resorption impairment in mice27. Thus, TRAcP5b down-regulation can explain the observed reduction on bone resorbing activity in Y1R−/− cultures. Furthermore, other study have also reported a correlation between osteoclast size and TRAP activity, where giant osteoclast cells showed decreased TRAP activity28, which is also consistent with our results.
The fusion of osteoclast precursors was also exacerbated in Y1R−/− cultures, as seen by increased number of nuclei and surface area. Among the known osteoclast fusion markers, Y1R−/− osteoclasts were shown to express high mRNA levels of MCP-1. Previous studies have demonstrated that the secretion of MCP-1 is significantly elevated in activated Y1R−/− intraperitoneal macrophages in vitro, and it seems to be specific to Y1R signalling pathway14, which is in agreement with our data since both macrophages and osteoclasts derived from myeloid cells in the hematopoietic niche1. Moreover, MCP-1 is a chemotactic factor expressed by mature osteoclasts shown to promote osteoclast formation and fusion through cell-to-cell contact, under the control of RANKL signaling18,29,30. It is known that the exogenous treatment with MCP-1 in the presence of RANKL induces an increase in TRAP-positive MNCs formation18. Furthermore, the formation of multinucleated osteoclasts was significantly inhibited in MCP-1 knockout mice29. Thus, possibly the increase in TRAP-positive MNCs and osteoclast size in cells derived from Y1R−/− mice might be due to an upregulation of MCP-1 expression through RANKL signalling. Overall, these data indicates that Y1R−/− mice display increased formation of TRAP-MNCs possibly regulated by RANKL-signalling, and enhanced osteoclast fusion and surface area under the control of MCP-1. Nevertheless, future investigation is warranted to unravel the signalling pathways linking RANKL, MCP-1 and Y1R in osteoclast-mediated formation and fusion.
The RANKL expression is an important determinant of elevated bone resorption that is often associated with bone loss and osteoporosis16. In contrast, despite an increase in RANKL expression and an elevated number of TRAP-positive MNCs in Y1R−/− cultures, Y1R−/− mice still exhibit a high-bone mass phenotype. In point of fact, the pieces of evidence presented here suggest that the Y1R deficiency led to the formation of giant multinucleated osteoclasts with impaired resorbing capacity, possibly due to the lack of essential factors required for the normal function of bone-resorbing osteoclasts, such as CTSK and MMPs, as described previously18,21.
CTSK is a crucial enzyme in bone matrix resorption. The CTSK-deficiency has been associated with impaired osteoclastic bone matrix resorption31, resulting in the development of abnormal bone formation and osteopetrosis, which corroborate the observation that CTSK is downregulated in Y1R−/− osteoclasts. Furthermore, the expression of MMP-9, a proteinase involved in collagen matrix degradation and bone resorption21, was also shown to be downregulated in Y1R−/− cultures. Together, these observations confirm the formation of non-resorbing large multinucleated osteoclasts when Y1R signalling is disrupted.
Exploratory studies have implicated MMP-9 in the regulation of endochondral ossification using stabilized and non-stabilized fracture models32,33,34. MMP-9 was shown to be expressed throughout all phases of fracture repair, and its deficiency led to anomalous fracture repair32. Moreover, MMP-9−/− mice displayed increased inflammatory populations at the fracture site and delayed hypertrophic cartilage turnover and matrix remodeling33. Furthermore, the broad inhibition of MMPs resulted in delayed endochondral ossification and fracture union in rats35. In the light of our findings, we speculate that the delay in hypertrophic cartilage removal and fracture union previously observed in Y1R−/− mice36 might have occurred due to decreased MMP-9 expression and impaired osteoclast resorptive activity. Of note, independently of the facts presented, the endochondral growth and skeletal development appears to be uncompromised in Y1R−/− mice7, which in turn suggests that albeit the resorption capacity has been affected in the absence of Y1R signalling, Y1R−/− osteoclasts still sustain a residual resorptive activity.
Although osteoclast multinucleation has been commonly accepted to improve the resorption efficiency of mature osteoclasts37, it was previously observed that the volume resorbed per nucleus tend to decrease with the increase in nuclei number per osteoclast38. This was further explained by the fact that only a certain number of nuclei within multinucleated osteoclasts are transcriptionally active39, which support our observations that Y1R−/− multinucleated osteoclasts exhibit decreased bone-resorbing activity regardless of the increased number of nuclei present.
Nevertheless, the intracellular signal transduction mechanisms triggered by Y1R deletion leading to the occurrence of these events remain to be uncovered. Y1R belongs to the family of G-protein coupled receptors (GPCRs). Knowledge gathered from previous studies demonstrated that Y1R is coupled to inhibitory heterotrimeric GTP-binding protein (Gi/Go)9. Its activation triggers a number of intracellular signal transduction cascades resulting in the: a) inhibition of adenylyl cyclase and cAMP; b) activation of phospholipase C and protein kinase C; c) elevation of cytosolic Ca2+; and d) activation of MAPK signalling pathway9. These transduction cascades are also known to be involved in osteoclastogenesis signalling cascades and in the regulation of MMPs and CTSK mRNA expression40,41, suggesting Y1R and osteoclastic signalling pathways (e.g. RANKL/RANK signalling) share common intracellular transduction pathways. Thus, we hypothesize that the disruption of Y1R intracellular signal cascade occurring in Y1R−/− mice affected the pathways regulating the formation of osteoclasts and its resorptive activity. This hypothesis should be further explored in future research.
Recent studies have recognized that the geometry of resorptive cavities produced by osteoclasts (pits versus trenches) affect the structure, determining bone quality and its mechanical properties, such as bone stiffness and trabecular microarchitecture42,43. To date, the role of Y1R signalling deletion in bone quality and its impact on bone mechanical properties is still unknown. Future work should be undertaken to analyse the geometry of the resorption cavities produced by Y1R−/− osteoclasts and evaluate the bone mechanical properties of Y1R−/− mice.
In conclusion, our data demonstrates that Y1R plays an important role in osteoclast formation and activity, prominently in osteoclast resorptive capacity. The Y1R deficiency led to the formation of larger multinucleated cells with diminished resorbing capacity, resulting in a substantial reduction in resorption pits formation and eroded area. Taking into consideration that Y1R−/− mice exhibit increased bone formation and in the light of the data presented we propose the use of Y1R antagonists as a clinically favourable therapeutic strategy for the treatment of osteoclast-related disorders, where bone resorption is chronically altered.
Methods
Animals
All research and animal care procedures were conducted following protocols approved by the Ethics Committee of the Portuguese Official Authority on Animal Welfare and Experimentation (DGAV). Mice were housed at 22 °C with a 12 h light/dark cycle with ad libitum access to water and food. All experiments were performed using 6–8 weeks-old male WT and Y1R−/− mice. The generation of Y1R−/− mice has been described in detail previously7,44. Y1R−/− mice were backcrossed to a C57BL/6 background for at least five generations. Genotyping was performed using a PCR-based method to detect WT and knockout alleles7.
Osteoclast cultures
Bone marrow cells were isolated from tibiae and femur (WT and Y1R−/− mice) by flushing the bone marrow with α-MEM (Gibco, Thermo Fisher Scientific, USA) containing 10% (v/v) heat inactivated (30 min at 56 °C) foetal bovine serum (FBS, Gibco) and 1% (v/v) penicillin/streptomycin (P/S, Gibco)11. To generate primary osteoclast precursors, cell suspension was plated in the presence of 30 ng/mL M-CSF (PeproTech, USA) for three days. Adherent cells were then detached with 50 mM EDTA for 20 min at 37 °C and seeded in the presence of 30 ng/mL M-CSF and 100 ng/mL RANKL (PeproTech) at a density of 3 × 105 cells/cm2. Cells were maintained at 37 °C in a humidified atmosphere of 5% CO2 for 4–5 days. To assess osteoclast resorptive capacity, osteoclast precursors were seeded on top of commercially available dentine substrate discs (5-mm diameter and 0.3-mm thick; OsteoSite Dentin Discs, Immuno Diagnostic Systems, UK) and allowed to generate resorption pits. At the end of the experiment, conditioned media were collected and stored at −80 °C before undergoing processing. Dentine substrates were prepared for electron microscopy and 3D quantitative analysis. All conditions were established in triplicates and repeated in 3 independent experiments.
Quantitative CTX-I analysis
The levels of CTX-I in conditioned medium were quantified by enzymeimmunoassay (EIA) according to the manufacturer’s protocol (RatLapsTM EIA CTX-I; Immunodiagnostic Systems, Denmark).
TRAP staining
TRAP staining was performed using an Acid phosphatase, Leukocyte (TRAP) kit (Sigma-Aldrich) according to manufacturer’s instructions. Images were acquired using a stereomicroscope (SZX10, Olympus, Center Valley, PA, USA) coupled to a digital camera (DP21, Olympus). TRAP-positive multinucleated cells (MNCs) with more than 3 nuclei were counted.
F-actin staining
Cells were incubated with Alexa Fluor® 488 phalloidin (1:100; Molecular Probes) in 1% BSA for 20 min at RT to label the cytoskeletal filamentous actin (F-actin). Nuclei were stained with DAPI. Six representative images were obtained from each triplicate using an inverted fluorescence microscope (Carl Zeiss, Germany) coupled to a camera AxioCam HRc. The number of nuclei per cell was quantified. Osteoclast area and maximum length measurements were performed using the “measure outline” tool of the AxioVision SE64 Rel. 4.8 software (Carl Zeiss).
SEM analysis
Dentine samples were fixed with 2.5% (v/v) glutaraldehyde in 0.1 M sodium cacodylate solution for 30 min and then washed with cacodylate buffer. Dentine discs were dehydrated in serially diluted ethanol solutions (50, 60, 70, 80, 90 and 99% v/v) for 10 min each dilution, and stored in absolute ethanol. Each sample was then critical point dried, sputtered-coated with gold and examined by SEM. Photomicrographs were obtained and the chemical composition of the dentine surfaces was evaluated by EDS analysis.
Quantitative analysis of 3D resorption pits
Cultured dentine discs were washed with PBS and immersed in a 2 mM EDTA solution for 10 min at 37 °C to remove adherent cells. Dentine mineralized matrices were then stained with 10 μg/mL calcein AM (Molecular Probes, Life Technologies, USA) for 30 min, washed and allowed to air dry19. Images were obtained in a TCS SP2 spectral confocal and multiphoton system (Leica) at a resolution of 1024 × 1024 pixels with a 40x oil objective. Samples were exposed to a 488 nm radiation through a pinhole setting of 1 airy. Images of resorption pits acquired were averaged twice, and stacked images with a voxel size of 0.3662 × 0.3662 × 0.2849 μm were generated. The custom made program to perform the semi-automated 3D reconstruction of resorption pits was written using MATLAB 2013a (MathWorks, USA) software. As depicted in Fig. 6, stacked images were loaded into the program and the resorption pit outline was manually outlined in every stack. A mask containing every outline was then generated and used to reconstruct the resorption pit. From this 3D reconstruction it was possible to calculate the resorption pit volume, depth, top section area and aspect ratio. Volume was calculated by multiplying the number of pixels contained in the outlines by the voxel size. Depth was obtained by calculating the difference between the maximum layer index and the minimum layer index and multiplying by the step size (0.2849 μm). Top section area was calculated by multiplying the pixels in the first layer by the pixel area. Finally, the aspect ratio was defined as the ratio between the maximum length and the perpendicular maximum width of the pit. The complete set points associated with the resorption pit outlines were used to calculate a 3D mesh representing the pit surface (Fig. 6). Software details can be visualized and downloaded at computools.i3s.up.pt/BonePit/.
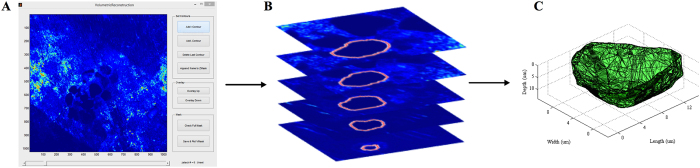
Figure 6. BonePit program – a computational tool for morphometric analysis of bone matrix resorption.
Stacked images of calcein-stained dentine substrates are loaded into BonePit algorithm (A), developed in MATLAB. The program applies a Gaussian filter to reduce noise and changes the colour representation to identify more easily pit regions. The contours of a single pit were then manually drawn in each stack and compiled into a mask (B). Finally, every point in the mask is connected to the neighbouring points creating a 3D reconstruction mesh of the resorption pit (C).
Gelatin zymography
Conditioned medium was replaced by a serum-free medium 24 h prior to experiment endpoint. The media were loaded into gelatin–SDS polyacrylamide gels (Mini-Protean Tetra Cell system, Bio-Rad), as described previously45. Following electrophoresis, gels were stained with 0.1% w/v Coomassie Blue solution (Sigma-Aldrich). Clear bands of proteolytic degradation in contrast to a blue background of the gelatin substrate represent the activity of MMPs. Band densities were quantified by densitometric analysis using ImageJ software.
qRT-PCR analysis
Total RNA was extracted using the Direct-zol™ RNA miniPrep according to the manufacturer’s protocol (Zymo Research, USA). RNA final concentration and purity (OD260/280) was determined using a NanoDrop 2000 instrument (NanoDrop Technologies, Thermo Fisher Scientific, Wilmington, Delaware, USA; NanoDrop 3.0.1 software). RNA was reverse transcribed into cDNA using the Superscript II reverse transcriptase kit (Invitrogen, Life Technology, Paisley, UK), according to the manufacturer’s protocol. qRT-PCR experiments were run using an iCycler iQ5 PCR thermal cycler (Bio-Rad Laboratories, Hercules, CA, USA) and analysed with the iCycler IQTM software (Bio-Rad; version 2.1). The specific primers used are described in Table 1. Target gene expression was quantified using the cycle threshold (Ct) values and relative mRNA expression levels were calculated as follows: 2^(Ct reference gene - Ct target gene). Mouse glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was used as a reference gene. Both target and reference genes were amplified with efficiencies between 100 ± 5%.
Table 1. Pairs of primers used in qRT-PCR analysis.
| Gene | Forward Primer (5′- > 3′) | Reverse Primer (5′- > 3′) | Product Length (base pairs) |
|---|---|---|---|
| ATP6V0D2 | TTCTTGAGTTTGAGGCCGAC | CAGCTTGAGCTAACAACCGC | 144 |
| CTSK | ATATGTGGGCCAGGATGAAAGTT | TCGTTCCCCACAGGAATCTCT | 90 |
| CD47 | CGATGCCATGGTGGGAAACT | TCAGTGTTGAAGGCCGTGC | 99 |
| CD9 | GCTGGGATTGTTCTTCGGGT | GCTTTGAGTGTTTCCCGCTG | 171 |
| DC-STAMP | AAGCGGAACTTAGACACAGGG | CAGCTAGGGCTTCGTGGAAA | 101 |
| GADPH | GCCTTCCGTGTTCCTACC | AGAGTGGGAGTTGCTGTTG | 183 |
| MCP-1 | AGCCAACTCTCACTGAAGCC | GCGTTAACTGCATCTGGCTG | 131 |
| MMP-9 | CGACTTTTGTGGTCTTCCCC | TAGCGGTACAAGTATGCCTCTG | 83 |
| OPG | GTGGAATAGATGTCACCCTGTGT | TTTGGTCCCAGGCAAACTGT | 110 |
| RANKL | CCCATCGGGTTCCCATAAAGT | AGCAAATGTTGGCGTACAGG | 114 |
| TRAcP5b | CGACCATTGTTAGCCACATACG | TCGTCCTGAAGATACTGCAGGTT | 77 |
| Y1R | CTCGCTGGTTCTCATCGCTGTGGAACGG | GCGAATGTATATCTTGAAGTAG | 325 |
All primers used were located on two different exons to ensure that only properly spliced mRNA and not genomic DNA contaminants was amplified.
Statistical analysis
Data are expressed as mean ± standard error of the mean (SEM). Normal distribution of the data was assessed through Shapiro-Wilk test. Statistical differences between groups were compared using a two-way ANOVA and post hoc comparisons were performed with an independent samples t-test. When normal distribution was not verified, the non-parametric Kruskal-Wallis test followed by the Mann-Whitney U-test to assess statistical significance was performed. Statistical analysis was carried out with SPSS for Windows (version 20; SPSS Inc., Chicago, IL, USA) and statistically significance was accepted when p < 0.05.
Additional Information
How to cite this article: Sousa, D. M. et al. Ablation of Y1 receptor impairs osteoclast bone-resorbing activity. Sci. Rep. 6, 33470; doi: 10.1038/srep33470 (2016).
Supplementary Material
Acknowledgments
This article is a result of the project NORTE-01-0145-FEDER-000012, supported by Norte Portugal Regional Operational Programme (NORTE 2020), under the PORTUGAL 2020 Partnership Agreement, through the European Regional Development Fund (ERDF). The authors would like to acknowledge Daniela Silva from Centro de Materiais da Universidade do Porto (CEMUP, REEQ/1062/CTM/2005 from FCT) for helping with SEM analysis.
Footnotes
Author Contributions D.M.S. and M.L. planned the experiment design. D.M.S., F.C. and D.I.S. conducted cell culture experiments. D.M.S., F.C., L.L., E.N., C.J.A. and I.S.A. collected and analysed data. F.C. and P.A. performed the 3D analysis. H.H. provided the animal colony. All authors revised the manuscript.
References
- Boyce B. F. Advances in the Regulation of Osteoclasts and Osteoclast Functions. J. Dent. Res. 92, 860–867 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims N. A. & Martin T. J. Coupling the activities of bone formation and resorption: a multitude of signals within the basic multicellular unit. BoneKEy Rep. 3, 481 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce B. F., Rosenberg E., de Papp A. E. & Duong L. T. The osteoclast, bone remodelling and treatment of metabolic bone disease. Eur. J. Clin. Invest. 42, 1332–1341 (2012). [DOI] [PubMed] [Google Scholar]
- Käkönen S.-M. et al. Transforming Growth Factor-β Stimulates Parathyroid Hormone-related Protein and Osteolytic Metastases via Smad and Mitogen-activated Protein Kinase Signaling Pathways. J Biol. Chem. 277, 24571–24578 (2002). [DOI] [PubMed] [Google Scholar]
- Gravallese E. M. et al. Identification of cell types responsible for bone resorption in rheumatoid arthritis and juvenile rheumatoid arthritis. Am. J. Pathol. 152, 943–951 (1998). [PMC free article] [PubMed] [Google Scholar]
- Elefteriou F. Regulation of bone remodeling by the central and peripheral nervous system. Arch. Biochem. Biophys. 473, 231–236 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldock P. A. et al. Novel Role of Y1 Receptors in the Coordinated Regulation of Bone and Energy Homeostasis. J. Biol. Chem. 282, 19092–19102 (2007). [DOI] [PubMed] [Google Scholar]
- Lee N. J. et al. Osteoblast specific Y1 receptor deletion enhances bone mass. Bone 48, 461–467 (2011). [DOI] [PubMed] [Google Scholar]
- Sousa D. M., Herzog H. & Lamghari M. NPY signalling pathway in bone homeostasis: Y1 receptor as a potential drug target. Curr. Drug Targets 10, 9–19 (2009). [DOI] [PubMed] [Google Scholar]
- Sousa D. M. et al. Neuropeptide Y Y1 receptor antagonism increases bone mass in mice. Bone 51, 8–16 (2012). [DOI] [PubMed] [Google Scholar]
- Teixeira L. et al. NPY revealed as a critical modulator of osteoblast function in vitro: new insights into the role of Y1 and Y2 receptors. J. Cell. Biochem. 107, 908–916 (2009). [DOI] [PubMed] [Google Scholar]
- Lee N. J. et al. Critical role for Y1 receptors in mesenchymal progenitor cell differentiation and osteoblast activity. J. Bone Miner. Res. 25, 1736–1747 (2010). [DOI] [PubMed] [Google Scholar]
- Wheway J. et al. A fundamental bimodal role for neuropeptide Y1 receptor in the immune system. J. Exp. Med. 202, 1527–1538 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macia L. et al. Neuropeptide Y1 receptor in immune cells regulates inflammation and insulin resistance associated with diet-induced obesity. Diabetes 61, 3228–3238 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeshita S., Kaji K. & Kudo A. Identification and characterization of the new osteoclast progenitor with macrophage phenotypes being able to differentiate into mature osteoclasts. J. Bone Miner. Res. 15, 1477–1488 (2000). [DOI] [PubMed] [Google Scholar]
- Kim H. et al. Selective inhibition of RANK blocks osteoclast maturation and function and prevents bone loss in mice. J. Clin. Invest. 119, 813–825 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing L., Xiu Y. & Boyce B. F. Osteoclast fusion and regulation by RANKL-dependent and independent factors. World J. Orthop. 3, 212–222 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M. S., Day C. J. & Morrison N. A. MCP-1 is induced by receptor activator of nuclear factor-{kappa}B ligand, promotes human osteoclast fusion, and rescues granulocyte macrophage colony-stimulating factor suppression of osteoclast formation. J. Biol. Chem. 280, 16163–16169 (2005). [DOI] [PubMed] [Google Scholar]
- Rumpler M. et al. Osteoclasts on bone and dentin in vitro: mechanism of trail formation and comparison of resorption behavior. Calcif. Tissue Int. 93, 526–539 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider R. In Surface and Thin Film Analysis: Principles, Instrumentation, Applications (eds Buhert H. et al.) Ch. 2.3, 293–310 (Wiley-VCH Verlag GmbH & Co. KGaA, 2011). [Google Scholar]
- Nyman J. S. et al. Differential effects between the loss of MMP-2 and MMP-9 on structural and tissue-level properties of bone. J. Bone Miner. Res. 26, 1252–1260 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morko J. et al. Overexpression of cathepsin K accelerates the resorption cycle and osteoblast differentiation in vitro. Bone 44, 717–728 (2009). [DOI] [PubMed] [Google Scholar]
- Caselli G. et al. Tartronates: a new generation of drugs affecting bone metabolism. J. Bone Miner. Res. 12, 972–981 (1997). [DOI] [PubMed] [Google Scholar]
- Yasuda H. et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc. Natl. Acad. Sci. USA 95, 3597–3602 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamashita Y. et al. RANKL pretreatment plays an important role in the differentiation of pit-forming osteoclasts induced by TNF-alpha on murine bone marrow macrophages. Arch. Oral Biol. 60, 1273–1282 (2015). [DOI] [PubMed] [Google Scholar]
- Amano S., Arai M., Goto S. & Togari A. Inhibitory effect of NPY on isoprenaline-induced osteoclastogenesis in mouse bone marrow cells. Biochim. Biophys. Acta 1770, 966–973 (2007). [DOI] [PubMed] [Google Scholar]
- Hayman A. R. & Cox T. M. Tartrate-resistant acid phosphatase knockout mice. J. Bone Miner. Res. 18, 1905–1907 (2003). [DOI] [PubMed] [Google Scholar]
- Metze K., Ciplea A. G., Hettwer H. & Barckhaus R. H. Size dependent enzyme activities of multinucleated (osteoclastic) giant cells in bone tumors. Pathol. Res. Pract. 182, 214–221 (1987). [DOI] [PubMed] [Google Scholar]
- Miyamoto K. et al. MCP-1 expressed by osteoclasts stimulates osteoclastogenesis in an autocrine/paracrine manner. Biochem. Biophys. Res. Commun. 383, 373–377 (2009). [DOI] [PubMed] [Google Scholar]
- Khan U. A., Hashimi S. M., Bakr M. M., Forwood M. R. & Morrison N. A. CCL2 and CCR2 are Essential for the Formation of Osteoclasts and Foreign Body Giant Cells. J. Cell. Biochem. (2015). [DOI] [PubMed] [Google Scholar]
- Saftig P. et al. Impaired osteoclastic bone resorption leads to osteopetrosis in cathepsin-K-deficient mice. Proc. Natl. Acad. Sci. USA 95, 13453–13458 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colnot C., Thompson Z., Miclau T., Werb Z. & Helms J. A. Altered fracture repair in the absence of MMP9. Development 130, 4123–4133 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X. et al. MMP9 regulates the cellular response to inflammation after skeletal injury. Bone 52, 111–119 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega N., Wang K., Ferrara N., Werb Z. & Vu T. H. Complementary interplay between matrix metalloproteinase-9, vascular endothelial growth factor and osteoclast function drives endochondral bone formation. Dis. Model. Mech. 3, 224–235 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald M. M. et al. Matrix metalloproteinase-driven endochondral fracture union proceeds independently of osteoclast activity. J. Bone Miner. Res. 28, 1550–1560 (2013). [DOI] [PubMed] [Google Scholar]
- Sousa D. M. et al. Neuropeptide Y modulates fracture healing through Y1 receptor signaling. J. Orthop. Res. 31, 1570–1578 (2013). [DOI] [PubMed] [Google Scholar]
- Boissy P., Saltel F., Bouniol C., Jurdic P. & Machuca-Gayet I. Transcriptional activity of nuclei in multinucleated osteoclasts and its modulation by calcitonin. Endocrin. 143, 1913–1921 (2002). [DOI] [PubMed] [Google Scholar]
- Piper K., Boyde A. & Jones S. J. The relationship between the number of nuclei of an osteoclast and its resorptive capability in vitro. Anat. Embryol. (Berl) 186, 291–299 (1992). [DOI] [PubMed] [Google Scholar]
- Youn M. Y., Takada I., Imai Y., Yasuda H. & Kato S. Transcriptionally active nuclei are selective in mature multinucleated osteoclasts. Genes Cells 15, 1025–1035 (2010). [DOI] [PubMed] [Google Scholar]
- Long C. L. & Humphrey M. B. Osteoimmunology: the expanding role of immunoreceptors in osteoclasts and bone remodeling. Bonekey Rep. 1 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takayanagi H. Osteoimmunology: shared mechanisms and crosstalk between the immune and bone systems. Nat. Rev. Immunol. 7, 292–304 (2007). [DOI] [PubMed] [Google Scholar]
- Merrild D. M. et al. Pit- and trench-forming osteoclasts: a distinction that matters. Bone Res. 3, 15032 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderoost J., Soe K., Merrild D. M., Delaisse J. M. & van Lenthe G. H. Glucocorticoid-induced changes in the geometry of osteoclast resorption cavities affect trabecular bone stiffness. Calcif. Tissue Int. 92, 240–250 (2013). [DOI] [PubMed] [Google Scholar]
- Howell O. W. et al. Neuropeptide Y is neuroproliferative for post-natal hippocampal precursor cells. J. Neurochem. 86, 646–659 (2003). [DOI] [PubMed] [Google Scholar]
- Fonseca K. B., Bidarra S. J., Oliveira M. J., Granja P. L. & Barrias C. C. Molecularly designed alginate hydrogels susceptible to local proteolysis as three-dimensional cellular microenvironments. Acta Biomater. 7, 1674–1682 (2011). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.