Abstract
Significance: Wounds sustained in a combat trauma often result in a composite tissue loss. Combat injuries, due to high energy transfer to tissues, lead to trauma at multiple anatomical sites. An early wound cover is associated with lower rate of infections and a faster wound healing. The concept of negative pressure wound therapy (NPWT) in the management of combat-related wounds has evolved from the civilian trauma and the wounds from nontraumatic etiologies.
Recent Advances: Encouraged by the results of NPWT in noncombat-related wounds, the military surgeons during Operation Iraqi Freedom and Operation Enduring Freedom used this novel method in a large percentage of combat wounds, with gratifying results. The mechanism of NPWT in wound healing is multifactorial and often complex reconstructive procedure can be avoided in a combat trauma setting.
Critical Issues: Wounds sustained in military trauma are heavily contaminated with dirt, patient clothing, and frequently associated with extensive soft tissue loss and osseous destruction. Delay in evacuation during an ongoing conflict carries the risk of systemic infection. Early debridement is indicated followed by delayed closure of wounds. NPWT helps to provide temporary wound cover during the interim period of debridement and wound closure.
Future Directions: Future area of research in combat wounds is related to abdominal trauma with loss of abdominal wall. The concept of negative pressure incisional management system in patients with a high risk of wound breakdown following surgery is under review, and may be of relevance in combat wounds.
Keywords: : combat wounds, negative pressure wound therapy, wound debridement, delayed wound closure, soft tissue reconstruction

Sanjay Maurya, MS, MCh
Scope and Significance
This review article discusses the characteristics of combat wounds and their general principles of management. It addresses the role of negative pressure wound therapy (NPWT) in managing such wounds with an emphasis on its mechanism of action. We also share our experience with NPWT in the management of combat wounds, and review certain critical aspects in this form of therapy.
Translational Relevance
The NPWT was introduced almost 20 years back. Much of its use was inferred in the civilian trauma and other nontraumatic wounds. This review describes how NPWT has evolved in the management of combat wounds and established as a key modality in combat trauma. Military surgeons have accepted this novel method of wound management and further evaluation in treating wounds at various anatomical sites will help in improving the care of wounded soldiers.
Clinical Relevance
This review describes the characteristics of combat wounds and principles of their management. It will guide the readers about the role of NPWT in the management of combat wounds. The literature is reviewed regarding its indications, mechanism of action, and advantages of NPWT. It will help the military surgeons to formulate guidelines in the management of combat wounds.
Background
Combat wounds pose a challenge to a military trauma surgeon. The wounds are sustained due to gunshots, grenade blasts, landmines, improvised explosive devices (IEDs), and bombs. These wounds are heavily contaminated with dust, soil, the patient's clothing, and other foreign bodies, and characterized by extensive loss of soft tissues and bony materials. Due to high energy transfer, multiple tissue planes are opened leading to contamination beyond the zone of trauma. Involvement of multiple anatomical sites, make these individuals critical, requiring urgent resuscitation and life support. In a war scenario, an early wound care may be delayed due to late evacuation to a forward surgical center.1
Traditionally these wounds have been managed with wound irrigation, debridement, and a delayed closure. The disadvantages of this form of management were well recognized. The benefits of NPWT in combat trauma have been reported by various authors.2,3 The popularity of NPWT can be gauged by the fact that during Operation Enduring Freedom (OEF) in March 2003, about 46% of wounds were managed with NPWT and in September 2003 its use had increased to over 90% of admitted wounds.4 Further technical refinements have validated its use during air transport, allowing casualties to receive continuous NPWT during air evacuation, from forward surgical center to a tertiary care center.5
Discussion
Although the use of negative pressure for medicinal purpose was described in 600 BC, it was only in 1997, when Morykwas et al. reported their results in animal studies.6 Using pig model, wound was covered by open cell foam and sealed by adhesive tape. Subatmospheric pressure of 125 mm Hg was applied to the covered foam. They found an increase in blood flow by fourfold with a negative pressure of 125 mm Hg and a significant increase in granulation tissue formation. They also reported a decrease in tissue bacterial counts and an increase in random flap survival by 21% as compared to controls. They concluded that application of controlled subatmospheric pressure creates an atmosphere conducive to wound healing. Subsequently numerous authors have described their experience with NPWT in noncombat wounds.7–10
The use of vacuum wound closure systems in war wounds was reported for the first time in 2004 by Burris et al.11 Their handbook on Emergency War Surgery describes its role in combat wounds with an improved and accelerated healing. The use of NPWT was widely reported during Operation Iraqi Freedom and OEF.3,5 It rapidly gained popularity among the military surgeons worldwide due to its versatility, ease of application, and varied indications in combat-related wounds. NPWT became a preferred method in combat trauma as compared to traditional methods, with saline-soaked dressings.4
Combat wound characteristics and wound ballistics
The tissue damage caused by a bullet is related to its kinetic energy transferred to the tissues, given by the formula of ½ mv2. High-velocity missile injuries produce extensive tissue damage due to a combination of shock waves and cavitation effect. The blast injuries due to explosive devices produce damage by various mechanisms. Primary blast injury is due to a high pressure generated by the blast effect. This can cause rupture of air-filled organs like tympanic membrane, lungs, and intestines. Secondary blast injury is caused by flying objects like splinters or other objects in the vicinity of blast. Tertiary blast injury is due to movement of the body from pressure generated by blast waves or due to fall of objects on the casualty. Quaternary blast injury is due to other factors like burns and chemical contamination.12 The injury caused by IEDs and antipersonnel mines can cause damage in multiple tissue planes with composite loss of tissues and amputations (Fig. 1). Certain factors make combat wounds different from those encountered in civilian practice—the high energy transfer to tissues, early wound contamination from dirt, soil, and the individual's own clothing, and a delay in evacuation to the forward surgical center for early wound debridement.
Figure 1.

Mine blast injury foot resulting in traumatic loss of foot. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Principles of combat wound management
The management of combat wounds aims to save life and limb. An aggressive management of these wounds reduces morbidity and mortality.
Wound debridement
It forms the basis of combat wound management. Contaminated nature of wounds call for timely debridement and wound irrigation preferably within 6 h of trauma. Early removal of devitalized tissue, foreign bodies, blood, debris, and dirt prevent local and systemic infection. Various authors have described the types of debridement.13 Both marginal and complete debridements are appropriate in combat wounds. However, Guthrie and Clasper recommend complete debridement in war wounds to optimize resources during war.14 High-pressure pulse lavage may be appropriate in civilian trauma, but is not recommended in combat-related injuries due to an increase in tissue damage and a heavy microbial contamination.15 Once the surgeon is satisfied with the debridement, the wound is then treated by NPWT system.
Further evaluation and definitive wound closure
Further evaluation and definitive closure should be planned at higher medical echelons. Ideally, combat wounds should be closed after 4–5 days of final debridement. This is associated with faster recovery and lower infection rates.16 However, with the experiences gained during Iraq conflict, wound reconstruction during the subacute period (7 days–3 months) has been reported with good outcomes.17
Indications of negative pressure therapy in combat wounds
Sorensen et al. reviewed the use of NPWT and published their results related to different treatment variables.18 The indications of NPWT are summarized below.
Temporary wound closure
NPWT provides an ideal interior milieu for wound management. It provides an airtight barrier which prevents contamination and allows moist wound healing. The NPWT can be started after first debridement and continued during casualty evacuation. It may be used after damage control surgery and temporary abdominal closure in abdominal trauma.3 Its use during casualty air evacuation decreases infection rates, reduces discomfort of dressing changes during transit, and helps in early wound closure.5,7
Wound preparation for final surgical closure
NPWT can be continued until a definitive reconstruction is undertaken or wound has healed by secondary intention. Use of NPWT is associated with reduction in size and depth of the wound and formation of healthy granulation tissue suitable for wound cover. Simpler reconstructive procedure can be undertaken instead of complex reconstructions that require more resources in terms of time, trained manpower, and infrastructure.
As an aid for successful graft take
Split-thickness skin graft (STSG) is one of the simpler ways to cover a wound. It is vital to achieve successful STSG take in combat wounds as it reduces morbidity and infective complications. NPWT when applied over STSG increases the graft take, reduces seroma formation, and allows an early mobilization.19,20
Adjunct therapy in combat wound reconstruction using dermal substitute
Large combat wounds with exposed bones and tendons that are not suitable for STSG can pose a challenge to the reconstructive surgeon. A major reconstructive procedure demands time, manpower, and resources that are often scanty during a period of mass casualty influx into a tertiary care military hospital. Helgeson et al. described the use of bioartificial dermal substitute in the management of complex combat-related soft tissue wounds in conjunction with NPWT. The matrix was covered with STSG within 3 weeks of avoiding complex flap coverage.21
Wound changes with NPWT and mechanism of action
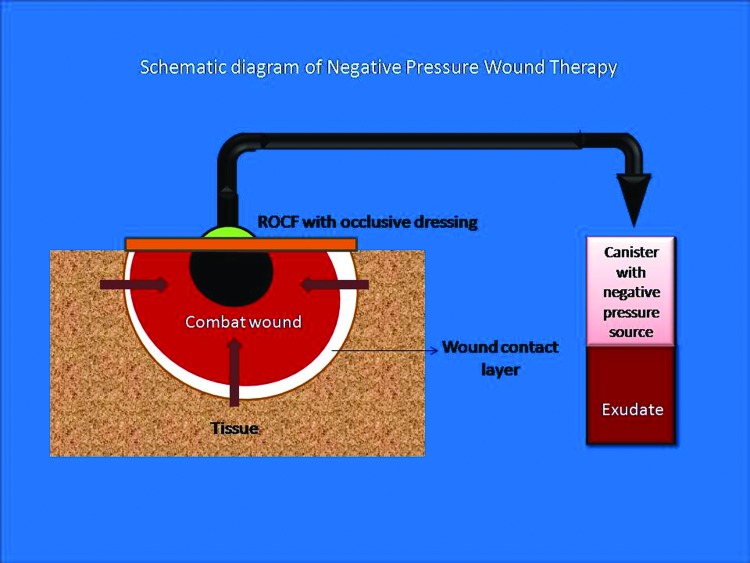
NPWT system consists of four major components: (1) Filler material or sponge commonly used as reticulated open cell foam (ROCF) placed directly over the wound, (2) barrier air-tight dressings to allow the system to transmit subatmospheric pressure, (3) a connecting tube, and (4) a vacuum device to generate subatmospheric pressure. An additional layer as wound contact layer (WCL) may be used at the interface between wound and the foam (Fig. 2). Large numbers of commercially available packs are available to cater for wounds of different sizes.
Figure 2.
Components of NPWT, which have been explained in the text. NPWT, negative pressure wound therapy; ROCF, reticulated open cell foam. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
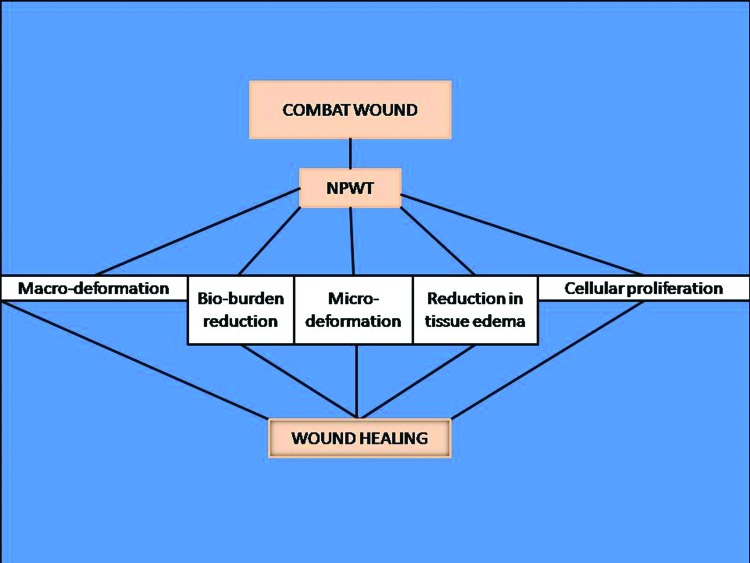
The wound healing associated with NPWT is multifactorial and is achieved by primary and secondary means (Fig. 3).
Figure 3.
Multifactorial mechanism of action of NPWT. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Wound contraction
Negative pressure of about 125 mm Hg applied over the sponge shrinks its size by 80%.22 This causes contraction of wound due to centripetal forces exerted on the wound, called the macrodeformation. The degree of macrodeformation depends upon the tissue type, tensile strength of surrounding tissue, and the degree of suction applied.23
Microdeformation
At the cellular level, the mechanical force generated by the negative pressure is transmitted to the individual cells through the extracellular matrix. This causes microdeformation of cytoskeleton, which is believed to stimulate cell proliferation by a process called mechanotransduction.22 These cellular changes lead to undulated wound surface induced by foam–tissue interface due to negative suction.24
Fluid removal
The negative pressure removes fluid from the depths of the wound in a closed system. This is beneficial for wound healing as it reduces local edema and hydrostatic pressure.25 Decrease in edema and hydrostatic pressure allows increase in blood flow to the wound, promoting healing.
Secondary mechanisms
These refer to mechanisms that promote wound healing due to cellular proliferation. Scherer et al. noted extended proliferated cell response in diabetic mouse model; they found an increased expression of Ki-67 a biological marker of cell proliferation.26 Increased fibroblasts, endothelial and epithelial cell migration are also seen with NPWT.27,28 This results in granulation tissue formation. The pressure around the periphery of the wound produces relative hypoxia, which stimulates angiogenesis due to increased expression of vascular endothelial growth factor (VEGF).29 The overall effect is reduction in size and depth of wound and formation of robust granulation tissue over exposed bone and other soft tissues. The microbial load in wound treated with NPWT is also believed to be reduced, which itself promotes wound healing.30 However, the bioburden reduction with NPWT remains a controversial topic and further studies are necessary to ascertain the effect of NPWT on bioburden.
Advantages of NPWT in combat-related wounds
Reduced frequency of dressing changes
Due to its ability to provide closed suction drainage and the fact that single dressings can be used for prolonged periods (72 h), saves manpower, time, and effort without compromising the safety. It also provides time to plan definitive management at a higher center. Penn-Barwell et al. noted that less frequent changes in NPWT dressings does not alter the infection rates in combat wounds.31
Reduction in wound infection rates
Leininger et al. reported their experience with NPWT in contaminated soft tissue injuries in Iraq. Despite high-energy soft tissue wounds, the infection rate were 0% with overall wound complication rate of 0%.2 This was attributed to early wound debridement and irrigation and reduced hospital stay facilitated by NPWT. In another study published by Peck et al. infection rate of only 4% was noted in extremity war wounds treated by NPWT.32
Casualty evacuation
Casualty transfer to a tertiary care hospital requires wound care during transit. Time to reach this apex care facility is paramount for a successful reconstruction and wound cover. Earlier reports of NPWT during air evacuation were associated with wound complications from failure of NPWT device. Fang et al. reported the feasibility of NPWT during intercontinental aeromedical evacuation of combat casualty with no increase in wound complications. Thirty patients with 41 combat wounds were air evacuated from Germany to continental United States (CONUS) with a portable NPWT system (VAC Freedom System; Kinetic Concepts Incorporated, San Antonio, TX). They did not observe failure of the system and reported no wound-related complications.33 Pollak et al. described the use of NPWT during aeromedical evacuation of casualties in blast-related injuries. Ninety-five percent of them had minor complications requiring redebridement. Only 2 of the 218 patients had features of wound sepsis which were managed with additional wound debridement and irrigation. Seven cases had in-flight device problems of which four could not be repaired. However, complications were not increased in this subset of patients. Authors considered the use of NPWT during aeromedical evacuation as safe and feasible.34
Variables in NPWT
The system of NPWT incorporates certain variables that can affect the clinical outcomes. A working knowledge of these variables can help a military surgeon in optimizing the use of NPWT.
Pressure settings
A negative pressure setting of 125 mm Hg for the NPWT was based upon its effect on granulation tissue formation in a porcein model.6 Later in 2001, Morykwas et al. reported their study in varying levels of subatmospheric pressure in experimental wounds in swine model. Wounds with negative pressure of 125 mm Hg had significant amount of granulation formation as compared to pressures of −25 and −500 mm Hg.35 Hence, a negative pressure of 125 mm Hg was adopted for the clinical settings although the studies to this effect are lacking in human subjects. However, in vivo studies on experimental models have suggested a range of −50 to −150 mm Hg as an effective therapeutic range of negative pressure.36,37
Intermittent versus continuous pressure
A typical continuous pressure NPWT consists of a set negative pressure (−125 mm Hg) at which the therapy is continued. The intermittent pressure therapy (IPT) consists of 5 min on and 2 min off cycle. Concept of IPT was introduced based on observations on animal models that granulation tissue formation was faster with IPT than with continuous therapy.6 This form of therapy is associated with pain and discomfort experienced by a patient at every cycle of negative pressure and spillage of body fluids in high exudative wounds during off periods. To overcome these disadvantages, the concept of variable pressure therapy (VPT) was introduced, which consists of a smooth transition between two extremes of set pressure, but never touching 0 mm Hg. Both IPT and VPT have better effect on granulation tissue formation than continuous pressure.38,39 VPT may be advantageous in terms of reduced pain and discomfort as compared to IPT.
Filler material
Two commonly used filler materials used in NPWT are polyurethane foam in the form of ROCF and antimicrobial gauze. Both have been found to be equally effective with regard to blood flow and wound contraction in smaller wounds.40,41 However, the pain experienced during removal of dressings was significantly less with gauze dressings as compared to foam dressings, which was due to lower ingrowth of tissues into gauze dressings.42 Therefore, choice of the filler material is based on individual wound characteristics and hence may be institutional protocol based. The foam may be beneficial in large deep wounds without significant contours like fasciotomy wounds in limbs which are amenable for direct wound closure after NPWT.43 However, the gauze is considered suitable for shallow irregular wounds or deep cavities due to ease of application and its better conforming nature.44
Dressing change frequency
Regular monitoring of wounds is necessary in NPWT. There are no fixed intervals for dressing and may vary from 2 to 4 days.45 This variation in dressing change is due to wound characteristics and degree of contamination. Shweiki et al. reported the safe interval for subsequent dressing change after initial dressing in acute contaminated wounds. They concluded that 1.7–4.1 days (2.9 mean±1 SD) interval as safe and effective for subsequent dressing change after initial placement.46
Indicators of successful NPWT
Successful NPWT is characterized by the change in color and amount of exudates. The exudates volume should gradually reduce with its color change from bloody to serosanguineous. The wound appearance changes to red as the granulation tissue appears on the wound. A velvety appearance of the wound indicates ingrowth of granulation into the filler material. The wound size should reduce serially with successful NPWT and new epithelial growth may be visible at the wound edge. Failure to observe these signs may call for introspection of NPWT.
Clinical use and protocols based on NPWT in managing combat wounds
We started using NPWT in combat wounds based on various reports published in literature.3,4 Casualties with gunshot wounds and mine blast injuries were managed with NPWT followed by delayed soft tissue cover. Patients were transferred from forward surgical center to a tertiary care center where advanced facilities of combat casualty care were available. Since the time for air evacuation was short, no NPWT was applied during aeromedical evacuation. On arrival to our center, all life-threatening conditions were first treated and then the patients were subjected to relook of wounds. Debridement of wound was undertaken if necessary and NPWT system was applied with a subatmospheric pressure of 125 mm Hg. Second-look surgery was undertaken only if wound revealed signs of contamination and an ongoing necrosis especially in blast injuries. Foam was placed on the wounds with a marginal overlap and sealed with an adhesive drape. Negative pressure of 125 mm Hg was used in the system. Appropriate delayed reconstruction was undertaken to cover the wound (Figs. 4–12). We have not used this device in the presence of wounds with necrotic tissue and with purulent exudates. WCL (antibiotic-impregnated paraffin gauze) is used when NPWT is required to stabilize a STSG.
Figure 4.

Mine blast foot with composite loss of tissue in foot (soft tissue and osseous destruction in heel region is obvious). To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 5.

Wound debridement showing the removal of devitalized tissue and foreign bodies. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 6.

Application of NPWT system. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 7.

After 3 weeks of NPWT showing healthy granulation tissue. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 8.

Soft tissue cover achieved with extended reverse sural artery flap. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 9.

Gunshot wound shoulder showing large exit wound. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 10.

Application of NPWT system. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 11.

After 2 weeks of NPWT. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Figure 12.

After 6 weeks of NPWT showing dramatic reduction in size. Direct wound closure was achieved. To see this illustration in color, the reader is referred to the web version of this article at www.liebertpub.com/wound
Complications with NPWT
Although there are reports of major complications with NPWT in noncombat-related wounds, only minor complications have been reported with NPWT in combat-related wounds. This could be due to the nature of wounds being subjected to NPWT. Most complications were due to bleeding and infections.47,48
Future directions
Management of abdominal injury in combat trauma holds a special significance. Open abdominal wounds pose a challenge to the combat surgeon. Repeated abdominal surgeries require temporary closure of abdomen with a device which can protect the underlying viscera and yet it should be easy to apply. The ABThera Open Abdomen Negative Pressure Therapy System (Kinetic Concepts Incorporated) provides a method in temporary abdominal closure due to blast injuries or as in damage control surgery. This system when applied to porcine model was associated with lower systemic response syndrome and reduced multiorgan failure due to sepsis.49 Similarly, the negative pressure incisional management system (NPIMS) was developed to manage surgical wounds, which continued to drain following surgical closure or were at a high risk of wound complications. This system maintains a closed environment and removes exudates, thereby reducing the local inflammatory response and hematoma. This can be of an immense value in a patient who is likely to have wound complications following surgery. Colli reported its use (Prevena Incisional Management System; Kinetic Concepts Incorporated) on surgical incisions after cardiac surgery in high-risk patients. This form of therapy was used in 10 patients with a mean Fowler risk score of 15.1 with no wound-related or device-related complication. This study was limited by a small cohort size.50 Similarly Matatov et al. reported its use in the prevention of groin wound infection in vascular surgery patients.51 Ninety patients underwent vascular procedures with a longitudinal or transverse femoral cut down. Thirty percent of incisions in non-Prevena group had groin wound infections while only 6% of incisions in Prevena group had wound infection. This was found to be statistically significant (p=0.0011). The role of NPIMS in combat wound management needs further evaluation and is an area of future research. It can aptly be stated that reducing wound complications in a surgically created wound will help in early recovery and faster rehabilitation of injured soldiers.
Summary
Use of NPWT has proved to be an important modality in the management of complex war injuries. Military surgeons have moved on from wet gauze dressings to this novel modality of wound therapy in resource depleted war conditions. Standardization of this therapy and protocol-based management of combat wounds helps to achieve favorable outcomes. Its role is still evolving in the management of open abdominal wounds and is an area of further research in high-risk surgical incisions. It is without doubt that NPWT has changed the way military surgeons manage combat wounds.
Take-Home Messages.
Basic science advances
• Combat wounds are characterized by extensive tissue damage and gross contamination with foreign bodies.
• Complete wound debridement and irrigation followed by delayed reconstruction forms the basis of management of combat-related wounds.
Clinical science advances
• The outcomes of these wounds have shown to improve with the use of NPWT. The mechanism of action is multifactorial—macrodeformation, microdeformation, and secondary mechanisms.
• Its use has extended from managing soft tissue wounds of trunk and extremities to open abdominal wounds sustained during war.
Relevance to clinical care
• NPWT can be used effectively during the acute phase of combat wound management. Its use is associated with reduced wound infection rates, decreased frequency of wound dressings, and manpower saving.
• NPIMS is being evaluated to prevent surgical wound breakdown in at-risk battle casualties.
Abbreviations and Acronyms
- CONUS
continental United States
- IED
improvised explosive device
- IPT
intermittent pressure therapy
- NPIMS
negative pressure incisional management system
- NPWT
negative pressure wound therapy
- OEF
Operation Enduring Freedom
- OIF
Operation Iraqi Freedom
- ROCF
reticulated open cell foam
- STSG
split-thickness skin graft
- VEGF
vascular endothelial growth factor
- VPT
variable pressure therapy
- WCL
wound contact layer
Acknowledgment and Funding Sources
The authors wish to acknowledge Sarthak for his assistance in the preparation of Figures 2 and 3. No outside funding sources were used in the preparation of this article.
Author Disclosure and Ghostwriting
No competing financial interests exist. The content of this article was expressly written by the authors listed. No ghostwriters were used to write this article.
About the Authors
Dr. Sanjay Maurya, MS, MCh, is a Senior Advisor, Plastic and Reconstructive Surgery at the Command Hospital, Udhampur, India. He is the chief in-charge of the Trauma Reconstructive Unit and Burn Center at the Command Hospital. He is actively involved in combat trauma reconstruction, hand surgery, acute and chronic wound management, and burns. His areas of interest include hand and reconstructive microsurgery, negative pressure wound therapy, peripheral nerve and brachial plexus surgery. Prem Singh Bhandari, MS, MCh, is a Consultant Plastic and Reconstructive Surgeon at the Command Hospital, Udhampur, India. His areas of interest include wound healing, brachial plexus and peripheral nerve injuries. He has a vast experience in negative pressure therapy in the management of traumatic and nontraumatic wounds.
References
- 1.Taylor C, Jaffery S. Management of military wounds in modern era. Wounds 2009;5:50–58 [Google Scholar]
- 2.Leininger BE, Rasmussen TE, Smith DC, Jenkins DH, Coppola C. Experience with wound VAC and delayed primary closure of contaminated soft tissue injuries in Iraq. J Trauma 2006;61:1207–1211 [DOI] [PubMed] [Google Scholar]
- 3.Powell ET. Role of negative pressure wound therapy with reticulated open cell foam in the treatment of war wounds. J Orthop Trauma 2008;22:S138–S141 [DOI] [PubMed] [Google Scholar]
- 4.Geiger S, McCormick F, Chou R, Wangel AG. War wounds: lessons learned from Operation Iraqi Freedom. Plast Reconstr Surg 2008;122:146–153 [DOI] [PubMed] [Google Scholar]
- 5.Couch KS, Stojadinovic A. Negative-pressure wound therapy in military: lessons learned. Plast Reconstr Surg 2011;127:S117–S130 [DOI] [PubMed] [Google Scholar]
- 6.Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuilt N. Vacuum assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg 1997;38:553–562 [DOI] [PubMed] [Google Scholar]
- 7.Argenta LC, Morkykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg 1997;38:563–577 [PubMed] [Google Scholar]
- 8.DeFranzo AJ, Argenta LC, Marks MW, et al. The use of vacuum-assisted closure therapy for the treatment of lower extremity wounds with exposed bone. Plast Reconstr Surg 2001;108:1184–1191 [DOI] [PubMed] [Google Scholar]
- 9.Blume PA. Walters J, Payne W, Ayala J, Lantis J. Comparison of negative pressure therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. Diabetes Care 2008;31:631–636 [DOI] [PubMed] [Google Scholar]
- 10.Agarwal JP, Ogilvie M, Wu LC, et al. Vacuum-assisted closure for sterna wounds: a first-line therapeutic management approach. Plast Reconstr Surg 2005;116:1035–1040 [DOI] [PubMed] [Google Scholar]
- 11.Burris DG, Dougherty PJ, Elliot DC, et al. Soft tissue injuries. In: Emergency War Surgery, 3rd United States Revision, chapter 22, 22.1–22.14. Washington, DC: Borden Institute, Walter Reed Army Medical Centre, 2004 [Google Scholar]
- 12.Horrocks C. Blast injuries: biophysics, pathophysiology and management principles. J R Army Med Corps 2001;147:28–40 [DOI] [PubMed] [Google Scholar]
- 13.Granick M, Boykin J, Gamelli R, Schultz G, Tenenhaus M. Towards a common language: surgical wound bed preparation and debridement. Wound Repair Regen 2006;14:S1–S10 [DOI] [PubMed] [Google Scholar]
- 14.Guthrie HC, Clasper JC. Historical origins & current concepts of wound debridement. J R Army Med Corps 2011;157:130–132 [DOI] [PubMed] [Google Scholar]
- 15.Murray CK, Hsu JR, Solomkin JS, et al. Prevention and management of infections associated with combat-related extremities injuries. J Trauma 2008;64:S238–S251 [DOI] [PubMed] [Google Scholar]
- 16.Bhandari PS, Maurya S, Mukherjee MK. Reconstructive challenges in war wounds. Indian J Plast Surg 2012;45:332–339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tintle SM, Gwinn DE, Anderson RC, Kumar AR. Soft tissue coverage of combat wounds. J Surg Orthop Adv 2010;19:29–34 [PubMed] [Google Scholar]
- 18.Sorensen HB, Malmsjo M, Rome P, et al. Evidence-based recommendations for negative pressure wound therapy: treatment variables (pressure levels, wound filler and contact layer)—steps towards an international consensus. J Plast Reconst Aesthet Surg 2011;64:S1–S16 [DOI] [PubMed] [Google Scholar]
- 19.Moisidis E, Heath T, Boorer C, et al. A prospective, blinded, randomized controlled clinical trial of topical negative pressure in skin grafting. Plast Reconst Surg 2004;15:917–922 [DOI] [PubMed] [Google Scholar]
- 20.Kim EK, Hong JP. Efficacy of negative pressure therapy to enhance take of 1-stage allodermis and split-thickness graft. Ann Plast Surg 2007;58:536–540 [DOI] [PubMed] [Google Scholar]
- 21.Helgeson MD, Porter BK, Evans KN, Shawen SB. Bioartificial dermal substitute: a preliminary report on its use for the management of complex combat-related soft tissue wounds. J Orthop Trauma 2007;21:394–399 [DOI] [PubMed] [Google Scholar]
- 22.Scherer SS, Pietramaggiori G, Mathews JC, Prsa MJ, Huang S, Orgill DP. The mechanism of action of vacuum assisted closure device. Plast Reconst Surg 2008;122:786–799 [DOI] [PubMed] [Google Scholar]
- 23.Orgill DP, Manders EK, Sumpio BE, et al. The mechanism of action of vacuum assisted closure: more to learn. Surgery 2009;146:40–51 [DOI] [PubMed] [Google Scholar]
- 24.Huang C, Leavitt T, Bayer LR, Orgill DP. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg 2014;51:301–331 [DOI] [PubMed] [Google Scholar]
- 25.Krug E, Berg L, Lee C, et al. Evidence based recommendation for negative pressure wound therapy in traumatic wounds and reconstructive surgery: steps forwards and international consensus. Injury 2011;42:S1–S12 [DOI] [PubMed] [Google Scholar]
- 26.Scherer SS, Pietramaggiori G, Mathews JC, Orgill DP. Short periodic applications of the vacuum-assisted closure device cause an extended tissue response in the diabetic mouse model. Plast Reconstr Surg 2009;124:1458–1465 [DOI] [PubMed] [Google Scholar]
- 27.Baldwin C, Potter M, Clayton E, Irvine L, Dye J. Topical negative pressure stimulates endothelial migration and proliferation: a suggested mechanism for improved integration of Integra. Ann Plast Surg 2009;62:92–96 [DOI] [PubMed] [Google Scholar]
- 28.McNulty AK, Schmidt M, Feeley T, Kieswetter K. Effects of negative pressure wound therapy on fibroblast viability, chemotactic signaling, and proliferation in a provisional wound (fibrin) matrix. Wound Repair Regen 2007;15:838–846 [DOI] [PubMed] [Google Scholar]
- 29.Erba P, Ogawa R, Ackermann M, et al. Angiogenesis in wounds treated by microdeformational wound therapy. Ann Surg 2011;253:402–409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morykwas MJ, Simpson J, Punger K, Argenta A, Kremers L, Argenta J. Vacuum-assisted closure: state of basic research and physiologic foundation. Plast Reconstr Surg 2006;117:S121–S126 [DOI] [PubMed] [Google Scholar]
- 31.Penn-Barwell JG, Fries A, Street L, Jeffery S. Use of topical negative pressure in british servicemen with combat wounds. Eplasty 2011;11:354–363 [PMC free article] [PubMed] [Google Scholar]
- 32.Peck MA, Clouse WD, Cox MW, et al. The complete management of vascular injury in a local population: a war time report from 332nd Expeditionary Medical Group/Air Force Theatre Hospital, Balad Air Base, Iraq. J Vasc Surg 2007;45:1197–1204 [DOI] [PubMed] [Google Scholar]
- 33.Fang R, Dorlac WC, Flaherty SF, et al. Feasibility of NPWT during intercontinental aeromedical evacuation of combat casualties. J Trauma 2010;69:140–145 [DOI] [PubMed] [Google Scholar]
- 34.Pollak AN, Powel ET, Fang R, Cooper EO, Ficke JR, Flanerty SF. Use of negative pressure wound therapy during aeromedical evacuation of patients with combat related blast injuries. J Surg Orthop Adv 2010;19:44–48 [PubMed] [Google Scholar]
- 35.Morykwas MJ, Faler BJ, Pearce DJ, Argenta LC. Effect of varying level of sub atmospheric pressure on the rate of granulation tissue formation in experimental wounds in swine. Ann Plast Surg 2001;47:547–551 [DOI] [PubMed] [Google Scholar]
- 36.Borgquist O, Ingemansson R, Malmsjo M. Wound edge microvascular blood flow during negative pressure wound therapy: examining the effects of pressure from −10 to −175 mm Hg. Plast Reconst Surg 2010;125:502–509 [DOI] [PubMed] [Google Scholar]
- 37.Chen SZ, Li J, Li XY, Xu LS. Effects of vacuum-assisted closure on wound microcirculation: an experimental study. Asian J Surg 2005;28:211–217 [DOI] [PubMed] [Google Scholar]
- 38.Borgquist O, Ingemansson R, Malmsjo M. Individualizing the negative pressure wound therapy for optimal wound healing: a focused review of literature. Ostomy Wound Manage 2011;57:44–54 [PubMed] [Google Scholar]
- 39.Malmsjo M, Gustafsson L, Lindstedt S, Gosslein B, Ingemansson R. The effects of variable, intermittent and continous negative pressure wound therapy, using foam or gauze on wound contraction, granulation tissue formation and ingrowth into wound filler. Eplasty 2012;11:42–54 [PMC free article] [PubMed] [Google Scholar]
- 40.Malmsjo M, Ingemansson R, Martin R, Huddleston E. Wound edge microvascular blood flow: effects of negative pressure wound therapy using gauze or polyurethane foam. Ann Plast Surg 2009;63:676–681 [DOI] [PubMed] [Google Scholar]
- 41.Borgquist O, Gustafsson L, Ingemansson R, Malmsjo M. Micro and macromechanical effects on the wound bed of negative pressure wound therapy using gauze or polyurethane foam. Ann Plast Surg 2010;64:789–793 [DOI] [PubMed] [Google Scholar]
- 42.Dorafshar A, Franczyk M, Lohman R. Gottlieb L. A prospective randomized trial comparing subatmospheric wound therapy with sealed gauze dressing and the standard vacuum assisted closure device. Ann Plast Surg 2012;69:79–84 [DOI] [PubMed] [Google Scholar]
- 43.Yang CC, Chang DS, Webb LX. Vacuum assisted closure for fasciotomy wounds following compartment syndrome of leg. J Surg Orthop Adv 2006;15:19–23 [PubMed] [Google Scholar]
- 44.Hurd T, Chadwick P, Cote J, Cockwill J, Mole TR, Smith JM. Impact of gauze-based NPWT on the patient and nursing experience in the treatment of challenging wounds. Int Wound J 2010;7:448–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hinck D, Franke A, Gatzka F. Use of vacuum-assisted closure negative pressure wound thearapy in combat-related injuries—literature review. Mil Med 2010;175:173–181 [DOI] [PubMed] [Google Scholar]
- 46.Shweiki E, Gallagher KE. Assessing a safe interval for subsequent negative pressure wound therapy change after initial placement in acute contaminated wounds. Wounds 2013;25:263–271 [PubMed] [Google Scholar]
- 47.Petzina R, Malmsjo M, Stamm C, Hetzer R. Major complications during negative pressure wound therapy in poststernotomy mediastinitis after cardiac surgery. J Thorac Cardiovasc Surg 2010;140:1133–1136 [DOI] [PubMed] [Google Scholar]
- 48.White RA, Miki RA, Kazmier P, Anglen JO. Vacuum-assisted closure complicated by erosion and hemorrhage of the anterior tibial artery. J Orthop Trauma 2005;19:56–59 [DOI] [PubMed] [Google Scholar]
- 49.Kubiac BD, Albert S, Gatto L, et al. Peritoneal negative pressure therapy prevents multiple organ failure in chronic porcine sepsis and ischemia/reperfusion model. Shock 2010;34:525–534 [DOI] [PubMed] [Google Scholar]
- 50.Colli A. First experience with a new negative pressure incisional management system on surgical incisions after cardiac surgery in high risk patients. J Cardiothorac Surg 2011;6:160–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Matatov T, Reddy KN, Doucet LD, Zhao CX, Zhang WW. Experience with a new negative pressure incisional management system in prevention of groin wound infection in vascular surgery patients. J Vasc Surg 2013;57:791–795 [DOI] [PubMed] [Google Scholar]