Abstract
Background
The use of screening scales in cosmetic practices may help to identify patients who require education to modify inappropriate expectations and/or psychological support.
Objectives
To describe the development and validation of scales that measure expectations (about how one's appearance and quality of life might change with cosmetic treatments) and appearance-related psychosocial distress.
Methods
The scales were field-tested in patients 18 years and older seeking facial aesthetic or body contouring treatments. Recruitment took place in clinics in the United States, United Kingdom, and Canada between February 2010 and January 2015. Rasch Measurement Theory (RMT) analysis was used for psychometric evaluation. Scale scores range from 0 to 100; higher scores indicate more inappropriate expectations and higher psychosocial distress.
Results
Facial aesthetic (n = 279) and body contouring (n = 90) patients participated (97% response). In the RMT analysis, all items had ordered thresholds and acceptable item fit. Person Separation Index and Cronbach alpha values were 0.88 and 0.92 for the Expectation scale, and 0.81 and 0.89 for the Psychosocial Distress scale respectively. Higher expectation correlated with higher psychosocial distress (R = 0.40, P < .001). In the facial aesthetic group, lower scores on the FACE-Q Satisfaction with Appearance scale correlated with higher expectations (R = −0.27, P = .001) and psychosocial distress (R = −0.52, P < .001). In the body contouring group, lower scores on the BODY-Q Satisfaction with Body scale correlated with higher psychosocial distress (R = −0.31, P = .003). Type of treatment and marital status were associated with scale scores in multivariate models.
Conclusions
Future research could examine convergent and predictive validity. As research data are accumulated, norms and interpretation guidelines will be established.
Level of Evidence
2 Risk
Risk
Cosmetic procedures performed in the United States rose from 1.7 million in 1997 to 10.7 million in 2014.1 As increasing numbers of people seek treatments to change aspects of their appearance and improve psychosocial wellbeing, it is important that physicians ensure their patients have realistic expectations about the outcomes that can be achieved. Pre-treatment consultations provide physicians with an opportunity to identify and address any misconceptions their patient might have about likely treatment outcomes. A literature review on negative predictors of satisfaction in patients seeking facial cosmetic surgery cites high or unrealistic expectations as a factor often described in regards to disappointing results.2 Such expectations should raise a “red flag” as these patients are inclined to dissatisfaction regardless of the quality of the surgical result.3
In addition to expectations, consultations provide the opportunity to identify patients who may have underlying psychological issues and might benefit from additional support or referral. A psychiatric diagnosis that is sometimes seen in plastic surgery and dermatology clinics is that of body dysmorphic disorder (BDD). A BDD diagnosis has four criteria: preoccupied with one or more nonexistent or slight defects or flaws in one's physical appearance; engagement in repetitive behaviors (eg, mirror checking) or mental acts (eg, comparing one's appearance to others) in response to one's appearance concerns; preoccupation with appearance such that it causes impairment in social, occupation, or other areas of function; and the preoccupation is not attributable to another psychiatric diagnosis.4 While the rate of BDD in the general population is about two percent,5,6 Sarwer and Crerand examined findings from cosmetic surgery and dermatology studies and suggested the rate was higher at between 5 and 15 percent.7 Also, according to surveys conducted by Sarwer et al, approximately 40 percent of plastic surgeons8 and 12 percent of dermatologists9 reported that they had been threatened (legally and/or physically) by a patient with symptoms of BDD. Of the plastic surgeons, 84 percent also indicated that they had operated on a patient they believed was appropriate for surgery, but then realised after the surgery that the patient may have had BDD. This finding would suggest that BDD can be hard for surgeons to spot.The use of a brief self-report instrument to screen cosmetic patients in real-time clinical decision making may enable physicians to identify patients who require further education to modify expectations and/or patients who require additional support and/or psychological referral. A systematic rapid evidence assessment (SREA)10 on cosmetic intervention research published between 2002 and 2012, which reviewed findings from 13 systematic reviews and 179 primary studies, identified factors that may be associated with poor post-cosmetic psychological outcomes, including gender, relationship issues, and having unrealistic expectations. The evidence from this review supported improvement in psychosocial functioning following cosmetic procedures, though reductions in psychiatric symptoms, such as anxiety, depression, and body dysmorphic disorder (BDD), were less clear. The authors call for the use of robust study design in further research, and for routine psychosocial screening of all cosmetic patients using screening tools designed to assess a range of psychosocial risk factors beyond the focus on BDD.
By appropriately identifying possible mental health issues and by identifying and dealing with unrealistic expectations, a physician may avoid causing harm as well as possible legal action. In a systematic review to identify and appraise screening tools used with cosmetic surgery patients prior to surgery, our team found three such instruments.11 The DAS5912 and its short-form DAS2413 were designed to measure problems of appearance in people with disfigurements and aesthetic concerns. The DAS59 was not developed as a screening tool, although the authors suggest that their tool could be used for that purpose. The third instrument – PreFACE14 – represents a composite scale that includes 9 items taken from other published questionnaires. A psychometric limitation of PreFACE is that its development did not involve qualitative interviews with cosmetic surgery patients, an approach that limits content validity.15-17 Our review helped to clarify that to measure psychosocial distress and expectations and/or motivation in cosmetic surgery patients, scientifically sound and clinically meaningful patient-reported scales were needed.
The primary aim of this article was to describe the development and psychometric evaluation of two new scales designed for use in clinical practice and research with cosmetic patients. These scales measure: (1) expectations about how one's appearance and quality of life might change with cosmetic treatments; and (2) appearance-related psychosocial distress. To advance knowledge about factors associated with expectations and psychosocial distress, a secondary aim was to explore relationships between the scales' scores and patient (ie, age, gender, ethnicity, marital status) and clinical (ie, type of cosmetic treatment) factors, and patient self-report ratings of satisfaction with appearance.
METHODS
The two new scales—Expectations and Psychosocial Distress—were developed following internationally recommended guidelines for the development of a patient-reported outcome (PRO) instrument.15-17 The two scales were developed as part of a set of 40 plus scales designed in the FACE-Q study, which is described in full elsewhere.18-23 The FACE-Q is a PRO instrument designed to measure important concepts of interest to surgical and nonsurgical facial aesthetics patients, including facial appearance, adverse effects, patient experience and quality of life. Briefly, a systematic review,24 interviews with 50 surgical and/or nonsurgical facial aesthetic patients, and input from 26 experts in the field, were used to develop the FACE-Q conceptual framework and scales and checklists. The scales and checklists were further refined through cognitive interviews with 35 facial aesthetic patients. Specifically, the interviews were used to obtain feedback from patients on the instructions, response options, and set of items for each scale, in order to identify where refinement was needed. Given the large number of FACE-Q scales addressing various facial anatomical areas and aspects of outcome, results for the scales have been published as a series of articles, each of which describes a clinically relevant grouping (eg, FACE-Q scales for rhinoplasty patients23) or aspect of outcome (eg, FACE-Q scale for measuring quality of life22).
In addition to the FACE-Q, we previously described the development of the BODY-Q conceptual framework and set of scales, which involved a literature review, 63 patient interviews, 22 cognitive patient interviews, and input from nine clinical experts (phase 1).25,26 The BODY-Q is a PRO instrument designed to measure appearance, patient experience of care, and quality of life in patients undergoing weight loss and/or body contouring. Rather than perform the psychometric evaluation using only facial aesthetics patients, we included the 2 scales in the BODY-Q development study. Specifically, the Expectations and Psychosocial Distress scales were shown to participants during cognitive interviews, in order to determine acceptability and content validity in body contouring patients.
The Expectations scale includes statements that people might use to describe how their appearance and quality of life might change following a cosmetic procedure (eg, “I will look fantastic,” “I will be transformed,” “My close relationships will improve”). The Psychosocial Distress scale includes statements to measure appearance-related concerns (eg, “I feel unhappy about how I look,” “I feel anxious when people look at me,” “I worry that I am ugly”). Both scales ask respondents to answer with their appearance in mind, and each has the following four response options: “Definitely Disagree,” “Somewhat Disagree,” “Somewhat Agree,” and “Definitely Agree.” Higher scores on the scales indicate higher (ie, less appropriate) expectations and more appearance-related psychosocial distress. The scoring algorithm to convert raw scale scores to a 0 to 100 scale is available from the authors.
Field-test data to evaluate the psychometric properties of the Expectations and Psychosocial Distress scales came from both the FACE-Q and BODY-Q field-test studies as described below.
Study 1: FACE-Q Field-Test
Ethics review board approval was obtained prior to study initiation. In the United States, institutional review board approval was obtained through the New School in New York City. In Canada, research ethics approval was obtained through the University of British Columbia (Behavioral Research Ethics Board) and McMaster University (Hamilton Integrated Research Ethics Board). In the United Kingdom, local research and developmental approval (National Health Services permission) was obtained from University College London Hospitals National Health Service Foundation Trust. In the FACE-Q field-test, the Expectations and Psychosocial Distress scales were completed by pre-treatment patients aged 18 years and older consulting for any type of surgical and/or nonsurgical facial aesthetic treatment. The first and last participant to complete the two scales in the FACE-Q study was recruited from nine clinics in Canada, the United States, England, and Scotland between February 2010 and January 2015. Staff recruited patients into the study upon check-in. Data were collected using an iPad directly into a web-based application or a questionnaire booklet that did not ask for any identifiable data to ensure patient anonymity. Participants were left alone to answer the questionnaire. Instructions provided to patients told them that if they were unsure how to answer a question, they should answer the best they can. The United States, Canadian, and Scottish participants were provided a coffee card to thank them for their time.
Study 2: BODY-Q Field-Test
Ethics review board approval for the BODY-Q study was also obtained prior to initiation. In Canada, research ethics approval was obtained at McMaster University (Hamilton Integrated Research Ethics Board) and the University of British Columbia (Behavioral Research Ethics Board). In the United States, ethics approval was obtained through the IRB Company Incorporated (Buena Park, CA). In the BODY-Q field-test, the Expectations and Psychosocial Distress scales were completed by pre-treatment cosmetic body contouring surgery patients aged 18 years and older. Participants were consulting for any type of body contouring. The first and last participant to complete the two scales in the BODY-Q study was recruited by staff from three clinics in Canada and the United States between December 2013 and December 2014. Staff recruited patients into the study upon check-in. Data were collected using an iPad directly into a web-based application or a questionnaire booklet that did not ask for any identifiable data to ensure patient anonymity. Participants were asked questions to indicate the type of body contouring procedure(s) they were seeking. As above, participants were left alone to answer the questionnaire. Instructions provided to patients told them that if they were unsure how to answer a question, they should answer the best they can. Participants were provided a coffee card to thank them for their time
Analysis
To address the psychometric aim, we used RUMM2030 software (Perth, Australia)27 and conducted Rasch Measurement Theory (RMT) analysis.28-29 RMT examines the difference between observed and predicted item responses to determine if data from a sample fit the Rasch model.28-29 The results from a range of statistical and graphical tests were examined, with the evidence from the various tests considered together to make a decision about each scale's overall quality. We performed the following tests, which are explained in more detail elsewhere:30
Thresholds for item response options: for each scale, we examined thresholds between response options (eg, between Definitely Agree and Somewhat Agree) to determine if a scale's response categories scored with successive integer scores increased as intended.
Item fit statistics: we examined three indicators of fit to determine if the items of each scale worked together to map out a clinically important construct in the form of a hierarchy: (i) log residuals (item–person interaction); (ii) chi-square values (item–trait interaction); and (iii) item characteristic curves (ICC). Fit residuals should be between −2.5 and +2.5, and chi-square values should be non-significant after Bonferroni adjustment. We interpreted fit statistics together and in relation to clinical usefulness of the scale.
Targeting: for each scale, we examined person and item locations to determine if items were evenly spread over a reasonable range that matched the range of the construct reported by the sample.
Dependency: residual correlations between pairs of items were inspected to identify any that were 0.30 or higher as high residual correlations can artificially inflate reliability.29
Stability: differential item functioning (DIF) was examined to determine if items in a scale worked the same across subgroups within the sample. Subgroups that were examined included age group (<30, 30-39, 40-49, 50-59, 60 ≥ years), race/ethnicity (white vs other), gender, field-test study (BODY-Q or FACE-Q), and procedure type (minimally invasive treatments, rhinoplasty, antiaging facial surgery, chin and/or jaw surgery, body contouring). Chi-square values significant after Bonferroni adjustment were used to indicate items with potential DIF.
Person separation index (PSI): we computed the PSI for each scale. PSI measures error associated with the measurement of people in a sample and is comparable to Cronbach's alpha31 which we also computed. For both PSI and Cronbach alpha, higher values indicate greater reliability.
To address the secondary aim, we computed Pearson or Spearman correlations as appropriate to examine relationships between scores on the Expectations, Psychosocial Distress, and Satisfaction with Appearance scales. Self-perceived appearance was measured using the FACE-Q Satisfaction with Appearance scale for facial aesthetic patients, and the BODY-Q Satisfaction with Body scale for body contouring participants. Previous publications19,26 supported these 10-item scales as reliable, valid, and responsive measurement tools that score appearance from 0 (lowest satisfaction) to 100 (highest satisfaction).
Potential predictors of Expectations and Psychological Distress were determined using univariate linear regression analyses. The following variables, which were analyzed in relation to the scales' scores, were included in the analysis as follows: age (continuous); gender (female = 1; male = 0); race/ethnicity (white = 1; other = 0); marital status, categorized as three variables (married/common-law, single, separated/divorced/widowed), with each category analyzed as a dichotomous variable (eg, married/common-law = 1; other = 0); and treatment type categorized as five variables (minimally invasive treatment, rhinoplasty, antiaging facial surgery, chin and/or jaw surgery, body contouring), with each category analyzed as a dichotomous variable. For the multivariate analysis, factors that were associated with Expectations and Psychosocial Distress scores at P < .1 were entered into a forward selection linear regression model. Statistical significance were two-sided tests and defined as P < .05.
RESULTS
Only a few patients declined to participate in this study, resulting in a response rate of 97 percent. Table 1 shows the sample characteristics. The screening scales were completed by 279 facial aesthetic and 90 body contouring participants. The mean age of the combined sample was 42.6 (range 18 to 85 years), 78 percent were female and 70 percent were Caucasian. The 90 participants seeking body contouring indicated that they were seeking between 1 and 8 procedures, which included the following: liposuction (n = 67), abdominoplasty (n = 52), breast lift/gynaecomastia (n = 29), buttocks lift (n = 4), inner thigh lift (n = 3), hips and outer thigh lift (n = 2), arm lift (N = 2), and backlift (n = 1). Two body contouring participants reported they had previously had bariatric surgery in the past.
Table 1.
Participant Characteristics
| N | 369 |
|---|---|
| Age (y) | |
| Mean (SD) | 42.6 (15) |
| Range | 18 to 85 |
| Gender | |
| Female | 288 (78) |
| Male | 68 (18.4) |
| Missing | 13 (3.5) |
| Race/ethnicity | |
| White | 257 (69.6) |
| Other | 91 (24.7) |
| Missing | 21 (5.7) |
| Marital status | |
| Married or living common-law | 189 (51.2) |
| Single | 110 (29.8) |
| Other (divorced, separated, widowed) | 51 (13.8) |
| Missing | 19 (5.1) |
| Country | |
| USA | 301 (81.6) |
| United Kingdom | 65 (17.6) |
| Canada | 3 (0.8) |
| Type of patient (%) | |
| Rhinoplasty | 97 (26.3) |
| Minimally invasive, injectable, and/or skin treatment | 72 (19.5) |
| Antiaging surgery - facelift, necklift, browlift, and/or blepharoplasty | 76 (20.6) |
| Jaw and/or chin procedure | 34 (9.2) |
| Body contouring | 90 (24.4) |
Psychometric Analyses
The RMT findings for the two scales supported their reliability and validity. For each scale, all items had ordered thresholds supporting the hypothesis that the successive integer scores worked as a continuum. Table 2 shows the item fit for the two scales; 15/16 items fit within the recommended range of −2.5 to + 2.5 and 16/16 were not significant in terms of the chi-square P values. The one item with marginal misfit was retained in the scale due to its clinical importance as an indicator of mood.
Table 2.
Rasch Measurement Theory Statistical Indicators of Fit
| Scale | Item | Item location | SE | Fit Residual | Chi-square | DF | P-value |
|---|---|---|---|---|---|---|---|
| Expectations | Will look fantastic | −1.53 | 0.09 | 1.78 | 16.97 | 5 | .005 |
| People will tell me I look great | −1.38 | 0.10 | 1.67 | 4.87 | 5 | .433 | |
| People will be proud of how I look | −0.08 | 0.08 | −0.60 | 7.35 | 5 | .196 | |
| Will be transformed | 0.14 | 0.08 | −1.12 | 10.58 | 5 | .060 | |
| Good things will happen to me | 0.30 | 0.08 | −2.19 | 13.39 | 5 | .020 | |
| Will feel like I fit in | 0.47 | 0.08 | −1.39 | 8.70 | 5 | .122 | |
| Close relationships will improve | 0.82 | 0.09 | −0.31 | 7.26 | 5 | .202 | |
| New people will want to know me | 1.25 | 0.09 | −1.45 | 15.12 | 5 | .010 | |
| Distress | Feel unhappy | −1.74 | 0.09 | 1.59 | 12.83 | 5 | .025 |
| Feel stressed | −0.75 | 0.09 | −0.67 | 10.22 | 5 | .069 | |
| Feel down | −0.53 | 0.09 | −3.12 | 18.73 | 5 | .002 | |
| Feel anxious | 0.02 | 0.09 | 1.11 | 5.78 | 5 | .328 | |
| Worry don′t look normal | 0.59 | 0.10 | −1.92 | 8.57 | 5 | .128 | |
| Worry I am ugly | 0.59 | 0.10 | −1.81 | 5.86 | 5 | .320 | |
| Avoid people | 0.85 | 0.10 | 0.06 | 4.28 | 5 | .510 | |
| Little interest doing things | 0.97 | 0.10 | −1.13 | 5.68 | 5 | .339 |
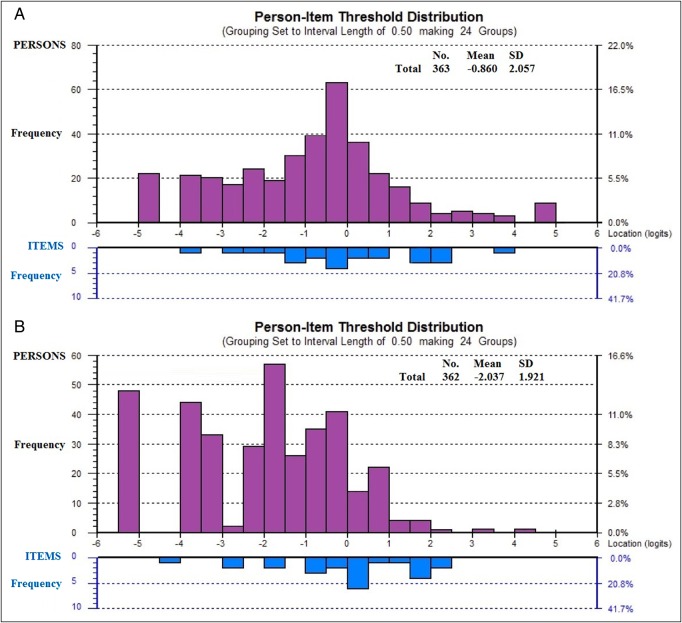
The scale-to-sample targeting are shown in Figure 1, with the scales' items (bottom histograms) mapping out the continuum for the constructs being measured. In each figure, the x-axis represents the construct, with higher expectations (Figure 1A) and more psychosocial distress (Figure 1B) increasing to the right. The y-axis shows the frequency of person measure locations (top histogram) and item locations (bottom histogram). The findings show the scales defined a continuum for the constructs being measured, with little evidence of a ceiling effect, which is important for screening.
Figure 1.
(A) Person Threshold Distribution for Expectation scale. The x-axis represents the construct (Expectations), with higher scores (more inappropriate expectations) increasing to the right. The y-axis shows the frequency of person measure locations (top histogram) and item locations (bottom histogram). (B) Person Threshold Distribution for Psychosocial Distress scale. The x-axis represents the construct (Psychosocial Distress), with higher scores (more distress) increasing to the right. The y-axis shows the frequency of person measure locations (top histogram) and item locations (bottom histogram).
Table 3 shows the proportion of participants to endorse each of the item response options. The items, sorted into hierarchical order, show the pattern of responses according to the clinical hierarchy for each construct. For example, in the Expectations scale, the first item “I will look fantastic” was endorsed by 68 percent of participants, whereas for last item “New people will want to get to know me” was endorsed by 22 percent of participants.
Table 3.
Proportion of Participants in the Sample to Endorse Each Item
| Definitely disagree |
Somewhat disagree |
Somewhat agree |
Definitely agree |
Missing |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| Expectations | ||||||||||
| 1. Will look fantastic | 54 | 14.8 | 55 | 15.1 | 163 | 44.8 | 86 | 23.6 | 6 | 1.6 |
| 2. People will tell me I look great | 42 | 11.5 | 78 | 21.4 | 183 | 50.3 | 55 | 15.1 | 6 | 1.6 |
| 3. People will be proud of how I look | 132 | 36.3 | 67 | 18.4 | 117 | 32.1 | 44 | 12.1 | 4 | 1.1 |
| 4. Will be transformed | 144 | 39.6 | 93 | 25.5 | 78 | 21.4 | 43 | 11.8 | 6 | 1.6 |
| 5. Good things will happen to me | 150 | 41.2 | 85 | 23.4 | 94 | 25.8 | 33 | 9.1 | 2 | 0.5 |
| 6. Will feel like I fit in | 168 | 46.2 | 89 | 24.5 | 73 | 20.1 | 31 | 8.5 | 3 | 0.8 |
| 7. Close relationships will improve | 196 | 53.8 | 69 | 19.0 | 71 | 19.5 | 27 | 7.4 | 1 | 0.3 |
| 8. New people will want to know me | 192 | 52.7 | 88 | 24.2 | 65 | 17.9 | 16 | 4.4 | 3 | 0.8 |
| Psychosocial distress | ||||||||||
| 1. Feel unhappy | 68 | 18.7 | 129 | 35.4 | 126 | 34.6 | 39 | 10.7 | 2 | 0.5 |
| 2. Feel stressed | 135 | 37.1 | 122 | 33.5 | 78 | 21.4 | 25 | 6.9 | 4 | 1.1 |
| 3. Feel down | 148 | 40.7 | 117 | 32.1 | 76 | 20.9 | 20 | 5.5 | 3 | 0.8 |
| 4. Feel anxious | 189 | 51.9 | 100 | 27.5 | 59 | 16.2 | 12 | 3.3 | 4 | 1.1 |
| 5. Worry don′t look normal | 240 | 65.9 | 71 | 19.5 | 42 | 11.5 | 8 | 2.2 | 3 | 0.8 |
| 6. Worry I am ugly | 267 | 73.4 | 54 | 14.8 | 30 | 8.2 | 12 | 3.3 | 1 | 0.3 |
| 7. Avoid people | 279 | 76.6 | 48 | 13.2 | 28 | 7.7 | 7 | 1.9 | 2 | 0.5 |
| 8. Little interest doing things | 285 | 78.3 | 44 | 12.1 | 25 | 6.9 | 7 | 1.9 | 3 | 0.8 |
Missing data ranged from 1 to 6 cases; Items are abbreviated, contact the authors for the complete scale and associated scoring tables (scale and tables are subject to the copyright of Memorial Sloan Kettering Cancer Center).
The item residual was 0.31 for one pair of items (“I tend to avoid being around people” and “I have little interest in doing things”). A subtest performed on the pairs of items revealed marginal impact on scale reliability (PSI value dropped by 0.01).
Two items in the Psychosocial Distress scale evidenced DIF for age group, and 3 items in the Expectations scale evidenced DIF for study, age-group, and/or gender. However, when the items were split on the variable with DIF, and the new person locations for the scale were correlated with the original person locations, the DIF was found to have negligible impact on the scales (Pearson correlations were 0.99).
In terms of reliability, the PSI and Cronbach alpha for the Expectation scale was 0.88 and 0.92 and for the Psychosocial Distress was 0.81 and 0.89, respectively. The Flesch-Kincaid grade reading levels for the two scales were low, with all but one item a grade 3.9 or lower (Expectations: mean, 1.5 [range, 0 to 7.6]; Psychosocial Distress: mean, 2.7 [range, 0.6 to 3.9]).
Exploratory Analyses
Participants with higher expectations tended to report more psychosocial distress (R = 0.40, P < .001). In the facial aesthetic group, lower scores on the Satisfaction with Facial Appearance scale correlated with higher scores on the Expectations (R = −0.27, P = .001) and Psychosocial Distress (R = −0.52, P < .001) scales. For the body contouring group, lower scores on the Satisfaction with Body scale correlated with higher scores on the Psychosocial Distress scale (R = −0.31, P = .003).
Figure 2 shows the mean scores for the Expectations and Psychosocial Distress scales by the type of treatment. The differences between mean scores for both scales were significant (P ≤ .003) on ANOVA. Participants seeking minimally invasive treatments reported the lowest mean score on the Expectations and the Psychosocial Distress scales. Patients seeking body contouring reported the highest mean score on the Expectations scale, while the highest mean score for Psychosocial Distress was shared by patients seeking a rhinoplasty and body contouring. Mean scores on the Satisfaction with Facial Appearance scale varied significantly by treatment type (P = .017 on Kruskal-Wallis test), with patients in the antiaging surgery group reporting the lowest satisfaction.
Figure 2.
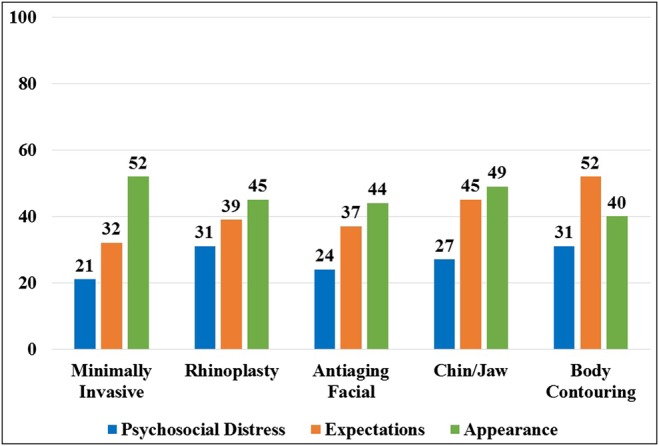
Mean score by procedural group in the sample.
Table 4 illustrates that factors significantly associated with lower scores on the Expectations scale included being married/living common-law as well as seeking minimally invasive treatments, while higher scores were associated with seeking body contouring surgery. Higher scores on the Psychosocial Distress scale were associated with younger age, not being married/living common-law, and seeking rhinoplasty or body contouring surgery, while lower scores were associated with seeking minimally invasive treatments.
Table 4.
Univariate Predictors of Expectations and Psychosocial Distress
| Variable | Expectations |
Psychosocial distress |
||
|---|---|---|---|---|
| B ± s.e. | P-value | B ± s.e. | P-value | |
| Demographic factors | ||||
| Age in years | −0.08 ± 0.08 | .28 | −0.17 ± 0.07 | .02 |
| Female | 2.66 ± 2.91 | .36 | −4.05 ± 2.83 | .15 |
| Race/ethnicity white | −4.95 ± 2.61 | .06 | 0.43 ± 2.55 | .87 |
| Married or common-law | −5.48 ± 2.28 | .02 | −5.02 ± 2.23 | .03 |
| Single | 1.34 ± 2.45 | .17 | 4.40 ± 2.39 | .07 |
| Divorced, Separated, Widowed | 5.04 ± 3.21 | .12 | 2.39 ± 3.20 | .45 |
| Cosmetic treatment | ||||
| Minimally invasive treatment | −11.46 ± 2.76 | <.001 | −7.73 ± 2.68 | .004 |
| Antiaging facial surgery | −4.25 ± 2.79 | .13 | −4.49 ± 2.63 | .09 |
| Rhinoplasty | −2.71 ± 2.55 | .29 | 5.46 ± 2.43 | .03 |
| Jaw and/or chin procedure | 4.39 ± 3.84 | .25 | −0.71 ± 3.69 | .85 |
| Body contouring | 14.14 ± 2.49 | <.001 | 5.34 ± 2.51 | .03 |
B, B-coefficient from univariate linear regression; s.e., standard error.
Positive B-coefficients mean that the predictor (or increasing values of the predictor) was associated with worse scores (higher expectations or more psychosocial distress), whereas negative B-coefficients suggested that the predictors (or increasing values of the predictor) was associated with better scores (lower expectations or less psychosocial distress).
In the multivariate models, variables that were independently associated with Expectations and Psychosocial Distress scale scores are shown in Table 5. Being married/common-law and seeking minimally invasive treatments were independently associated with lower expectations, while seeking body contouring was associated with higher expectations. Seeking minimally invasive treatments or antiaging facial surgery were independently associated with reporting lower scores for appearance-related psychosocial distress.
Table 5.
Multivariate Analysis for Expectations and Psychosocial Distress
| Variables | B ± s.e. | P-value |
|---|---|---|
| Expectation score | ||
| Body contouring | 14.89 ± 2.65 | <.001 |
| Married or common-law | −9.44 ± 2.25 | <.001 |
| Injectable and/or skin treatment | −7.20 ± 2.88 | .013 |
| Psychosocial distress score | ||
| Minimally invasive treatment | −10.07 ± 2.89 | .001 |
| Antiaging facial surgery | −7.11 ± 2.79 | .011 |
B, B-coefficient from univariate linear regression; s.e., standard error.
Positive B-coefficients mean that the predictor (or increasing values of the predictor) was associated with worse scores (higher expectations or more psychosocial distress), whereas negative B-coefficients suggested that the predictors (or increasing values of the predictor) were associated with better scores (lower expectations or less psychosocial distress).
DISCUSSION
People coming forward for cosmetic surgery can have inappropriate expectations and experience appearance-related psychosocial distress. Cosmetic practitioners may benefit from the use of short, clinically meaningful scales in the clinical encounter to identify patients who may require additional education and attention.
Patient-centered self-report instruments were initially designed for use in academic and industry research, but are increasingly being used in clinical care, patient/consumer education, benchmarking, and quality improvement.32 We anticipate that some plastic surgeons will be keen to use these screening scales with patients to identify concerns and use this information in patient management. We intentionally kept the current scales short to minimize the burden associated with using self-report instruments in clinical care. By testing the scales in a large sample that included participants from the FACE-Q and the BODY-Q field-test studies, we aimed to ensure the two scales' generalizability in clinical practice given the variety of patients many cosmetic practitioners see. The psychometric findings showed that the scales evidenced reliability and validity, and that neither scale had a significant ceiling effect. Future prospective studies are now needed to examine other measurement properties, including convergent and predictive validity, and to establish norms and interpretation guidelines.
Our exploratory analysis identified that not being in a marital or common-law relationship was associated with reporting more psychosocial distress. In a recent large US study of BDD prevalence in facial plastic surgery patients, Dey et al found that in their sample of 234 patients (122 cosmetic and 112 reconstructive), those diagnosed with BDD were younger and more likely to be single or divorced.33 We also found, not surprisingly, that expectations and psychosocial distress was higher in patients seeking surgical over minimally invasive treatments. In particular, patients seeking body contouring reported the highest scores for both expectations and psychosocial distress. Body contouring is in fact the most invasive of the procedures included in our sample as such treatments aim to alter the shape and size of the body. Body contouring is increasingly sought by patients who have experienced massive weight loss and have excess hanging skin, which can be highly distressing.34-36 The goal in facial aesthetic treatments, on the other hand, is usually more subtle (ie, to improve the appearance of a facial feature such as the nose) or to make someone look younger or more refreshed, but not necessarily dramatically different.
Many studies of different surgical patient groups have shown that expectations play an important role in patient assessment of the results of surgery.36-39 Studying expectations and patient-reported outcomes (PROs), a systematic review by Walijee et al suggests patient expectations are inconsistently correlated with PROs following surgery.39 These authors examined 60 studies and reported that while most showed that positive expectations correlated with improved PROs, even when expectations were not completely met, a large proportion of studies reported worse PROs with fulfilment of expectations, and some studies failed to identify any relationship between patient expectations and PROs. The authors note that few validated methods for measuring patient expectations exist and that a vast array of instruments has been used to collect this information. In cosmetic surgery, research using our new validated scales is needed to gain knowledge about expectations and appearance-related psychosocial distress for different types of cosmetic interventions and how these relate to patient factors and important patient-centered outcomes. Further insight into the efficacy of educational interventions would also be important to examine whether expectations in cosmetic patients can be modified and how modification relates to satisfaction with appearance and quality of life outcomes.
Both our FACE-Q and BODY-Q field-test studies have limitations that we have previously described.18-23,25-26 Specifically, both the FACE-Q and BODY-Q samples included more women compared with men, which reflects the nature of cosmetic surgery patients in the general population. Also, both samples were heterogeneous in terms of patient characteristics. While heterogeneity can be good in PRO instrument development studies, as the variability makes it possible to develop scales targeted to a wide and diverse sample, it can also limit our ability to report findings beyond the psychometric. While we performed DIF by age, race/ethnicity, gender, field-test sample, and procedure type, the small number of Canadian participants limited our ability to examine DIF by country. Another limitation is that the office staff who recruited the sample may have introduced bias in the selection of patients. We have no way of knowing for sure if “highly distressed” clients, for example, were not recruited. Our study is also limited in the use of a cross-sectional design, which did not allow us to examine predictive validity (ie, that high expectations and psychosocial distress are related to worse outcomes). Prospective outcomes studies that examine additional psychometric properties, including that of convergent and predictive validity, are called for. As research data are accumulated, we will be able to establish norms and interpretation guidelines.
CONCLUSION
To conclude, in treatments that aim to change someone's physical appearance for aesthetic rather than medical reasons, the use of pre-treatment instruments during a clinical encounter could help physicians to efficiently identify patients who may require education to ensure their expectations are appropriate and/or additional support or psychological referral. Further research is needed to determine if the use of screening tools in cosmetic practice may improve quality of care, with better patient safety and outcomes.
Disclosures
Drs Cano, Klassen, and Pusic are co-developers of the FACE-Q and, as such, receive a share of any license revenues as royalties based on Memorial Sloan Kettering Cancer Center's inventor sharing policy. Dr Cano is cofounder of Modus Outcomes, a research and consulting firm that provides services to pharmaceutical, medical device, and biotechnology companies. The other authors have no disclosures to report in relation to this study.
Funding
Grant funding to develop and field-test the FACE-Q came from The Plastic Surgery Foundation, and grant funding for the BODY-Q came from The Plastic Surgery Foundation and the Canadian Institutes of Health Research. The Expectations and Psychosocial Distress scales belong to the FACE-Q, which is owned by Memorial Sloan-Kettering Cancer Center.
Acknowledgments
The authors acknowledge and thank all participating clinicians for their invaluable assistance with the recruitment of patients, and the patients who were willing to participate and complete the scales.
REFERENCES
- 1.Cosmetic surgery national data bank statistics. Aesthet Surg J. 2015;35(Suppl 2):1-24. [DOI] [PubMed] [Google Scholar]
- 2.Herruer JM, Prins JB, van Heerbeek N, Verhage-Damen GW, Ingels KJ. Negative predictors for satisfaction in patients seeking facial cosmetic surgery: a systematic review. Plast Reconstr Surg. 2015;135:1596-1605. [DOI] [PubMed] [Google Scholar]
- 3.Gorney M. Recognition and Management of the Patient Unsuitable for Aesthetic Surgery. Plast Reconstr Surg. 2010;126:2268-2071. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed Arlington VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 5.Rief W, Buhlmann U, Wilhelm S, Borkenhagen A, Brähler E. The prevalence of body dysmorphic disorder: a population-based survey. Psychol Med. 2006;36:877-885. [DOI] [PubMed] [Google Scholar]
- 6.Koran LM, Abujaoude E, Large MD, Serpe RT. The prevalence of body dysmorphic disorder in the United States adult population. CNS Spectr. 2008;13:316-322. [DOI] [PubMed] [Google Scholar]
- 7.Sarwer DB, Crerand CE. Body dysmorphic disorder and appearance enhancing medical treatments. Body Image. 2008;5:50-58. [DOI] [PubMed] [Google Scholar]
- 8.Sarwer DB. Awareness and identification of body dysmorphic disorder by aesthetic surgeons: results of a survey of American Society for Aesthetic Plastic Surgery members. Aesthet Surg J. 2002;22:531-535. [DOI] [PubMed] [Google Scholar]
- 9.Sarwer DB, Spitzer JC, Sobanko JF, Beer KR. Identification and management of mental health issues by dermatologic surgeons: a survey of American Society for Dermatologic Surgery members. Dermatol Surg. 2015;41:352-357. [DOI] [PubMed] [Google Scholar]
- 10.Brunton G, Paraskeva N, Caird J et al. Psychosocial predictors, assessment, and outcomes of cosmetic procedures: a systematic rapid evidence assessment. Aesthetic Plast Surg. 2014;38:1030-1040. [DOI] [PubMed] [Google Scholar]
- 11.Wildgoose P, Scott A, Pusic AL, Cano S, Klassen AF. Psychological screening measures for cosmetic plastic surgery patients: a systematic review. Aesthet Surg J. 2013;33:152-159. [DOI] [PubMed] [Google Scholar]
- 12.Harris DL, Carr AT. The Derriford Appearance Scale (DAS59): a new psychometric scale for the evaluation of patients with disfigurements and aesthetic problems of appearance. Br J Plast Surg. 2001;54:216-222. [DOI] [PubMed] [Google Scholar]
- 13.Carr T, Moss T, Harris D. The DAS24: a short form of the Derriford Appearance Scale DAS59 to measure individual responses to living with problems of appearance. Br J Health Psychol. 2005;10(pt 2):285-298. [DOI] [PubMed] [Google Scholar]
- 14.Honigman RJ, Jackson AC, Dowling NA. The PreFACE: a preoperative psychosocial screen for elective facial cosmetic surgery and cosmetic dentistry patients. Ann Plast Surg. 2011;66:16-23. [DOI] [PubMed] [Google Scholar]
- 15.International Society for Pharmacoeconomics and Outcomes Research. Guidance for industry: Patient-reported outcome measures: Use in medical product development to support labeling claims. http://www.ispor.org/workpaper/FDA%20PRO%20Guidance.pdf Accessed December 4, 2015. [DOI] [PMC free article] [PubMed]
- 16.Patrick DL, Burke LB, Gwaltney CJ et al. Content validity--establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 1--eliciting concepts for a new PRO instrument. Value Health. 2011;14:967-977. [DOI] [PubMed] [Google Scholar]
- 17.Patrick DL, Burke LB, Gwaltney CJ et al. Content validity--establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2--assessing respondent understanding. Value Health. 2011;14:978-988. [DOI] [PubMed] [Google Scholar]
- 18.Klassen AF, Cano SF, Scott A, Snell L, Pusic AL. Measuring patient-reported outcomes in facial aesthetic patients: development of the Face-Q. Facial Plast Surg. 2010;26:303-309. [DOI] [PubMed] [Google Scholar]
- 19.Pusic A, Klassen AF, Scott AM, Cano SJ. Development and psychometric evaluation of the FACE-Q Satisfaction with Appearance Scale: A new patient-reported outcome instrument for facial aesthetics patients. Clin Plast Surg. 2013;40:249-260. [DOI] [PubMed] [Google Scholar]
- 20.Panchapakesan V, Klassen AF, Cano SJ, Scott AM, Pusic AL. Development and Psychometric Evaluation of the FACE-Q Aging Appraisal Scale and Patient-Perceived Age Visual Analog Scale. Aesthet Surg J. 2013;33:1099-1109. [DOI] [PubMed] [Google Scholar]
- 21.Klassen AF, Cano SJ, Scott AM, Pusic AL. Measuring outcomes that matter to facelift patients: development and validation of FACE-Q Appearance Appraisal Scales and Adverse Effects Checklist for the lower face and neck. Plast Reconstr Surg. 2014;133:21-30. [DOI] [PubMed] [Google Scholar]
- 22.Klassen AF, Cano SJ, Schwitzer J, Scott AM, Pusic AL. FACE-Q scales for health-related quality of life, early life impact and satisfaction with outcomes and decision to have treatment: development and validation. Plast Reconstr Surg. 2015;135:375-386. [DOI] [PubMed] [Google Scholar]
- 23.Klassen AF, Cano SJ, East CA et al. Development and psychometric evaluation of the FACE-Q scales for patients undergoing rhinoplasty. JAMA Facial Plast Surg. 2016;18:27-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kosowski TR, McCarthy C, Reavey PL et al. A systematic review of patient reported outcome measures after facial cosmetic surgery and/or non-surgical facial rejuvenation. Plast Reconstr Surg. 2009;123:1819-1827. [DOI] [PubMed] [Google Scholar]
- 25.Klassen AF, Cano SJ, Scott A, Tsangaris E, Johnson J. Assessing outcomes in body contouring. Clin Plast Surg. 2014;41:645-654. [DOI] [PubMed] [Google Scholar]
- 26.Klassen AF, Cano SJ, Soldin M et al. An International Study to Develop and Validate the BODY-Q: A Patient-Reported Outcome Instrument for use in Obesity, Bariatric Treatment and Body Contouring. Plast Reconstr Surg Glob Open. 2016;1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andrich D, Sheridan B. RUMM2030. Perth, Australia: RUMM Laboratory; 1997-2011. [Google Scholar]
- 28.Rasch G. Probabilistic Models for Some Intelligence and Attainment Tests. Chicago, United States: MESA Press; 1993. [Google Scholar]
- 29.Wright BD, Masters G. Rating Scale Analysis: Rasch Measurement. Chicago, United States: MESA, 1982. [Google Scholar]
- 30.Hobart JC, Cano SJ. Improving the evaluation of therapeutic intervention in multiple sclerosis: The role of new psychometric methods. Health Technol Assess. 2009;13:1-200. [DOI] [PubMed] [Google Scholar]
- 31.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297-334. [Google Scholar]
- 32.Black N. Patient reported outcome measures could help transform healthcare. BMJ. 2013;346:167. [DOI] [PubMed] [Google Scholar]
- 33.Dey JK, Ishii M, Phillis M et al. Body dysmorphic disorder in a facial plastic and reconstructive surgery clinic: measuring prevalence, assessing comorbidities, and validating a feasible screening instrument. JAMA Facial Plastic Surg. 2015;17:137-143. [DOI] [PubMed] [Google Scholar]
- 34.Song AY, Rubin JP, Thomas V et al. Body image and quality of life in post massive weight loss body contouring patients. Obesity (Silver Spring). 2006;14:1626-1636. [DOI] [PubMed] [Google Scholar]
- 35.van der Beek ES, Te Riele W, Specken TF, Boerma D, van Ramshorst B. The impact of reconstructive procedures following bariatric surgery on patient well-being and quality of life. Obes Surg. 2010;20:36-41. [DOI] [PubMed] [Google Scholar]
- 36.Pusic AL, Klassen AF, Snell L et al. Measuring and managing patient expectations for breast reconstruction: impact on quality of life and patient satisfaction. Expert Rev Pharmacoecon Outcomes Res. 2012;12:149-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dyck BA, Zywiel MG, Mahomed A et al. Associations between patient expectations of joint arthroplasty surgery and pre- and post-operative clinical status. Expert Rev Med Devices. 2014;11:403-415. [DOI] [PubMed] [Google Scholar]
- 38.Haanstra TM, van den Berg T, Ostelo RW et al. Systematic review: Do patient expectations influence treatment outcomes in total knee and total hip arthroplasty? Health Qual Life Outcomes. 2012;10:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walijje J, McGlinn EP, Sears ED, Chung KC. Patient expectations and patient-reported outcomes in surgery: A systematic review. Surgery. 2014;155:799-808. [DOI] [PMC free article] [PubMed] [Google Scholar]