Abstract
IMPORTANCE
While urban African American adolescents face significant health disparities associated with overweight and obesity that follow them into adulthood; there is limited data on body image, emotional well-being, and weight control behaviors in this population to design effective public health interventions.
OBJECTIVE
This study was designed to understand the association of weight status to adolescent weight control, body image, and emotional well-being responses, in African American high school students.
DESIGN/SETTING/PARTICIPANTS
The study cohort consisted of 776 students, mean age 15.8 years (±1.2). Data from Guidelines for Adolescent Preventive Services (GAPS) student surveys and anthropometric studies were collected at School-Based Health Centers.
MAIN OUTCOME MEASURES
Associations between adolescent responses on the GAPS and body mass index (BMI) status (healthy weight: 5th to less than 85th percentile, overweight: 85th to less than 95th percentile, obese: 95th percentile or greater) were estimated using logistic regression and dose- response plots.
RESULTS
There were statistically significant associations between BMI category and weight control (ranging from a mean 5.18 to 7.68 odds of obesity) and body image (3.40 to 13.26 odds of obesity) responses. Responses to weight control and body image questions exhibited a dose-response for odds of overweight and obesity. Feelings of depressed mood were associated with obesity (1.47 times the odds of obesity compared to students who did not endorse depressed mood; 95% CI, 1.01 to 2.13) but not overweight status.
CONCLUSION AND RELEVANCE
Overweight and obese urban African American adolescents are more likely to screen positively on weight control risk behaviors and negative body image questions than their normal weight peers. The weight control and body image measures on the GAPS may provide information to identify youth in need of services and those motivated for brief school-based weight control interventions.
Keywords: Obesity, overweight, weight control behaviors, African American
INTRODUCTION
Obesity is a national public health concern that has reached epidemic proportions among children and adults in the United States.1–3 The prevalence of overweight children and adolescents has increased from 6.1% in 1974 to an estimated 21% in 2012, making it one of the greatest health risks facing the current generation of youth.3–6 Excess weight serves as a positive predictor for coronary heart disease, type 2 diabetes, hypertension, sleep apnea, and osteoarthritis.7,8 As such, Healthy People 2020 objectives include reduction of the proportion of children and adolescents with overweight and obesity.9 To achieve this objective, studies designed to improve screening and understanding of behaviors associated with overweight and obese status in high-risk youth are necessary.
Although the prevalence of overweight and obesity in children and adolescents has generally increased over time, African American youth face significant disparities.10–12 In a racial/ethnic comparison among girls aged 12–19 years, NHANES 2011–2012 data demonstrated that African American girls had the highest prevalence of overweight (42.5%) compared to that of white (31%) and Latino counterparts (36.5%).10 Importantly, prepubescent African American girls were not heavier than comparably aged white girls.13 By early adulthood, however, African American females were significantly heavier. This observation led researchers to believe the disparity in adiposity evolved during adolescence.14
Consequences of overweight and obese conditions extend beyond physical disorders. Several psychological disorders are associated with increased body weight, including depression and eating disorders.15–17 Although the prevalence of co-occurring obesity and psychological disorders vary by race18–20, depressive symptoms, anxiety, and eating disorders co-occur with obesity.15,18 Studies assessing the correlation between weight and poor self-concept demonstrated lower self-concept in individuals with higher body weight.16 Body dissatisfaction and depression differentially affected adolescent girls more than boys.17,20
Studies, however, suggest that African American adolescent girls were more satisfied with their bodies and less frequently engaged in dieting and disordered eating than their white female peers.21–25 The effects of obesity on poor self-esteem and depression may be buffered by increased acceptance of varied body sizes within the African American community22,24,26 and strong relationships with social networks.27 Thus, it is possible that African American adolescents’ positive body image and weight related attitudes are related to cultural norms and beliefs28 that contribute to less healthy lifestyles and decreased readiness to change behaviors. Supporting this theory, studies found that African American women underestimated their body weight and did not view themselves accurately, even if they were clinically overweight.29–31 Understanding the beliefs, attitudes, and behaviors of African American adolescents may assist in developing early and effective health promotion strategies to reduce the disparities associated with obesity.
The purpose of this study to determine the association of overweight status to emotional problems, body image dissatisfaction, and unhealthy weight related behaviors in urban African American high school students receiving care in School-Based Health Centers (SBHC). Based on the previous research, we hypothesized that overweight and obese African American adolescents will 1) show no difference in the odds of engaging in unhealthy weight control behaviors compared to their normal weight peers, 2) accept their body image compared to normal weight peers, and 3) show no difference in emotional well-being compared to normal weight peers.
METHODS
Overview
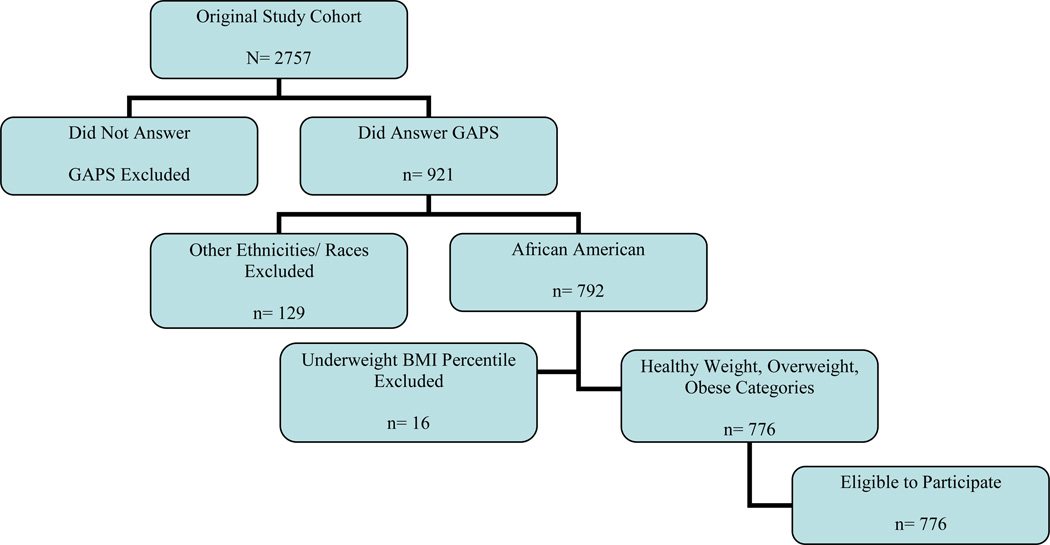
This study utilizes secondary data from a cross-sectional study 9th–12th grade Baltimore City public school students (N=2757) collected in eight comprehensive high school-based health centers (SBHCs) in the 2003–2004 academic school year. The SBHCs in Baltimore were primarily developed to serve low-income adolescents. The cohort was originally studied to estimate the prevalence of overweight and obesity in the SBHC program and to identify potential targets for intervention. Of the 2757 students from whom anthropometric data were collected, 921 also completed Guideline of Adolescent Preventive Services (GAPS) questionnaire during their SHBC clinic assessment. Of the 921, students who reported any other race/ethnicity category other than “Black or African American” were removed from the analysis as the goal of the study was to examine health behaviors and weight status in urban African American students. Students classified as “underweight” were less than 4% of the original sample and were excluded based on the study’s goal to investigate overweight and obesity and to avoid type II error. After inclusion and exclusion criteria had been met, 776 students remained in the final sample. (Figure 1). Detail of the study methods were described in an earlier publication,32 and are briefly outlined in the following text.
FIGURE 1.
Flow Chart of Student Eligibility
Setting
The Baltimore City Health Department provided comprehensive primary health services through the SBHC Program. Health risk behaviors are assessed using the American Medical Association’s Guideline for Adolescent Preventive Services (GAPS) survey. GAPS is a questionnaire that is used to assess at-risk behavior in adolescents.33 Participation in survey completion was voluntary and confidential. GAPS data were maintained as a part of an administrative dataset by the city health department. Anthropometric data was collected on each student. Students were weighed on a 400-lb capacity digital scale (Tanita Digital Professional X-TRA Capacity Scale (Model BWBsooS)) and height was obtained using a mechanical wall-mounted stadiometer (SECA Mechanical Full Telescopic Stadiometer (Model 222)).
The database used for this analysis was created by merging data from prospectively collected anthropometric measurement with GAPS data using medical record numbers as the matching variable. Body mass index (BMI) was calculated using the SAS statistical program made available from the Centers for Disease Control and Prevention. The Johns Hopkins Institutional Review Board and the Baltimore City Health Department Institutional Review Board approved this study.
Measures
The GAPS survey was administered by health care professionals to identify adolescents with health behaviors and attitudes that put them at risk for adverse health outcomes.33 Twelve questions from the 61-item GAPS questionnaire were grouped into three domains based on psychosocial behaviors and attitudes, namely (1) weight control behavior, (2) body image, and (3) emotional well-being. These three domains were the independent variables of the study. Adolescents’ (yes/no) responses to the questions were summed. Higher scores indicated poorer weight control and health behaviors. The weight control domain assessed eating behaviors and attitudes. Questions 1 and 2 were reverse scored. The body image domain questions targeted adolescents’ concerns about their body weight and shape. The emotional well-being domain questions examined adolescents’ happiness and/or satisfaction with life. Question 1 was reverse scored. (Table 1).
Table 1.
Twelve questions from the 61-item GAPS questionnaire used in the analysis grouped by domains.
| Domains | Items |
|---|---|
| Weight Control |
|
| Body Image |
|
| Emotional Well-bing |
|
The associations between these weight control, well-being, and health behaviors responses and the primary study outcome, BMIs of participants were analyzed. BMIs categories were defined based on CDC guidelines: less than the 5th percentile defined underweight, 5th percentile to less than the 85th percentile defined healthy weight, 85th percentile to less than the 95th percentile defined overweight and equal to or greater than the 95th percentile defined obese.34
Data Analysis
Descriptive statistics were calculated for demographic variables (age and gender) and the outcome and exposure variables. Exploratory bivariate logistic regression models were used to quantify the association between BMI category (healthy=0 versus overweight=1 and healthy=0 versus obese=1) and the responses to the individual GAPS questions used to create the domains. Multinomial logistic regression analyses were used to quantify the association between BMI category (overweight and obese vs. normal weight) and the responses to the questions from the GAPS survey used to create the domains. Age and gender adjusted dose response plots for the odds of obesity were estimated from logistic regression models for obesity vs. normal weight with the primary predictor being the psychosocial and behavioral domains. STATA Release 13.0 software was used to perform statistical analysis.35 Results were considered statistically significant if the p-value was at or below 0.05.
RESULTS
Selected Sample characteristics
Of the 776 students in the total sample, 466 were female (60%) and the mean age of students in the sample was 15.8 ± 1.2 years. Mean BMI was 25.8 ± 7.0 kg/m2. There were 441 normal weight students (56.8%), 146 overweight students (18.8%), and 189 obese students (24.4%). Females had 82% higher odds of being overweight (95% CI, 1.22 to 2.72). There were no differences in the odds of obesity by gender or weight category by age.
Weight Control Behaviors
Two of the four weight control behaviors were associated with BMI categories after adjusting for age and gender (Table 2). Specifically, the odds of being obese and overweight relative to normal weight among adolescents who were unhappy with their eating habits were 5.18 times (95% CI, 3.48 to 7.71) and 1.90 times (95% CI, to1.18 to 3.06) higher compared to adolescents who were satisfied with their eating habits, respectively. Students who tried to lose weight or control weight by vomiting, taking diet pills or laxatives, or starving oneself within the past year had odds for being obese relative to normal weight that were 7.68 times (95% CI, 3.94 to 14.96) greater and odds for being overweight relative to normal that were 5.88 times (95% CI, 2.88 to 12.03) greater than those of adolescents who did not use these methods to control weight. Exercise and “eats in secret” were not associated with BMI category.
Table 2.
Odds Ratios and Log Likelihood for the Associations between Weight Categories based on GAPS Responses (N=776)
| Normal Weight n (%) |
Overweight n (%) |
Obese n (%) |
||||
|---|---|---|---|---|---|---|
| Number of Participants (%) by Weight Category |
441 (56.8) | 146 (18.8) | 189 (24.4) | |||
| Frequency of Yes Responses of Normal Weight Population N (%) |
Frequency of Yes Responses of Overweight Adolescents N (%) |
*Adjusted OR for Overweight vs. Normal Weight (95% CI) P Value |
Number of Yes Respondents from Obese Adolescents N (%) |
*Adjusted OR for Obese vs. Normal Weight (95% CI) P value |
+Multinomial P value |
|
|
Weight Control Risk Behavior |
||||||
| NOT satisfied with your eating habits |
61(13.9) | 36 (24.8) | 1.90 (1.18 to 3.06) .008 |
86 (45.7) | 5.18 (3.48 to 7.71) .000 |
.0000 |
| Does NOT exercise or participate in sports activities at least three times or more each week |
153 (34.9) | 56 (38.6) | 1.04 (0.68 to 1.57) .872 |
83 (44.4) | 1.42 (0.98 to 2.05) .065 |
.0923 |
| Eats in secret | 18 (4.1) | 11 (7.6) | 2.07 (0.92 to 4.66) .078 |
12 (6.4) | 1.70(.80 to 3.63) .171 |
.2254 |
| In the past year, have tried to lose weight or control your weight vomiting, taking diet pills or laxatives, or starving yourself |
13 (3.0) | 24 (16.6) | 5.88 (2.88 to12.03) .000 |
36 (19.3) | 7.68 (3.94 to14.96) .000 |
.0000 |
|
Body Image Risk Responses |
||||||
| Spends a lot of time thinking about ways to be thin |
24 (5.5) | 38 (26.8) | 5.65 (3.21 to 9.94) .001 |
80 (43.5) | 13.26 (7.97 to 22.06) .001 |
.0000 |
| Concerns about the size or shape of your body, or your physical appearance |
91 (21.1) | 49 (34.8) | 1.96 (1.28 to 3.00) .002 |
87 (48.1) | 3.40 (2.34 to 4.95) .001 |
.0000 |
|
Emotional Well-Being Risk Responses |
||||||
| Has NOT had fun during the past 2 weeks |
68 (15.5) | 18 (12.4) | 0.73 (.42 to 1.29) .277 |
34 (18.2) | 1.19 (.76 to 1.87) .455 |
.3502 |
| Felt sad or down or as though you have nothing to look forward to during the past few weeks |
111 (25.3) | 47 (32.4) | 1.35 (.89 to 2.05) .155 |
62 (33.2) | 1.43 (0.98 to 2.08) .062 |
.0716 |
| Have seriously thought about killing yourself, made a plan or actually tried to kill yourself |
48 (10.9) | 11 (7.6) | .66 (.33 to 1.33) .248 |
22 (11.8) | 1.05 (0.61 to 1.80) .871 |
.4136 |
| There is something you often worry about or fear |
108 (24.6) | 31 (21.7) | .83 (.51 to 1.34) .435 |
47 (25.1) | 1.02 (0.69 to 1.52) .905 |
.7281 |
| Would like to get counseling about something on their mind |
38 (9.5) | 16 (12.6) | 1.24 (.66 to 2.35) .501 |
22 (12.9) | 1.37 (0.78 to 2.40) .276 |
.4031 |
| Worried about problems at home or in your family |
70 (17.1) | 27 (20.0) | 1.16 (.70 to 1.92) .554 |
38 (21.8) | 1.33 (0.85 to 2.07) .207 |
.3835 |
Logistic regression models adjusted for age and gender
Multinomial regression model for each GAP question
Body Image & Emotional Well-Being
Students who reported spending a lot of time thinking of ways to be thin had odds of being obese relative to normal that were 13.26 times (95% CI, 7.97 to 22.06) greater and had odds of being overweight relative to normal that are 5.65 times (95% CI, 3.21 to 9.94) greater compared to youth who did not endorse spending time thinking about ways to get thin. The students concerned with body, size, and physical appearance had 3.40 times (95% CI, 2.34 to 4.95) the odds of being obese relative to normal and 1.96 times (95% CI, 1.28 to 3.00) the odds of being overweight relative to normal compared to those not concerned with body appearance (Table 1). After adjusting for age and gender, none of the emotional well-being questions was related to weight status.
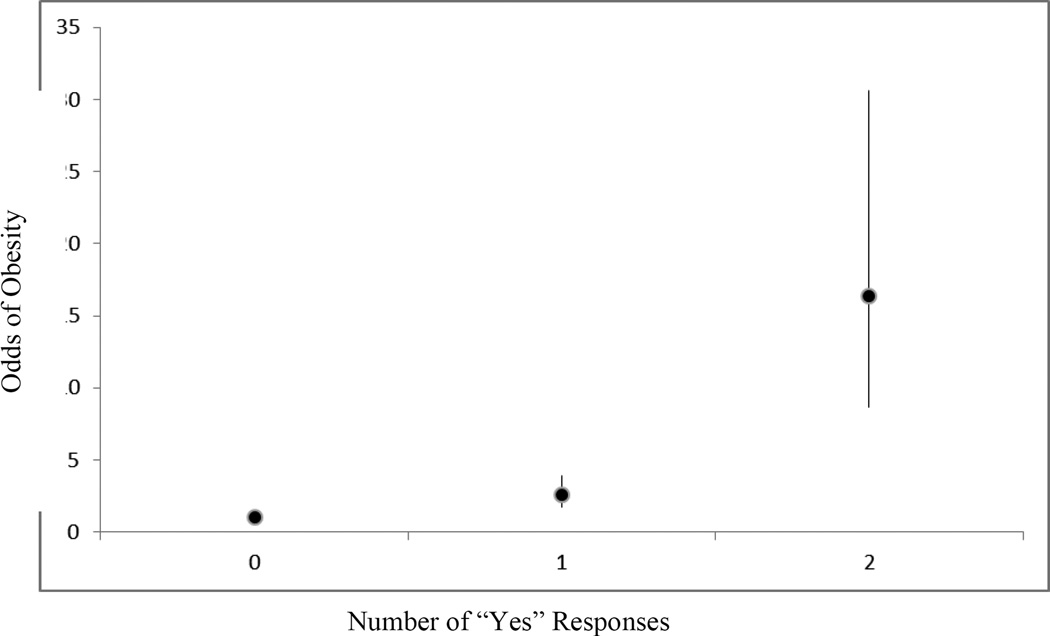
Dose Response
There was a statistically significant dose response noted for weight control behavior questions for both comparisons of overweight and obesity relative to normal weight after adjusted for age and gender. Odds for overweight did not reach significance for reporting just one weight control behavior .14 (95% CI, .74 to 1.75), but for two or more behaviors. The odds of being overweight relative to normal weight were 2.48 (95% CI, 1.40 to 4.40) and 5.02 (95% CI 1.68 to 15.00) times greater if adolescents answered “yes” to two or more of the weight control behaviors, respectively, relative to answering “no” to all of the questions. Similarly, the odds of being obese relative to normal weight ranged from 1.35 (95% CI, 0.90 to 2.02) for one “yes” response to 9.2 (95% CI, 3.47 to 24.39) for three “yes” responses to weight control questions compared to students who answered “no” (Figure 2).
Figure 2.
Dose Response to Weight Control Questions and Odds of Obesity adjusted for Age and Gender, Odds Ratios Compare the Odds of Obesity for Adolescents with 1, 2, 3 “Yes” Responses Compared to Adolescents with Zero “Yes” Responses
There was also a statistically significant dose response for the body image domain responses for overweight and obesity. Two questions were used in this domain. The odds of being overweight relative to normal weight were 1.64 (95% CI 1.02 to 2.66) times greater for students answering “yes” to one question and 6.70 (95% CI 3.34 to 13.41) time greater for students answering “yes” to two questions compared to students who answered “no”. The odds of being obese relative to normal weight were over twice (2.55; 95% CI, 1.65 to 3.94) as high for students who answered “yes” to one question and 16.40 (95% CI, 8.71 to 30.89) times higher if they answered “yes” to two of the questions in the body image domain relative to answering “no” to both questions (Figure 3). Positive responses within the emotional well-being domain did not demonstrate a statistically significant dose response curve with the odds of being overweight or obese.
Figure 3.
Dose Response to Body Image Questions and Odds of Obesity adjusted for Age and Gender, Odds Ratios Compare the Odds of Obesity for Adolescents with 1 and 2 “Yes” Responses Compared to Adolescents with Zero Responses
DISCUSSION
Prevailing evidence in the literature supports the belief that African American individuals are overall satisfied with body image regardless of weight status.22,24,29,30,36 However, this study suggests that overweight and obesity are associated with body dissatisfaction and use of unhealthy weight control behaviors in African American adolescents. Overweight and obese African American youth were more likely to screen positive on both body dissatisfaction questions on the GAPS compared to their normal weight peers. Students who spent more time thinking about ways to be thin and who had concerns about physical appearance were more likely to be overweight/ obese. This strong association with increased BMI category and concern about body size and shape contradicts the studies that support the notion that African American adolescents are accepting of larger or “thick” body types.24
Past studies have documented the racial/ethnic disparities associated with calorically dense unhealthy eating habits.21,22 A recent study by Gonsalves et. al.37 found African American, Hispanic and ‘other’ race middle school students, but not high school students, were more likely to report unhealthy weight control behaviors compared to white students. The current study, however, identifies an existing, and largely undetected problem of unhealthy dieting habits among overweight and obese African American high school students. High school students who were not satisfied with their eating habits and had attempted to lose weight through unhealthy measures were significantly more likely to be overweight and obese. Further, the more positive responses on the weight control questions, the greater the likelihood of being overweight/obese.
Even though the majority (61.6%) of students in this sample with 40% overweight/obesity prevalence reported regular exercise and there were no significant associations between students’ reports of frequency of exercise and weight classification group. Sedentary behavior is a major risk factor for the development of obesity in adolescence. Social factors such as poverty, built environment, accessibility of healthy foods, safety, and school physical education and sports team availability and policies may lead to decreased opportunities for routine exercise in urban youth.38–41
Previous studies document an association between weight status and emotional disorders, especially depression.18,20 Of the students endorsing depressive symptoms in the current study, the majority were females (67.7%). The overall rate of depressive symptoms was high in this cohort, 28.4%. Rates of suicidal ideation (10.4%) and perceived need of counseling (9.8%) were also notable for the current study population. As a comparison, in 2012 an estimated 2.2 million youth (9.1%) reported major depression within the last year.42 The prevalence of major depression for African American youth during that year was 7.9%. While the students in this study were not formally assessed for major depression, the high rate of depressive symptoms is concerning and may mask the significance of the association between depressed mood and increased odds of obesity in the adjusted model. No dose response was exhibited over the six emotional well-being questions. Lack of a demonstrated dose-response partially supports our hypothesis that there will not be an association between emotional status and BMI category in African American youth.
The false notion that African American youth are accepting of overweight and obese status may reduce health care practitioners’ willingness to intervene, leading to deleterious long-term health consequences. In a study of overweight youngsters, African American and Hispanic parents were more likely to report the quality of weight counseling they received as poor or fair compared to parents of white children.43 If not addressed within the clinical setting, poor health behaviors during adolescence may continue into adulthood; setting the stage for complications of obesity (e.g. diabetes, cancer, cardiovascular disease, stroke). Overweight status may also influence a youth’s self-concept and academic and life choices. Women who were overweight as adolescents were significantly more likely to have the poorer sociodemographic (e.g. lower income, employment status, and marriage) and self-concept outcomes (e.g. social connectedness).44
LIMITATIONS
The findings from this analysis must be considered in light of several limitations. This school based study sample included a large group of urban African American adolescents in SBHC (n=776); however, the extrapolation of results may be limited as participants’ lifestyles, socioeconomic status, and racial and cultural practices may differ from other adolescents in the United States. Importantly, findings of this study are similar to the behavioral associations found in studies of predominantly white youth. The study utilized the self-reported data from the GAPS survey.33 The GAPS survey is a clinical screening instrument, not designed to measure attitudes and behaviors for research or diagnostic purposes. Finally, the data from this sample derives from a study conducted in the 2003–2004 academic year. Unfortunately, 2013 Youth Risk Behavior Survey Data indicates that youth overweight and obesity remain suggesting the current applicability and value of these findings to city youth and public health policy design.45 Replication of this work may be useful to assess longitudinal shifts self-reported risk behaviors for more targeted intervention. Notwithstanding the aforementioned limitations, the results of the study provide important new knowledge regarding behaviors and attitudes among urban African American adolescents related to health behaviors, body image, and emotional well-being.
IMPLICATIONS
This study indicates that overweight and obese African American youth are struggling with body image and engaging in unhealthy weight control behaviors. Given national health objectives for overweight and obesity and the shift to primary care delivery in schools, SBHC providers and health policy professionals must understand of attitudes and behaviors related to body weight, image and healthy lifestyles and to intervene with youth for health promotion and behavior change. The weight control and body image measures on the GAPS may provide information to identify youth in need of services and those motivated for brief school-based weight control interventions.
Acknowledgments
This work was supported by a Faculty Development Award through the Center for Adolescent Health at Johns Hopkins Bloomberg School of Public Health, Centers for Disease Control and Prevention (CDC) Research Centers: U48/CCU309674, CDC Research Initiatives for Student Enhancement (RISE) training grant U50/CCU325127, NIH/NCMHD: L32MD000660, and the DC Baltimore Research Center on Child Health Disparities [5P20MD000198-13]. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the Baltimore City Health Department or the Centers for Disease Control and Prevention of the Department of Health and Human Services. Most importantly, the authors would like to thank the SBHC staff serving on the front lines of care public for youth in Baltimore and who assisted with data collection.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among adults: United States, 2011–2012. NCHS Data Brief. 2013(131):1–8. [PubMed] [Google Scholar]
- 2.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rudolf M, Christie D, McElhone S, et al. WATCH IT: a community based programme for obese children and adolescents. Arch. Dis. Child. 2006;91(9):736–739. doi: 10.1136/adc.2005.089896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. [Accessed 10/11/2014, 2014];Childhood Obesity Facts. 2014 http://www.cdc.gov/obesity/data/childhood.html.
- 6.Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 7.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6 Pt 1):1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 8.Sugiyama T, Xie D, Graham-Maar RC, Inoue K, Kobayashi Y, Stettler N. Dietary and lifestyle factors associated with blood pressure among U.S. adolescents. J. Adolesc. Health. 2007;40(2):166–172. doi: 10.1016/j.jadohealth.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion Healthy People 2020. [Accessed 10/10/2014, 2014];2010 http://www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status/objectives.
- 10.Ogden CL, Carroll MD, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Center for Disease Control and Prevention. CDC Health Disparities and Inequalities Report — United States, 2013. Atlanta, GA: Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 12.Office of Minority Health. Obesity and African Americans. [Accessed 9/27/2014, 2014];2013 http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlID=25.
- 13.Whitaker RC, Orzol SM. Obesity among US urban preschool children: relationships to race, ethnicity, and socioeconomic status. Arch. Pediatr. Adolesc. Med. 2006;160(6):578–584. doi: 10.1001/archpedi.160.6.578. [DOI] [PubMed] [Google Scholar]
- 14.Kimm SY, Barton BA, Obarzanek E, et al. Racial divergence in adiposity during adolescence: The NHLBI Growth and Health Study. Pediatrics. 2001;107(3):E34. doi: 10.1542/peds.107.3.e34. [DOI] [PubMed] [Google Scholar]
- 15.Herget S, Rudolph A, Hilbert A, Bluher S. Psychosocial Status and Mental Health in Adolescents before and after Bariatric Surgery: A Systematic Literature Review. Obesity Facts. 2014;7(4):233–245. doi: 10.1159/000365793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ali MM, Minor T, Amialchuk A. Estimating the biases associated with self-perceived, self-reported, and measured BMI on mental health. PloS One. 2013;8(12):e81021. doi: 10.1371/journal.pone.0081021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Witherspoon D, Latta L, Wang Y, Black MM. Do depression, self-esteem, body-esteem, and eating attitudes vary by BMI among African American adolescents? J Pediatr Psychol. 2013;38(10):1112–1120. doi: 10.1093/jpepsy/jst055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lincoln KD, Abdou CM, Lloyd D. Race and socioeconomic differences in obesity and depression among Black and non-Hispanic White Americans. J Health Care Poor Underserved. 2014;25(1):257–275. doi: 10.1353/hpu.2014.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell-Young YM, Zabaleta J, Velasco-Gonzalez C, Sothern MS. A cohort study evaluating the implications of biology, weight status and socioeconomic level on global self-esteem competence among female African-American adolescents. JNBNA. 2013;24(1):1–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Whaley AL, Smith M, Hancock A. Ethnic/racial differences in the self-reported physical and mental health correlates of adolescent obesity. Journal of Health Psychology. 2011;16(7):1048–1057. doi: 10.1177/1359105311398683. [DOI] [PubMed] [Google Scholar]
- 21.Thompson SH, Rafiroiu AC, Sargent RG. Examining gender, racial, and age differences in weight concern among third, fifth, eighth, and eleventh graders. Eat Behav. 2003;3(4):307–323. doi: 10.1016/s1471-0153(02)00093-4. [DOI] [PubMed] [Google Scholar]
- 22.Gluck M, Geliebter A. Racial/ethnic differences in body image and eating behaviors. Eating Behaviors. 2002;3:143–151. doi: 10.1016/s1471-0153(01)00052-6. [DOI] [PubMed] [Google Scholar]
- 23.Neumark-Sztainer D, Croll J, Story M, Hannan PJ, French SA, Perry C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: findings from Project EAT. Journal of psychosomatic research. 2002;53(5):963–974. doi: 10.1016/s0022-3999(02)00486-5. [DOI] [PubMed] [Google Scholar]
- 24.Franko DL, Striegel-Moore RH. The role of body dissatisfaction as a risk factor for depression in adolescent girls: are the differences Black and White? J. Psychosom. Res. 2002;53(5):975–983. doi: 10.1016/s0022-3999(02)00490-7. [DOI] [PubMed] [Google Scholar]
- 25.Field AE, Aneja P, Austin SB, Shrier LA, de Moor C, Gordon-Larsen P. Race and gender differences in the association of dieting and gains in BMI among young adults. Obesity. 2007;15(2):456–464. doi: 10.1038/oby.2007.560. [DOI] [PubMed] [Google Scholar]
- 26.Botta RA. The Mirror of Television: A Comparison of Black and White Adolescents’ Body Image. Journal of Communication. 2000;50(3):144. [Google Scholar]
- 27.Slater JM, Guthrie BJ, Boyd CJ. A feminist theoretical approach to understanding health of adolescent females. J. Adolesc. Health. 2001;28(6):443–449. doi: 10.1016/s1054-139x(00)00207-x. [DOI] [PubMed] [Google Scholar]
- 28.Johnson-Askew WL, Fisher R, Henderson K, Schwartz M. Attitudes of African American advocates toward childhood obesity. Ethnicity & Disease. 2011;21(3):268–273. [PubMed] [Google Scholar]
- 29.Flynn KJ, Fitzgibbon M. Body images and obesity risk among black females: a review of the literature. Ann. Behav. Med. 1998;20(1):13–24. doi: 10.1007/BF02893804. 1998. [DOI] [PubMed] [Google Scholar]
- 30.Sivalingam SK, Ashraf J, Vallurupalli N, Friderici J, Cook J, Rothberg MB. Ethnic differences in the self-recognition of obesity and obesity-related comorbidities: a cross-sectional analysis. Journal of general internal medicine. 2011;26(6):616–620. doi: 10.1007/s11606-010-1623-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fan M, Jin Y, Khubchandani J. Overweight Misperception among Adolescents in the United States. Journal of Pediatr Nurs. 2014 doi: 10.1016/j.pedn.2014.07.009. pii So882-5963(14)00204-8. [DOI] [PubMed] [Google Scholar]
- 32.Trent M, Jennings JM, Waterfield G, Lyman LM, Thomas H. Finding targets for obesity intervention in urban communities: school-based health centers and the interface with affected youth. J. Urban. Health. 2009;86(4):571–583. doi: 10.1007/s11524-009-9355-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klein JD, Slap GB, Elster AB, Cohn SE. Adolescents and access to health care. Bull. N. Y. Acad. Med. 1993;70(3):219–235. [PMC free article] [PubMed] [Google Scholar]
- 34.Nihiser AJ, Lee SM, Wechsler H, et al. Body mass index measurement in schools. J. Sch Health. 2007;77(10):651–671. doi: 10.1111/j.1746-1561.2007.00249.x. [DOI] [PubMed] [Google Scholar]
- 35.Stata Intercooled: Release 13 [computer program] College Station, TX: 2013. [Google Scholar]
- 36.Edwards NM, Pettingell S, Borowsky IW. Where perception meets reality: self-perception of weight in overweight adolescents. Pediatrics. 2010;125(3):e452–e458. doi: 10.1542/peds.2009-0185. [DOI] [PubMed] [Google Scholar]
- 37.Gonsalves D, Hawk H, Goodenow C. Unhealthy weight control behaviors and related risk factors in massachusetts middle and high school students. Maternal and Child Health J. 2014;18(8):1803–1813. doi: 10.1007/s10995-013-1424-5. [DOI] [PubMed] [Google Scholar]
- 38.Li F, Harmer P, Cardinal BJ, Bosworth M, Johnson-Shelton D. Obesity and the built environment: does the density of neighborhood fast-food outlets matter? American J Health Promot. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Owen N, Leslie E, Salmon J, Fotheringham MJ. Environmental determinants of physical activity and sedentary behavior. Exerc. Sport Sci. Rev. 2000;28(4):153–158. 10/2000. [PubMed] [Google Scholar]
- 40.Gomez JE, Johnson BA, Selva M, Sallis JF. Violent crime and outdoor physical activity among inner-city youth. Prev. Med. 2004;39(5):876–881. doi: 10.1016/j.ypmed.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 41.Whitaker D, Milam AJ, Graham CM, Cooley-Strickland M, Belcher HM, Furr-Holden CD. Neighborhood environment and urban schoolchildren's risk for being overweight. American Journal of Health Promot. 2013;27(6):410–416. doi: 10.4278/ajhp.100827-QUAN-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 43.Taveras EM, Gortmaker SL, Mitchell KF, Gillman MW. Parental perceptions of overweight counseling in primary care: the roles of race/ethnicity and parent overweight. Obesity. 2008;16(8):1794–1801. doi: 10.1038/oby.2008.264. [DOI] [PubMed] [Google Scholar]
- 44.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N. Engl. J. Med. 1993;329(14):1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 45.National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Division for Adolescent and School Health. [Accessed, 1/4/15]; Youth Online, http://www.cdc.gov/nchhstp/
- 46.Obama M. Let's Move. [Accessed 10/22/2014, 2014];2010 http://www.letsmove.gov/