Abstract
Objective
Although the global burden of HIV infection among sex workers (SW) has been well recognized, HIV-related risks among sex workers who inject drugs (SW-IDU) have received less attention. We investigated the relationship between sex work and HIV incidence among people who inject drugs (IDU) in a Canadian setting.
Design
Prospective cohort study.
Methods
Using Kaplan–Meier methods and the extended Cox regression, we compared HIV incidence among SW-IDU and non-SW-IDU in Vancouver, Canada, after adjusting for potential confounders.
Results
Between 1996 and 2012, 1647 participants were included in the study, including 512 (31.1%) IDU engaged in sex work. At 5 years the HIV cumulative incidence was higher among SW-IDU in comparison to other IDU (12 vs. 7%, P = 0.001). In unadjusted Cox regression analyses, HIV incidence among SW-IDU was also elevated [relative hazard: 1.69; 95% confidence interval (CI): 1.13–2.53]. However, in a multivariable analysis, sex work did not remain associated with HIV infection (adjusted relative hazard: 0.74; 95% CI: 0.45–1.20), with cocaine injection appearing to account for the elevated risk for HIV infection among SW-IDU.
Conclusion
These data suggest that local SW-IDU have elevated rates of HIV infection. However, our exploration of risk factors among SW-IDU demonstrated that drug use patterns and environmental factors, rather than sexual risks, may explain the elevated HIV incidence among SW-IDU locally. Our findings highlight the need for social and structural interventions, including increased access to harm reduction programs and addiction treatment.
Keywords: HIV, injection drug use, sex work
INTRODUCTION
HIV infection remains high among sex workers (SW) in various settings [1,2], and has been attributed to social, structural and biological conditions shaping sexual risk pathways with client and noncommercial partners [3,4]. Sex work is also prevalent among other populations at risk for HIV infection, including men who have sex with men and people who inject drugs (IDU) [5,6]. Sex workers who inject drugs (SW-IDU) face elevated risk of HIV acquisition through dual sexual and drug risk pathways [6–8]: practices often arising from or amplified by various social-structural forces, including violence, engagement in street-based economies and the criminalization of SW and IDU [1,9]. Given these challenges, new HIV infections among SW-IDU can be critical within generalized HIV epidemics [9,10].
The extent of overlap between IDU and SW populations can be significant, with the proportion of SW among IDU ranging from 14 to 80% across diverse settings [10–14]. Further, it is known that many IDU resort to high-risk income-generating activities, including drug dealing and exchange of sex for drugs, to acquire funds for basic survival and drug use [15]. These activities can elevate risk for infectious disease acquisition[7], violence [15], and high-intensity drug use [15]. Street-based SW often engage in drug use as a means of coping with the stress of sex work [7,16], and drug use with clients is also common [17] and known to increase risk for violence as well as sex- and drug-related risk behaviour [17,18]. Drug-related harm experienced by SW who use drugs has also been found to reflect low access to harm reduction and other HIV prevention programs as a result of displacement due to policing activities [19].
Despite the exceptional risks experienced by SW-IDU [8], there is limited HIV incidence data specific to this population and few studies have examined whether SW-IDU remain at elevated HIV risk, after adjusting for a range of drug and sexual risks, as well as contextual factors. Therefore, taking advantage of a longstanding community-recruited cohort of HIV-negative IDU, we sought to characterize HIV incidence among SW-IDU in Vancouver. Although a 2003 study from Vancouver identified that sex work did not predict HIV incidence among local IDU [20], Vancouver has since implemented a range of policy and programmatic changes specific to drug use and sex work. Further, unlike this past work, the present study seeks to explore how the relationship between sex work and HIV incidence may be confounded by individual and contextual factors.
METHODS
The Vancouver Injection Drug Users Study (VIDUS) is an open prospective cohort of HIV-negative IDU recruited through snowball sampling and street-based outreach methods in the Downtown Eastside (DTES) of Vancouver starting in May 1996, and has been described previously [21]. Briefly, individuals were eligible for the VIDUS project if they had injected illicit drugs at least once in the previous month, were aged 18 years or older, and resided in greater Vancouver. At baseline and semi-annually thereafter, subjects gave blood samples for HIV serology and completed an interviewer-administered questionnaire. The questionnaire captures demographic data in addition to information regarding drug use, HIV risk behaviour, sex work involvement, and addiction treatment exposures occurring in the previous six months. Sex work was defined as exchanging sex for money, gifts, shelter, or anything else in the past six months and was treated as a time-updated variable. All participants provided informed consent and were given a stipend ($20 CDN) at each study visit to compensate for their time. This study has been approved by the University of British Columbia/Providence Healthcare Research Ethics Board. For the present analyses, participants were eligible if they were recruited between 1 May 1996 and 30 November 2012, and have had at least one follow-up visit.
The present study was conducted to examine the association between sex work involvement and the rate of HIV seroconversion. An a priori defined statistical protocol was developed based on previous findings from the VIDUS study [21]. This protocol involved the following steps.
Kaplan–Meier analyses
Based on an earlier analysis from our setting [20], the primary risk factor for HIV infection among Vancouver IDU was the daily injection of cocaine. Further, we know from other studies in North America that risks among SW-IDU are often driven by risk pathways associated with cocaine injection [22–24]. It was therefore hypothesized that, if an elevated HIV incidence was observed among SW-IDU, high-intensity cocaine use could be associated with sex work, and that if this hypothesis was supported, the higher proportion of daily cocaine injectors among those engaged in sex work might partially confound the association between sex work and HIV incidence. Therefore, the cumulative HIV incidence among SW-IDU and IDU not involved in sex work at baseline was plotted, and this pattern was compared with the cumulative HIV incidence among those that did and did not report daily cocaine injection at baseline. In an effort to disentangle the potentially confounding effect of daily cocaine injection, the association between sex work and HIV incidence was then examined while stratifying the cohort into those that reported daily cocaine injection and those that did not report daily cocaine injection at baseline. Survival curves were compared using the log-rank test.
As previously [21], the date of seroconversion was estimated using the midpoint between the last negative and the first positive antibody test result. Time zero was defined as the date of enrolment into the study, and participants who remained persistently seronegative were right censored at the time of their most recent interview date prior to 30 May 2013.
Multivariable analyses
As the above approach did not account for changes in behaviours over time, as well as other possible confounders, the unadjusted and adjusted relative hazards of HIV seroconversion were calculated using the extended Cox model. Demographic and drug use variables considered as potential confounders included sex, age (per 10 year increase), aboriginal ancestry (yes vs. no), residency in DTES, recent incarceration (yes vs. no), any unprotected vaginal or anal intercourse (yes vs. no), syringe borrowing (yes vs. no), daily crack smoking (yes vs. no), daily cocaine injecting (yes, vs. no), daily heroin injecting (yes vs. no), requiring help injecting (yes vs. no), and current enrolment in methadone maintenance treatment (yes vs. no). Unless otherwise noted, all behavioural variables, including sex work, were treated as time-updated covariates based on semi-annual follow-up data.
An a priori defined modelling approach was applied where it was examined how the unadjusted relative hazard of HIV infection among IDU was altered by adjustment for daily cocaine injection, and then further altered by the subsequent inclusion of residence in the drug and sex work epicentre (DTES vs. other). This second potential confounder was selected based on the findings of earlier studies [25,26], and the a prioriassumption that residence in this area would be strongly associated with street-based sex work engagement.
As some confounders could potentially mask an association between sex work and HIV, a fixed model was built that adjusted for all variables described above that were associated with the time to HIV seroconversion in unadjusted analyses at P less than 0.05. Finally, we conducted a subanalysis in which we re-ran our final multivariate model restricted to female participants. Analyses were conducted using SAS 9.3 (Cary, North Carolina, USA) and the threshold for statistical significance was set at P less than 0.05. All P values were two sided.
RESULTS
Between May 1996 and December 2012, 1647 HIV-negative participants were enrolled and completed at least one follow-up. In comparison to the participants who did not return for follow-up, those included in the study sample were more likely to be older at baseline (median age: 36 years vs. 32 years, P < 0.001) and less likely to engage in unprotected sex (37 vs. 45%, P = 0.025). There were no differences with respect to engagement in sex work (P > 0.05).
Analysis of baseline characteristics
As indicated in Table 1, in comparison to those not involved in sex work (n = 1277; 78%), SW-IDU (n = 370; 22%) were more likely to be younger, female, of aboriginal ancestry, to have had unprotected sex, smoke crack daily, inject cocaine and heroin daily, and need help injecting (all P < 0.001). SW-IDU were also less likely to be enrolled in methadone maintenance treatment (P = 0.012). At baseline, SW-IDU and IDU not involved in sex work were similar with respect to all other variables noted above (all P > 0.05).
Table 1.
Baseline characteristics of our study sample, stratified by sex work (n = 1647).
| Sex worka | ||||
|---|---|---|---|---|
| Characteristic | Total (%) (n = 1647) | Yes (%) (n = 370) | No (%) (n = 1277) | P value |
| Age per 10 years (med, IQR) | 3.6 (2.8–4.2) | 2.8 (2.3–3.7) | 3.8 (3.1–4.4) | <0.001 |
| Male sex | 1098 (66.7) | 75 (20.3) | 1032 (80.1) | <0.001 |
| Aboriginal ancestry | 450 (27.3) | 157 (42.4) | 293 (22.9) | <0.001 |
| DTES residencea | 1036 (62.9) | 242 (65.4) | 794 (62.2) | 0.258 |
| Incarcerationa | 223 (13.5) | 52 (14.1) | 171 (13.4) | 0.743 |
| Unprotected sexa,b | 614 (37.3) | 173 (46.8) | 441 (34.5) | <0.001 |
| Syringe borrowinga | 474 (28.8) | 119 (32.2) | 355 (27.8) | 0.103 |
| Daily crack smokinga | 392 (23.8) | 133 (36.0) | 259 (20.3) | <0.001 |
| Daily cocaine injectiona | 500 (30.4) | 152 (41.1) | 348 (27.3) | <0.001 |
| Daily heroin injectiona | 722 (43.8) | 200 (54.1) | 522 (40.9) | <0.001 |
| Need help injectinga | 590 (35.8) | 181 (48.9) | 409 (32.0) | <0.001 |
| Current enrolment in MMT | 334 (20.3) | 58 (15.7) | 276 (21.6) | 0.012 |
DTES, Downtown Eastside neighbourhood; IQR, interquartile range; MMT, methadone maintenance therapy.
Activities/behaviours in the previous 6 months.
Any unprotected vaginal or anal intercourse.
Kaplan–Meier analyses
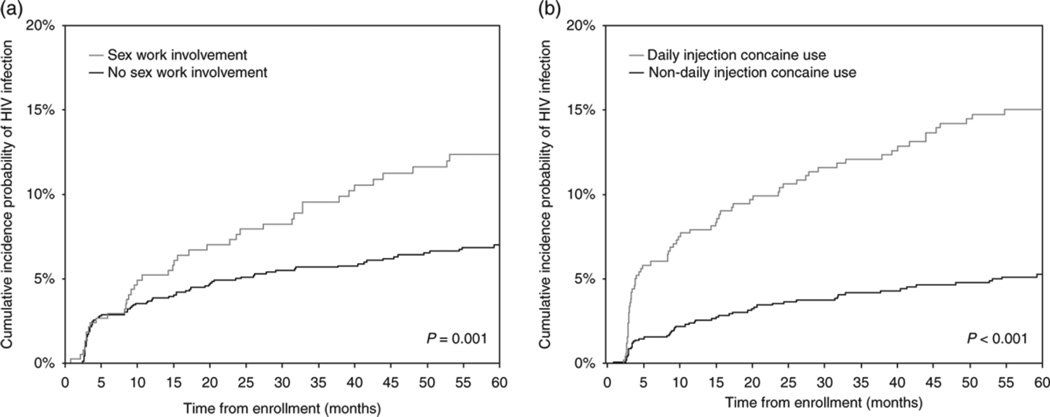
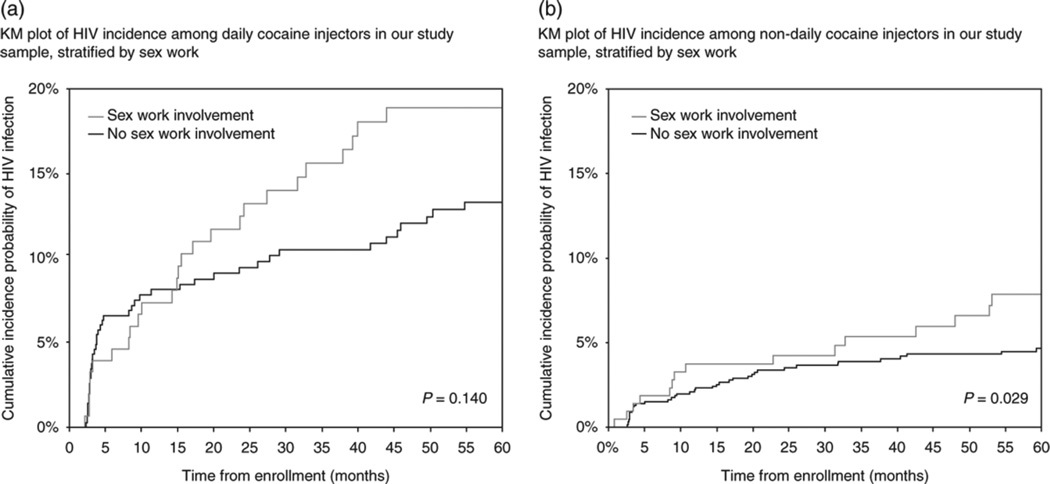
As of 30 May 2013, 138 (8.38%) of 1647 participants had become HIV-infected. As shown in Fig. 1, at 60 months after recruitment into the study, the Kaplan–Meier cumulative HIV incidence was 12.36% [95% confidence interval (CI): 9.23–16.46] among SW-IDU at baseline, compared with 7.00% (95% CI: 5.66–8.64) among IDU not involved in sex work at baseline (Fig. 1, panel a; log-rank P = 0.001). This can be compared with the cumulative HIV incidence of 15.02% (95% CI: 12.01–18.71) among those who reported daily cocaine injection at baseline and 5.27% (95% CI: 4.05–6.84) among those who did not report daily cocaine injection at baseline (Fig. 1, panel b; log-rank P < 0.001). When we restricted analyses to the 500 individuals who reported daily cocaine injection at baseline, the cumulative incidence was 18.89% (95% CI: 13.24–26.56) among SW-IDU at baseline, compared with 13.31% (95% CI: 9.97–17.64) among IDU not engaged in sex work at baseline (Fig. 2, panel a; log-rank P = 0.140). Similarly, among the 1147 individuals who did not report daily cocaine injection at baseline, the cumulative incidence was 7.85% (95% CI: 4.78–12.74) among SW-IDU at baseline, compared with 4.65% (95% CI: 3.41–6.33) among IDU not engaged in sex work at baseline (Fig. 2, panel b; log-rank P = 0.029).
Figure 1.
Kaplan–Meier analyses of time to HIV infection stratified by sex work and cocaine injection (n = 1647).
Figure 2.
Kaplan–Meier analyses of time to HIV infection stratified by sex work among daily cocaine injectors (n = 500) and non-daily cocaine injectors (n = 1147).
Multivariable analyses
Table 2 shows the unadjusted relative hazards for risk factors positively and significantly associated with HIV seroconversion, which included sex work, younger age, female sex, aboriginal ancestry, DTES residency, recent incarceration, syringe borrowing, daily cocaine injecting, daily heroin injecting and requiring help injecting (all P < 0.05). Enrolment in methadone maintenance treatment was negatively associated with HIV seroconversion (P < 0.001).
Table 2.
Univariable and multivariable extended Cox regression analyses of factors associated with HIV incidence among our study sample (n = 1647).
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Characteristic | Relative hazard (95% Cl) | P value | Relative hazard (95% Cl) | P value |
| Sex worka | ||||
| (yes vs. no) | 1.69 (1.13–2.53) | 0.010 | 0.74 (0.45–1.20) | 0.221 |
| Age | ||||
| (per 10 year increase) | 0.71 (0.61–0.83) | <0.001 | 0.77 (0.64–0.92) | 0.005 |
| Sex | ||||
| (male vs. female) | 0.57 (0.41–0.80) | 0.001 | 0.73 (0.48–1.12) | 0.148 |
| Aboriginal ancestry | ||||
| (yes vs. no) | 2.06 (1.47–2.88) | <0.001 | 1.59 (1.12–2.27) | 0.010 |
| DTES residencea | ||||
| (yes vs. no) | 3.18 (2.01–5.01) | <0.001 | 2.81 (1.78–4.43) | <0.001 |
| Incarcerationa | ||||
| (yes vs. no) | 1.64 (1.15– 2.35) | 0.007 | 1.18 (0.80–1.73) | 0.400 |
| Unprotected sexa,b | ||||
| (yes vs. no) | 1.22 (0.85–1.74) | 0.279 | ||
| Syringe borrowinga | ||||
| (yes vs. no) | 1.99 (1.38–2.87) | <0.001 | 1.65 (1.12–2.43) | 0.011 |
| Daily crack smokinga | ||||
| (yes vs. no) | 1.10 (0.76–1.59) | 0.603 | ||
| Daily cocaine injectinga | ||||
| (yes vs. no) | 4.33 (3.05–6.15) | <0.001 | 3.17 (2.20–4.56) | <0.001 |
| Daily heroin injectinga | ||||
| (yes vs. no) | 1.91 (1.36–2.70) | <0.001 | 1.06 (0.73–1.53) | 0.761 |
| Need help injectinga | ||||
| (yes vs. no) | 2.30 (1.61–3.30) | <0.001 | 1.58 (1.07–2.32) | 0.021 |
| Current enrolment in MMT | ||||
| (yes vs. no) | 0.50 (0.33–0.75) | 0.001 | 0.67 (0.44–1.03) | 0.066 |
CI, confidence interval; DTES, Downtown Eastside neighbourhood; MMT, methadone maintenance therapy.
Activities/behaviours in the previous 6 months.
Any unprotected vaginal or anal intercourse.
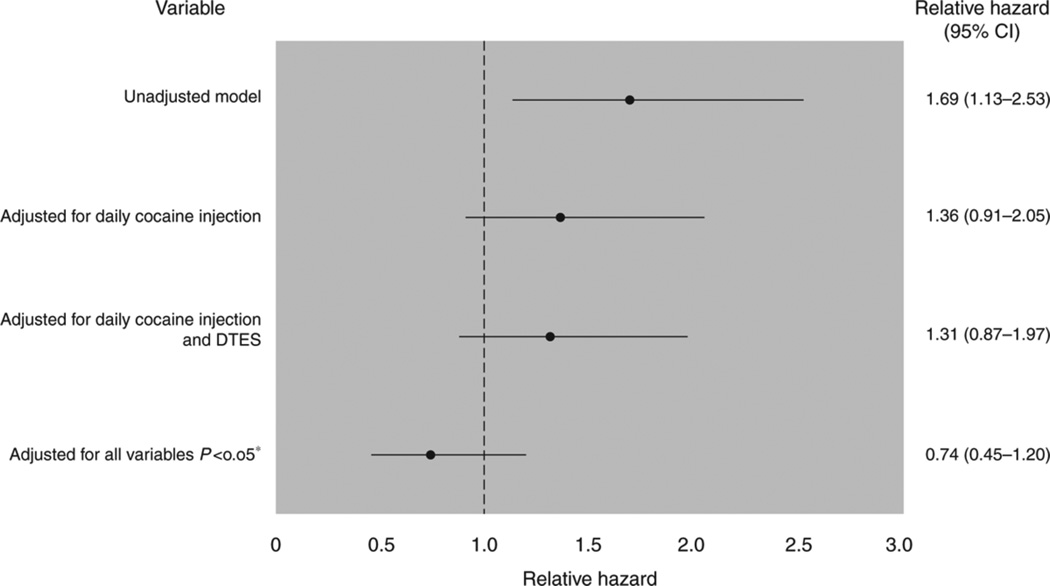
Figure 3 also shows the results of the extended Cox regression analysis of the time to HIV infection by sex work status after the stepwise inclusion of potential confounders. In unadjusted analyses, the relative hazard of HIV seroconversion for SW-IDU was 1.69 (95% CI: 1.13–2.53). After adjustment for daily cocaine injection, the relative hazard changed to 1.36 (95% CI: 0.91–2.05;P = 0.137); after further adjustment for DTES residency, the relative hazard changed to 1.31 (95% CI: 0.87–1.97; P = 0.191). After adjustment for variables associated with HIV seroconversion at the P < 0.05 level in unadjusted analyses, the relative hazard of HIV seroconversion for SW-IDU was 0.74 (95% CI: 0.45–1.20; P = 0.221). When we restricted our sample to female IDU, our results were largely unchanged (data not shown), with sex work failing to retain an independent association with HIV incidence (adjusted relative hazard = 0.75, 95% CI: 0.43–1.30, P = 0.296).
Figure 3.
Relative hazards and 95% confidence intervals for HIV infection associated with sex work after the stepwise inclusion of potential confounders.
DTES, Downtown Eastside neighbourhood
*Adjusted for all variables associated with the time to HIV infection at P < 0.05 in unadjusted analyses.
DISCUSSION
We found strong associations between baseline engagement in sex work, baseline daily cocaine injection and subsequent HIV seroconversion among our cohort of IDU. However, when the cohort was stratified into those who did and did not report daily cocaine use at baseline, the association between sex work and HIV incidence appeared to be partially explained by the higher rate of daily cocaine injection among SW-IDU. Further, when sex work was treated as a time-updated variable, the relationship between sex work and HIV seroconversion was significant in the unadjusted analysis. However, after adjustment for a range of other known risks for seroconversion, the relationship between sex work and HIV seroconversion was no longer significant, suggesting that in addition to daily cocaine injection, other contextual factors (rather than sex work itself) are operating within the broader risk environment of SW-IDU to shape risk of HIV infection.
Our findings are consistent with a study assessing HIV prevalence among SW-IDU in the United Kingdom [27], which found that rates of HIV infection did not differ among those IDU who were and were not engaged in sex work. Further, past work has suggested that cocaine injection may drive dual parenteral and sexual risk pathways among SW-IDU (e.g. anonymous sexual exchanges, drug sharing with clients, sex for drug exchanges, pressure for unprotected sex) [28]. However, to our knowledge, our study is among only a very small number of studies to model HIV incidence among SW-IDU and non-SW-IDU [22].
In the current environment of drug prohibition, drugs are sold at inflated prices, and given that drug users are typically marginalized from mainstream employment opportunities [29], many turn to alternative, informal economic opportunities within drug scenes to acquire money for drugs and necessities of daily living [15]. A growing body of literature has pointed to the role that such alternative income-generating activities play in shaping health-related harms among IDU, including among IDU within street-based sex work scenes [8,9,15]. Indeed, the elevated burden of HIV among street-based SW-IDU in North America and other higher income settings has been largely attributed to the social and structural conditions surrounding sex work, including criminalized laws and punitive approaches targeting sex work [1,30].
Our findings suggest that, for SW-IDU in this setting, high rates of daily cocaine injecting may explain much of the risk for HIV infection experienced by this population. This finding is consistent with another study involving SW in this setting [31], as well as recent work showing that IDU engaged in sex work were more likely to share syringes than IDU not engaged in sex work [27]. Given the short half-life of cocaine, many IDU inject cocaine numerous times a day, and high-intensity cocaine injection has been shown to be associated with HIV incidence in this setting [20]. The relationship between cocaine use and sex work is complex, as past research has indicated that stimulant use can serve an adaptive function by helping SW-IDU stay awake and alert through nighttime working hours, by enhancing sexual performance, and by offsetting the stress arising from undertaking sex work in environments where drug use and aspects of sex work are criminalized [7,16]. Further, drug use among SW-IDU may be particularly risky, given the known harms arising from drug sharing with clients, including violence, sex- and drug use-related risks [17,32], as well as the fact that in comparison to SW who do not inject drugs, SW-IDU are more likely to have partners who are IDU[9,33]. Future studies should seek to identify the factors that predict incident HIV infection among SW-IDU, and given past research from Mexico pointing to the role that injecting with clients and police confiscation of syringes play in shaping HIV risk among SW-IDU [18], future studies should assess a range of potential social, structural and environmental drivers of HIV infection.
Recent research has pointed to the potential benefit of altering the risk environment of SW-IDU to prevent HIV infection in this uniquely vulnerable population, including through structural reform to existing laws and policies that exacerbate risk for HIV infection, violence, and high-risk drug use [30,34–36]. A recent modelling paper revealed that decriminalizing sex work could serve to avert 33–46% of HIV infections within a decade [1]. Further, given the lack of effective treatments for cocaine dependence [37], there is an urgent need to develop novel treatments for cocaine users.
Our study has limitations. First, our study was observational in nature, and this limits our ability to infer causation. Second, a potential for residual confounding comes from the fact that data on risk behaviours, such as the frequency of cocaine injection and unprotected sex, can never be precisely ascertained in observational studies. Third, there are undoubtedly additional unmeasured risk factors, such as social network characteristics, which are typically more elaborate among SW-IDU in comparison to IDU not engaged in sex work [8,9]. Fourth, as with other community-recruited cohort studies, our sample was not randomly selected and may not be representative of other IDU and SW. Finally, we made use of self-reported data, which may be vulnerable to response biases. However, it should be noted that our outcome of interest, HIV infection, was derived from laboratory assays.
In summary, we found that SW-IDU are highly vulnerable to HIV acquisition. However, our analysis revealed that sex work engagement did not retain its independent association with HIV incidence among IDU after covariate adjustment, suggesting that it is individual drug use patterns and factors operating within the broader risk environment that shape the risk of HIV acquisition among SW-IDU. Our findings highlight the need for social and structural interventions, including increased access to harm reduction programs and addiction treatment.
Acknowledgments
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff. The study was supported by the US National Institutes of Health (VIDUS: R01DA011591, U01DA038886). This research was undertaken, in part, thanks to funding for a Tier 1 Canada Research Chair in Inner City Medicine, which supports E.W., and a Tier 2 Canada Research Chair in Global Sexual Health and HIV/AIDS, which supports K.S. K.H. and L.T. are supported by the Canadian Institutes of Health Research. J.M. is supported with grants paid to his institution by the British Columbia Ministry of Health and by the US National Institutes of Health (R01DA036307). He has also received limited unrestricted funding, paid to his institution, from Abbvie, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck, and ViiV Healthcare.
Footnotes
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shannon K, Strathdee SA, Goldenberg SM, Duff P, Mwangi P, Rusakova M, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet. 2015;385:55–71. doi: 10.1016/S0140-6736(14)60931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:538–549. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- 3.Morris M, Podhisita C, Wawer MJ, Handcock MS. Bridge populations in the spread of HIV/AIDS in Thailand. AIDS. 1996;10:1265–1271. doi: 10.1097/00002030-199609000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Graham SM, Raboud J, Jaoko W, Mandaliya K, McClelland RS, Bayoumi AM. Changes in sexual risk behavior in the Mombasa cohort: 1993–2007. PLoS One. 2014;9:e113543. doi: 10.1371/journal.pone.0113543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oldenburg CE, Perez-Brumer AG, Reisner SL, Mimiaga MJ. Transactional sex and the HIV epidemic among men who have sex with men (MSM): results from a systematic review and meta-analysis. AIDS Behav. 2015;19:2177–2183. doi: 10.1007/s10461-015-1010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strathdee SA, Abramovitz D, Lozada R, Martinez G, Rangel MG, Vera A, et al. Reductions in HIV/STI incidence and sharing of injection equipment among female sex workers who inject drugs: results from a randomized controlled trial. PLoS One. 2013;8:e65812. doi: 10.1371/journal.pone.0065812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patterson TL, Semple SJ, Fraga M, Bucardo J, de la Torre A, Salazar J, et al. Comparison of sexual and drug use behaviors between female sex workers in Tijuana and Ciudad Juarez, Mexico. Subst Use Misuse. 2006;41:1535–1549. doi: 10.1080/10826080600847852. [DOI] [PubMed] [Google Scholar]
- 8.El-Bassel N, Wechsberg WM, Shaw SA. Dual HIV risk and vulnerabilities among women who use or inject drugs: no single prevention strategy is the answer. Curr Opin HIV AIDS. 2012;7:326–331. doi: 10.1097/COH.0b013e3283536ab2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, et al. Correlates of injection drug use among female sex workers in two Mexico-U.S. border cities. Drug Alcohol Depend. 2008;92:132–140. doi: 10.1016/j.drugalcdep.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gu J, Bai Y, Lau JT, Hao Y, Cheng Y, Zhou R, et al. Social environmental factors and condom use among female injection drug users who are sex workers in China. AIDS Behav. 2014;(18 Suppl 2):S181–S191. doi: 10.1007/s10461-013-0434-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roy E, Richer I, Morissette C, Leclerc P, Parent R, Claessens C, et al. Temporal changes in risk factors associated with HIV seroconversion among injection drug users in eastern central Canada. AIDS. 2011;25:1897–1903. doi: 10.1097/QAD.0b013e32834ad6bb. [DOI] [PubMed] [Google Scholar]
- 12.Couture MC, Evans JL, Sothy NS, Stein ES, Sichan K, Maher L, et al. Correlates of amphetamine-type stimulant use and associations with HIV-related risks among young women engaged in sex work in Phnom Penh, Cambodia. Drug Alcohol Depend. 2012;120:119–126. doi: 10.1016/j.drugalcdep.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sosa-Estani S, Rossi D, Weissenbacher M. Epidemiology of human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome in injection drug users in Argentina: high seroprevalence of HIV infection. Clin Infect Dis. 2003;37(suppl 5):S338–S342. doi: 10.1086/377556. [DOI] [PubMed] [Google Scholar]
- 14.Platt L, Rhodes T, Judd A, Koshkina E, Maksimova S, Latishevskaya N, et al. Effects of sex work on the prevalence of syphilis among injection drug users in 3 Russian cities. Am J Public Health. 2007;97:478–485. doi: 10.2105/AJPH.2005.069732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeBeck K, Shannon K, Wood E, Li K, Montaner J, Kerr T. Income generating activities of people who inject drugs. Drug Alcohol Depend. 2007;91:50–56. doi: 10.1016/j.drugalcdep.2007.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cruz MF, Mantsios A, Ramos R, Case P, Brouwer KC, Ramos ME, et al. A qualitative exploration of gender in the context of injection drug use in two US-Mexico border cities. AIDS Behav. 2007;11:253–262. doi: 10.1007/s10461-006-9148-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shannon K, Kerr T, Bright V, Gibson K, Tyndall MW. Drug sharing with clients as a risk marker for increased violence and sexual and drug-related harms among survival sex workers. AIDS Care. 2008;20:228–234. doi: 10.1080/09540120701561270. [DOI] [PubMed] [Google Scholar]
- 18.Strathdee SA, Lozada R, Martinez G, Vera A, Rusch M, Nguyen L, et al. Social and structural factors associated with HIV infection among female sex workers who inject drugs in the Mexico-US border region. PLoS One. 2011;6:e19048. doi: 10.1371/journal.pone.0019048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shannon K, Rusch M, Shoveller J, Alexson D, Gibson K, Tyndall MW. Mapping violence and policing as an environmental-structural barrier to health service and syringe availability among substance-using women in street-level sex work. Int J Drug Policy. 2008;19:140–147. doi: 10.1016/j.drugpo.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 20.Tyndall MCS, Spittal P, Li K, Wood E, O'Shaughnessy MV, Schechter MT. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003:887–893. doi: 10.1097/00002030-200304110-00014. [DOI] [PubMed] [Google Scholar]
- 21.Wood E, Lloyd-Smith E, Li K, Strathdee SA, Small W, Tyndall MW, et al. Frequent needle exchange use and HIV incidence in Vancouver, Canada. Am J Med. 2007;120:172–179. doi: 10.1016/j.amjmed.2006.02.030. [DOI] [PubMed] [Google Scholar]
- 22.Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: risk-factor analysis. Lancet. 2001;357:1397–1401. doi: 10.1016/S0140-6736(00)04562-1. [DOI] [PubMed] [Google Scholar]
- 23.Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and noninjection drug users. J Urban Health. 2003;80:iii7–iii14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Des Jarlais DC, Perlis T, Arasteh K, Torian LV, Hagan H, Beatrice S, et al. Reductions in hepatitis C virus and HIV infections among injecting drug users in New York City. AIDS. 2005;(19 Suppl 3):S20–S25. doi: 10.1097/01.aids.0000192066.86410.8c. [DOI] [PubMed] [Google Scholar]
- 25.Wood E, Tyndall MW, Spittal PM, Li K, Hogg RS, Montaner JS, et al. Factors associated with persistent high-risk syringe sharing in the presence of an established needle exchange programme. AIDS. 2002;16:941–943. doi: 10.1097/00002030-200204120-00021. [DOI] [PubMed] [Google Scholar]
- 26.Wood E, Tyndall MW, Spittal P, Li K, RS H, O'Shaughnessy M, et al. Needle exchange and difficulty with needle access during an ongoing HIV epidemic. Int J Drug Policy. 2002;13:95–102. [Google Scholar]
- 27.Croxford S, Platt L, Hope VD, Cullen KJ, Parry JV, Ncube F. Sex work amongst people who inject drugs in England, Wales and Northern Ireland: findings from a National Survey of Health Harms and Behaviours. Int J Drug Policy. 2015;26:429–433. doi: 10.1016/j.drugpo.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 28.Watson D, Kail B, Ray S, Brown BS, Beschner GM Consortium TNAR. Handbook on risk of AIDS: injection drug users and sexual partners. Connecticut: Greenwood Press; 1993. Sex for money and drugs; pp. 211–223. [Google Scholar]
- 29.Richardson L, Wood E, Kerr T. The impact of social, structural and physical environmental factors on transitions into employment among people who inject drugs. Soc Sci Med. 2013;76:126–133. doi: 10.1016/j.socscimed.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shannon K, Kerr T, Allinott S, Chettiar J, Shoveller J, Tyndall MW. Social and structural violence and power relations in mitigating HIV risk of drug-using women in survival sex work. Soc Sci Med. 2008;66:911–921. doi: 10.1016/j.socscimed.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 31.Shannon K, Bright V, Gibson K, Tyndall MW. Sexual and drug-related vulnerabilities for HIV infection among women engaged in survival sex work in Vancouver, Canada. Can J Public Health. 2007;98:465–469. doi: 10.1007/BF03405440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paone D, Cooper H, Alperen J, Shi Q, Des Jarlais DC. HIV risk behaviours of current sex workers attending syringe exchange: the experiences of women in five US cities. AIDS Care. 1999;11:269–280. doi: 10.1080/09540129947910. [DOI] [PubMed] [Google Scholar]
- 33.Astemborski J, Vlahov D, Warren D, Solomon L, Nelson KE. The trading of sex for drugs or money and HIV seropositivity among female intravenous drug users. Am J Public Health. 1994;84:382–387. doi: 10.2105/ajph.84.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Booth RE, Dvoryak S, Sung-Joon M, Brewster JT, Wendt WW, Corsi KF, et al. Law enforcement practices associated with HIV infection among injection drug users in Odessa, Ukraine. AIDS Behav. 2013;17:2604–2614. doi: 10.1007/s10461-013-0500-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, et al. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376:268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.DeBeck K, Kerr T, Li K, Milloy MJ, Montaner J, Wood E. Incarceration and drug use patterns among a cohort of injection drug users. Addiction. 2009;104:69–76. doi: 10.1111/j.1360-0443.2008.02387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Castells X, Casas M, Perez-Mana C, Roncero C, Vidal X, Capella D. Efficacy of psychostimulant drugs for cocaine dependence. Cochrane Database Syst Rev. 2010;2:CD007380. doi: 10.1002/14651858.CD007380.pub3. [DOI] [PubMed] [Google Scholar]