Abstract
Background:
Patients with status migrainosus often need to be admitted due to the severity of their headaches. Their hospitalization is often prolonged due to poor headache control. Large sample studies looking into the factors associated with prolonged length of stay (pLOS) in status migrainosus are lacking.
Methods:
We utilized the Nationwide Inpatient Sample database to identify 4325 patients with primary discharge diagnosis of status migrainosus. Length of inpatient stay (LOS) of more than 6 days (90th percentile of LOS) was defined as pLOS. Patient demographics, hospital characteristics, mood disorders, anxiety disorder, and common medical comorbidities were identified. Multivariable logistic regression was used to identify factors associated with pLOS.
Results:
We found 402 patients with pLOS. Female gender, African American race, mood disorder, obesity, opioid abuse, congestive heart failure, and chronic renal failure were significant independent predictors of pLOS. Median inflation-adjusted cost of hospitalization was USD$3829 (interquartile range: 2419-5809).
Conclusion:
We were able to identify several factors associated with pLOS in status migrainosus. Most of the factors we found were similar to those known to increase the prevalence and severity of migraine in the general population. Knowledge of these factors may help physicians identify high-risk patients to institute early migraine abortive and prophylactic treatment in order to shorten the length of hospital stay.
Keywords: headache, migraine, status migrainosus, length of hospitalization, cost of hospitalization
Introduction
Migraine is prevalent in 5.6% of men and 17.1% of women.1 Status migrainosus is defined as a debilitating migraine attack lasting for more than 72 hours according to the International Headache Society classification criteria.2 In a study by Insinga et al, estimated number of admissions for migraine in the United States was found to be 51,116 cases in year 2008.3 Patients with status migrainosus are often hospitalized for investigation and/or treatment. According to a Scottish study, among nonstroke patients admitted to hyperacute stroke unit, 22% comprised migraine/headache.4 Longer hospital stay in these patients can serve as an indirect indicator of poor headache control and/or a refractory underlying primary headache disorder. Predictors of prolonged length of stay (pLOS) for status migrainosus have not been studied in real-world data. Identification of such predicting factors would allow better targeting of resources and the use of early, aggressive strategies in a selected group of patients. In this study, we attempted to identify 3 groups of predefined potential predictors of pLOS: (1) patient demographics; (2) common conditions known in the literature to affect the severity or prevalence of migraine in the general population; and (3) common medical comorbidities that are encountered by an inpatient physician in the United States (ie, obesity, diabetes mellitus, hypertension, and chronic heart, lung, liver, and kidney disease).
Methods
Patient Selection
We utilized data from the Nationwide Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project to include the time period between September 2008 and December 2011. The NIS is sponsored by Agency for Healthcare Research and Quality (AHRQ) of the US Department of Health and Human Services. The NIS represents approximately 20% sample of all discharges in nonfederal US hospitals.5 The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used to identify particular diseases, complications, and inpatient procedures. The NIS database was searched to isolate patients with a primary diagnosis of status migrainosus (ICD-9 codes 346.x2, 346.x3).
Exclusion Criteria
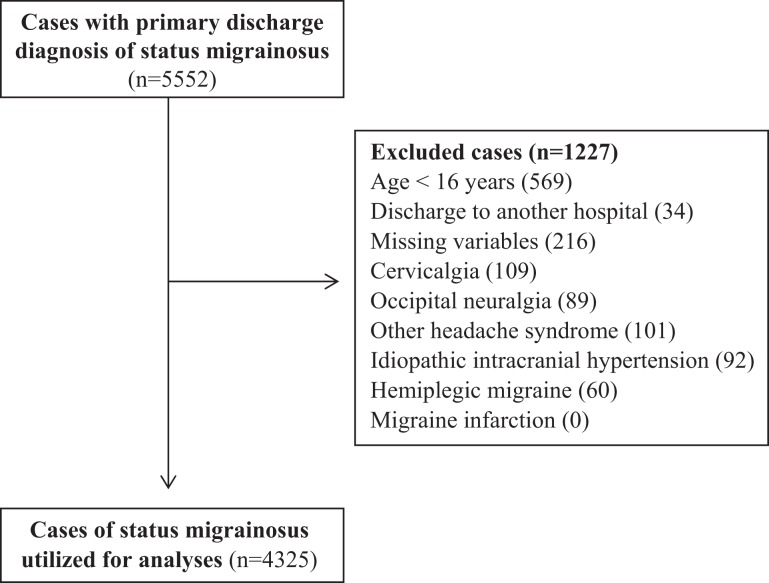
Patients younger than 16 years of age were excluded. Those who were discharged to another hospital were excluded to prevent single patients from being represented multiple times. Observations with any missing variables (except for the ethnicity) were excluded. Also, cases with reported hospital charge value less than 0 were excluded due to the possibility of erroneous entry. Patients with secondary diagnosis of other headache syndromes (339.xx; includes cluster headache, tension-type headache, posttraumatic headache, drug-induced headache, complicated headache syndrome, other specific headache syndrome), idiopathic intracranial hypertension (348.2), cervicalgia (723.1), and occipital neuralgia (723.8) were excluded to improve the diagnostic certainty of status migrainosus. Patients with a secondary diagnosis of hemiplegic migraine (346.3x) and migraine with cerebral infarction (346.6x) were excluded due to the requirement of more intensive workup and treatment in this group of patients. Further details on the number of excluded cases are provided in Figure 1.
Figure 1.
Excluded cases from the sample (not mutually exclusive).
Outcome Measures and Comorbidities
The primary outcome measure was pLOS, which was defined as in-hospital stay of more than 6 days (90th percentile of length of inpatient stay [LOS]).6,7 We searched for following coexisting conditions: mood disorder (311, 296.xx), bipolar disorder (296.0x, 296.4x, 296.5x, 296.6x, 296.80. 296.89), depression (311, 296.2x, 296.3x, 296.82), obstructive sleep apnea (327.23), anxiety disorder (300.0x), and opioid abuse (304.0x, 304.7x). The AHRQ comorbidity measures8 were used to identify patients with common medical comorbidities including obesity, hypertension, diabetes mellitus, congestive heart failure, chronic renal disease, chronic liver disease, and chronic lung disease.
Statistics
Patient demographics, hospital characteristics, and complications were described by percent proportions (for categorical and ordinal variables) and median and interquartile range (IQR; for numeric variables). Univariate logistic regression was used to identify predictors of pLOS, and only those variables with pLOS association significance P value <.2 were included in the multivariable logistic regression. In the final model, predictors with P values <.05 were considered statistically significant. Patients with missing race information were included in the analyses as a separate group, because some states suppressed the racial information in the NIS and hence the information was not missing at random. Patients with depression, bipolar disorder, and other mood disorder were grouped into a category of “mood disorder.” Age was divided into groups of 10 years for the purpose of regression analysis. Patients with Asian, Pacific Islander, Native American, and other races were grouped into “other” class due to low proportion of these races. Cost of hospital stay was calculated whenever hospital charge and cost-to-charge ratios were available. Inflation adjustment for the year 2015 was done using the consumer price index calculator of the Bureau of Labor Statistics.9 All analyses were performed using SAS Studio 3.1 (SAS Institute Inc, Cary, North Carolina).
Results
We included 4325 patients in our study after excluding cases as per previously mentioned exclusion criteria, of which 85.5% were females, almost 70% patients were Caucasians, and median age was 38 years (IQR: 18 [29-47]). Vast majority of these admissions were in urban hospitals (92%) and large hospital bed size (63.9%). Details of patient demographics and hospital characteristics are described in Table 1. Median LOS was 3 days (IQR: 2 [2-4]), and 402 (9.3%) patients had pLOS. Median inflation-adjusted cost of hospitalization (for 4027 cases) was USD$3829 (IQR: 2419-5809).
Table 1.
Baseline Patient Characteristics and Univariate Association With pLOS.
| n (%) | Patients With pLOS, % | OR (95% CI) | P | |
|---|---|---|---|---|
| Calendar year | – | – | 0.93 (0.83-1.03) | .153 |
| Demographics | ||||
| Agea (median) | 38 (IQR: 29-47) | – | 1.01 (0.93-1.09) | .896 |
| Gender | ||||
| Female | 3697 (85.5) | 9.9 | 1.81 (1.27-2.57) | .001 |
| Male | 628 (14.5) | 5.7 | ||
| Ethnicity | ||||
| Caucasian | 3014 (69.7) | 8.7 | 1.0 | – |
| African American | 381 (8.8) | 13.1 | 1.59 (1.15-2.20) | .024 |
| Hispanic | 277 (6.4) | 11.9 | 1.43 (0.97-2.10) | .185 |
| Otherb | 132 (3.1) | 6.8 | 0.77 (0.39-1.54) | .168 |
| Missingc | 521 (12.1) | 9.4 | 1.10 (0.80-1.51) | .787 |
| Median household income quartile (percentile)d | ||||
| 0-25th | 985 (22.8) | 11.6 | 1.0 | – |
| 26th-50th | 1124 (26) | 8.7 | 0.73 (0.55-0.97) | .444 |
| 51st-75th | 1130 (26.1) | 8.5 | 0.71 (0.53-0.94) | .285 |
| 76th-100th | 1085 (25.1) | 8.7 | 0.73 (0.54-0.97) | .406 |
| Hospital characteristics | ||||
| Hospital teaching status | ||||
| Teaching | 2295 (53.1) | 10.0 | 1.19 (0.97-1.46) | .099 |
| Nonteaching | 2030 (46.9) | 8.5 | ||
| Hospital location | ||||
| Urban | 3978 (92) | 9.4 | 1.14 (0.77-1.68) | .530 |
| Rural | 347 (8) | 8.4 | ||
| Hospital bed sizee | ||||
| Small | 474 (11) | 7.8 | 1.0 | – |
| Medium | 1087 (25.1) | 9.2 | 1.20 (0.81-1.77) | .632 |
| Large | 2764 (63.9) | 9.6 | 1.25 (0.88-1.79) | .256 |
Abbreviations: CI, confidence interval; IQR, interquartile range; OR, odds ratio; pLOS, prolonged length of stay.
a Age divided into groups of 10 years in the regression model.
b Includes Asian, Pacific Islander, Native American, and other.
c Racial information suppressed by some states.
d Median household income quartile for patient’s zip code during that year.
e Refer to http://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp for hospital bed size information.
Table 2 describes certain psychiatric conditions and medical comorbidities and their association with pLOS. The prevalence of mood disorder and anxiety disorder was 24.6% and 11.8%, respectively. Some common medical comorbidities that we identified were obesity (10.5%), obstructive sleep apnea (3.5%), hypertension (25.8%), chronic lung disease (13.9%), and diabetes mellitus (8.4%). Significant univariate association with pLOS was present with mood disorder, obesity, opioid abuse, congestive heart failure, chronic lung disease, and chronic renal disease.
Table 2.
Medical and Psychiatric Conditions and Association With pLOS.
| n (%) | Patients With pLOS, % | OR (95% CI) | P | |
|---|---|---|---|---|
| Mood disordera | 1065 (24.6) | 11.6 | 1.41 (1.13-1.77) | .003 |
| Anxiety disorder | 509 (11.8) | 10.2 | 1.13 (0.83-1.53) | .447 |
| Obesity | 455 (10.5) | 12.8 | 1.50 (1.11-2.02) | .008 |
| Opioid abuse | 47 (1.1) | 25.5 | 3.42 (1.76-6.64) | <.001 |
| Obstructive sleep apnea | 153 (3.5) | 11.1 | 1.23 (0.74-2.06) | .432 |
| Chronic hypertension | 1117 (25.8) | 10.7 | 1.25 (0.99-1.57) | .052 |
| Diabetes mellitus | 362 (8.4) | 11.9 | 1.36 (0.97-1.90) | .075 |
| Congestive heart failure | 33 (0.8) | 27.3 | 3.72 (1.72-8.06) | <.001 |
| Chronic renal failure | 59 (1.4) | 23.7 | 3.11 (1.69-5.72) | <.001 |
| Chronic liver disease | 47 (1.1) | 14.9 | 1.76 (0.78-3.97) | .170 |
| Chronic lung disease | 599 (13.9) | 11.9 | 1.38 (1.05-1.81) | .021 |
Abbreviations: CI, confidence interval; OR, odds ratio; pLOS, prolonged length of stay.
a Includes depression, bipolar disorder, and other mood disorders.
Table 3 describes the multivariable regression model. Female gender, African American race (compared to the Caucasian), mood disorder, opioid abuse, and comorbid congestive heart failure and chronic renal failure were significant predictors of pLOS in the multivariable analysis.
Table 3.
Multivariable Logistic Regression: Predictors of pLOS.
| aOR (95% CI) | P | |
|---|---|---|
| Calendar year (every year increase) | 0.91 (0.81-1.01) | .076 |
| Female | 1.77 (1.24-2.53) | .002 |
| Ethnicity | ||
| Caucasian | 1.0 | − |
| African American | 1.51 (1.08-2.11) | .040 |
| Hispanic | 1.40 (0.95-2.08) | .173 |
| Othera | 0.78 (0.39-1.56) | .218 |
| Missingb | 1.01 (0.73-1.40) | .542 |
| Teaching hospital status | 1.19 (0.96-1.47) | .108 |
| Mood disorderc | 1.36 (1.09-1.71) | .008 |
| Obesity | 1.33 (0.98-1.82) | .072 |
| Opioid abuse | 3.40 (1.73-6.72) | <.001 |
| Chronic hypertension | 1.08 (0.84-1.38) | .567 |
| Diabetes mellitus | 1.07 (0.74-1.55) | .707 |
| Congestive heart failure | 2.34 (1.05-5.45) | .037 |
| Chronic renal failure | 2.61 (1.36-5.01) | .004 |
| Chronic liver disease | 1.66 (0.72-3.80) | .231 |
| Chronic lung disease | 1.22 (0.92-1.61) | .165 |
Abbreviations: aOR, adjusted odds ratio (adjusted for other covariates in the model); CI, confidence interval; pLOS, prolonged length of stay.
a Includes Asian, Pacific Islander, Native American, and other.
b Racial information suppressed by some states.
c Includes depression, bipolar disorder, and other mood disorders.
Discussion
Our study intends to identify factors that prolong the length of hospital stay in patients admitted with a primary diagnosis of status migrainosus under the presumption that the most probable cause would be poor headache control. Identifying length of hospital stay is also an important part of developing cost-cutting strategies, as during the year 2012, each day of hospital stay costed average USD$10,400 in the United States.10 We have summarized and discussed the significant predictors of pLOS in this article.
In the general US population, prevalence of migraine in females is 3 times higher than in males (17.1% vs 5.6%).1 But our study showed that among the patients admitted for status migrainosus, the number of females was almost 6 times higher than the number of males (85.5% vs 14.5%). Furthermore, female gender appeared to be a significant independent predictor of pLOS. The American Migraine Prevalence and Prevention study demonstrated that women have a higher prevalence of chronic migraine and that women with chronic migraine have higher rates of “very severe headache-related disability” than men with chronic migraine. It is possible that patients with chronic migraine and very severe headache-related disability are more likely to require hospitalization for status migrainosus.11
A multicenter study with cohort from headache subspecialty clinics revealed that the African Americans reported more frequent and severe headaches compared to the Caucasians. We found concordant results with the African American race being independent predictor of pLOS compared to the Caucasians.12
Anxiety, mood, and personality disorders are known to be associated with migraine in prospective studies.13–15 Prevalence of depression in migraine has been reported as high as 28.1%.16 Merikangas et al were able to demonstrate that migraine and anxiety/depression have a syndromic rather than causative relationship.13 According to one study, bipolar spectrum disorder has been found to be prevalent in 8.8% of patients with migraine compared to 3.3% of patients without migraine. Similarly, anxiety disorder has been reported to be present in 9.1% of patients with migraine.17,18 We found anxiety disorder to be present in 11.8% of patients. It, however, did not affect the length of hospitalization. It is possible that the true prevalence of these conditions is even higher. This is because of the lack of formal evaluation and documentation of the mood and anxiety disorders in every inpatient admission for status migrainosus.
Hemodialysis is also known to cause headaches, and according to one study, its prevalence in hemodialysis patients is 6% to 7%.19–21 We identified chronic renal failure (including end-stage renal disease) as a significant independent predictor of pLOS. However, in such patients, hospitalization may be lengthened by medical complications or comorbidities rather than the direct effect of chronic renal failure. It is also possible that the inability to use headache medications that are contraindicated in renal failure results in pLOS.
Migraine, especially more than 10-year duration, has been significantly associated with diastolic heart failure.22 Additionally, chronic pain is prevalent and significantly affects the quality of life of patients with heart failure.23 In our study, although the number of patients with congestive heart failure was small (n = 37; 0.8%), it was a significant predictor of pLOS. We postulate that this is related to medical complications, inability to use certain relevant medications (eg, nonsteroidal anti-inflammatory medications), and a potential direct effect on the intractability of the headache disorder.
Univariate analysis by Scher et al has shown that obesity is significantly associated with onset of chronic daily headaches.24 Another study revealed that obesity was a strong predictor of 10 or more migraine headaches per month (5.8% in overweight, 13.6% in obese, and 20.7% in morbidly obese compared to 4.4% in normal-weight individuals).25 Obesity did prolong hospital stay in univariate analysis in our study; however, it failed to do so in the multivariate model. Undiagnosed idiopathic intracranial hypertension may affect headache severity in obese population, which we were not able to evaluate in this study.
We found 1.1% of patients with opioid abuse in our study with strong association with pLOS. Actual prevalence may even be higher because of the uncertainty of the screening process and coding in our sample. Hence, the validity of coding for opioid abuse remains uncertain in our administrative database. The type of opioids could not be determined either (medication vs recreational drugs). It should also be noted that the patients with medication overuse headaches were excluded from our study, as the definition of status migrainosus requires the absence of medication overuse.2 This likely resulted in the exclusion of some patients with concurrent opioid abuse. Furthermore, the use of drugs other than opioid as the etiology of headaches may go unrecognized if appropriate diagnostic coding is not done. Therefore, this result should be interpreted with caution.
The results of our study have to be viewed with consideration of several limitations and potential sampling bias. In the NIS database, diagnostic validity of status migrainosus remains uncertain and depends upon correct and appropriate diagnostic codes used by the discharging physician and/or the abstractors. Such a sampling bias is often an inherent limitation of the studies using an administrative database. We attempted to minimize such uncertainty by excluding diagnoses that may confound the diagnosis of status migrainosus. Similarly, validity of secondary diagnoses also relies upon the use of appropriate ICD-9 diagnostic codes. Each hospital admission is considered as a separate case, and there are no unique patient identifier variables in the NIS database. This may potentially introduce a sampling bias in our study because of the possibility of a single patient being counted multiple times. We attempted to reduce such cases by excluding patients who were discharged to another hospital (n = 34). Furthermore, NIS is a 20% sample of discharges from the State Inpatient Database (SID),5 thus eliminating 80% of total cases from the SID. This could significantly reduce the number of duplicate cases in the NIS. Patients, especially those with chronic heart or renal disease, may develop complications during their inpatient stay. Many such complications may be primarily responsible for pLOS rather than status migrainosus itself. Because of the large number of such possible complications, we did not attempt to identify each of them individually. We only included chronic medical conditions and comorbidities that are commonly encountered by the treating inpatient physicians in the United States. It should also be noted that our study was discovery oriented in design, and therefore, the findings should be viewed as hypothesis generating only.
Conclusion
In this study, we identified factors that predict prolonged hospital stay such as female gender, African American race, mood disorder, opioid abuse, and comorbid chronic renal failure and congestive heart failure. Such prolonged hospital stay may indirectly indicate poor headache control in patients with status migrainosus. The majority of these factors are already known to be associated with either a higher prevalence or an increased severity of migraine in the general population. In addition, we found that general medical comorbidities such as chronic heart and kidney failure prolong inpatient stay in these patients. This may indirectly be related to higher intensity and refractoriness of the headaches in this subgroup of patients. Future research may be indicated to investigate clinical or pathological basis of association of these factors with the headache control. Knowledge of these factors may help physicians identify high-risk patients to institute early migraine abortive and prophylactic treatment26 in order to shorten the length of hospital stay.
Ethics
Nationwide Inpatient Sample (NIS) is a publicly available database and contains no patient identifying information5 and therefore meets the criteria for exemption from review by institutional review board (IRB).27
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–349. [DOI] [PubMed] [Google Scholar]
- 2. Web site http://ihs-classification.org/en/02_klassifikation/02_teil1/01.05.02_migraine.html. Accessed March 2016.
- 3. Insinga RP, Ng-Mak DS, Hanson ME. Costs associated with outpatient, emergency room and inpatient care for migraine in the USA. Cephalalgia. 2011;31(15):1570–1575. [DOI] [PubMed] [Google Scholar]
- 4. Reid JM, Currie Y, Baird T. Non-stroke admissions to a hyperacute stroke unit. Scott Med J. 2012;57(4):209–211. [DOI] [PubMed] [Google Scholar]
- 5. Web site http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed March 2016.
- 6. Hollenbeck BK, Roberts WW, Wolf JS. Importance of perioperative processes of care for length of hospital stay after laparoscopic surgery. J Endourol. 2006;20(10):776–781. [DOI] [PubMed] [Google Scholar]
- 7. Torrecillas JM, Millan EM, Garcia IS, Pereira MC. Factors associated with unusually long stays in heart failure hospitalizations in Spain [in Spanish]. An Sist Sanit Navar. 2011;34(2):203–217. [DOI] [PubMed] [Google Scholar]
- 8. Web site http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed March 2016.
- 9. Web site http://www.bls.gov/data/inflation_calculator.htm. Accessed March 2016.
- 10. Web site http://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf. Accessed March 2016.
- 11. Buse DC, Manack AN, Fanning KM, et al. Chronic migraine prevalence, disability, and sociodemographic factors: results from the American Migraine Prevalence and Prevention Study. Headache. 2012;52(10):1456–1470. [DOI] [PubMed] [Google Scholar]
- 12. Heckman BD, Merrill JC, Anderson T. Race, psychiatric comorbidity, and headache characteristics in patients in headache subspecialty treatment clinics. Ethn Health. 2013;18(1):34–52. [DOI] [PubMed] [Google Scholar]
- 13. Merikangas KR, Merikangas JR, Angst J. Headache syndromes and psychiatric disorders: association and familial transmission. J Psychiatr Res. 1993;27(2):197–210. [DOI] [PubMed] [Google Scholar]
- 14. Hamelsky SW, Lipton RB. Psychiatric comorbidity of migraine. Headache. 2006;46(9):1327–1333. [DOI] [PubMed] [Google Scholar]
- 15. Merikangas KR, Stevens DE, Angst J. Headache and personality: results of a community sample of young adults. J Psychiatr Res. 1993;27(2):187–196. [DOI] [PubMed] [Google Scholar]
- 16. Patel NV, Bigal ME, Kolodner KB, Leotta C, Lafata JE, Lipton RB. Prevalence and impact of migraine and probable migraine in a health plan. Neurology. 2004;63(8):1432–1438. [DOI] [PubMed] [Google Scholar]
- 17. McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain. 2004;111(1-2):77–83. [DOI] [PubMed] [Google Scholar]
- 18. Merikangas KR, Risch NJ, Merikangas JR, Weissman MM, Kidd KK. Migraine and depression: association and familial transmission. J Psychiatr Res. 1988;22(2):119–129. [DOI] [PubMed] [Google Scholar]
- 19. Web site http://ihs-classification.org/en/02_klassifikation/03_teil2/10.02.00_homoeostasis.html. Accessed March 2016.
- 20. Milinkovic M, Zidverc-Trajkovic J, Sternic N, et al. Hemodialysis headache. Clin Nephrol. 2009;71(2):158–163. [DOI] [PubMed] [Google Scholar]
- 21. Jesus AC, Oliveira HA, Paixao MO, Fraga TP, Barreto FJ, Valenca MM. Clinical description of hemodialysis headache in end-stage renal disease patients. Arq Neuropsiquiatr. 2009;67(4):978–981. [DOI] [PubMed] [Google Scholar]
- 22. Ekici B, Unal-Cevik I, Akgul-Ercan E, Morkavuk G, Yakut Y, Erkan AF. Duration of migraine is associated with cardiac diastolic dysfunction. Pain Med (Malden, Mass). 2013;14(7):988–993. [DOI] [PubMed] [Google Scholar]
- 23. Udeoji DU, Shah AB, Bharadwaj P, Katsiyiannis P, Schwarz ER. Evaluation of the prevalence and severity of pain in patients with stable chronic heart failure. World J Cardiol. 2012;4(8):250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106(1-2):81–89. [DOI] [PubMed] [Google Scholar]
- 25. Bigal ME, Liberman JN, Lipton RB. Obesity and migraine: a population study. Neurology. 2006;66(4):545–550. [DOI] [PubMed] [Google Scholar]
- 26. Nagy AJ, Gandhi S, Bhola R, Goadsby PJ. Intravenous dihydroergotamine for inpatient management of refractory primary headaches. Neurology. 2011;77(20):1827–1832. [DOI] [PubMed] [Google Scholar]
- 27. Web site http://www.hhs.gov/ohrp/policy/checklists/decisioncharts.html. Accessed March 2016.