Abstract
Articular cartilage injuries, and corresponding surgical procedures, are occurring with increasing frequency as identified by a review of recent surgical trends. Concerns have grown in recent years regarding the longevity of results following microfracture, with a shift toward cartilage restoration procedures in recent years. This case report describes 2 cases of acute failure following the use of commercially available osteochondral allograft plugs used for the treatment of osteochondral defects of the distal femur. In both cases the chondral surface of the plug delaminated from the underlying cancellous bone, resulting in persistent pain and swelling requiring reoperation and removal of the loose fragments. Caution should be employed when considering use of these plugs for the treatment of osteochondral lesions, as similar outcomes have not been noted with other cartilage restoration techniques.
Keywords: knee, cartilage restoration, osteochondral allograft, complication
Introduction
Full-thickness chondral injuries represent a challenging entity to treat. Due to limited regenerative capacity, the presence of full-thickness lesions is often associated with high levels of morbidity and functional decline.1,2 Historically, microfracture has been considered the gold standard for management of these lesions given the procedure’s technical ease and limited surgical morbidity; however, microfracture has questionable durability and limited efficacy in the treatment of larger lesions (>2 cm2).3,4 Autologous chondrocyte implantation (ACI) has also been used as a treatment method for these lesions but is associated with increased cost and surgical morbidity with both a harvesting procedure and an implantation procedure.2 Osteochondral autograft transplantation (OAT) has also been commonly used; however, donor site morbidity and articular congruency mismatch are common pitfalls of the procedure.2,5
More recently, commercially produced osteochondral allograft plugs have been made available, including Chondrofix (Zimmer, Warsaw, IN), for the treatment of chondral defects. While a seemingly attractive alternative to the previously mentioned surgical interventions, there is limited information on their efficacy in treating osteochondral lesions. We present 2 cases of early failure following the use of these commercially available plugs.
Case 1
At the onset of injury, the patient was a healthy 37-year-old male participating in a crossfit training program when he experienced activity-related knee pain. He presented for evaluation, and radiographic investigations revealed chondral lesions on both his lateral and medial femoral condyles as well as a medial meniscal tear. There were no associated tibial chondral lesions or significant malalignment of the limb warranting realignment considerations.
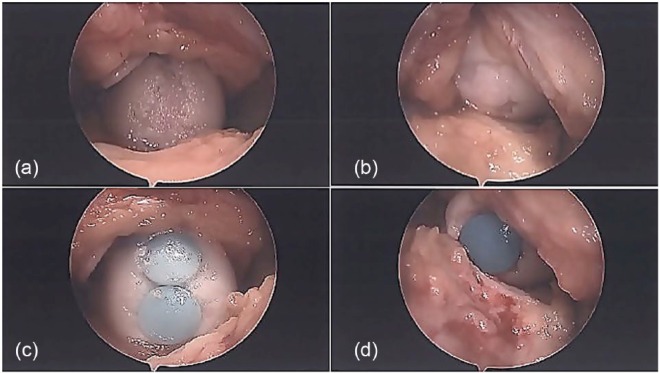
Arthroscopic exploration confirmed the MRI findings, revealing a large grade IV medial femoral condyle cartilage lesion (3.0 cm × 1.2 cm) ( Fig. 1a ) and a grade IV lateral femoral condyle cartilage lesion (2.0 cm × 1.5 cm) ( Fig. 1b ). The patient underwent a partial medial meniscectomy (>50%) and the chondral lesions were treated with Chondrofix osteochondral allograft implantation. The lateral chondral lesion was treated with a single Chondrofix plug (15 mm) ( Fig. 1c ), while the medial chondral lesion was treated with 3 abutting Chondrofix plugs (all 11 mm) ( Fig. 1d ). All 4 plugs were inserted as per manufacturer’s instructions and found to have good fixation, with stable borders providing good restoration of the congruency of the chondral surface.
Figure 1.
Intraoperative photos from Case 1: (a) medial femoral condyle lesions; (b) lateral femoral condyle lesion; (c) medial osteochondral allograft plugs; (d) lateral osteochondral allograft plug.
The patient underwent standard postoperative rehabilitation initiating continuous passive motion from 0° to 60° in the recovery room and continued for 4 to 6 hours per day for 6 weeks, increasing flexion gradually as tolerated. Weight bearing was protected for 2 weeks. No brace was required.
The postoperative period was relatively uncomplicated, with progression through physiotherapy with restoration of full motion. On presenting in clinic for routine 6-month follow-up, the patient was found to have persistent knee pain with a notable effusion. The symptomatic knee was aspirated by the attending surgeon and an injection of corticosteroids was administered to treat for presumed synovitis. A corresponding decrease was noted in clinical outcome scores at that time ( Table 1 ). An MRI was ordered that showed delamination of one of the medial plugs ( Fig. 2 ) and the lateral plug ( Fig. 3 ).
Table 1.
Case 1: Clinical Outcome Scores.
| Activities of Daily Living | IKDC Subjective Score | Marx Activity Score | |
|---|---|---|---|
| Preoperative | 78.75 | 50.57 | 12 |
| 6-Month postoperative | 70 | 39.08 | 0 |
IKDC = International Knee Documentation Committee.
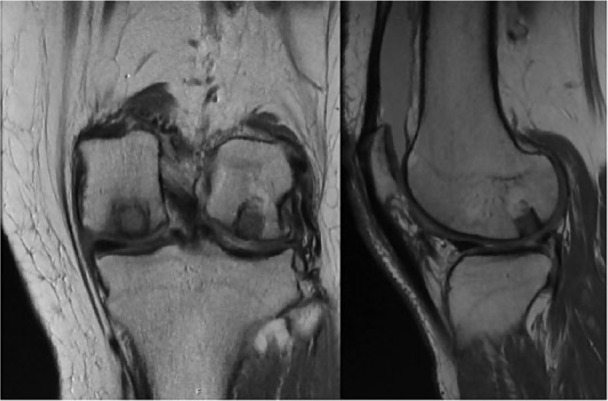
Figure 2.
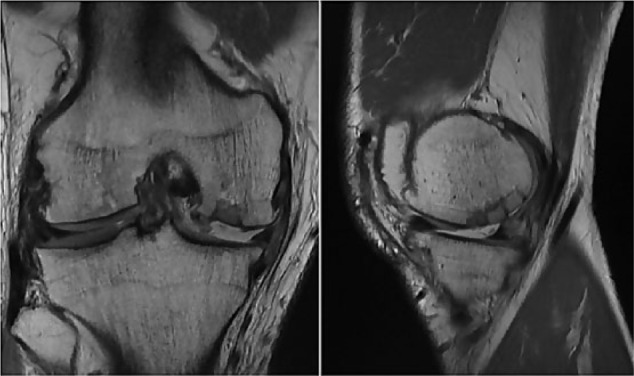
Postoperative MRI scan demonstrating medial plug delamination.
Figure 3.

Postoperative MRI scan demonstrating lateral plug delamination.
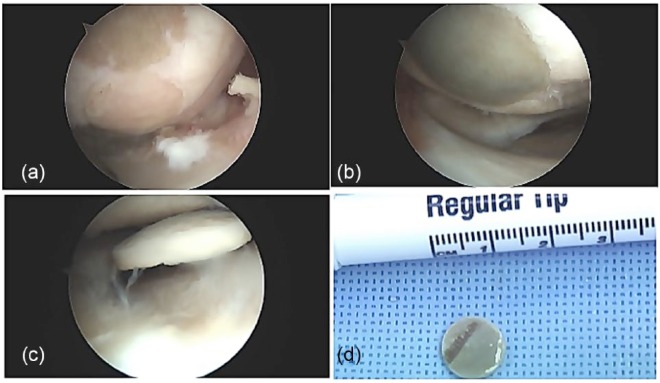
A repeat right knee arthroscopy was subsequently performed. In the medial compartment, the superficial layer of the central Chondrofix plug had delaminated ( Fig. 4a ) and multiple loose bodies were present. Similarly, in the lateral compartment, the superficial layer of the Chondrofix plug had also delaminated ( Fig. 4b ) and was found in its entirety within the lateral compartment ( Fig. 4c ). All loose bodies were removed with a grasper or shaver ( Fig. 4d ). Postoperatively, rehabilitation guidelines included full weight-bearing with progression of range of motion as tolerated.
Figure 4.
Intraoperative photos from revision arthroscopy of Case 1: (a) medial femoral plug delamination; (b) lateral femoral plug delamination; (c) loose chondral fragment from lateral femoral plug; (d) retrieved loose body.
Case 2
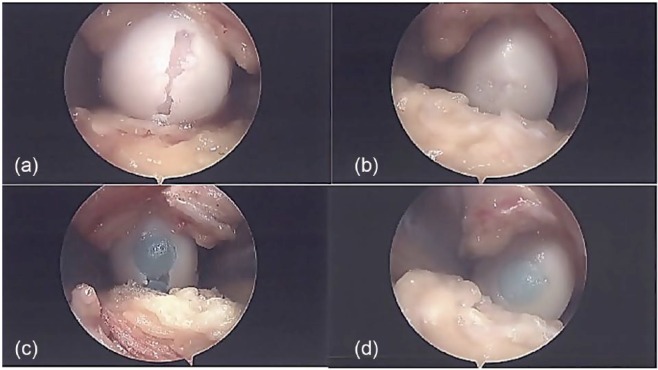
A healthy 47-year-old female participating in exercise classes began experiencing activity-related knee pain. Investigations revealed a lateral meniscal tear in her left knee. Additionally, she had evidence of full-thickness chondral defects involving both the medial and lateral femoral condyles. After failing a trial of conservative management, arthroscopic evaluation confirmed both degenerative medial and lateral meniscal tears, as well as a large grade IV medial femoral condyle cartilage lesion (2.0 cm × 1.0 cm) ( Fig. 5a ) and a grade IV lateral femoral condyle cartilage lesion (1.0 cm × 1.0 cm) ( Fig. 5b ).
Figure 5.
Intraoperative photos from Case 2: (a) medial femoral condyle lesions; (b) lateral femoral condyle lesion; (c) Medial osteochondral allograft plugs; (d) lateral osteochondral allograft plug.
Partial medial and lateral meniscectomies (>50%) were performed, following which the chondral lesions were treated with Chondrofix osteochondral allograft plug implantation. The medial lesion was treated with 2 Chondrofix plugs (7 mm and 11 mm; Fig. 5c ), while the lateral chondral lesion was treated with 1 Chondrofix plug (9 mm; Fig. 5d ). All 3 plugs were again inserted as per manufacturer’s recommendations and found to have good fixation, with stable borders and good restoration of the articular surface.
Again, the early postoperative course was uneventful with standard postoperative rehabilitation. At 3-month follow-up, the patient was doing well clinically, with a full range of motion. On examination, a small amount of prepatellar bursal thickening was noted, with an otherwise normal exam with no effusion. Five months postoperatively the patient was seen again due to the return of presurgical left knee symptoms, including swelling and pain. The patient’s MRI did not show any loose bodies at this time ( Fig. 6 ) and therefore the knee was treated with an injection of corticosteroids for presumed synovitis.
Figure 6.
Postoperative MRI demonstrating intact allograft plugs.
Due to the continuation of symptoms, a repeat MRI was conducted at 7-month follow-up appointment, which revealed a delamination of the chondral surface of the superficial layer of the Chondrofix implant in the lateral compartment ( Fig. 7 ). A corresponding decrease was noted in clinical outcome scores ( Table 2 ).
Figure 7.
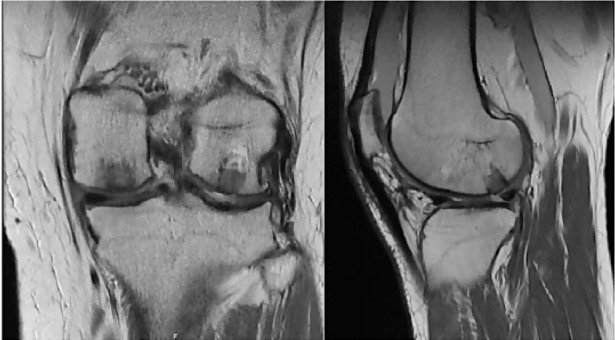
Postoperative MRI scan demonstrating lateral plug delamination.
Table 2.
Case 2: Clinical Outcome Scores.
| Activities of Daily Living | IKDC Subjective Score | Marx Activity Score | |
|---|---|---|---|
| Preoperative | 85.00 | 63.22 | 7 |
| 6-Month postoperative | 83.75 | 63.22 | 12 |
IKDC = International Knee Documentation Committee.
The patient was brought in for a repeat left knee arthroscopy. In the lateral compartment, the Chondrofix-filled lesion was seen with the deeper scaffold portion still in place, but with the superficial layers absent ( Fig. 8 ). In the medial compartment and the posterior aspect of the knee, multiple small loose bodies were found as well. All loose bodies were removed with a shaver. Again, postoperative range of motion allowed full weight-bearing as tolerated with progressive range of motion as tolerated.
Figure 8.

Intraoperative photo of delaminated lateral femoral condyle plug.
Postoperatively, this patient continued to have pain. They subsequently underwent revision surgery, with insertion of fresh osteochondral allograft plugs.
Discussion
The incidence of symptomatic focal cartilage lesions is increasing annually6; however, the optimal method of treatment for these lesions continues to be debated. Treatment options range from palliative (chondroplasty or debridement) to repair (microfracture) to restoration techniques (OATs, ACI, osteochondral allograft, or synthetic scaffold plugs), with widely variable reports of success. While more recent evidence suggests that restoration procedures are superior to repair,1,2,7,8 there is no consensus on the gold standard among cartilage restoration procedures. These restoration procedures have the capability of providing pain relief, while also potentially delaying the progression of degenerative joint disease. As such, they have received significant attention in recent years in attempts to identify the procedure that provides maximal clinical benefit with the least amount of associated surgical morbidity and cost.
As briefly described above, Chondrofix osteochondral allograft is a commercially available product composed of donated human decellularized hyaline cartilage and cancellous bone. It is theorized to offer the same structural and osteoconductivity benefits of an OATs procedure, while removing the associated donor site morbidity and eliminating the wait for fresh osteochondral allograft. Additionally, it is theorized to retain the normal mechanical properties of the articular cartilage during processing, to allow early range of motion and weight-bearing. Our study is the first report of chondral delamination following the use of these plugs in 2 separate cases within 8 months of their primary surgical procedure. Both patients were healthy, active patients who met surgical indications for the procedure, which was performed as per the described surgical technique. Both also presented in a similar manner with residual knee pain roughly 6 months postoperatively, initially thought to be secondary to synovitis. Imaging confirmed delamination of the Chondrofix plugs, requiring repeat surgical intervention for removal of loose bodies. This is a concerning finding and has not been noted to occur with either osteochondral autograft transfer (OATs) or fresh osteochondral allograft (OCA) plugs. As such, concern should be raised over the structural properties of these implants and further experimental study should precede widespread clinical use.
There is a paucity of literature available on the utility of this product, although similar findings were reported in a recent abstract by Farr et al.9 They retrospectively reviewed their results with 32 cases treated with Chondrofix implants. They noted failure, defined as structural damage to the allograft plug documented on MRI or arthroscopic evaluation, in 72% of the cases. Given the findings of these 2 reports, caution should be employed in utilization of these plugs, as failure rates of this magnitude have not been found with alternative cartilage restoration procedures.
Since identifying these cases of acute failure, we have reviewed all patients who were treated with these allograft plugs at our institution. A total of 36 cases have been performed to date. Aside from the 2 reported cases, there have been an additional 2 patients that have undergone revision with fresh osteochondral allograft. An additional 7 patients continue to have pain, with evidence of active knee inflammation and swelling. These additional patients are all considering revision surgery. Including all revised patients and those with persistent symptoms, 11 of our 36 cases (31%) are classified as failures to date.
Conclusion
In summary, we recommend caution in adopting the use of these commercially available osteochondral allograft plugs as delamination poses a challenging clinical problem that has not been encountered with the use of OAT or OCA procedures. Beyond the need for repeat surgery, and potential need for revision cartilage restoration procedures, their failure is associated with an extended period of disability and increased cost. Additionally, with the increasing number of cartilage restoration procedures performed each year, it is important for orthopedic surgeons to be aware of this potential complication as a cause for early failure following these procedures.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: Ethical approval for this study was obtained from the Instituional Review Board at the Hospital for Special Surgery (IRB # 25023).
References
- 1. Krych AJ, Harnly HW, Rodeo SA, Williams RJ. Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee. J Bone Jt Surg Am. 2012;94(11):971-8. doi: 10.2106/JBJS.K.00815. [DOI] [PubMed] [Google Scholar]
- 2. Camp CL, Stuart MJ, Krych AJ. Current concepts of articular cartilage restoration techniques in the knee. Sports Health. 2013;6(3):265-73. doi: 10.1177/1941738113508917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goyal D, Keyhani S, Lee EH, Hui JHP. Evidence-based status of microfracture technique: a systematic review of level I and II studies. Arthroscopy. 2013;29(9):1579-88. doi: 10.1016/j.arthro.2013.05.027. [DOI] [PubMed] [Google Scholar]
- 4. Williams RJ, Harnly HW. Microfracture: indications, technique, and results. Instr Course Lect. 2007;56:419-28. [PubMed] [Google Scholar]
- 5. Shaha JS, Cook JB, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Return to an athletic lifestyle after osteochondral allograft transplantation of the knee. Am J Sports Med. 2013;41(9):2083-9. doi: 10.1177/0363546513494355. [DOI] [PubMed] [Google Scholar]
- 6. McCormick F, Harris JD, Abrams GD, Frank R, Gupta A, Hussey K, et al. Trends in the surgical treatment of articular cartilage lesions in the United States: an analysis of a large private-payer database over a period of 8 years. Arthroscopy. 2014;30(2):222-6. doi: 10.1016/j.arthro.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 7. Crawford DC, DeBerardino TM, Williams RJ. NeoCart, an autologous cartilage tissue implant, compared with microfracture for treatment of distal femoral cartilage lesions: an FDA phase-II prospective, randomized clinical trial after two years. J Bone Joint Surg Am. 2012;94(11):979-89. doi: 10.2106/JBJS.K.00533. [DOI] [PubMed] [Google Scholar]
- 8. Gudas R, Gudaitė A, Mickevičius T, Masiulis N, Simonaitytė R, Cekanauskas E, et al. . Comparison of osteochondral autologous transplantation, microfracture, or debridement techniques in articular cartilage lesions associated with anterior cruciate ligament injury: a prospective study with a 3-year follow-up. Arthroscopy. 2013;29(1):89-97. doi: 10.1016/j.arthro.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 9. Farr J, Gracitelli G, Gomoll AH. Decellularized osteochondral allograft for the treatment of cartilage lesions in the knee. Orthop J Sport Med. 2015;3(2 suppl). doi: 10.1177/2325967115S00068. [DOI] [PubMed] [Google Scholar]