Abstract
Aim
Despite its declining incidence, sudden infant death syndrome (SIDS) is still an important cause of death in infancy. This study investigated the environmental circumstances associated with SIDS, by analysing data from all sudden unexpected deaths in infancy (SUDI) in Sweden from 2005 to 2011.
Methods
All Swedish infants forensically autopsied up to the age of 365 days from 2005 to 2011 were included. Medical records were obtained from the hospitals and supplementary data from the Swedish Medical Birth Register.
Results
Of the 261 infants, 136 were defined as SIDS and 125 as explained SUDI. The documentation in the medical records was poor when it came to issues such as bed sharing, sleep position, smoking, breastfeeding and pacifier use. The main findings were a significantly higher prevalence of bed sharing in SIDS than in explained deaths (odds ratio 7.77, 95% confidence interval 2.36–25.57) and that prone sleeping was still overrepresented. Bronchopneumonia, other infections and congenital anomalies were the most common causes of explained SUDI.
Conclusion
Bed sharing and prone sleeping were more common in SIDS than in explained SUDI. Sparse data in medical records were a problem, and the authors are now working with the National Board of Health and Welfare on a project to establish new routines.
Keywords: Bed sharing, Epidemiology, Sudden infant death syndrome, Sudden unexpected death in infancy
Abbreviations
- CI
Confidence interval
- OR
Odds ratio
- SIDS
Sudden infant death syndrome
- SUDI
Sudden unexpected death in infancy
Key notes.
We investigated the environmental circumstances associated with sudden infant death syndrome (SIDS), by analysing Swedish data on all sudden unexpected deaths in infancy (SUDI) from 2005 to 2011.
All Swedish infants forensically autopsied up to one year of age were included: 136 with SIDS and 125 with explained SUDI.
Bed sharing and prone sleeping were more common in SIDS than in explained SUDI, and work is underway to tackle insufficient environmental data in medical records.
Introduction
Sudden infant death syndrome (SIDS) is defined as the death of an infant that cannot be explained, despite a thorough case investigation, including death scene investigation, autopsy and review of the clinical history 1. Sudden unexpected death in infancy (SUDI) is a term used to describe any sudden and unexpected death, whether explained or unexplained, including SIDS, which occurs during the first year of life 2.
In Sweden, as in other countries, the incidence of SIDS has decreased dramatically since the beginning of the 1990s, following the introduction of the recommended supine sleeping position for infants (Fig. 1). In 2006, the National Board of Health and Welfare in Sweden revised the guidelines to prevent SIDS, including the introduction of the advice not to share a bed with an infant if the mother was a smoker, had taken alcohol, other drugs or sedatives or if the mother was very tired 3. It was also mentioned that a pacifier could reduce the risk of SIDS 4, 5.
Figure 1.
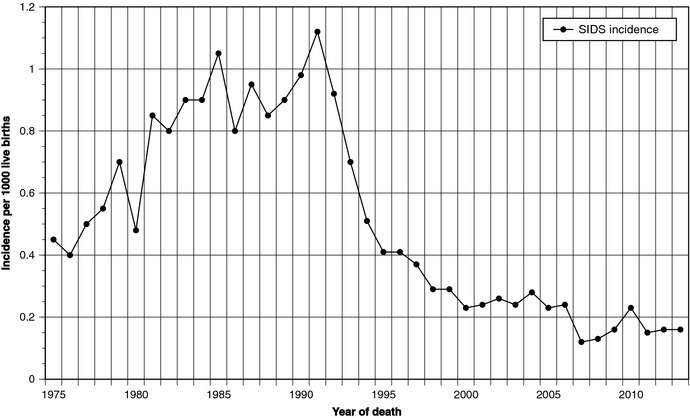
SIDS incidence per 1000 live births in Sweden in 1975–2013. Based on data from the Swedish Departments of Forensic Medicine.
The aim of this study was to investigate the environmental circumstances in infant deaths in recent years. We collected data from all cases of SUDI in Sweden from 2005 to 2011 that underwent forensic autopsy and compared cases diagnosed as SIDS with explained SUDI cases. We were particularly interested in the practice of bed sharing, defined as when the infant sleeps on the same surface as another person 6. The term ‘co‐sleeping’ is often used in the same context, but it is not synonymous, as co‐sleeping can include bed sharing or sleeping in the same room in close proximity 7. A study from 2013 demonstrated that bed sharing was a risk factor for SIDS, even in the absence of other known risk factors 8.
Methods
According to Swedish law, all cases involving young people who die suddenly and unexpectedly must be reported to the police. A forensic autopsy is then performed at the Departments of the National Board of Forensic Medicine. Although the diagnosis of SIDS demands a death scene investigation, this is very seldom carried out in Sweden, unless a crime is suspected. All infants in Sweden, aged 0–365 days, who underwent a forensic autopsy in 2005–2011, were included (n = 261). The autopsies included histological examinations and toxicological analyses. Bacteriological and virological analyses were performed in most of the cases. The classification made by the forensic examiner was used as the diagnosis. Classification codes 798A, C and X (ICD‐9) and R95 (ICD‐10) were defined as SIDS cases. In the explained SUDI cases, the cause of death was classified into different groups according to ICD‐9.
Supplementary data were obtained from the Swedish Medical Birth Register, and medical records were obtained from the hospitals for all cases. Three paediatricians (PM, BA and GW) reviewed the medical records and analysed the data.
SIDS cases and cases of explained SUDI were compared in terms of age at death, maternal age and parity, seasonality, sleeping position, breastfeeding, smoking, Apgar score, birthweight, prematurity, bed sharing and social factors, such as parental education and employment status.
In the statistical analysis, 2 × 2 tables with the chi‐square test and binary logistic regression were used. Effects were estimated using odds ratios (OR) with 95% confidence intervals (CI). For comparisons of continuous variables, we used Student's t‐test. Seasonal variations in SIDS and explained deaths were evaluated with the Edwards' and Freedman's tests 9. All other statistical calculations were carried out with the SPSS version 22 package (IBM Corp., Armonk, NY, USA).
Due to sparse data in the medical records, especially relating to environmental factors, such as the use of pacifiers, maternal alcohol use and social factors, correct statistical comparisons between SIDS and explained deaths were not possible when it came to these factors.
Ethics
The study was approved by the ethics committee at the University of Gothenburg.
Results
Of the 261 infants, 136 were defined as SIDS and 125 as explained SUDI. Age at death in SIDS cases was a median of 64 days compared with 79 days in explained deaths (p = 0.79). The number of cases of SIDS and explained SUDI in 2005–2011 and age at death are shown in Figure 2.
Figure 2.
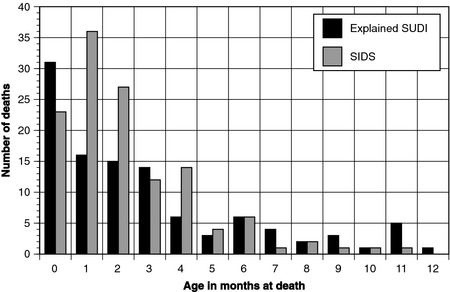
Age at death in cases of SIDS and explained SUDI in Sweden in 2005–2011.
Causes of explained SUDI
The final diagnosis was made by the forensic examiner and in most cases classified by ICD‐9. In nine cases, ICD‐10 was used and recoded by us to ICD‐9. The most common cause of death in explained SUDI was infectious diseases affecting the respiratory system (27.2%), mostly bronchopneumonia or bacterial pneumonia (Table 1). The second most common cause (16.0%) was other infectious diseases including septicaemia, bacterial meningitis and severe viral disease. Congenital anomalies were not uncommon (14.4%) as a cause of death and cardiac malformations, such as atrial septal defects, ventricular septal defects or transposition of the great vessels, dominated. Four cases of congenital anomalies of the nervous systems were also found. Conditions originating in the perinatal period (8.8%), diseases of the nervous system (8.8%) and diseases of the circulatory system (8.0%) represented other important groups. Injury and poisoning (7.2%) and metabolic disorders (4.8%) represented other common causes of death in explained SUDI. As seen in Table 1, there was a great variety of different diagnoses in each ICD chapter text. Three deaths were due to accidental suffocation and strangulation in bed (E913 in ICD‐9 and W75 in ICD‐10). One of these was a newly born baby at the maternity ward. The baby was found lifeless with the mother who had fallen asleep during breastfeeding attempts. The baby was resuscitated but died from severe anoxic brain damage after a few days. Of the other infants, one was entangled in the bed cover and one had got a hairdryer cord around his neck.
Table 1.
Causes of explained sudden unexpected death in infancy (explained SUDI) by ICD‐9 codes, n = 125
| ICD | ICD chapter text | n | % | Code (n) |
|---|---|---|---|---|
| 001‐139 | Infectious and parasitic diseases | 20 | 16.0 | Intestinal infection 008 (1), viral enteritis 008W (1), gastroenteritis 009A (1), meningococcal meningitis 036 (1), septicaemia 038 (2), streptococcal septicaemia 038A (2), staphylococcal septicaemia 038B (2), anaerobal septicaemia 038D (1), Gram negative septicaemia 038E (1), other septicaemia 038W (1), septicaemia NUD 038X (2), viral meningitis 047X (1), viral CNS disease 049X (1), RSV disease 079.6 (1), viral disease 079W (1), viral infection NUD 079X (1) |
| 140‐239 | Neoplasms | 0 | ||
| 240‐279 | Endocrine, nutritional and metabolic diseases, and immunity disorders | 6 | 4.8 | Carbohydrate metabolic disease 271X (1), lipid metabolic disease 272W (1), lipid metabolic disease NUD 272X (2), metabolic disorder NUD 277X (2) |
| 280‐289 | Diseases of the blood and blood‐forming organs | 0 | ||
| 290‐319 | Mental disorders | 0 | ||
| 320‐359 | Diseases of the nervous system | 11 | 8.8 | Encephalitis NUD 323X (1), epilepsy NUD 345X (1), anoxic brain damage 348B (4), cerebral oedema 348F (3), cerebral disorder NUD 348X (1), disorder of the nervous system NUD 349.9 (1) |
| 360‐389 | Diseases of the sense organs | 2 | 1.6 | Otitis media NUD 382X (1), ear disorder 388 (1) |
| 390‐459 | Diseases of the circulatory system | 10 | 8.0 | Acute myocardial infarction 410 (1), ischaemic heart disease NUD 411X (2), acute pericarditis 420 (1), acute myocarditis NUD 422X (1), hypertrophic cardiomyopathy 425B (1), primary cardiomyopathy NUD 425E (1), heart failure NUD 428X (1), cardiomegaly 429D (1), subarachnoid haemorrhage 430 (1) |
| 460‐519 | Diseases of the respiratory system | 34 | 27.2 | Acute bronchiolitis 466B (1), viral pneumonia RSV 480B (1), viral pneumonia NUD 480X (4), pneumococcal pneumonia 481 (2), staphylococcal pneumonia 482E (1), mycoplasma pneumonia 483 (1), bronchopneumonia 485 (14), pneumonia 486 (6), pneumonia NUD 486X (1), pneumonitis due to solids and liquids 507A (1), post inflammatory pulmonary fibrosis NUD 515X (1), other bronchial disease 519B (1) |
| 520‐579 | Diseases of the digestive system | 0 | ||
| 580‐629 | Diseases of the genitourinary system | 0 | ||
| 630‐679 | Complications of pregnancy, childbirth, and the puerperium | 4 | 3.2 | Foetal distress 656D (2), intrauterine foetal death 656E (2) |
| 680‐709 | Diseases of the skin and subcutaneous tissue | 0 | ||
| 710‐739 | Diseases of the musculoskeletal system and connective tissue | 0 | ||
| 740‐759 | Congenital anomalies | 18 | 14.4 | Congenital anomalies of the nervous system 742.2 (3), congenital anomalies of the nervous system NUD 742X (1), transposition of the great vessels 745B (2), tetralogy of Fallot 745C (2), ventricular septal defect 745E (1), atrial septal defect 745F (1), endocardial cushion defect 745G (2), anomalies of cardiac septal closure 745W (3), congenital anomalies of heart, other 746W (1), congenital anomaly of pulmonary artery 747D (1), congenital diaphragmal hernia 756G (1) |
| 760‐779 | Certain conditions originating in the perinatal period | 11 | 8.8 | Death secondary to maternal death 761G (1), death due to complication during delivery 763G (1), foetal distress 768D (1), birth asphyxia 768X (3), other respiratory condition of foetus and newborn 770 (1), neonatal sepsis 771.81 (2), adrenal haemorrhage 772F (1), necrotizing enterocolitis 777F (1) |
| 800‐999 | Injury and poisoning | 9 | 7.2 | Skull fracture 800K (1), foreign body in pharynx or larynx 933 (1), burn of upper limb 934K (1), traumatic shock 958E (1), sepsis 995.92 (1), cerebral anoxia 997A (1), accidental suffocation E913 (3) |
Cases classified as SIDS [798A (n = 120), 798C (n = 2), 798X (n = 14)] are excluded from the table.
Risk factors for SIDS
The most prominent finding was a higher prevalence of bed sharing in SIDS than in explained deaths. In the medical records, where place of sleep was stated, 93.5% of SIDS cases involved bed sharing, compared with 65.1% of explained SUDI. This gave an OR of 7.77 (2.36–25.57) for bed sharing (Table 2).
Table 2.
Incidence of potential risk factors for sudden infant death and explained deaths in infancy with odds ratios and 95% confidence intervals. ORs denote SIDS risk compared with explained SUDI. Data from medical records
| SIDS | Explained SUDI | OR | 95% CI | p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Position placeda | |||||||
| Prone | 20 | 66.7 | 10 | 33.3 | 0.73 | 0.26–2.06 | 0.80 |
| Supine | 19 | 59.4 | 13 | 40.6 | 1 | ref | ref |
| Side | 7 | 58.3 | 5 | 41.7 | 1.04 | 0.27–4.02 | 0.95 |
| Position founda | |||||||
| Prone | 42 | 60.0 | 28 | 40.0 | 4.67 | 0.54–40.03 | 0.16 |
| Supine | 13 | 46.4 | 15 | 53.6 | 1 | ref | ref |
| Side | 7 | 87.5 | 1 | 12.5 | 8.08 | 0.88–74.59 | 0.07 |
| Slept in parental beda | |||||||
| Yes | 58 | 67.4 | 28 | 32.6 | 7.77 | 2.36–25.57 | <0.001 |
| No | 4 | 21.1 | 15 | 78.9 | 1 | ref | ref |
| Any breastfeedinga | |||||||
| Yes | 75 | 58.6 | 53 | 41.4 | 2.48 | 1.29–4.76 | 0.006 |
| No | 20 | 36.4 | 35 | 63.6 | 1 | ref | ref |
| Genderb | |||||||
| Male | 86 | 53.1 | 76 | 46.9 | 0.90 | 0.55–1.49 | 0.67 |
| Female | 50 | 50.5 | 49 | 49.5 | 1 | ref | ref |
| Gestational age <37 weeksb | |||||||
| Yes | 18 | 40.9 | 26 | 59.1 | 0.49 | 0.25–0.95 | 0.036 |
| No | 109 | 58.6 | 77 | 41.4 | 1 | ref | ref |
| Birthweightb | |||||||
| <2500 g | 18 | 45.0 | 22 | 55.0 | 0.58 | 0.29–1.16 | 0.12 |
| 2500–4500 g | 107 | 58.5 | 76 | 41.5 | 1 | ref | ref |
| >4500 g | 2 | 40.0 | 3 | 60.0 | 0.47 | 0.08–2.90 | 0.42 |
| Smoking during 1st trimesterb | |||||||
| Nil | 74 | 53.2 | 65 | 46.8 | 1 | ref | ref |
| 1–9 cig/day | 30 | 68.2 | 14 | 31.8 | 1.95 | 0.96–3.97 | 0.07 |
| 10+ cig/day | 13 | 52.0 | 12 | 48.0 | 0.99 | 0.42–2.30 | 0.98 |
Data from medical records.
Data from the Medical Birth Register.
Where data were available, 67% of SIDS cases were found prone. Ten SIDS cases were placed to sleep in the side position but were found dead in the prone position. No infant was placed in the side position and found dead on its back.
Maternal smoking was considerably higher in SIDS (35.7%) than in explained SUDI (23.6%). Breastfeeding was more common among the mothers of SIDS cases than among explained SUDI (78.9% versus 60.2%, OR 2.48, 95% CI 1.29–4.76). Preterm birth was more common among explained SUDI cases.
In a multivariate model containing the univariate significant variables breastfeeding and preterm birth, bed sharing was still significant (OR 14.89, 95% CI 1.11–199.82), albeit with a broad confidence interval, due to small numbers.
We found no significant seasonal variations in SIDS and no significant difference between SIDS versus explained SUDI in terms of Caesarean section, parity or maternal age.
Due to sparse documentation in medical records, there were not enough data to analyse the use of pacifiers, alcohol use and social background. The records did show that 14 infants with SIDS and 11 infants with explained SUDI were found dead in places such as sofas, armchairs and child car seats.
Discussion
The main finding in this study was the high incidence of bed sharing in SIDS compared with explained SUDI. Where place of sleep was mentioned in the medical records, more than 90% of SIDS cases involved bed sharing compared with two‐thirds of explained SUDI. This strengthens the notion that bed sharing is a significant risk factor for SIDS 8. Compared with an earlier Swedish study, in which 20% of children were sharing a bed 10, bed sharing appeared to be more common in this study. This supports the Swedish guidelines from 2014 11 that state that the safest place for an infant of up to three months of age to sleep is in his or her own bed, in the same room as the parents.
Bed sharing should be avoided, regardless of the infant's age, if the mother is a smoker, has taken drugs or alcohol, or if the baby sleeps in a place other than the crib, usually a sofa 8, 12, 13, 14.
Why bed sharing increases the risk of SIDS is not totally understood, but it is possible that the infant's airways are obstructed by the parent's body or that the head becomes covered by a blanket or pillow 8, 15, 16. Several studies have also shown that bed sharing leads to a higher infant body temperature and thereby increases the risk of thermal stress 17, 18. Another possibility is that the infant's small jaw can be pushed backwards so that the tongue closes the upper airway 19. Also, if there is a connection between altered sleep patterns and bed sharing, this could act as an external trigger and increase the risk of SIDS 20. In a study comparing sleep characteristics in two‐month‐old infants, where infants in one group slept on their own and the infants in the other group was bed sharing, there were more reports of disturbed sleep among the infants that were bed sharing 21.
A prone sleeping position is still common in SIDS, despite the recommendation that the supine sleeping position is the safest. Where data were available, two‐thirds of SIDS cases were found prone. This can be compared with a Swedish study that showed that 5.6% of the population of six‐month‐old infants slept prone in 2004 22. Assuming that all infants with missing data on sleep position were sleeping supine, the prone sleepers would still represent a third of SIDS infants.
If the infant is placed in the side position, there is a risk that it can roll over into a prone position, which increases the risk of SIDS, especially if the baby is not used to sleeping prone 23. We found that several SIDS cases were placed on their side, but were found dead in the prone position, while no infant was placed on its side and found dead on its back. This emphasises that the side position is not stable 24 and that the risk of SIDS is greatly increased when a child who is not used to the prone position rolls over 23.
Maternal smoking is a well‐known environmental factor that makes it more difficult for the vulnerable child to respond when oxygen saturation falls 25 and both the SIDS and explained deaths showed higher frequencies than comparable national Swedish figures (10%). The fact that maternal smoking is more common in SIDS than in SUDI has been reported before in two major case–control studies. The present data show that maternal smoking is a risk factor not only for SIDS but also for explained SUDI 26, 27, 28.
When it was documented, breastfeeding was less common in explained SUDI than in SIDS. This may reflect the fact that the infants with explained deaths had more frequently been ill, preterm or both and that the mother had therefore had difficulty to initiate breastfeeding. However, breastfeeding in the general population was more frequent than in both SIDS and explained SUDI.
The median age at death in the SIDS cases in this study was the same as in our earlier Swedish study in 1997–2005, which was 64 days 29. There was no statistically significant difference between SIDS cases and explained SUDI cases regarding age at death.
From the present study, we conclude that there are three highly important measures to be taken to further reduce the incidence of SIDS in Sweden: firstly, avoid bed sharing until three months of age as a matter of routine and extend this period if the parents have risk factors such as maternal smoking; secondly, always place infants to sleep supine; and thirdly, reduce maternal smoking still further. This provides an opportunity for targeted information in prenatal care and at child healthcare centres.
This study also provides new information about the causes of explained infant deaths in Sweden. Infectious diseases, such as sepsis or localised infections in the lungs, brain and heart, are the most common causes of explained SUDI. This is in line with case–control studies from Germany 26 and England 27. Malformations in the heart and the central nervous system, as well as perinatal events leading to asphyxia, are other important causes. Metabolic disorders, involving lipid synthesis, for example, and trauma or violence are quite uncommon and together represent less than every tenth death. Trauma and violence are preventable in most circumstances, and there is a need for further, more detailed studies of this.
We found three infant deaths diagnosed as accidental suffocation or strangulation in the bed (E913 in ICD‐9 and W75 in ICD‐10). One of the deaths occurred in the maternity ward shortly after birth and demonstrates that when placed skin‐to‐skin, the newly born baby can have problems keeping its airways free. This may be unnoticed by a mother who is exhausted by the delivery. It should therefore be stressed that when a newly born baby is placed skin‐to‐skin, for example to initiate breastfeeding, checks must be made to ensure that breathing is free. The two other deaths illustrate the importance of safe bedding environment.
A study from New Zealand 30 has shown that accidental suffocation is not an uncommon cause of sudden unexpected infant death, particularly in a bed‐sharing situation. During sleep, accidental suffocation may occur due to overlaying or wedging of the infant. The risk is most prominent during the first months of life. The reason why we have few diagnosed cases of accidental suffocation in our study is probably the lack of routine death scene investigations in Sweden. We believe that death scene investigation would improve the validity of the final diagnoses in cases of SUDI. Also, it would add to our knowledge of unsafe sleeping conditions and make it possible to prevent such deaths.
Finally, this study shows that Swedish paediatric records must be improved in SUDI cases. The authors, together with the Swedish National Board of Health and Welfare and Swedish National Board of Forensic Medicine, have initiated a project to promote this. In the future, we hope to be able to study environmental factors on a yearly basis, which will give us the opportunity to notice changes and communicate this to the public, with the goal of reducing the incidence of SIDS still further.
Funding
The study was supported by the Sahlgrenska Academy at the University of Gothenburg, Queen Silvia Children's Hospital Research Foundation and the Health and Medical Care Committee of the Regional Executive Board, Västra Götaland Region, Sweden.
Acknowledgement
We thank Mainor Åmark, RN, for valuable help with the data collection.
References
- 1. Krous HF, Beckwith JB, Byard RW, Rognum TO, Bajanowski T, Corey T, et al. Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics 2004; 114: 234–8. [DOI] [PubMed] [Google Scholar]
- 2. Task Force on Sudden Infant Death Syndrome , Moon RY. SIDS and other sleep‐related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics 2011; 128: 1030–9. [DOI] [PubMed] [Google Scholar]
- 3. Socialstyrelsen [National Board of Health and Welfare] . Minska risken för plötslig spädbarnsdöd [Reducing the risk of cot death]. Stockholm: Socialstyrelsen, 2006. Artikelnr 2006‐114‐40. [Google Scholar]
- 4. Hauck FR, Omojokun OO, Siadaty MS. Do pacifiers reduce the risk of sudden infant death syndrome? A meta‐analysis. Pediatrics 2005; 116: e716–23. [DOI] [PubMed] [Google Scholar]
- 5. Mitchell EA, Blair PS, L'Hoir MP. Should pacifiers be recommended to prevent sudden infant death syndrome? Pediatrics 2006; 117: 1755–8. [DOI] [PubMed] [Google Scholar]
- 6. McKenna JJ, Ball HL, Gettler LT. Mother‐infant cosleeping, breastfeeding and sudden infant death syndrome: what biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am J Phys Anthropol 2007; 134(Suppl. 45): 133–61. [DOI] [PubMed] [Google Scholar]
- 7. McKenna JJ, Thoman EB, Anders TF, Sadeh A, Schectman VC, Glotzbach SF. Infant‐parent co‐sleeping in an evolutionary perspective: implications for understanding infant sleep development and the sudden infant death syndrome. Sleep 1993; 16: 263–82. [DOI] [PubMed] [Google Scholar]
- 8. Carpenter R, McGarvey C, Mitchell EA, Tappin DM, Vennemann MM, Smuk M, et al. Bed sharing when parents do not smoke: is there a risk of SIDS? An individual level analysis of five major case‐control studies. BMJ Open 2013; 3: e002299. doi:10.1136/bmjopen‐2012‐002299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gahlinger PM, Abramson JH. Computer Programs for Epidemiologic analysis: PEPI Version 2. Stone Mountain, Georgia: USD Inc, 1995. [Google Scholar]
- 10. Möllborg P, Wennergren G, Norvenius SG, Alm B. Bed‐sharing among six‐month‐old infants in western Sweden. Acta Paediatr 2011; 100: 226–30. [DOI] [PubMed] [Google Scholar]
- 11. Socialstyrelsen [National Board of Health and Welfare] . Minska risken för plötslig spädbarnsdöd [Reducing the risk of cot death]. 2014; Available at: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19370/2014-3-3.pdf (accessed 21 April 2015). [Google Scholar]
- 12. Blair PS, Sidebotham P, Evason‐Coombe C, Edmonds M, Heckstall‐Smith EM, Fleming P. Hazardous cosleeping environments and risk factors amenable to change: case‐control study of SIDS in south west England. BMJ 2009; 339: b3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tappin D, Ecob R, Brooke H. Bedsharing, roomsharing, and sudden infant death syndrome in Scotland: a case‐control study. J Pediatr 2005; 147: 32–7. [DOI] [PubMed] [Google Scholar]
- 14. Blair PS, Fleming PJ, Bensley D, Smith I, Bacon C, Taylor E, et al. Smoking and the sudden infant death syndrome. Results from 1993‐5 case‐control study for confidential inquiry into stillbirths and deaths in infancy. Confidential inquiry into Stillbirths and Deaths Regional Coordinators and Researchers. BMJ 1996; 313: 195–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schlaud M, Dreier M, Debertin AS, Jachau K, Heide S, Giebe B, et al. The German case‐control scene investigation study on SIDS: epidemiological approach and main results. Int J Legal Med 2010; 124: 19–26. [DOI] [PubMed] [Google Scholar]
- 16. Blair PS, Mitchell EA, Heckstall‐Smith EM, Fleming PJ. Head covering – a major modifiable risk factor for sudden infant death syndrome: a systematic review. Arch Dis Child 2008; 93: 778–83. [DOI] [PubMed] [Google Scholar]
- 17. Williams SM, Taylor BJ, Mitchell EA. Sudden infant death syndrome: insulation from bedding and clothing and its effect modifiers. The National Cot Death Study Group. Int J Epidemiol 1996; 25: 366–75. [DOI] [PubMed] [Google Scholar]
- 18. Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Sauerland C, Mitchell EA. Sleep environment risk factors for sudden infant death syndrome: the German Sudden Infant Death Syndrome Study. Pediatrics 2009; 123: 1162–70. [DOI] [PubMed] [Google Scholar]
- 19. McIntosh CG, Tonkin SL, Gunn AJ. What is the mechanism of sudden infant deaths associated with co‐sleeping? N Z Med J 2009; 122: 69–75. [PubMed] [Google Scholar]
- 20. Kahn A, Groswasser J, Franco P, Scaillet S, Sawaguchi T, Kelmanson IA, et al. Factors influencing the determination of arousal thresholds in infants–a review. Sleep Med 2000; 1: 273–8. [DOI] [PubMed] [Google Scholar]
- 21. Kelmanson IA. Sleep disturbances in two‐month‐old infants sharing the bed with parent(s). Minerva Pediatr 2010; 62: 161–9. [PubMed] [Google Scholar]
- 22. Alm B, Möllborg P, Erdes L, Pettersson R, Åberg N, Norvenius G, et al. SIDS risk factors and factors associated with prone sleeping in Sweden. Arch Dis Child 2006; 91: 915–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber J, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet 2004; 363: 185–91. [DOI] [PubMed] [Google Scholar]
- 24. Skadberg BT, Morild I, Markestad T. Abandoning prone sleeping. Effect on the risk of sudden infant death syndrome. J Pediatr 1998; 132: 340–3. [DOI] [PubMed] [Google Scholar]
- 25. Kato I, Franco P, Groswasser J, Scaillet S, Kelmanson I, Togari H, et al. Incomplete arousal processes in infants who were victims of sudden death. Am J Respir Crit Care Med 2003; 168: 1298–303. [DOI] [PubMed] [Google Scholar]
- 26. Vennemann M, Bajanowski T, Butterfass‐Bahloul T, Sauerland C, Jorch G, Brinkmann B, et al. Do risk factors differ between explained sudden unexpected death in infancy and sudden infant death syndrome? Arch Dis Child 2007; 92: 133–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Platt MW, Blair P, Fleming P, Smith I, Cole T, Leach C, et al. A clinical comparison of SIDS and explained sudden infant deaths: how healthy and how normal? Arch Dis Child 2000; 82: 98–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Leach CE, Blair PS, Fleming PJ, Smith IJ, Platt MW, Berry PJ, et al. Epidemiology of SIDS and explained sudden infant deaths. Pediatrics 1999; 104: e43. [DOI] [PubMed] [Google Scholar]
- 29. Möllborg P, Alm B. Sudden infant death syndrome during low incidence in Sweden 1997–2005. Acta Paediatr 2010; 99: 94–8. [DOI] [PubMed] [Google Scholar]
- 30. Hayman RM, McDonald G, Baker NJ, Mitchell EA, Dalziel SR. Infant suffocation in place of sleep: New Zealand national data 2002–2009. Arch Dis Child 2014. doi:10.1136/archdischild‐2014‐306961. [DOI] [PubMed] [Google Scholar]


