Abstract
Aim
To provide estimates of the costs of severe and non‐severe insulin‐related hypoglycaemia in the UK using the Local Impact of Hypoglycaemia Tool.
Methods
Rates of hypoglycaemia were extracted from the UK Hypoglycaemia Study Group observational study. The costs of severe and non‐severe hypoglycaemic episodes in insulin‐treated adults with Type 1 and Type 2 diabetes were estimated from UK data sources. The rates and costs were then applied to specific populations to give an estimate of the cost of insulin‐related hypoglycaemia for the UK, a specific locality, or a user‐defined population. User‐specific rates and costs could also be applied.
Results
The estimated cost of a hypoglycaemic episode can range from as much as £2,152 for severe episodes (for which the patient is admitted to hospital) to as little as £1.67 for non‐severe episodes. With a UK population of 64.1 million, the total estimated cost of managing insulin‐related hypoglycaemia is £468.0 m per year (£295.9 m for severe episodes, £172.1 m for non‐severe episodes). On a local health economy level, using a hypothetical general population of 100 000, the total cost of managing insulin‐related hypoglycaemia is estimated to be £730,052 per year (£461,658 for severe and £268,394 for non‐severe episodes).
Conclusions
The Local Impact of Hypoglycaemia Tool highlights the economic burden of insulin‐related hypoglycaemia. Non‐severe episodes are often overlooked because of their low individual cost, but their high frequency makes the cumulative cost substantial. The Local Impact of Hypoglycaemia Tool also shows clinicians and budget‐holders the economic impact of lower rates of hypoglycaemia.
What's new?
The combination of published research and data from multiple UK sources has led to the development of a novel model to identify the economic burden of insulin‐related hypoglycaemia in the UK and offers an opportunity for its better management in the future.
This is the first example of an innovative model allowing the user to estimate the cost of insulin‐related hypoglycaemia not only on a national level, but also within any specific locality in the UK, whether it is a Primary Care Organization, a general practice or a user‐defined population.
What's new?
The combination of published research and data from multiple UK sources has led to the development of a novel model to identify the economic burden of insulin‐related hypoglycaemia in the UK and offers an opportunity for its better management in the future.
This is the first example of an innovative model allowing the user to estimate the cost of insulin‐related hypoglycaemia not only on a national level, but also within any specific locality in the UK, whether it is a Primary Care Organization, a general practice or a user‐defined population.
Introduction
Diabetes mellitus
Diabetes is a chronic metabolic condition characterised by elevated blood glucose levels (hyperglycaemia). In the UK there are 3.2 million adults diagnosed with diabetes, corresponding to 6.0% of the adult population 1. Hyperglycaemia is associated with an increased risk of cardiovascular disease, kidney disease, eye disease, amputation and depression 1.
Hypoglycaemia
Hypoglycaemia occurs when blood glucose levels drop to below normal (defined as < 3.9 mmol/l by the American Diabetes Association 2), and is accompanied by symptoms such as anxiety, palpitations, weakness and confusion 3. In severe cases, hypoglycaemia can cause seizure, loss of consciousness, coma and even death 3. Insulin therapy is the antidiabetic treatment that is most associated with hypoglycaemia.
Hypoglycaemia may be severe or non‐severe, and may occur at any time of day or night. It is defined as severe when assistance from another individual is required, and non‐severe when it can be self‐treated 4. People in the UK with Type 1 diabetes mellitus treated with insulin for > 15 years are reported to experience, on average, 3.2 severe and 29.0 non‐severe hypoglycaemic episodes per year, whereas the rate is 0.7 severe and 10.2 non‐severe per year for people with Type 2 diabetes mellitus treated with insulin for > 5 years 5.
Current treatments
The current UK diabetes clinical guidelines referring to the use of basal insulin treatments are summarised in Table 1 6, 7, 8 . Insulin therapy is required for all people with Type 1 diabetes. Other glucose‐lowering medications are available for people with Type 2 diabetes, including oral agents (that can be used in a variety of combinations) such as metformin, sulphonylureas, glinides, thiazolidinediones, sodium/glucose co‐transporter 2 inhibitors, α‐glucosidase inhibitors and dipeptidyl peptidase‐4 inhibitors, and injectable treatments such as glucagon‐like peptide‐1 receptor agonists. Nevertheless, insulin therapy is eventually required for a considerable proportion of people with Type 2 diabetes, because of the progressive nature of the disease and the decline in endogenous insulin production over time. While hypoglycaemia is a recognised adverse effect of sulphonylurea therapy, the greatest burden of hypoglycaemia is associated with exogenous insulin therapy.
Table 1.
UK diabetes clinical guidelines referring to the use of basal insulin treatments
| NICE (Type 1 diabetes) 6 | Basal insulin supply should be provided by NPH insulin or a basal insulin analogue. Recommend long‐acting insulin analogues when nocturnal hypoglycaemia is a problem on isophane (NPH) insulin. |
| NICE (Type 2 diabetes) 7 | Begin with human NPH insulin. Recommend long‐acting insulin analogues if the person's lifestyle is restricted by recurrent symptomatic hypoglycaemic episodes, the person does not reach their target HbA1c because of significant hypoglycaemia, or the person experiences significant hypoglycaemia on NPH insulin irrespective of the level of HbA1c reached. With Type 2 diabetes, insulin treatment is a last‐line therapy after diet, exercise and other antidiabetic agents. |
| SIGN (Type 1 diabetes) 8 | Recommend basal insulin analogues in people who are experiencing severe or nocturnal hypoglycaemia and who are using an intensified insulin regimen. People who are not experiencing severe or nocturnal hypoglycaemia may use basal analogues or NPH insulin. Continuous subcutaneous insulin infusion therapy should be considered in people who experience recurring episodes of severe hypoglycaemia. |
| SIGN (Type 2 diabetes) 8 | Recommend an HbA1c target of 53 mmol/mol [7.0%] (48 mmol/mol [6.5%] may be appropriate at diagnosis). Once‐daily bedtime NPH insulin should be used when adding insulin to metformin and/or sulphonylurea therapy. Basal insulin analogues should be considered if there are concerns regarding hypoglycaemia risk. |
Economic burden of hypoglycaemia
Hypoglycaemia is associated with substantial costs, including both direct costs (ambulance services, accident and emergency admissions, hospitalisation, healthcare professional visits, use of glucose and glucagon preparations and extra blood glucose testing) 9, 10 and indirect costs (working time lost as a result of a hypoglycaemic episode) 4.
A reduction in hypoglycaemia, achieved, for example, by changing insulin treatment to a treatment with a lower hypoglycaemic risk, may result in lower costs to the National Health Service (NHS) and wider society.
Aims
In developing the Local Impact of Hypoglycaemia Tool (LIHT), the aim was to provide estimates of the costs of severe and non‐severe insulin‐related hypoglycaemia in the UK, and specifically at the Primary Care Organisation or general practice population level. The focus of the model was on insulin‐treated patients with diabetes only, as insulin is the antidiabetic treatment most associated with hypoglycaemia, and the widest body of published data is available for hypoglycaemia in insulin‐treated people with diabetes.
Methods
Key functions of the Local Impact of Hypoglycaemia Tool
The LIHT is used to perform calculations based on UK epidemiological data, insulin usage and healthcare unit costs and utilisation values, which can be applied to a geographical or user‐defined general population (Fig. 1).
Figure 1.
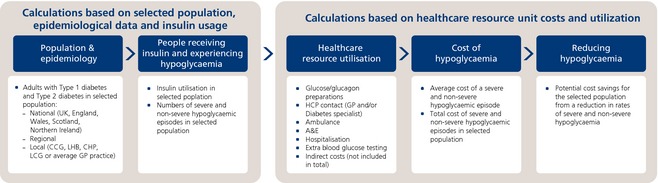
Descriptive flow of calculations performed by the Local Impact of Hypoglycaemia Tool. Abbreviations: A&E, accident and emergency; CCG, clinical commissioning group; CHP, Community Health Partnership; GP, general practitioner; HCP, healthcare professional; LCG, local commissioning group; LHB, Local Health Board; LIHT, Local Impact of Hypoglycaemia Tool.
The user can input specific data to indicate the population size, as well as the prevalence of diabetes, percentage of people receiving insulin, rates of severe and non‐severe hypoglycaemia, percentage of severe episodes that are treated in the community or in hospital, as opposed to at home or at work, and the individual costs and utilisation of healthcare resources. These inputs can be entered for people with Type 1 diabetes and Type 2 diabetes separately, and are used to calculate the direct costs of hypoglycaemia.
The LIHT can also be used to calculate indirect costs, and the user can edit the mean weekly salary, number of working days per week, percentage of people employed, and the average number of working days lost as a result of severe or non‐severe hypoglycaemic episodes to customise the calculations.
Data retrieval
A structured literature review was conducted (available from the authors on request) to identify published papers reporting rates and resource utilisation values associated with hypoglycaemia in insulin‐treated people with diabetes within the UK. The Medline, EMBASE, NHS EED and EconLIT databases were searched, and publications were limited to those in the English language and to population‐based, observational, non‐randomised controlled trials conducted in the UK. The search highlighted the lack of data on hypoglycaemia rates and resource use for the treatment of severe and non‐severe episodes; however, the key studies identified in the review were the UK Hypoglycaemia Study Group 2007 study 5 (for rates of severe and non‐severe hypoglycaemia) and Hammer et al. 10, Leese et al. 11 and Brod et al. 4 (for resource utilisation associated with hypoglycaemia).
Rates of hypoglycaemia for the model were obtained from the UK Hypoglycaemia Study Group study 5, which was identified by the literature review as having the most complete and comprehensive data on severe and non‐severe hypoglycaemia rates in people with Type 1 diabetes and Type 2 diabetes.
Resource utilisation values (Fig. 2) were extracted from NHS data 12, two publications 4, 11, and National Institute for Health and Care Excellence (NICE) quality standards 13. The publication by Leese et al. 11 is the only publication to give absolute numbers of people using an ambulance, accident and emergency and hospital after severe hypoglycaemic episodes. The publication by Brod et al. 4 concerned non‐severe hypoglycaemia resource utilisation. It found that 25.7% of people visited a healthcare professional after a non‐severe hypoglycaemic episode (this included a general practitioner, diabetes clinic or nurse but was assumed to be a general practitioner in the model), and that people used an average of 6.2 extra blood glucose tests after a non‐severe episode. No data were found for the use of extra self‐monitoring of blood glucose tests after a severe episode; therefore values were conservatively assumed to be the same as those for non‐severe episodes.
Figure 2.
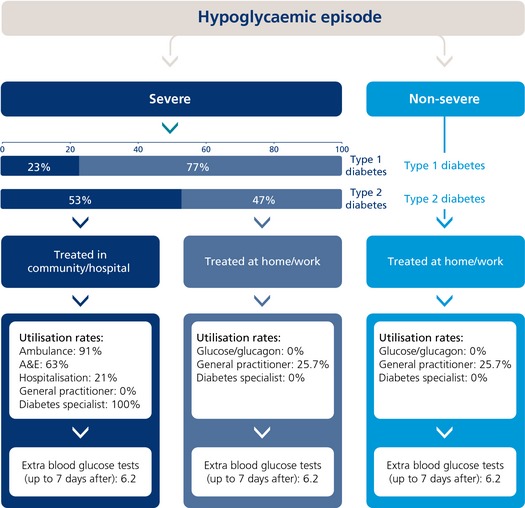
Treatment pathway and healthcare resource utilisation values. A&E, accident and emergency.
Healthcare resource unit costs (Table 2) were obtained from the Personal Social Services Research Unit 14 and the Department of Health 12, 15. Population size estimates were retrieved from NHS 18, 19 and government 20, 21 data, and diabetes prevalence was obtained from Diabetes UK 1. NICE pathways 22, 23 were used to obtain the proportions of people with Type 1 diabetes and Type 2 diabetes receiving insulin.
Table 2.
Unit costs for healthcare resources
| Treatment/service | Cost | Description (code) | Reference |
|---|---|---|---|
| Healthcare professional (general practitioner) visit | £45.00 | Cost per patient contact lasting 11.7 minutes | Personal Social Services Research Unit 14 |
| Healthcare professional (diabetes specialist) visit | £139.00 | Cost of medical consultant, per contract hour, with qualifications | Personal Social Services Research Unit 14 |
| Ambulance use | £230.00 | Ambulance services: see and treat and convey (ASS02) | Department of Health 12 |
| Accident and emergency admission | £77.00 | Category 1 investigation with category 1–2 treatment (VB09Z) | Department of Health 15 |
| Hospitalisation | £1,704.00 (average of the two tariff codes, £2,156 and £1,251) | Diabetes with hypoglycaemic disorders, 70 years and over, non‐elective spell tariff (KB01A); Diabetes with hypoglycaemic disorders, 69 years and under, non‐elective spell tariff (KB01B) | Department of Health 15 |
| Blood glucose test | £0.27 | Blood glucose test, OneTouch® Ultra™,50 = £11.99; Blood lancet, OneTouch® Ultrasoft™, 100 = £3.49 | MIMS 17 |
| Mean weekly salary (used for indirect costs) | £449.00 | Labour Market Statistics | Office for National Statistics 16 |
Cost calculations
To calculate the average direct cost per severe and non‐severe hypoglycaemic episode, the healthcare resource unit costs (Table 2) were applied to the treatment pathway and resource utilisation values shown in Fig. 2. All non‐severe episodes were assumed to be treated at home or work, whereas severe episodes could either be treated at home or work (by a friend, relative or colleague), or in community settings (out‐of‐hours clinics, NHS walk‐in centres and specialist centres) or hospital. The average cost per hypoglycaemic episode was then multiplied by the estimated number of severe and non‐severe episodes per year for people with Type 1 diabetes and Type 2 diabetes within the population of interest to calculate the total annual costs associated with hypoglycaemia.
Hypoglycaemic episodes treated at home or work have a small cost to the NHS, with people visiting their general practitioner after 25.7% of non‐severe episodes 4 (also assumed for severe episodes treated at home/work); however, some severe episodes (23% with Type 1 diabetes, 53% with Type 2 diabetes) require other more costly NHS resources, such as ambulances, accident and emergency care, and hospitalisation 10. The study by Leese et al. 11 showed that, among severe hypoglycaemic episodes using a NHS hospital over the course of 1 year, 91% required an ambulance, 63% resulted in admission to accident and emergency and 21% required hospitalisation. Upon discharge, patients need to be seen by a healthcare professional, with NICE quality standards recommending a diabetes specialist when medical attention was required 13. Glucose and glucagon utilisation values were set to zero because of insufficient data and to avoid possible double counting if included in the ambulance tariff; however, the costs are included in the model so that the user can input specific utilisation values if known.
Indirect costs
Indirect costs were calculated using the percentage of adults employed and the UK mean weekly salary, obtained from the Office for National Statistics 16. The average number of days worked per week was calculated from the average annual hours worked from the Organisation of Economic Co‐operation and Development statistics 24, assuming 52 weeks per year, 5 working days per week, and 7.5 working hours per day. A weighted average of lost productivity (0.37 days) attributable to missing work after a non‐severe episode was calculated from data from a study by Brod et al. 4; because of a lack of data, this was also conservatively assumed for severe episodes.
Results
The calculated direct cost of a hypoglycaemic episode can range from as much as £2,152 for severe episodes (where the patient is admitted to hospital), although this can increase in the case of an extended hospital stay, to as little as £1.67 for a non‐severe episode. The maximum cost of £2,152 was derived from the cost of a severe episode in which the patient was admitted to hospital, required an ambulance and used the accident and emergency department. The minimum cost of £1.67 is the cost of using 6.2 extra blood glucose tests after a hypoglycaemic episode.
The direct cost for an average hypoglycaemic episode was estimated to be £184.15 for a severe episode in insulin‐treated people with Type 1 diabetes, £407.08 for a severe episode in insulin‐treated people with Type 2 diabetes, and £13.24 for a non‐severe episode; the breakdown per resource is shown in Fig. 3. The average cost of a severe episode is lower for people with Type 1 diabetes than for those with Type 2 diabetes because of a lower utilisation of healthcare resources (ambulance, hospital and healthcare professional consultations). This is probably attributable to, on average, a longer duration of diabetes for people with Type 1 diabetes and a consequent familiarity, of them and their friends and family, with hypoglycaemia and its symptoms.
Figure 3.
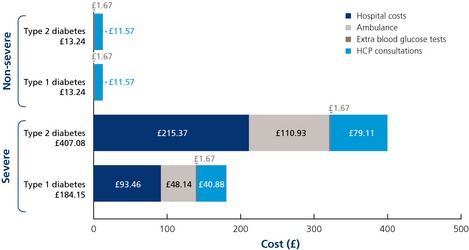
Cost breakdown for direct costs per resource for an average hypoglycaemic episode. HCP, healthcare professional.
The total direct cost of insulin‐related hypoglycaemia in the UK is estimated to be £468.0 million per year (Table 3). £295.9 m of this cost is attributable to severe episodes, and £172.1 m is attributable to non‐severe episodes, the latter being a cost that is often overlooked or underestimated. The cost of hypoglycaemia for a hypothetical general population of 100 000 is £730,052 (Table 3). Although there are many more insulin‐treated people with Type 2 diabetes than Type 1 diabetes in the UK, the total costs are higher for people with Type 1 diabetes as they have far more hypoglycaemic episodes per year (despite the lower cost per severe episode).
Table 3.
Cost breakdown for direct costs for hypoglycaemic episodes in the UK (population 64 105 654) and a sample general population of 100 000
| Population | Severe | Non‐severe | Total | |
|---|---|---|---|---|
| UK (64 105 654) | Type 1 diabetes (303 861 people) | £179,057,682 | £116,661,581 | £295,719,263 |
| Type 2 diabetes (2 734 747 people) | £116,890,685 | £55,394,137 | £172,284,822 | |
| Total | £295,948,367 | £172,055,718 | £468,004,085 | |
| Sample general population (100 000) | Type 1 diabetes (474 people) | £279,317 | £181,983 | £461,300 |
| Type 2 diabetes (4266 people) | £182,341 | £86,411 | £268,752 | |
| Total | £461,658 | £268,394 | £730,052 |
Indirect costs attributable to loss of work productivity were calculated to be £28.01 per hypoglycaemic episode, based on the average time lost for non‐severe episodes 4 (also assumed for severe).
Once aggregated, the indirect costs are substantial, estimated to be £399.4 m per year for the UK and £622,986 for a sample population of 100 000 (Table 4). They are dominated by non‐severe episodes, because of their higher rate compared with severe episodes; however, if a true value were known for the lost productivity attributable to a severe episode, these costs would probably be significantly higher.
Table 4.
Cost breakdown for indirect costs for hypoglycaemic episodes in the UK (population 64 105 654) and a sample general population of 100 000
| Population | Severe | Non‐severe | Total | |
|---|---|---|---|---|
| UK (64 105 654) | Type 1 diabetes (303 861 people) | £27,240,364 | £246,865,798 | £274,106,162 |
| Type 2 diabetes (2 734 747 people) | £8,044,420 | £117,218,691 | £125,263,111 | |
| Total | £35,284,784 | £364,084,489 | £399,369,273 | |
| Sample general population (100 000) | Type 1 diabetes (474 people) | £42,493 | £385,092 | £427,585 |
| Type 2 diabetes (4266 people) | £12,549 | £182,852 | £195,401 | |
| Total | £55,042 | £567,944 | £622,986 |
The indirect costs are not included in the final cost summary in the LIHT, as they do not directly affect the clinician or NHS budget‐holder, but are an indication of the additional economic burden of hypoglycaemia on the wider society.
Sensitivity analysis
A number of sensitivity analyses were performed on the model.
Rates of severe and non‐severe hypoglycaemic episodes were varied separately in a one‐way sensitivity analysis (Table 5), and in combination in a two‐way sensitivity analysis (Table 6), to illustrate the potential savings from a lower incidence of hypoglycaemia.
Table 5.
Costs associated with rates of hypoglycaemia in a sample general population of 100 000†
| Severe | Saving/loss (severe) | Non‐severe | Saving/loss (non‐severe) | Total cost | Total saving/loss (severe and non‐severe) | |
|---|---|---|---|---|---|---|
| 50% reduction | £230,829 | £230,828 | £134,197 | £134,197 | £365,026 | £365,025 |
| 40% reduction | £276,994 | £184,663 | £161,036 | £107,358 | £438,030 | £292,021 |
| 30% reduction | £323,160 | £138,497 | £187,876 | £80,518 | £511,036 | £219,015 |
| 20% reduction | £369,326 | £92,331 | £214,715 | £53,679 | £584,041 | £146,010 |
| 10% reduction | £415,491 | £46,166 | £241,555 | £26,839 | £657,046 | £73,005 |
| Default | £461,657 | – | £268,394 | – | £730,052 | – |
| 10% increase | £507,823 | –£46,166 | £295,233 | –£26,839 | £803,056 | –£73,005 |
| 20% increase | £553,989 | –£92,331 | £322,073 | –£53,679 | £876,062 | –£146,010 |
| 30% increase | £600,154 | –£138,497 | £348,912 | –£80,518 | £949,066 | –£219,015 |
| 40% increase | £646,320 | –£184,663 | £375,752 | –£107,358 | £1,022,072 | –£292,021 |
| 50% increase | £692,486 | –£230,828 | £402,591 | –£134,197 | £1,095,077 | –£365,025 |
Table 6.
Total hypoglycaemia costs associated with rates of severe and non‐severe hypoglycaemia in a sample general population of 100 000
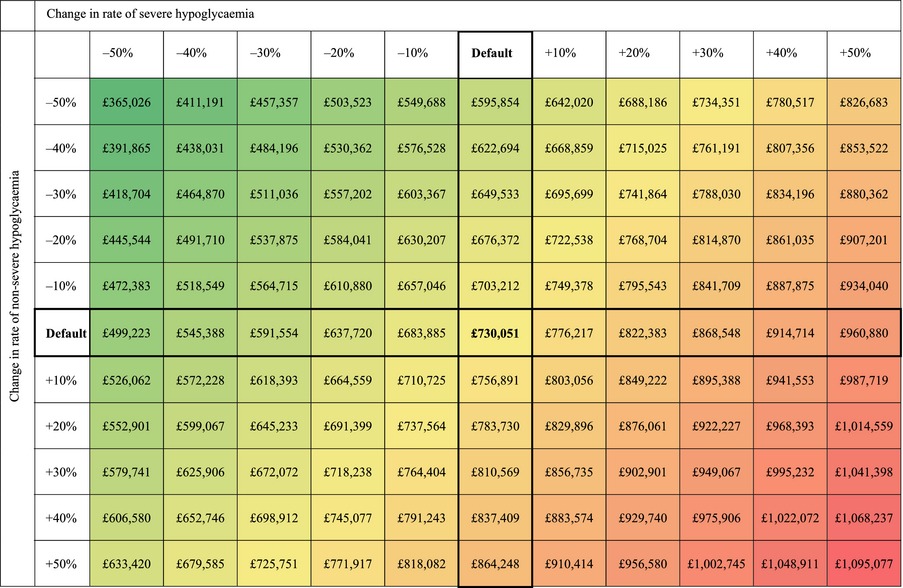
Hypoglycaemia can be difficult to manage, and, even with optimum treatment, is impossible to eradicate completely, as it is also dependent on behaviour and lifestyle. Modern insulin treatments, however, are associated with a lower risk of hypoglycaemia with equivalent glycaemic control compared with neutral protamine Hagedorn (NPH) insulin 25. A reduction in hypoglycaemia of 10–50% was therefore deemed plausible.
A 25% reduction in hypoglycaemia rates (similar to the reduction found for insulin analogues compared with NPH insulin) results in substantial cost savings of £182,513 for a sample population of 100 000, equating to £117.0 m for the UK.
A sensitivity analysis was also performed that varied all the unit costs and the percentage utilisation of resources by ± 20%, with the exception of the cost of extra blood glucose testing, which used the cheapest (£0.14) and most expensive (£0.39) blood glucose tests in MIMS 2014 17 as the lower and upper limits. The main driver of the model is the percentage utilisation of a diabetes specialist for non‐severe and severe episodes treated at home/work (set to 0% as default, as those who contacted a healthcare professional were assumed to have contacted their general practitioner only). The next two main drivers are associated with hospitalisation. The top 10 drivers of the model are shown in Fig. 4.
Figure 4.
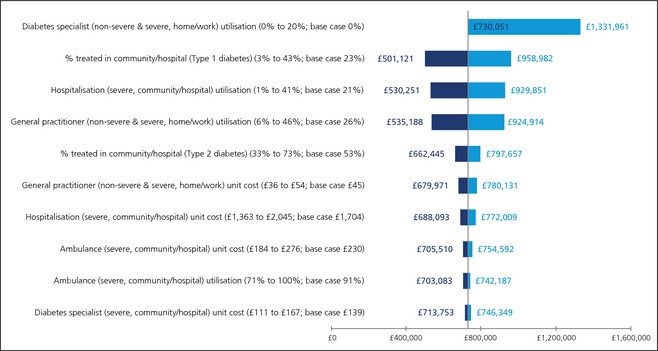
A tornado diagram of the 10 main drivers of the model for a sample general population of 100 000.
Additionally, the prevalence rates of diabetes in adults vary throughout the UK for different localities, from 3.5 to 8.9% 20; therefore, the costs of hypoglycaemia were calculated for different prevalence rates within this range (Table 7).
Table 7.
Variation of cost of hypoglycaemia with diabetes prevalence for a sample general population of 100 000
| Prevalence | Severe | Non‐severe | Total |
|---|---|---|---|
| 3.5% | £269,300 | £156,563 | £425,863 |
| 4.0% | £307,771 | £178,929 | £486,701 |
| 4.5% | £346,243 | £201,295 | £547,538 |
| 5.0% | £384,714 | £223,662 | £608,376 |
| 5.5% | £423,186 | £246,028 | £669,214 |
| 6.0% (base case) | £461,657 | £268,394 | £730,051 |
| 6.5% | £500,129 | £290,760 | £790,889 |
| 7.0% | £538,600 | £313,126 | £851,726 |
| 7.5% | £577,071 | £335,492 | £912,564 |
| 8.0% | £615,543 | £357,859 | £973,402 |
| 8.5% | £654,014 | £380,225 | £1,034,239 |
| 8.9% | £684,792 | £398,118 | £1,082,909 |
Discussion
The results of the present study indicate a substantial cost to the NHS for hypoglycaemia, both severe and non‐severe, in insulin‐treated adults with diabetes. Budget‐holders now have the facility to offset costs of new insulin treatments with the cost of hypoglycaemia, based on the hypoglycaemia profile of the new insulin. It is, however, important to recognise that multiple factors beyond the choice of insulin contribute to hypoglycaemia rates. In particular, the availability of structured patient education strategies is important. This model thus also enables local budget‐holders to offset costs for the provision of education programmes in relation to potential reductions in the economic burden of hypoglycaemia. Additionally, there are other antidiabetic medicines for people with Type 2 diabetes, such as glucagon‐like peptide‐1 receptor agonists and sodium‐glucose co‐transporter‐2 inhibitors, which are associated with a reduced risk of hypoglycaemia. Most of the glucose‐lowering drugs, however, may be used in various combinations and, when combined with insulin, sulphonylureas or glinides, the benefit of a low hypoglycaemia risk with these drugs may be partly attenuated. There are also certain patient groups with an inherently higher risk of hypoglycaemia, such as patients with recurrent hypoglycaemia, hypoglycaemia unawareness, chronic kidney disease stage 4/5, and the elderly, and interventions should perhaps be focused on reducing the rates (and therefore costs) of hypoglycaemia among these patients.
There are also multiple patient‐level considerations beyond the healthcare‐related economic burden of hypoglycaemia, namely significant detrimental effects on health‐related quality of life 26. Hypoglycaemia and the fear of hypoglycaemia, both from a patient and a healthcare professional perspective, can result in suboptimal insulin dose titration, along with missed or reduced insulin doses after an episode of hypoglycaemia 27. Furthermore, concerns over hypoglycaemia are frequently cited as a barrier to the timely initiation of insulin in people with Type 2 diabetes 28. Taken together, these considerations contribute to suboptimal glucose control, leading to an increased risk of vascular complications, which represent the main long‐term economic implication of diabetes 9.
A recent publication by Hex et al. 9 estimated the annual cost of severe hypoglycaemia in the UK as £72.2 m, which is substantially lower than the estimate from the LIHT. The main reason for this is that different definitions of the severity of hypoglycaemia were used. Hypoglycaemic episodes were divided into severe and moderate, with non‐severe data excluded; however, both these categories would be defined as ‘severe’ according to the American Diabetes Association definition (used in the LIHT) 4, and in fact some data classified as ‘mild’, which were therefore excluded from the study by Hex et al., would also have been classed as ‘severe’ by the American Diabetes Association. Another possible reason for the discrepancy was that non‐UK specific data were used for a number of variables and assumed to be applicable to the UK. Finally, the costs were obtained using data from the 2010/2011 financial year, whereas more recent costs were used in the LIHT.
To complete further validation of the LIHT, it would be beneficial to collect patient‐level data from randomised controlled trials or real‐world observational studies concerning the frequency and impact of hypoglycaemia in insulin‐treated people with diabetes. For example, upcoming data from a real‐world questionnaire‐based study on rates and resource use associated with non‐severe hypoglycaemia in the UK should shed more light on the validity of the values used for non‐severe hypoglycaemia in the LIHT 29. When new data are available, the model has the added benefit of being easy to update with new values for hypoglycaemia rates, resource utilisation and costs.
The LIHT is also potentially transferable to other countries with cost, prevalence and resource utilisation data specific to the country of interest; however, the transferability of the model would depend on local patient and healthcare factors, such as patients' approaches to the management of hypoglycaemia, the structure of care and the treatment pathway for hypoglycaemia in the country of interest.
There are certain assumptions and some limitations associated with the LIHT. The main assumption in the model is that the UK population is representative of the individual populations of the smaller localities, with regard to prevalence, insulin use, hypoglycaemia rates, costs and utilisation values, for example, the assumption that hypoglycaemia rates are constant across the UK. This is, however, accounted for by the ability to input specific data based on known values.
The LIHT calculations are unlikely to be overestimated because of a number of conservative assumptions. Firstly, the baseline rates of hypoglycaemia used are likely to be conservative. Recent published data show that people using insulin report an average of 91 (Type 1 diabetes) and 20–35 (Type 2 diabetes, with different insulin treatments) non‐severe episodes per year 30. Secondly, only adult data are included, thus all costs for all populations will be underestimated overall. Another important factor is that there are insufficient data available for the use of glucose or glucagon for severe and non‐severe episodes; therefore utilisation values were set to zero. The costs for Dextrogel® and a GlucaGen Hypokit® 17 are included in the model so that the user can input specific utilisation values if known. There are also no data available for the number of extra blood glucose tests used in the week following a severe episode or for the working days lost as a result of a severe episode; therefore, it is assumed that these are the same as for a non‐severe episode. Additionally, NICE recommends that patients visit a diabetes specialist after a hypoglycaemic episode that requires medical attention; therefore, to avoid double counting in this model, we have assumed that people do not visit their general practitioner after a severe hypoglycaemic episode treated in community/hospital, and that people do not visit a diabetes specialist after a non‐severe episode or a severe episode treated at home/work. Finally, there are no data for the percentage of people that visit their general practitioner after a severe episode treated at home/work, therefore this utilisation was assumed to be identical to a non‐severe episode. In reality, all values discussed above are likely to be higher than these assumed values.
In the model it was assumed that 50% of patients that were hospitalised were ≥ 70 years of age, and 50% were < 70 years; therefore the hospitalization tariff used was a straight average of the two individual tariffs. The International Diabetes Federation estimate that 42.2% of the UK adult population with diabetes are < 60 years of age 31, therefore, this was a reasonable assumption that is likely to be close to the actual age distribution.
Additionally, there is likely to be an under‐reporting of hypoglycaemic episodes by patients. Non‐severe episodes are frequently not reported by patients to their general practitioner 30, and severe episodes are also likely to be under‐reported, partly because of the risk of losing a driving licence. The Driving and Vehicle Licensing Agency requires patients to report episodes of severe hypoglycaemia so it can assess whether it is safe for the patient to continue driving, and licences can be revoked on this basis 32.
The duration of insulin therapy is also one of the predictors of hypoglycaemia. This is not incorporated into the LIHT, as it would be impossible to have real‐time information on length of insulin therapy for all insulin‐treated people in the UK. However, the LIHT represents an average cost, and so is likely to incorporate a wide spread of people with different durations of insulin therapy. A consequence of presenting average costs is that the actual cost associated with any single episode may be over‐ or underestimated. The LIHT, however, is very flexible and can incorporate real‐life values for all variables outlined to explore any of these potential limitations.
In conclusion, the cost of hypoglycaemia in the UK is significant and often underestimated, especially for non‐severe episodes. The LIHT is a useful model for estimating the costs of severe and non‐severe hypoglycaemic episodes in insulin‐treated adults with Type 1 diabetes and Type 2 diabetes for the UK as a whole, and for a specific locality, a Primary Care Organisation, general practice or a user‐defined population.
The LIHT also provides the opportunity to explore how reducing hypoglycaemia rates could result in substantial budget savings, which may aid clinicians and NHS budget‐holders in their choice of insulin treatment. The component costs of a hypoglycaemic episode are also highlighted, further leading to the possibility of cost reductions for the NHS by effectively managing the individual resources, which could lead to additional funding to improve other aspects of diabetes care.
Funding sources
Research and subsequent development of the model and manuscript were funded by Novo Nordisk Limited, UK.
Competing interests
None declared.
Acknowledgements
The authors acknowledge writing and editorial support from Abacus International (sponsored by Novo Nordisk). The literature review was conducted by Pharma Co. Logic Ltd and funded by Novo Nordisk.
Diabet. Med. 32, 1156–1166 (2015)
References
- 1. Diabetes UK . Diabetes in the UK 2013 ‐ Key statistics in diabetes. Available at http://www.diabetes.org.uk/Documents/About%20Us/Statistics/Diabetes-key-stats-guidelines-April2014.pdf. Last accessed 16 June 2014.
- 2. American Diabetes Association . Standards of medical care in diabetes–2014. Diabetes Care 2014; 37(Suppl. 1): S14–80. [DOI] [PubMed] [Google Scholar]
- 3. Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care 2003; 26: 1902–1912. [DOI] [PubMed] [Google Scholar]
- 4. Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non‐severe hypoglycemic events on work productivity and diabetes management. Value Health 2011; 14: 665–671. [DOI] [PubMed] [Google Scholar]
- 5. U. K. Hypoglycaemia Study Group . Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 2007; 50: 1140–1147. [DOI] [PubMed] [Google Scholar]
- 6. National Institute for Health and Care Excellence . NICE CG15: Diagnosis and management of type 1 diabetes in children, young people and adults. Available at http://www.nice.org.uk/nicemedia/live/10944/29390/29390.pdf Last accessed 7 October 2013.
- 7. National Institute for Health and Clinical Excellence . Clinical Guideline 87 Quick Reference Guide 2010. Available at http://www.nice.org.uk/nicemedia/pdf/CG87QuickRefGuide.pdf Last accessed 24 April 2014.
- 8. Scottish Intercollegiate Guidelines Network . SIGN 116: Management of diabetes. Available at http://www.sign.ac.uk/pdf/sign116.pdf Last accessed 7 October 2013.
- 9. Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med 2012; 29: 855–862. [DOI] [PubMed] [Google Scholar]
- 10. Hammer M, Lammert M, Mejías SM, Kern W, Frier BM. Costs of managing severe hypoglycaemia in three European countries. J Med Econ 2009; 12: 281–290. [DOI] [PubMed] [Google Scholar]
- 11. Leese GP, Wang J, Broomhall J, Kelly P, Marsden A, Morrison W et al Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population‐based study of health service resource use. Diabetes Care 2003; 26: 1176–1180. [DOI] [PubMed] [Google Scholar]
- 12. Department of Health . NHS reference costs 2012‐2013. Available at www.gov.uk/government/publications/nhsreference-costs-2012-to-2013 Last accessed 16 June 2014.
- 13. National Institute for Health and Care Excellence . NICE Diabetes in adults quality standard (Quality statement 14: Hypoglycaemia). Available at http://publications.nice.org.uk/diabetes-in-adults-quality-standard-qs6/quality-statement-14-hypoglycaemia Last accessed 7 October 2013.
- 14. Personal Social Services Research Unit . Unit Costs of Health and Social Care 2013. Available at http://www.pssru.ac.uk/project-pages/unit-costs/2013/index.php Last accessed 16 June 2014.
- 15. Department of Health . PbR tariff information spreadsheet for 2014‐2015. Available at www.gov.uk/government/publications/national-tariff-paymentsystem-2014-to-2015. Last accessed 16 June 2014.
- 16. Office for National Statistics . Labour Market Statistics, June 2014 Report. Available at http://www.ons.gov.uk/ons/dcp171778_363998.pdf. Last accessed 16 June 2014.
- 17. MIMS . June 2014. Available at http://www.mims.co.uk/ Last accessed 16 June 2014.
- 18. NHS England . Total Allocations. Available at http://www.england.nhs.uk/wp-content/uploads/2013/12/ccg-allocation-big-table-v2.pdf. Last accessed 13 January 2014.
- 19. Information Services Division Scotland . GP Workforce & Practice Populations. Available at http://www.isdscotland.org/Health-Topics/General-Practice/Practices-and-Their-Populations/ Last accessed 13 January 2014.
- 20. Quality and Outcomes Framework, 2012‐2013. Available at http://www.hscic.gov.uk/catalogue/PUB12262 Last accessed 16 June 2014.
- 21. Office for National Statistics . Population Estimates for UK, England and Wales, Scotland and Northern Ireland, Mid‐2013. Available at http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-322718. Last accessed 16 June 2014.
- 22. National Institute for Health and Care Excellence . NICE Pathways: Managing type 1 diabetes in adults. Available at http://pathways.nice.org.uk/pathways/diabetes/managing-type-1-diabetes#path=view%3A/pathways/diabetes/managing-type-1-diabetes-in-adults.xml&content=close Last accessed 7 October 2013.
- 23. National Institute for Health and Care Excellence . NICE Pathways: Type 2 diabetes: newer agents for blood glucose control ‐ Costing template. Available at http://guidance.nice.org.uk/CG87/CostingTemplate/xls/English Last accessed 7 October 2013.
- 24. OECD Stats Extracts . Average annual hours actually worked per worker. Available at http://stats.oecd.org/Index.aspx?DatasetCode=ANHRS Last accessed 7 October 2013.
- 25. Monami M, Marchionni N, Mannucci E. Long‐acting insulin analogues vs. NPH human insulin in type 1 diabetes. A meta‐analysis. Diabetes Obes Metab 2009; 11: 372–378. [DOI] [PubMed] [Google Scholar]
- 26. Evans M, Khunti K, Mamdani M, Galbo‐Jorgensen CB, Gundgaard J, Bogelund M et al Health‐related quality of life associated with daytime and nocturnal hypoglycaemic events: a time trade‐off survey in five countries. Health Qual Life Outcomes 2013; 11: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Brod M, Rana A, Barnett AH. Impact of self‐treated hypoglycaemia in type 2 diabetes: a multinational survey in patients and physicians. Curr Med Res Opin 2012; 28: 1947–1958. [DOI] [PubMed] [Google Scholar]
- 28. Peyrot M, Barnett AH, Meneghini LF, Schumm‐Draeger PM. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med 2012; 29: 682–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chubb BD, Jensen MM, Frier BM. Self‐reported frequency and effects of non‐severe hypoglycaemia in insulin‐treated adults in the UK. Poster presentation 2014; ISPOR 17th Annual European Congress.
- 30. Ostenson CG, Geelhoed‐Duijvestijn P, Lahtela J, Weitgasser R, Markert Jensen M, Pedersen‐Bjergaard U. Self‐reported non‐severe hypoglycaemic events in Europe. Diabet Med 2014; 31: 92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. International Diabetes Federation (IDF) . Diabetes Atlas, Sixth Edition, 2013. Available at http://www.idf.org/sites/default/files/EN_6E_Atlas_Full_0.pdf Last accessed 20 January 2014.
- 32. Diabetes UK . Driving and the new medical standards for people with diabetes. Available at http://www.diabetes.org.uk/Documents/Professionals/News,%20updates,%20prizes%20and%20alerts/Driving-diabetes-professional-guidance0212.pdf Last accessed 22 January 2015.


