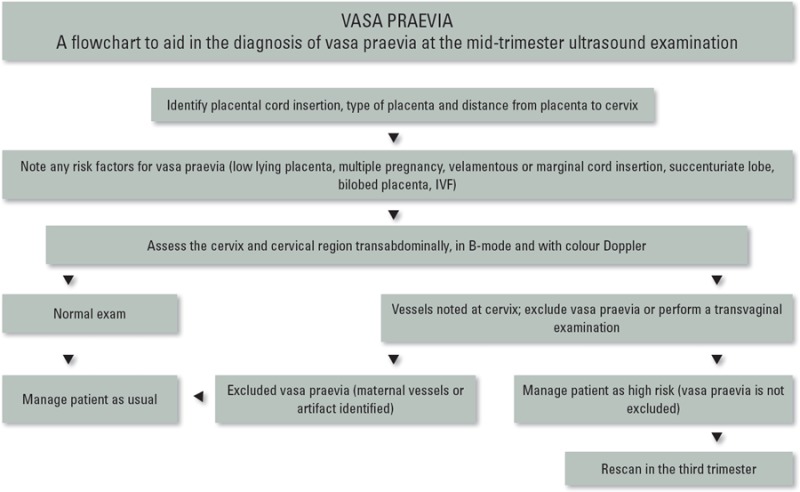
Abstract
Background: Vasa praevia is a condition in which fetal vessels, unsupported by the umbilical cord or placenta, run on the fetal membranes in the lower uterine segment near the cervix. Rupture of these vessels prior to or at the time of delivery is associated with a very high perinatal mortality rate. Antenatal diagnosis of this condition with ultrasound is readily available, alters management and significantly decreases the risk of fetal loss.
Materials and methods: We describe our experience of diagnosing vasa praevia at a tertiary referral ultrasound centre. The ultrasound characteristics that led to the diagnosis of vasa praevia and associated risk factors will be discussed. A guide to aid sonographers when performing an obstetric examination to help screen for this condition has been included.
Conclusions: Where suspicion of vasa praevia is raised, and cannot be ruled out on transvaginal ultrasound, a third trimester scan is required.
Keywords: fetal vessels, low lying placenta, mid‐trimester scan, placenta praevia, succenturiate lobe, vasa praevia, velamentous cord insertion, ultrasound
Introduction
The mid‐trimester scan often focuses on excluding abnormalities of the fetus with less emphasis on anomalies of the placenta and umbilical cord. Vasa praevia is a condition in which fetal vessels, unsupported by the umbilical cord or placenta run on the fetal membranes in the lower uterine segment near the cervix. 1 Rupture of these vessels prior to, or at the time of delivery can result in catastrophic blood loss from the fetus and is associated with a very high perinatal mortality rate. 1 Ultrasound diagnosis of this condition in the second and third trimesters has made a vast improvement on neonatal mortality and morbidity. Oyelese, et al. 2 reported that prenatal diagnosis of vasa praevia by ultrasound reduced perinatal mortality from 56% to 3% in a large study of 155 cases of vasa praevia.
The incidence of vasa praevia was previously reported to be 1 in 1275 to 1 in 8333. 3 However, many of these figures relied on diagnosis at delivery and were calculated before the availability of transvaginal ultrasound and colour Doppler. 4 More recently, Baulies, et al. 1 reported an incidence of 1 in 1351 in a retrospective study of 12, 063 deliveries from January 2000 to March 2005. Currently accepted risk factors for vasa praevia include placenta praevia, multiple pregnancies, velamentous cord insertion, succenturiate lobe and bilobed placentas. 1 , 3 , 5 Studies have also suggested that in‐vitro fertilisation (IVF) is a risk factor for vasa praevia due to an increase in abnormal placentation from poor orientation of the blastocyst at implantation. 6
Our aim is to describe our experience in diagnosing vasa praevia in a tertiary obstetric ultrasound practice and to increase awareness and understanding of this condition amongst sonographers. We suggest some practical techniques to assist in excluding vasa praevia at the mid‐trimester scan and highlighting patients at high risk requiring follow‐up in the third trimester.
Ultrasound diagnosis of vasa praevia
Ultrasound is the method of choice for the antenatal diagnosis of vasa praevia. 7 It can be suspected at the time of the mid‐trimester scan and confirmed in the third trimester. 8 Several techniques for identifying vasa praevia on ultrasound include: identification of the placental cord insertion, 9 applying colour Doppler over the cervix, 10 transvaginal ultrasound 7 and three‐dimensional (3D) ultrasound. 11 Sonographic identification of the placental cord insertion is accurate, sensitive and adds little or no extra time to the routine mid‐trimester scan. 2 , 5 In addition, if the placental cord insertion is difficult to identify, it may be abnormal. 5
Hasegawa, et al. 10 have recommended the use of colour Doppler to aid in the identification of aberrant vessels in the region of the cervix for those women at increased risk of vasa praevia.
Risk factors at the mid‐trimester scan
Several studies have identified the following as risk factors for vasa praevia: velamentous cord insertion, marginal cord insertion, succenturiate or bilobed placentas, low lying placenta, IVF and multiple pregnancies. 1 , 3 , 5 These risk factors increase the likelihood of unprotected fetal vessels traversing the lower uterine segment which constitutes a vasa praevia.
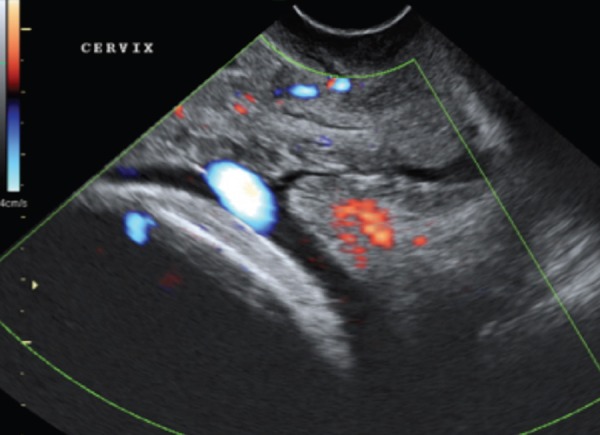
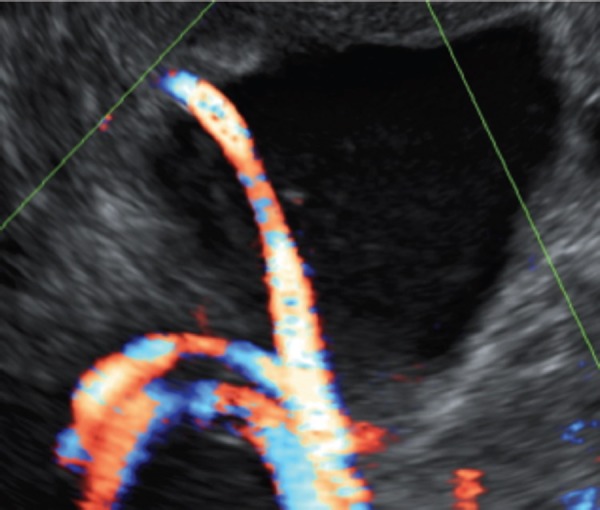
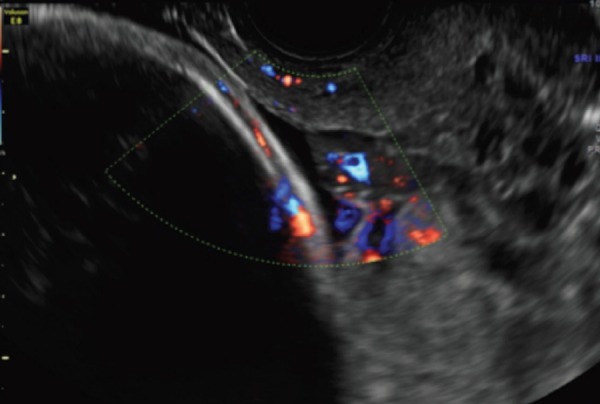
Figure 1.
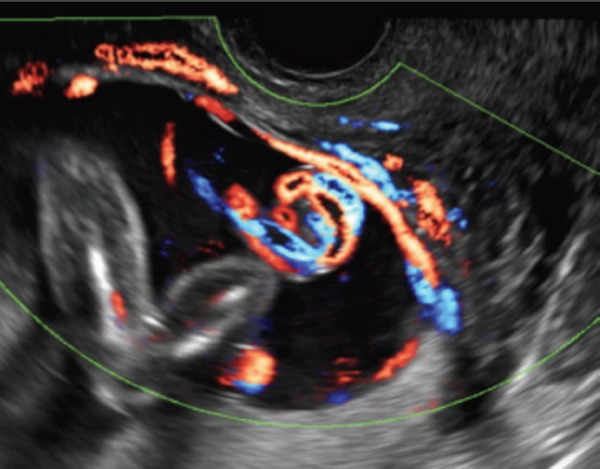
Transvaginal colour Doppler image of fetal vessels crossing the cervix in the third trimester.
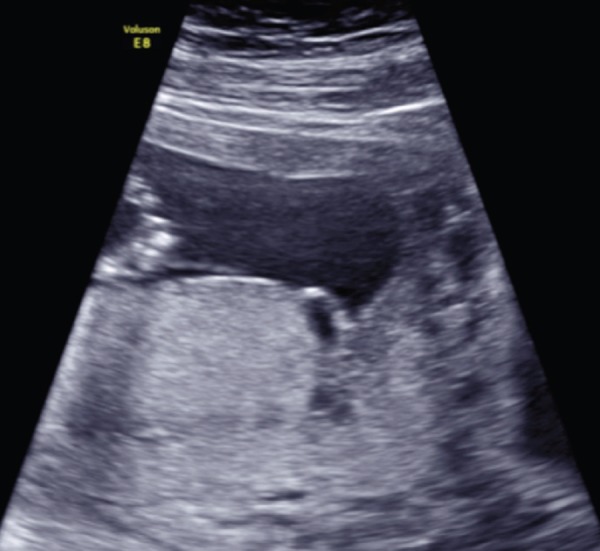
Figure 2.
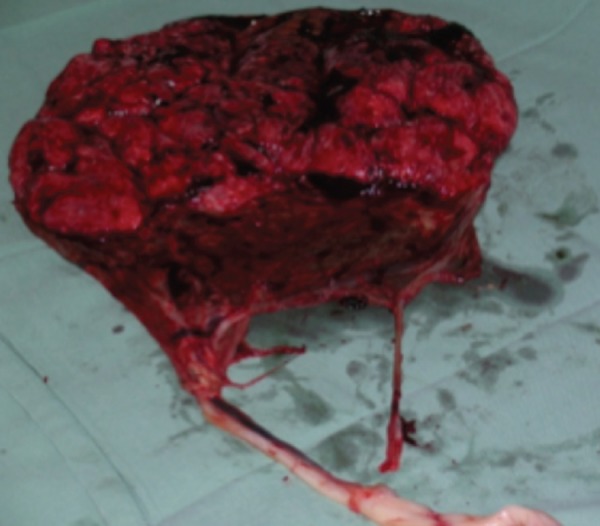
Pathology specimen of a patient diagnosed with vasa praevia. Note the velamentous cord insertion and unprotected fetal vessels.
Figure 3.
Transabdominal image of a velamentous cord insertion on the anterior wall at 19 weeks gestation. The placenta is positioned posteriorly, therefore this patient is at high risk for vasa praevia.
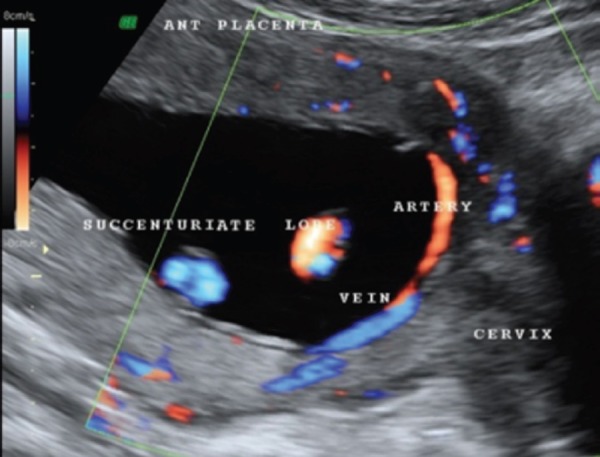
Figure 4.

Transvaginal image at 30 weeks gestation. This patient has a low lying placenta with a marginal cord insertion at the lower edge of the placenta.
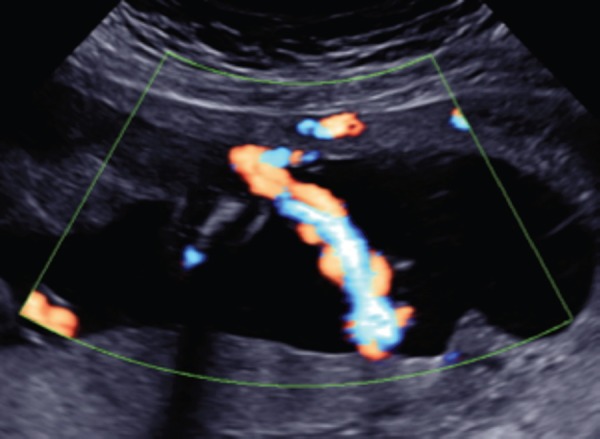
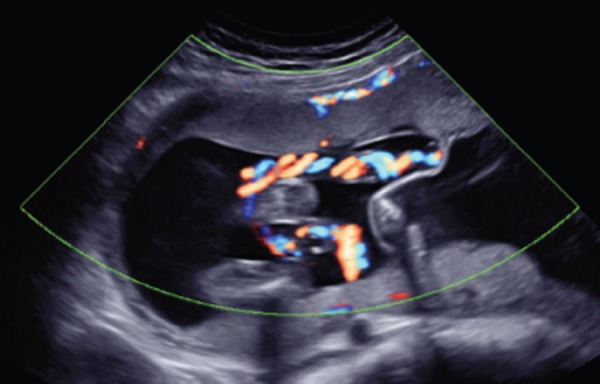
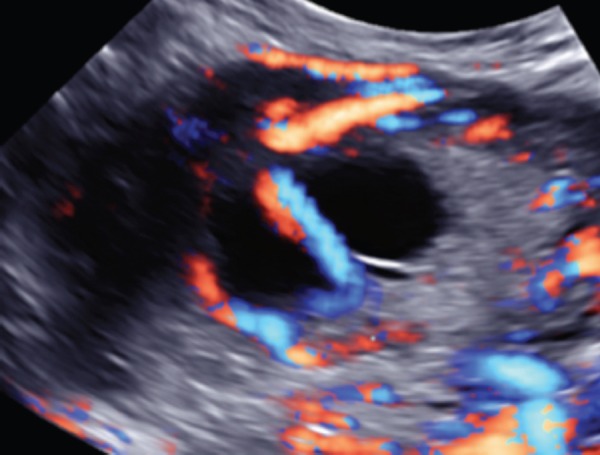
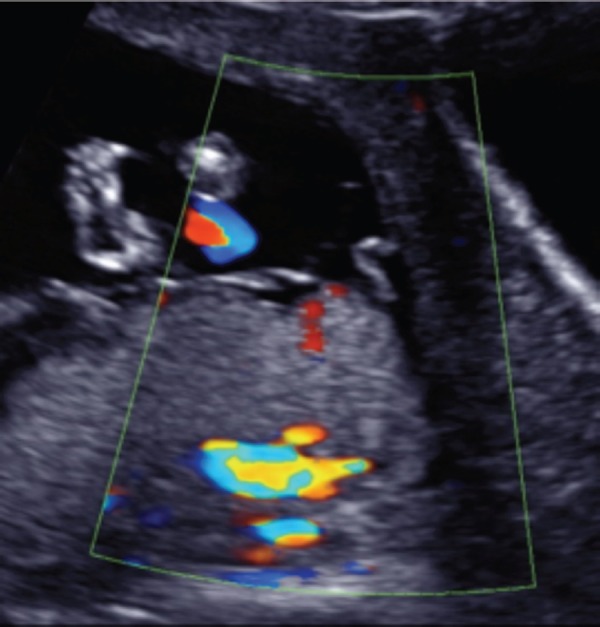
Figure 5.
Transabdominal colour Doppler image of a fetal vein and artery crossing the cervix at 19 weeks gestation. This patient has an anterior placenta and posterior succenturiate lobe.
Velamentous cord insertion is where the umbilical cord inserts away from the main body of the placenta and traverses the chorioamniotic membranes before inserting into the placenta. 12 If the vessels from the velamentous cord insertion run across or near the cervix, this may become a vasa praevia.
Marginal cord insertion has been described by Gudmundson, et al. as being within 1 cm from the placental edge. 13 If we use the analogy of a spider web of vessels, and the placental cord insert is the centre, we can then appreciate how the vessels may run in many directions. Inferior marginal cord insert further increases the risk or a vasa praevia occurring.
Succenturiate or bilobed placentas are where the placenta forms in two or several parts, and fetal blood vessels run across the membranes to connect them. If these vessels run across the lower segment they may become a vasa praevia. 14
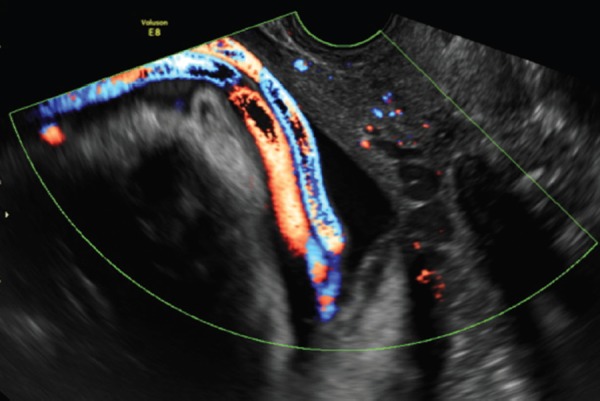
Figure 6.
Transvaginal colour Doppler image in the third trimester. Demonstrates an unprotected fetal vessel adjacent to the internal cervical os. Note the vessel extends from the leading edge of the anterior low‐lying placenta.
Low lying placenta is abnormal implantation of the placenta that is overlying or generally within 2 cm of the internal os, at the mid‐trimester scan. This may become placenta praevia in the third trimester, after the formation of the lower uterine segment. 14 When the placenta is near the internal os, there is an increased risk of aberrant vessels over the cervix.
Even if there is regression of the placenta in the third trimester, there is still potential for vessels to remain in the lower segment for the non‐praevia patient. This concept of a low lying placenta at the mid‐trimester scan (without placenta praevia in the third trimester) was introduced by Oyelese in 1998 15 as a risk factor and discussed in more recent articles. 2 , 8
IVF has been reported to increase the risk for anomalies of the placenta and cord, which in turn increases the risk for vasa praevia. 6 For example, a velamentous cord insertion is reported in up to 12.7% 6 of IVF patients. Schachter, et al. 16 suggest that the incidence of vasa praevia in IVF pregnancies was as high as 1 in 293.
Multiple pregnancies have several cord insertion sites, therefore increasing the risk of aberrant fetal vessels occurring. A 10‐fold increase in velamentous cord insertions has been reported in multiple pregnancies. 5
Multiple pregnancies are commonly associated with IVF which carries the inherent risks as discussed previously. The concept of vasa praevia is mainly concerned with aberrant vessels related to the presenting fetus in a multiple pregnancy. However, we suggest that there is a similar risk of vasa praevia if there are exposed fetal vessels on the dividing membrane from the non‐presenting fetus.
While there are no vessels between the presenting fetus and the cervix, if there is rupture of the membranes with a vaginal delivery there may be catastrophic blood loss from the non‐presenting fetus with rapid demise. Therefore, we suggest it is just as important to assess the placenta, cord insertion and dividing membranes for the non‐presenting fetuses in multiple pregnancies.
Rare cases of vasa praevia without any of the classical risk factors have also been observed. Below is an example of a unique case of vasa praevia that did not fit the risk factors quoted.
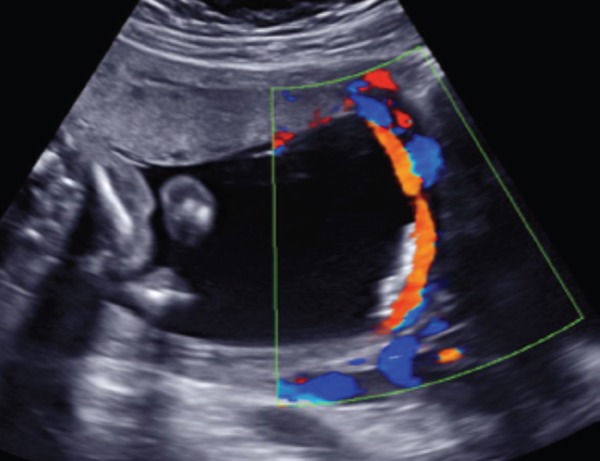
Figure 7.
Transabdominal colour Doppler image of 19 week twin pregnancy. A velamentous cord insertion for twin 2 is seen to attach on the membranes dividing these dichorionic diamniotic twins.
Figure 8.
Transabdominal colour Doppler longitudinal image at 19 weeks gestation. The antero‐lateral placenta is not low, and there is no succenturiate or bilobed placentas. The umbilical cord inserts into the centre of the placenta. This image demonstrates unprotected fetal vessels running from the leading edge of the anterior portion of the antero‐lateral placenta to the posterior aspect of the uterus, near the cervix.
Techniques
Mid‐trimester scan
The techniques we would suggest to exclude vasa praevia at the mid‐trimester scan are:
-
1
When assessing placental location we also identify the type of placenta and the placental cord insertion. Suspicion is raised in the presence of a velamentous insertion, marginal cord insertion, succenturiate or bilobed placentas
-
2
Using colour Doppler, note the vessels on the surface of the placenta, the course they take, and the proximity to the cervical os
-
3
Measure the distance of the placenta from the internal os and assess the cervical length (as per ASUM Guidelines for the Mid‐trimester Obstetric Scan 17 )
Figure 9.
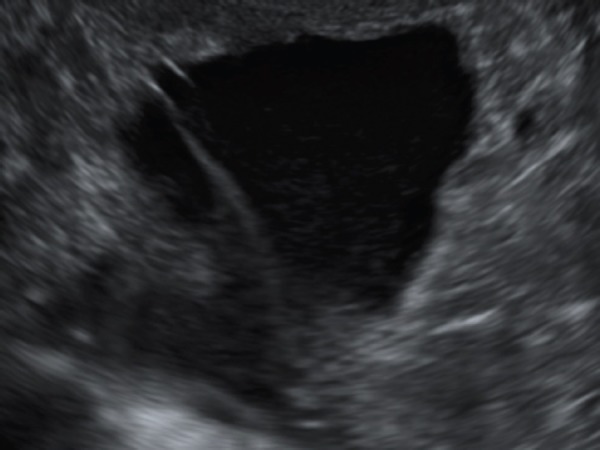 Transvaginal B‐mode image at 19 weeks gestation, demonstrating a linear echolucent structure superior to the cervix.
Transvaginal B‐mode image at 19 weeks gestation, demonstrating a linear echolucent structure superior to the cervix. -
4
Apply colour Doppler over the lower part of the uterus, sweeping out to the lateral margins. Take note of any vessels in close proximity to the cervix. If a vessel is suspected, identify if it is of maternal or fetal origin.
On B‐mode ultrasound, vasa praevia can be seen as linear echolucent structures within the membranes overlying the cervix. 15 This can be appreciated when applying colour Doppler, confirming this structure is a vessel.
When to use transvaginal (TV) ultrasound?
If vasa praevia cannot be excluded on transabdominal ultrasound at the mid‐trimester scan, a transvaginal scan is required, with patient consent. Transvaginal ultrasound offers improved resolution due to the proximity to the area of interest (which allows for the use of a higher frequency probe). It also offers reduced attenuation from subcutaneous layers. 18 The same techniques used transabdominally can now be applied in the transvaginal setting to identify aberrant fetal vessels in close proximity to the cervix. 15 , 18
Three‐dimensional sonography (3D)
If three‐dimensional imaging is available, a longitudinal 3D data set of the cervix region with colour Doppler maybe advantageous. The 3D data volume can be manipulated to produce a coronal plane or colour rendered image, which may better explain the relationship of the vessels to the cervix. Three‐dimensional imaging may assist in the case of remote reporting, allowing the reporting doctor to make the diagnosis of vasa praevia. 11 , 14 We have also found that cine loop capture is as helpful as 3D in assisting in the diagnosis. However, this requires very fast software capabilities and large data storage facilities.
Other gestations
Screening for vasa praevia in the first and third trimesters follow the same principles and understanding of placental morphology. The same techniques used in the mid‐trimester scan can be applied. In particular, at our practice we aim to identify the placental cord insertion and place colour Doppler over the cervix at all gestations. When required, transvaginal scanning always offers increased resolution.
Figure 10.
Transvaginal image with colour Doppler of the same patient as The structure contains Doppler flow, representative of a vessel.
Figure 11.

Transabdominal 3D colour data volume at 19 weeks gestation in a patient with vessels overlying the cervical region.
The assessment for vasa praevia in the first trimester has been discussed by Hasegawa, et al. 5 and Oyelese, et al. 2 The placental location will alter from the first to third trimesters, due to the formation of the lower uterine segment. Therefore, it seems difficult to diagnose and exclude vasa praevia at first trimester ultrasound. However, it may be helpful to identify those patients in the first trimester who are potentially at high risk of developing vasa praevia in subsequent trimesters. Velamentous, marginal cord insertions, succenturiate and bilobed placentas maybe diagnosed as early as the first trimester. 5 These patients may be flagged for closer inspection at the mid‐trimester scan to exclude vasa praevia.
In the third trimester:
We recommend always performing a transvaginal scan (with patient consent) if there has been any suspicion of a vasa praevia from the mid‐trimester scan. This is recommended due to the position of the fetal head in the third trimester and increased distance of the probe from the area of interest. 18 Vasa praevia must be excluded to allow the patient to have a vaginal delivery. 18 However, if vasa praevia is suspected, this has an impact on management, and influences mode and timing of delivery.
When conducting a third trimester ultrasound whether a vasa praevia has been suspected or not, it is important to note whether the patient had a low lying placenta at the mid‐trimester scan. There may be regression of the placenta, but fetal vessels may remain in the lower uterine segment. As a result, a transvaginal scan would be highly recommended. 15 , 19
Figure 12.
Transabdominal 3D colour data volume at 19 weeks gestation of the same patient from The data volume can be manipulated to produce a coronal image of the vessel/s immediately superior to the cervix.
What if I find a vasa praevia?
A prenatal diagnosis of vasa praevia will require delivery by lower uterine segment caesarean section. When scanning a patient with vasa praevia in the third trimester it is important to also check the position of the fetal vessels in relation to the proposed incision site i.e. lower segment.
It is imperative that the referring doctor, obstetrician and/or place of intended delivery are made aware of the diagnosis of vasa praevia so that appropriate management plans can be made. Currently in Australia there are no agreed guidelines for obstetric management of these patients. 20 Gagnon 7 found that these patients are however at increased risk of premature rupture of membranes.
Australian statements
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) released a statement in July 2012 regarding prenatal diagnosis of vasa praevia. 20
This statement advocates:
The use of colour Doppler to all routine ultrasound examinations of singleton pregnancies to identify the placental cord insertion
A targeted ultrasound examination of the lower segment and cervical region using colour Doppler in all pregnancies with risk factors.
Figure 13.

Transvaginal colour Doppler image of 32 week gestation pregnancy. Flash artifact noted in red on the image due to fetal movement. This can be mistaken for vasa praevia.
Transvaginal screening of the entire population is not considered to be cost effective, 20 however this may be necessary in some patients where transabdominal imaging is unclear. We advocate that applying colour Doppler when examining the cervix at the mid‐trimester scan will further highlight patients at risk of vasa praevia.
Artifacts and pitfalls
There are several artifacts that may be encountered when following this guide in an effort to diagnose vasa praevia.
Flash artifact
Flash artifact occurs when there is fetal movement or movement of amniotic fluid causing colour flow to appear over the cervix as a flash of colour. Careful waiting and watching will demonstrate that when the movement ceases there will no longer be colour flow and that this was not caused by the presence of a blood vessel. 21 The use of spectral analysis will differentiate between the consistent waveform of a vessel and the disorganised signal of flash artifact.
Maternal versus fetal vessels
Occasionally, it may be difficult to differentiate between fetal and maternal vessels.
-
1
Try to assess the location of the vessel(s). Is it within the membranes or within maternal structures i.e. uterine wall?
-
2
Discover the origin of the vessels, i.e. placenta
-
3
Apply pulse wave Doppler to ascertain the waveform. If the waveform is arterial measure the heart rate. If it is between 120 and 180 bpm it is likely to be of fetal origin. However, if it is between 70 and 90 bpm it will most likely be maternal. If the waveform is venous it may be more difficult to ascertain if it is of fetal or maternal origin. Reassess the origin and location of the vein. Valsalva manoeuvre is a technique which may be helpful in identifying maternal veins versus fetal veins. A fetal vein will display no change in phasicity with valsalva manoeuvre. This may assist in proving a fetal vein; however we are currently investigating this technique. 11 , 22
Figure 14.
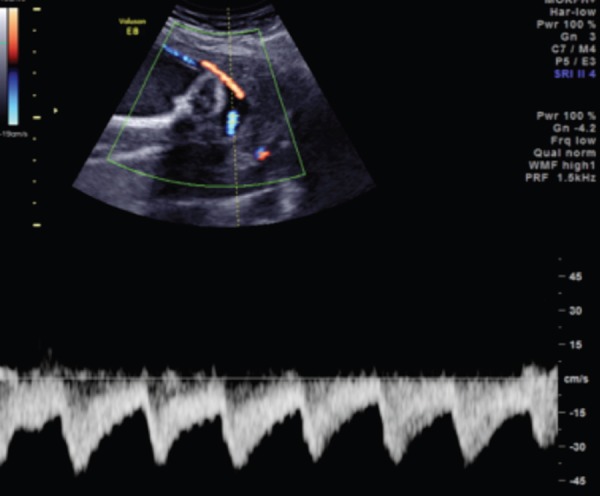
Transabdominal colour Doppler image of a 19 week gestation pregnancy. Applying a spectral trace to suspected vessels for vasa praevia can help distinguish if it is a fetal artery. The trace depicted above demonstrates a typical waveform for an umbilical artery.
Figure 15.
Transvaginal colour Doppler image in the third trimester, displaying vessels in the lower uterine segment. The vessels are seen between the presenting fetus and the cervix. However, they are not within the membranes; it is free floating umbilical cord.
Figure 16.
Transvaginal colour Doppler image in the third trimester. Colour flow demonstrates vessels in the lower uterine segment. These vessels are however within the uterine tissue, and are maternal varicosities.
Figure 17.
Transabdominal B‐mode image at 19 weeks gestation. At the inferior portion of the placenta, a hypoechoic region is seen. This can be mistaken as a vessel within the membranes; it is a placental lake.
Suboptimal machine settings
Suboptimal machine settings may contribute to missing the crucial diagnosis of vasa praevia. We suggest optimising the following machine parameters to assist in making the diagnosis:
Frequency: should be the highest possible for the appropriate depth (transvaginal probes always offer higher frequency)
Colour gain: should be set as high as possible without introducing speckle
Wall filter: should be decreased, so low flow is not missed
Pulse Repetition Frequency (PRF): should be decreased to identify low velocity flow. 23
Maternal body habitus
Maternal habitus (obesity and maternal scarring) decreases the image quality particularly in the lower uterine segment, making vasa praevia difficult to diagnose. Transvaginal scanning will offer improved resolution of the internal os, which is critical in excluding vasa praevia. 18
Time
Sonographer daily time constraints may be considered a pitfall in the diagnosis of vasa praevia. However, it has been estimated that incorporating a search for vasa praevia transabdominally in the mid‐trimester scan, adds approximately 1 minute to the standard scan time. 1 When a transvaginal scan is required this will also add additional time to the length of the examination. In practice this will only be required for a very few patients and is necessary in excluding a condition that has the potential to cause fetal mortality.
Figure 18.

Transabdominal B‐mode image at 19 weeks gestation of the placenta in front of the cervix. An echolucent region is visualised that can be mistaken for a potential vasa praevia.
Figure 19.
Transabdominal colour Doppler image at 19 weeks of the placenta in front of the cervix of the same patient as When colour is applied to the region of interest, no flow is identified, this is a fold of amniotic membranes.
Our recommendations
Differential diagnoses
Free floating cord
Free floating cord between the lower uterine segment (and/or cervix) and the presenting part of the fetus may be mistaken for vasa praevia. This may be differentiated from vasa praevia by applying gentle pressure to the abdominal wall with either the non‐scanning hand or ultrasound probe. This movement will temporarily displace free floating cord, whereas vasa praevia or aberrant vessels will not have this mobility. 10 , 11
Varicosities of the uterine veins
During pregnancy blood flow increases 60 fold in the uterine vessels, which causes venous congestion and associated varicosities. 11 If these prominent vessels are located within the lower uterine segment they maybe mistaken for vasa praevia. Careful examination of the location of these vessels and the type of spectral trace they produce will help to differentiate from vasa praevia.
Placental lakes
Placental lakes are seen as hypoechoic structures within the placenta that may bulge into the amniotic space. On real time scanning the slow swirling vascular pattern may be observed in B‐mode. When these are seen adjacent to or above the cervix it may be mistaken for vasa praevia. However, technically this is within the placental tissue and therefore qualifies for a low lying placenta, or placenta praevia if in the third trimester. 24
Amniotic membranes, placental shelf or uterine synechae
If linear structures are noted on ultrasound above the cervix, and are not fetal vessels, the differential diagnoses include: amniotic membranes, placental shelves or uterine synechae. A small amount of vascularity maybe noted in the case of placental shelves. 25
Conclusion
Vasa praevia is a serious condition that may be excluded at the second trimester ultrasound when assessing for low lying placenta. Where suspicion is raised, and cannot be ruled out on transvaginal ultrasound, a third trimester scan is required. Diagnosing vasa praevia prenatally, can make a difference to the outcome of these pregnancies.
References
- 1. Baulies S, Maiz N, Munoz A, Torrents M, Echevarria M, Serra B. Prenatal ultrasound diagnosis of vasa praevia and analysis of risk factors. Prenat Diagn 2007; 27: 595–99. [DOI] [PubMed] [Google Scholar]
- 2. Oyelese Y, Catanzarite V, Prefumo F, Lashley S, Schachter M, Tovbin Y, et al. Vasa previa: The impact of prenatal diagnosis on outcomes. Obstet Gynecol 2004; 103 (5): 937–42. [DOI] [PubMed] [Google Scholar]
- 3. Oyelese KO, Turner M, Lees C. Vasa Praevia: an avoidable obstetric tragedy. Obstet Gynecol Surv 1999; 54: 138. [DOI] [PubMed] [Google Scholar]
- 4. Merz E. Basic Principles and Practical Application of Transvaginal Doppler Ultrasound in Gynecology. Ultrasound in Obstetrics and Gynecology, Vol. 2: Gynecology 2nd Edn. New York: Thieme; 1997. pp 198–99. [Google Scholar]
- 5. Hasegawa J, Matsuoka R, Ichizuka K, Sekizawa A, Okai T. Velamentous cord insertion: Significance of prenatal detection to predict perinatal complications. Taiwan J Obstet Gynecol 2006; 45 (1): 21–25. [DOI] [PubMed] [Google Scholar]
- 6. Burton G, Saunders DM. Vasa praevia: another cause for concern in In Vitro Fertilization pregnancies. Aust N Z J Obstet Gynaecol 1988; 28: 180–81. [DOI] [PubMed] [Google Scholar]
- 7. Gagnon R. Guidelines for the management of vasa previa. J Obstet Gynaecol Can 2009; 231: 748–53. [DOI] [PubMed] [Google Scholar]
- 8. Lee W, Lee VL, Kirk JS, Sloan CT, Smith RS, Comstock CH. Vasa previa: prenatal diagnosis, natural evolution, and clinical outcome. Obstet Gynecol 2000; 95: 572–76. [DOI] [PubMed] [Google Scholar]
- 9. Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol 2006; 107: 927–41. [DOI] [PubMed] [Google Scholar]
- 10. Hasegawa J, Matsuoka R, Ichizuka K, Sekizawa A, Okai T. Ultrasound diagnosis and management of umbilical cord abnormalities. Taiwan J Obstet Gynecol 2009; 48 (1): 23–27. [DOI] [PubMed] [Google Scholar]
- 11. Oyelese Y, Chavez MR, Yeo L, Giannina G, Kontopoulos EV, Smulian JC, et al. Three‐dimensional sonographic diagnosis of vasa previa. Ultrasound Obstet Gynecol 2004; 54: 211‐15. [DOI] [PubMed] [Google Scholar]
- 12. Cipriano L, Barth W, Zaric G. The cost‐effectiveness of targeted or universal screening for vasa praevia at 18–20 weeks of gestation in Ontario. BJOG 2010; 117: 1108–18. [DOI] [PubMed] [Google Scholar]
- 13. Gudmundsson S, Dubiel M, Sladkevicius P. Placental morphologic and functional imaging in high‐ risk pregnancies. Semin Perinatol 2009; 4 (5): 270–80. [DOI] [PubMed] [Google Scholar]
- 14. Abramowicz JS, Sheiner E. Ultrasound of the placenta: A systematic approach. Part I: Imaging. Placenta 2008; 29: 225–40. [DOI] [PubMed] [Google Scholar]
- 15. Oyelese KO, Schwärzler P, Coates S, Sanusi FA, Hamid R, Campbell S. A strategy for reducing the mortality rate from vasa praevia using transvaginal sonography with color Doppler. Ultrasound Obstet Gynecol 1998; 12: 434–38. [DOI] [PubMed] [Google Scholar]
- 16. Schachter M, Tovbin Y, Arieli S, Friedler S. Ron‐EI R, Sherman D. In vitro fertilisation is a risk factor for vasa praevia. Fertil Steril 2002; 78: 642–43. [DOI] [PubMed] [Google Scholar]
- 17. Australasian Society for Ultrasound in Medicine . Policies and Statements D2:2005. Guidelines For The Mid‐trimester Obstetric Scan. Sydney: AS UM; 2005. [Google Scholar]
- 18. Nyberg DA, Hill LM, Böhm‐Vélez M, Mendelson EB. Transvaginal Sonography: Applications, Equipment, and Technique. Patterson AS. editor. Transvaginal Ultrasound. Missouri: Mosby; 1992. pp 1–3. [Google Scholar]
- 19. Oyelese Y, Spong C, Fernandez MA, McLaren RA. Second trimester low‐lying placenta and in‐vitro fertilization? Exclude vasa previa. J Matern Fetal Med 2000; 9: 370–72. [DOI] [PubMed] [Google Scholar]
- 20. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. College Statements C‐Obs 47: 2012. Vasa Praevia. Melbourne: RANZCOG; 2012. [Google Scholar]
- 21. Campbell SC, Cullinan JA, Rubens DJ. Slow flow or no flow? Color and power Doppler US pitfalls in the abdomen and pelvis. Radiographics 2004; 24: 497–506. [DOI] [PubMed] [Google Scholar]
- 22. Baschat AA, Gembruch U. Ante‐ and intrapartum diagnosis of vasa praevia in singleton pregnancies by colour coded Doppler sonography. Eur J Obstet Gynecol Reprod Biol 1998; 79: 19–25. [DOI] [PubMed] [Google Scholar]
- 23. Gent R. Colour Flow Imaging. Applied Physics and Technology of Diagnostic Ultrasound. Prospect: Milner Publishing; 1997. pp 276. [Google Scholar]
- 24. Sanders R, Winter TC. Second and Third Trimester Bleeding. Dietz KC. editor. Clinical Sonography: A practical guide, 4th Edn. Philidelphia: Lippincott Williams & Wilkins; 2007. 423. [Google Scholar]
- 25. Brown DL, Felker RE, Emerson DS. Intrauterine Shelves in Pregnancy: Sonographic Observations. AJR 1989; 153: 821–24. [DOI] [PubMed] [Google Scholar]


