Abstract
Introduction: Patients with acute abdominal pain may have unsuspected pneumoperitoneum, and be investigated with ultrasound. Although not the primary imaging modality for this condition, ultrasound will usually demonstrate signs of free intraperitoneal or extra‐luminal gas.
Methods: Sonographic signs of pneumoperitoneum are described, along with the limitations and pitfalls of the technique. The reported accuracy of these signs is described.
Conclusion: The different signs that may be seen are described, and it is suggested that all who ultrasound patients for abdominal pain should be aware of these.
Keywords: free, gas, intraperitoneal, pneumoperitoneum
Introduction
Acute abdominal pain is a common symptom in patients who present to emergency departments. The differential diagnoses of these patients are varied, and it is often difficult to be certain based only on the history and examination. As a result, imaging is frequently employed to further investigate the cause of the pain. Ultrasound (US) is commonly used, although it is generally not considered to be the investigation of choice for diagnosing perforations. 1 , 2 The usual explanation for this is that gas, as a strong reflector that prevents transmission of ultrasound waves and creates reverberation artifacts, inhibits diagnostic information from being obtained. In addition, the physiological gas within bowel will further prevent accurate interpretation. 3
However, when considering the criteria used to diagnose pneumoperitoneum on plain x‐ray and CT, it becomes evident that the same criteria can be used with ultrasound. This paper will discuss the sonographic signs and criteria that can be used to diagnose pneumoperitoneum, and describe the accuracy and limitations of the technique.
Sonographic criteria for diagnosing pneumoperitoneum
The diagnosis of pneumoperitoneum, whether by plain xray, CT or ultrasound relies upon the detection of gas in the abdomen outside its usual position, i.e. outside the bowel lumen. Due to it's low density, gas will generally move in an anti‐gravitational direction to the most elevated areas. In the case of pneumoperitoneum, in the supine patient, this will result in gas being seen adjacent to the peritoneal line or gas above the liver. Gas may also be seen, particularly small locules, outside bowel in the region of a perforation.
Gas appears on ultrasound as a bright reflective surface with shadowing that obscures the underlying anatomy, with either long path reverberation artifacts (for large gas collections) or short path ‘ringdown’ artifacts (for small gas collections), although very small locules of gas may not cast an acoustic shadow or generate reverberation artifacts. Based upon this, there have been a number of sonographic signs described in the literature over the last 30 years. 4
Gas above the liver
Usually the liver lies against the diaphragm with no intervening gas. In pneumoperitoneum, gas may lie above the liver, obscuring the liver parenchyma. In contradistinction to shadowing from the lung edge, this gas does not move with respiration. Further, liver parenchyma may be seen superior to the free intraperitoneal gas, inferior to the lung margin (Figure 1). If the gas is traced inferiorly and medially, it can be seen to lie against the peritoneal line. The patient should be in a supine or left lateral decubitus position. 5 , 6 The liver capsule may appear similarly bright to free gas, but will not result in the loss of visualisation of the underlying liver architecture. Chilaiditi's anomaly is a variant where bowel is interposed between liver and diaphragm, which may appear similar. In this condition, examination with a high frequency linear probe will reveal that if the gas is traced across the abdomen, it is not in continuity with the peritoneal line and that Haustral folds can usually be seen. It could be postulated that a loculated basal pneumothorax may give a similar appearance of gas not moving and obscuring the liver, but this has not been described. Usually the clinical presentation of these conditions are distinct, but if there remains confusion then the signs described below could help to distinguish between these conditions.
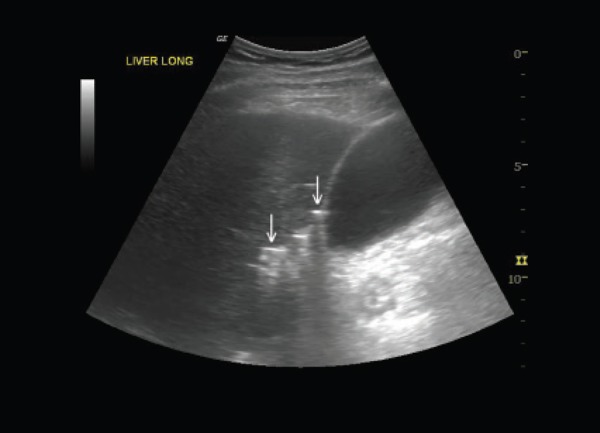
Figure 1.
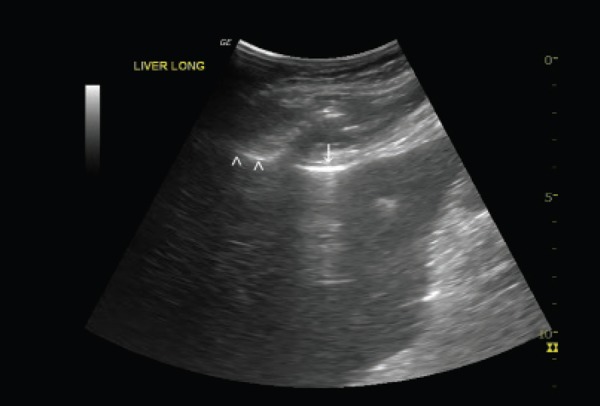
Gas is seen above the liver, obscuring the liver architecture (down pointing arrow). The normal lung was seen to move separately more superiorly (arrowheads).
Moveable gas
Free gas can move with patient positioning or probe pressure. Movement with patient repositioning has been described when doubt exists in whether gas is in bowel or within the peritoneal cavity. Usually the patient is rolled to a left lateral decubitus position and re‐examined. 7 With large quantities of free gas, probe pressure can be used to rapidly move the gas (providing pain and rigidity does not prevent the manoeuver). The pressure will cause the gas to ‘part’ creating an effect that has been described as similar to curtains parting or scissors opening 8 (Figures 2, 3, video 1).
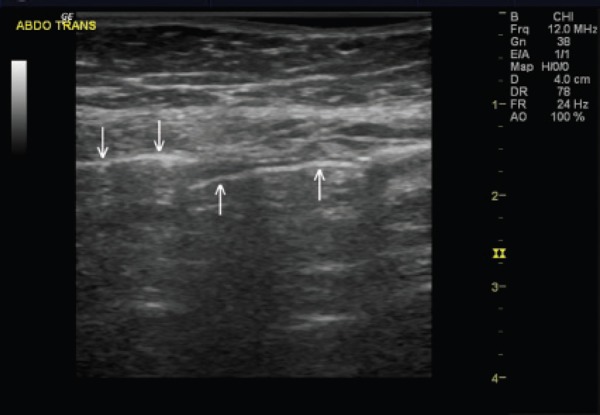
Figure 2.
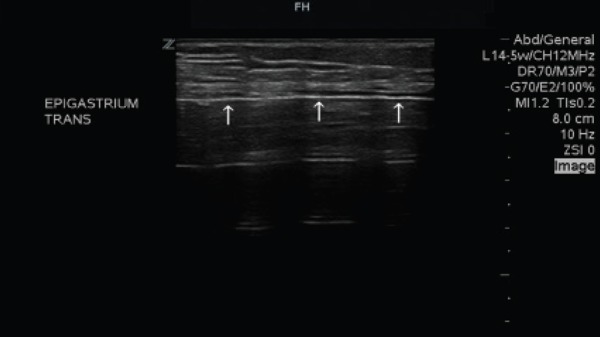
A bright echogenic line with gas shadowing behind it traverses the abdomen posterior to the abdominal wall (arrows).
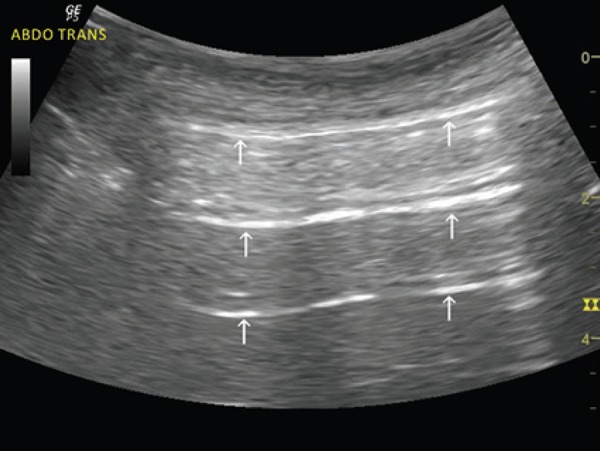
Figure 3.
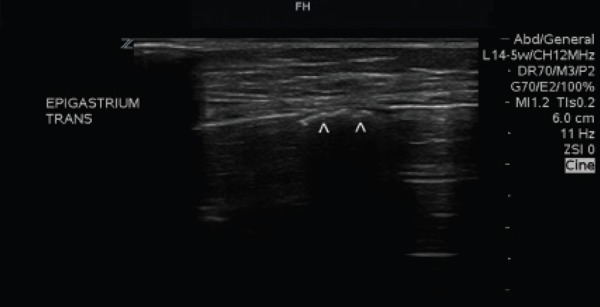
With probe pressure the line ‘opens’ to reveal gas within a loop of bowel beneath (arrowheads).
Video 1
Patient with abdominal pain of uncertain cause. A bright echogenic line with reverberation artefact posterior is seen across the abdomen.
Probe pressure results in the gas ‘parting’ to reveal the underlying bowel, confirming it is free intra‐abdominal gas.
YouTube Video Link: http://youtu.be/‐nk8jNpHbVA
Peritoneal line enhancement
As a strong reflector, gas creates a bright reflection which creates the appearance of thickening of the peritoneal line. 3 It is essential to ensure that the gas seen is adjacent to, or continuous with, the peritoneal line. Physiological gas, within bowel, will rise to be near the peritoneal line but will be separated from it by the bowel wall thickness, which will appear as a thin, hypoechoic line between the bright peritoneal line and the bright gas surface. Use of a high frequency linear transducer may be required to demonstrate this. In addition, gas within bowel will, if followed, be seen to either move away from the peritoneal line as the bowel loop folds deeper into the abdomen, or show the normal mucosal folds of bowel. Peristalsis or movement with respiration may also be observed, confirming the gas is within a loop of bowel. 9 The peritoneal line, by comparison, can be traced as a continuous line around the abdomen with no folds. The difference can be seen in Figure 4. If ascites is present, then the presence of gas against the peritoneal line is more easily visible (Figure 5).
Figure 4.
Downward arrow shows a bright gas reflection which is continuous with the peritoneal line, demonstrating free gas. Upward arrows show a bright gas reflection which curves away from the peritoneal line and is separated from it by a thin echolucent line, representing gas within bowel.
Figure 5.

Patient with known alcoholic liver disease who presented with pain and increased swelling. Gas shadowning is seen emanating from the peritoneal line (arrowheads) which is easily seen due to the ascites.
Gas outside bowel
Gas may be seen in anatomical locations where it does not occur physiologically. The most common site in patients with an acute abdomen is around the porta hepatis as a result of peptic ulcer perforation. Small gas locules may be seen around the gall bladder and under the liver (Figure 6). Colonic perforation usually results in a large amount of free gas, which is easily seen on ultrasound. 10 Intra‐abdominal or retroperitoneal abscesses (e.g. appendiceal, diverticular or post operative) can cause small collections of gas outside bowel. Uncomplicated diverticular disease can result in gas locules that may appear to be outside the bowel lumen, although the mucosa may be visible surrounding the gas. 11 Gas in superficial structures (cutaneous emphysema and intramuscular gas) can also give a similar appearance, but will be superficial to the peritoneal line and lack the mobility of intraperitoneal gas.
Other described signs
Analogous to the prominent ‘A lines’ seen in pneumothorax, the bright, evenly spaced reverberation artefacts arising from a large collection of gas can be expected in a large pneumoperitoneum. 12 However, this can also occur in dilated gut or stomach, and so should be interpreted with caution (Figures 6,7,8).
Figure 6.
Small locules of gas are seen outside bowel in the gallbladder fossa and porta hepatis (arrows).
Figure 7.
Bright, regular spaced reverberation artifacts (analogous to lung A‐lines) are seen. It is not clear if they originate from the peritoneal line or not in this image (subsequent imaging with a high frequency linear probe revealed the bowel wall thickness separating the reflection from the peritoneal line).
Figure 8.
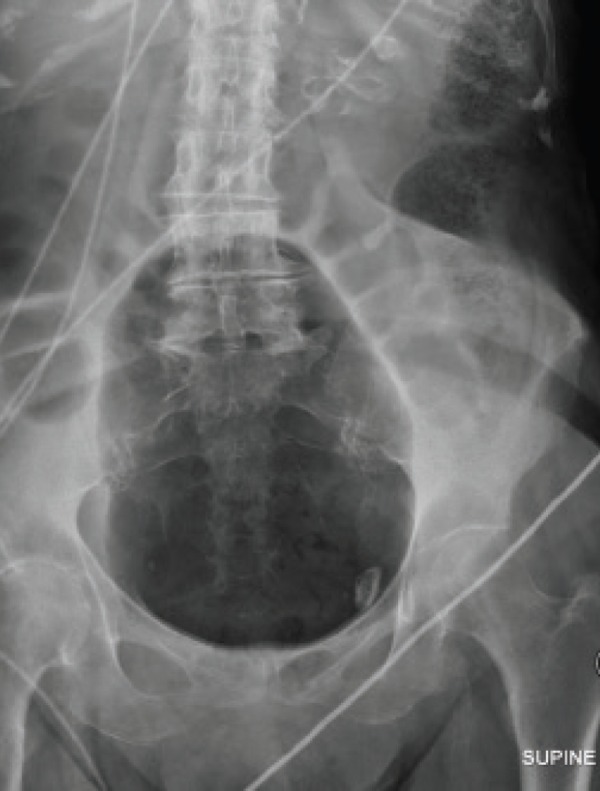
Plain X‐Ray demonstrating the dilated and gas filled bowel that gave rise to the artefact.
Accuracy
Early animal models and series of post laparoscopy patients suggested that ultrasound was sensitive in detecting even small amounts of free intraperitoneal gas. Prospective series of patients with abdominal trauma or abdominal pain have confirmed that ultrasound has a high sensitivity (85–100%). 4 , 6 , 8 , 13 , 14 Most studies also show a high specificity (84–100%), although in one series it was 53%, which was the equivalent of plain radiography in that study. 10 Overall, these studies consistently demonstrate that ultrasound is as accurate as plain radiography, although CT remains the imaging gold standard.
Limitations
Ultrasound examination of the patient with abdominal pain may be limited due to the degree of tenderness and guarding, as may be the ability for the patient to be repositioned. This may prevent performing many of the manoeuvres described above. Technical settings, particularly high level edge enhancement, may give the appearance of a thin black line superficial to the bright gas surface, which may be confused for bowel wall thickness rather than demonstrating the gas lies on the peritoneal line. Sweeping the probe across to determine if this is the peritoneal line can avoid this confusion. Finally, small amounts of gas, particularly those that have not risen to the peritoneal line, may be difficult or impossible to see by ultrasound due to overlying bowel gas.
Conclusion
Although not usually considered the first line investigation for possible hollow organ perforation and not as sensitive as CT, ultrasound can usually detect signs of pneumoperitoneum if present. As patients with undiagnosed abdominal pain often undergo ultrasound as part of the diagnostic process, all ultrasound users should be aware of these signs.
References
- 1. Mendelson R. Diagnostic Imaging Pathways. Perth: Health Dept Western Australia; 2012. Available at http://www.imagingpathways.health.wa.gov.au/includes/index.html. Accessed 28th December 2012. [Google Scholar]
- 2. Anderson SW, Lucey BC, Soto JA. Nontrauma Abdomen. In: Soto JA, Lucey BC, editors. Emergency Radiology: The Requisites. Philadelphia: Elsevier; 2009. pp. 275–309. [Google Scholar]
- 3. Muradali D, Wilson S, Burns PN, Shapiro H, Hope‐Simpson D. A specific sign of pneumoperitoneum on sonography: enhancement of the peritoneal stripe. AJR Am J Roentgenol 1999; 173 (5): 1257–62. [DOI] [PubMed] [Google Scholar]
- 4. Hoffmann B, Nurnberg D, Westergaard MC. Focus on abnormal air: diagnostic ultrasonography for the acute abdomen. Eur J Emerg Med 2012; 19 (5): 284–91. [DOI] [PubMed] [Google Scholar]
- 5. Lee DH, Lim JH, Ko YT, Yoon Y. Sonographic detection of pneumoperitoneum in patients with acute abdomen. AJR Am J Roentgenol 1990; 154 (1): 107–09. [DOI] [PubMed] [Google Scholar]
- 6. Braccini G, Lamacchia M, Boraschi P, Bertellotti L, Marrucci A, Goletti O, et al. Ultrasound versus plain film in the detection of pneumoperitoneum. Abdom Imaging 1996; 21 (5): 404–12. [DOI] [PubMed] [Google Scholar]
- 7. Gee P. Shifting Gas Artefact Sign: Early sonographic detection of pneumoperitoneum. Emerg Med Australas 2011; 23 (5): 647–50. [DOI] [PubMed] [Google Scholar]
- 8. Karahan OI, Kurt A, Yikilmaz A, Kahriman G. New method for the detection of intraperitoneal free air by sonography: scissors maneuver. J Clin Ultrasound 2004; 32 (8): 381–85. [DOI] [PubMed] [Google Scholar]
- 9. Lichtenstein DA. Whole Body Ultrasonography in the Critically Ill. Heidelberg: Springer; 2010. [Google Scholar]
- 10. Chen SC, Yen ZS, Wang HP, Lin FY, Hsu CY, Chen WJ. Ultrasonography is superior to plain radiography in the diagnosis of pneumoperitoneum. Br J Surg 2002; 89 (3): 351–54 [DOI] [PubMed] [Google Scholar]
- 11. Rodgers PM, Verma R. Transabdominal ultrasound for bowel evaluation. Radiol Clin North Am 2013; 51 (1): 133–48. [DOI] [PubMed] [Google Scholar]
- 12. Bowmann JS. Abdominal a‐lines: a simpler sonographic sign of pneumoperitoneum. Crit Ultrasound J. 2011; 3: 41–42. [Google Scholar]
- 13. Moriwaki Y, Sugiyama M, Toyoda H, Kosuge T, Arata S, Iwashita M, et al. Ultrasonography for the diagnosis of intraperitoneal free air in chest‐abdominal‐pelvic blunt trauma and critical acute abdominal pain. Arch Surg 2009; 144 (2): 137–41. Discussion 42. [DOI] [PubMed] [Google Scholar]
- 14. Asrani A. Sonographic diagnosis of pneumoperitoneum using the ‘enhancement of the peritoneal stripe sign.’ A prospective study. Emerg Radiol 2007; 14 (1): 29–39. [DOI] [PubMed] [Google Scholar]


