Abstract
Context
Heart failure (HF) is the most common complication of infective endocarditis. However, clinical characteristics of HF in patients with infective endocarditis, use of surgical therapy, and their associations with patient outcome are not well described.
Objectives
To determine the clinical, echocardiographic, and microbiological variables associated with HF in patients with definite infective endocarditis and to examine variables independently associated with in-hospital and 1-year mortality for patients with infective endocarditis and HF, including the use and association of surgery with outcome.
Design, Setting, and Patients
The International Collaboration on Endocarditis–Prospective Cohort Study, a prospective, multicenter study enrolling 4166 patients with definite native- or prosthetic-valve infective endocarditis from 61 centers in 28 countries between June 2000 and December 2006.
Main Outcome Measures
In-hospital and 1-year mortality.
Results
Of 4075 patients with infective endocarditis and known HF status enrolled, 1359 (33.4% [95% CI, 31.9%–34.8%]) had HF, and 906 (66.7% [95% CI, 64.2%–69.2%]) were classified as having New York Heart Association class III or IV symptom status. Within the subset with HF, 839 (61.7% [95% CI, 59.2%–64.3%]) underwent valvular surgery during the index hospitalization. In-hospital mortality was 29.7% (95% CI, 27.2%–32.1%) for the entire HF cohort, with lower mortality observed in patients undergoing valvular surgery compared with medical therapy alone (20.6% [95% CI, 17.9%–23.4%] vs 44.8% [95% CI, 40.4%–49.0%], respectively; P<.001). One-year mortality was 29.1% (95% CI, 26.0%–32.2%) in patients undergoing valvular surgery vs 58.4% (95% CI, 54.1%–62.6%) in those not undergoing surgery (P<.001). Cox proportional hazards modeling with propensity score adjustment for surgery showed that advanced age, diabetes mellitus, health care–associated infection, causative microorganism (Staphylococcus aureus or fungi), severe HF (New York Heart Association class III or IV), stroke, and paravalvular complications were independently associated with 1-year mortality, whereas valvular surgery during the initial hospitalization was associated with lower mortality.
Conclusion
In this cohort of patients with infective endocarditis complicated by HF, severity of HF was strongly associated with surgical therapy and subsequent mortality, whereas valvular surgery was associated with lower in-hospital and 1-year mortality.
Infective endocarditis is associated with substantial morbidity and mortality. Several published studies have reported in-hospital mortality of 15% to 20% and 1-year mortality of 40%.1 In the United States alone, approximately 15 000 new cases of infective endocarditis are diagnosed each year.1 A variety of complications contribute to the high rates of morbidity and mortality in infective endocarditis, particularly heart failure (HF), which occurs in approximately 40% of patients.2,3 Several observational studies have shown a mortality benefit for valvular surgery in infective endocarditis complicated by HF,2 and this indication for surgery is strongly recommended in current American College of Cardiology/American Heart Association and European Society of Cardiology guidelines.4,5
The patient characteristics associated with HF in those with infective endocarditis are not clearly defined. Furthermore, the use and timing of valvular surgery in patients with infective endocarditis and HF have been evaluated, with conflicting results. Several studies have reported no reduction of in-hospital mortality with valvular surgery compared with medical therapy alone,6–8 whereas other investigators have observed an early and sustained mortality benefit.2,9
The objectives of the present study were to determine the clinical, echocardiographic, and microbiological variables associated with the development of HF in patients with definite infective endocarditis and to examine variables independently associated with in-hospital and 1-year mortality for patients with infective endocarditis and HF, including the use and effects of surgery on outcome.
METHODS
Data from the International Collaboration on Endocarditis–Prospective Cohort Study (ICE-PCS) were used for this study. The background and inclusion criteria of this prospective, multicenter, international registry of infective endocarditis have been reported.10,11 Between June 2000 and December 2006, 4166 patients with definite native- or prosthetic-valve endocarditis by the modified Duke criteria from 61 centers in 28 countries were enrolled.12 The ICE-PCS database is maintained at the Duke Clinical Research Institute, which is the coordinating center for International Collaboration on Endocarditis studies. Informed consent (oral or written) was obtained from patients as needed according to institutional review board or ethics committee guidelines at each center.
Patient Selection and Data Collection
Patients were identified prospectively using site-specific procedures to ensure consecutive enrollment.10,12,13 To provide a cross-sectional, prospective characterization of infective endocarditis and in-hospital outcome, patients were enrolled in ICE-PCS if they met criteria for possible or definite infective endocarditis based on modified Duke criteria.13 Only patients with definite infective endocarditis were included in the current study. To preserve the assumption of independence of observations, only the first episode of infective endocarditis recorded for an individual patient during study enrollment was used in the analysis.
The method of data collection for ICE-PCS has been reported.14 Briefly, a standard case report form was used at all sites to collect data. This case report form included 275 variables and was developed by the International Collaboration on Endocarditis according to standard definitions. Data were collected during the index hospitalization and entered at the coordinating center or by site investigators using an Internet-based data entry system.
To describe longer-term outcome of infective endocarditis, sites enrolling patients in ICE-PCS were queried in 2008 regarding 1-year outcome of these patients. An additional case report form was used to collect data retrospectively from the date of index hospital admission to 1 year. One-year outcome was determined by site investigators using medical records and national death records, as available.
Definitions
The definitions used in the ICE-PCS data set have been described.14 The presence of HF was determined by physicians at each enrolling site based on clinical symptoms, signs, and laboratory and radiographic findings.15 Severity of heart failure was categorized according to New York Heart Association (NYHA) functional classification.14 Paravalvular complication was defined as transthoracic or transesophageal echocardiographic evidence of intracardiac abscess or fistula.16,17 Health care–associated infective endocarditis was specified as nosocomial or nonnosocomial acquisition of health care–associated infective endocarditis.18,19 Stroke was defined as acute development of a neurologic deficit of vascular origin lasting more than 24 hours.14 Prosthetic valve was defined as any nonnative valve (eg, mechanical, bioprosthetic, homograft, or autograft) or annuloplasty ring.
Statistical Analysis
Patient demographic and clinical variables were evaluated with counts and percentages in contingency tables or with medians and interquartile ranges (IQRs). The statistical significance of the associations between congestive heart failure and these variables were assessed using the Kruskal-Wallis test for continuous measures and the Fisher exact test for cross-classifications of categorical data. Risk estimates for in-hospital mortality are presented as odds ratios (ORs) and 95% confidence intervals. Associations with P<.05 were considered statistically significant; all significance tests were 2-sided.
Multivariable logistic regression modeling to evaluate surgical treatment for endocarditis was performed to determine the factors independently associated with surgery among patients with HF. This model included all demographic and clinical variables considered a priori by an experienced cardiologist (A.W.) to contribute to surgical treatment of endocarditis and included age in 4 categories (≤45 years, 46–60 years, 61–70 years, >70 years), sex, geographic region (North America, South America, Europe, other), time since first manifestation of infective endocarditis, transfer from another facility, diabetes mellitus, hemodialysis, injection drug use, valve status (native, prosthetic), location of infective endocarditis (left- or right-sided), health care–associated infective endocarditis, new valvular regurgitation, intravascular vegetation, paravalvular complications, stroke, embolization, persistent bacteremia, NYHA class III or IV (vs NYHA class I or II), positive blood culture result, and causative microorganism. The patients’ probabilities for surgical treatment derived from this model were used to calculate inverse probability of surgery weights as described previously,20 and these were used as weights in proportional hazards models.
To evaluate the factors associated with mortality among patients with HF, proportional hazards models were fit for in-hospital mortality and for all mortality through 1 year after discharge. These models included as variables the patient demographic and clinical data. To account for individual differences in time between admission and surgery, surgery was modeled as a time-dependent factor. These models were further weighted by the inverse probability of treatment using the propensity score for surgery, which we derived from the logistic model previously described. All analyses were performed using SAS version 9.2.
RESULTS
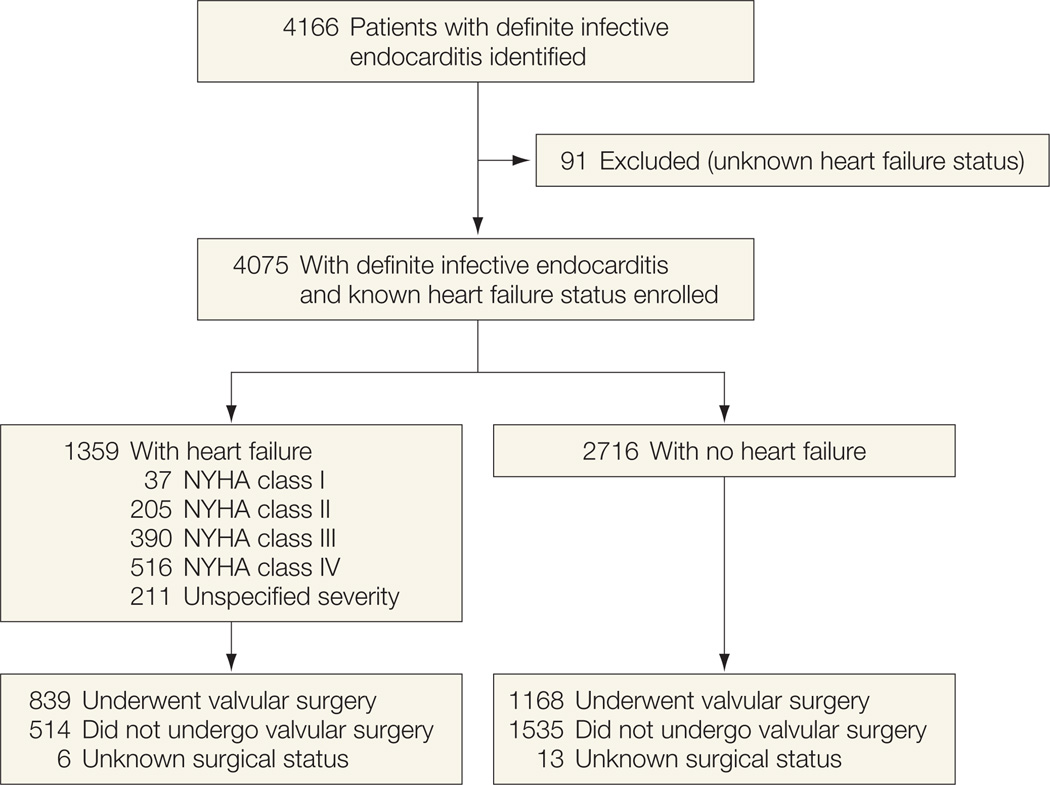
The study population is shown in Figure 1. Within the ICE-PCS cohort of patients with definite infective endocarditis and known HF status (n=4075), HF was present in 1359 (33.4% [95% CI, 31.9%–34.8%]) and absent in 2716 (66.6% [95% CI, 65.2%–68.1%]). Heart failure status was not specified in an additional 91 patients (2.2% [95% CI, 1.7%–2.6%]). Among the patients with HF, the distribution of HF severity included NYHA class I symptom status in 37 patients (2.7% [95% CI, 1.9%–3.6%]), NYHA class II in 205 (15.1% [95% CI, 13.2%–17.0%]), NYHA class III in 390 (28.7% [95% CI, 26.3%–31.1%]), NYHA class IV in 516 (38.0% [95% CI, 35.4%–40.5%]), and unspecified HF severity in 211 (15.5% [95% CI, 13.6%–17.5%]). During the years of patient enrollment, the percentage of patients with infective endocarditis and HF ranged from 30% to 35%, without variation in incidence. For 2457 patients with available chest radiography data (before the removal of this variable from the case report forms in August 2005), radiographic evidence of pulmonary edema was present in 6 of 23 (26.1% [95% CI, 8.1%–44.0%]) patients with NYHA class I symptoms, 35 of 124 (28.2% [95% CI, 20.3%–36.1%]) with NYHA class II symptoms, 99 of 251 (39.4% [95% CI, 33.4%–45.5%]) with NYHA class III symptoms, and 194 of 312 (62.2% [95% CI, 56.8%–67.6%]) with NYHA class IV symptoms.
Figure 1.
Study Population of Patients With Infective Endocarditis
The baseline characteristics of the overall study population are shown in Table 1. Older age, transfer from another hospital, health care–associated infection, new or worsening murmur, left-sided native-valvular infection with new aortic or mitral regurgitation, and paravalvular complications were significantly more common in patients with HF. For patients with infective endocarditis with or without HF, the prevalence of congenital heart disease (8.7% [95% CI, 7.3%–10.4%] vs 9.8% [95% CI, 8.7%–11.0%], respectively) and predisposing native-valve disease (33.5% [95% CI, 31.0%–36.1%] vs 31.0% [95% CI, 29.3%–32.8%], respectively) were not statistically different.
Table 1.
Comparison of Patients With or Without Heart Failure Complicating Infective Endocarditis
| No. (%) | ||||
|---|---|---|---|---|
| Characteristic | Heart Failure (n = 1359) |
No Heart Failure (n = 2716) |
P Value |
|
| Age, median (IQR), y | 59.4 (47.4–73.2) | 56.9 (43.5–71.3) | <.001 | |
| Men | 914 (67.3) | 1858 (68.5) | .41 | |
| Region | ||||
| North America | 247 (18.2) | 456 (16.8) | <.001 | |
| South America | 164 (12.1) | 205 (7.5) | ||
| Europe | 707 (52.0) | 1391 (51.2) | ||
| Other | 241 (17.7) | 664 (24.4) | ||
| Transferred from another facility | 672 (49.9) | 1113 (41.4) | <.001 | |
| Diabetes mellitus | 257 (19.4) | 434 (16.1) | .01 | |
| Hemodialysis | 93 (6.8) | 198 (7.3) | .65 | |
| Congenital heart disease | 115 (8.7) | 257 (9.8) | .30 | |
| Predisposing native-valve disease | 443 (33.5) | 829 (31.0) | .11 | |
| Health care–associated infection | 339 (26.2) | 586 (22.7) | .02 | |
| New or worsening murmur | 822 (60.5) | 1213 (44.7) | <.001 | |
| Causative microorganism | ||||
| Staphylococcus aureus | 381 (28.0) | 833 (30.7) | .09 | |
| Viridans group streptococcus | 206 (15.2) | 510 (18.8) | .005 | |
| Infective endocarditis | ||||
| Left-sided, native valve | 871 (64.1) | 1533 (56.4) | <.001 | |
| Left-sided, prosthetic valve | 244 (18.0) | 459 (16.9) | .40 | |
| Right-sided vegetation only | 116 (9.1) | 413 (16.1) | <.001 | |
| New aortic regurgitation | 597 (44.9) | 719 (27.2) | <.001 | |
| New mitral regurgitation | 577 (43.1) | 857 (32.3) | <.001 | |
| Paravalvular complication | 426 (31.8) | 561 (20.9) | <.001 | |
Abbreviation: IQR, interquartile range.
Of the 1359 patients with HF, 839 (61.7% [95% CI, 59.2%–64.3%]) underwent valvular surgery during the initial hospitalization, compared with 1168 (43.0% [95% CI, 41.1%–44.9%]) without HF (OR, 2.15 [95% CI, 1.88–2.45]; P<.001) (Figure 1). The frequency of valvular surgery by year did not change consistently during the study period (range, 44%–53%). In addition, the median duration from hospital admission to surgery did not differ between the groups with and without HF (7 [IQR, 2–18] days vs 8 [IQR, 3–20] days, P=.10). Surgical valvular procedures included aortic valve surgery (n=612, including mechanical valve replacement in 274, xenograft biologic replacement in 192, homograft in 60, repair in 21, and autograft in 6); mitral valve surgery (n=429, including mechanical valve replacement in 204, xenograft biologic replacement in 108, and repair in 106); and tricuspid valve surgery (n=93, including repair in 59, xenograft biologic replacement in 19, and mechanical valve replacement in 7). For patients with heart failure in infective endocarditis, clinical characteristics as a function of surgical therapy are shown in Table 2. One hundred twenty-six of 240 (52.5% [95% CI, 46.2%–58.8%]) patients with NYHA class I or II symptoms and 572 of 904 (63.3% [95% CI, 60.1%–6.4%]) with NYHA class III or IV symptoms underwent surgery.
Table 2.
Characteristics of Patients With Infective Endocarditis and Heart Failure Associated With Surgerya
| No. (%) [95% CI] | |||||
|---|---|---|---|---|---|
| Characteristic | Surgery (n = 839) |
No Surgery (n = 514) |
P Value |
OR (95% CI) | |
| Age, y | |||||
| ≤45 | 220 (26.2) [23.2–29.2] | 65 (12.6) [9.8–15.5] | <.001 | 4.60 (2.75–7.69) | |
| 46–60 | 242 (28.8) [25.8–31.9] | 117 (22.8) [19.1–26.4] | 3.11 (2.02–4.80) | ||
| 61–70 | 183 (21.8) [19–24.6] | 88 (17.1) [13.9–20.4] | 2.92 (1.93–4.42) | ||
| >70 | 194 (23.1) [20.3–26.0] | 244 (47.5) [43.2–51.8] | 1 [Reference] | ||
| Men | 605 (72.1) [69.1–75.1] | 305 (59.3) [55.1–63.6] | <.001 | NAb | |
| Region | |||||
| North America | 144 (17.2) [14.6–19.7] | 102 (19.8) [16.4–23.3] | .004 | NAb | |
| South America | 113 (13.5) [11.2–15.8] | 51 (9.9) [7.3–12.5] | |||
| Europe | 454 (54.1) [50.7–57.5] | 250 (48.6) [44.3–53.0] | |||
| Other | 128 (15.3) [12.8–17.7] | 111 (21.6) [18.0–25.2] | |||
| ≥1 mo since first infective endocarditis manifestation | 234 (27.9) [24.9–30.9] | 65 (12.6) [9.8–15.5] | <.001 | 1.69 (1.12–2.54) | |
| Transferred from another facility | 485 (57.8) [54.5–61.1] | 186 (36.2) [32.0–40.3] | <.001 | 1.83 (1.33–2.51 | |
| Diabetes mellitus | 125 (14.9) [12.5–17.3] | 131 (25.5) [21.7–29.3] | <.001 | ||
| Hemodialysis | 35 (4.2) [2.8–5.5] | 57 (11.1) [8.4–13.8] | <.001 | 0.36 (0.18–0.75) | |
| Left-sided, native-valve infective endocarditis | 565 (67.3) [64.2–70.5] | 302 (58.8) [54.5–63.0] | .002 | 1.61 (1.06–2.44) | |
| Health care–associated infection | 164 (19.5) [16.9–22.2] | 172 (33.5) [29.4–37.5] | <.001 | NAb | |
| Causative microorganism | |||||
| Staphylococcus aureus | 179 (21.3) [18.6–24.1] | 200 (38.9) [34.7–43.1] | <.001 | 0.52 (0.31–0.86) | |
| Viridans group streptococcus | 139 (16.6) [14.1–19.1] | 67 (13.0) [10.1–15.9] | .09 | ||
| NYHA class III or IV | 572 (68.2) [65–71.3] | 332 (64.6) [60.5–68.7] | .003 | 2.15 (1.49–3.11) | |
| New valve regurgitation | 698 (83.2) [80.7–85.7] | 336 (66.4) [61.3–69.5] | <.001 | 1.79 (1.23–2.60) | |
| Paravalvular complication | 327 (39.0) [35.7–42.3] | 99 (19.3) [15.9–22.7] | <.001 | 3.07 (2.15–4.39) | |
| Stroke | 153 (18.2) [15.6–20.8] | 135 (26.3) [22.5–30.1] | <.001 | NAb | |
Abbreviations: NYHA, New York Heart Association; OR, odds ratio; NA, not applicable.
ORs and CIs calculated from the multivariable logistic model used to determine the propensity score for surgical treatment.
Not statistically significant in multivariable model.
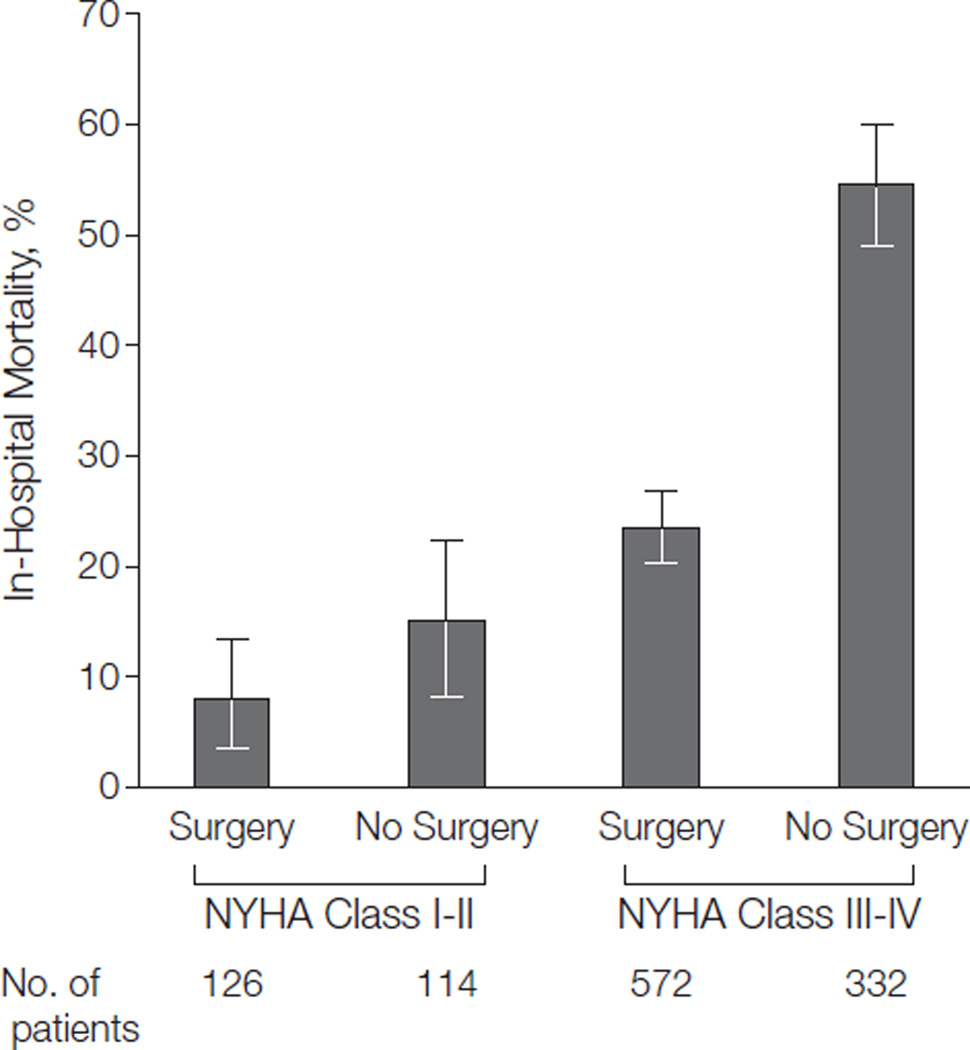
The presence of HF with infective endocarditis was associated with significantly higher in-hospital mortality when compared with infective endocarditis without HF (29.7% [95% CI, 27.2%–32.1%] vs 13.1% [95% CI, 11.8%–14.4%], respectively; OR, 2.80 [95% CI, 2.38–3.29]; P<.001). The median duration of hospitalization for patients with HF (28 [IQR, 15–47] days) was similar to that for patients without HF (29 [IQR, 16–44] days) (P=.63). Patients with HF who underwent surgical intervention had a significantly lower unadjusted in-hospital mortality rate compared with patients with HF not undergoing surgery (20.6% [95% CI, 17.9%–23.4%] vs 44.7% [95% CI, 40.4%–49.0%], respectively; P<.001). Among patients with NYHA class I or II HF, the mortality rate in surgically treated patients was 7.9% (95% CI, 3.2%–12.7%), vs 15.0% (95% CI, 8.5%–21.6%) in those not surgically treated (P=.03); for those with NYHA class III or IV HF, corresponding mortality rates were 23.4% (95% CI, 20.0%–26.9%) vs 54.5% (95% CI, 49.2%–59.9%), respectively (P<.001) (Figure 2).
Figure 2.
In-Hospital Mortality Rates for Patients With Infective Endocarditis and Heart Failure as a Function of Surgical Treatment
Fisher exact P<.05 for surgery vs no surgery in the New York Heart Association (NYHA) class I–II cohort; P<.001 for surgery vs no surgery in the NYHA class III–IV cohort. Error bars indicate 95% confidence intervals.
Survival status at 1 year after index admission date was available for 1202 of 1358 patients (88.5%); 544 of 1358 patients with HF during the index hospitalization (40.1% [95% CI, 37.6%–42.8%]) had died. The 1-year mortality rate was 29.1% (244/839 [95% CI, 26.0%–32.2%]) for patients treated with surgery vs 58.4% (300/514 [95% CI, 54.1%–62.6%]) for patients treated with medical therapy alone during the index hospitalization (relative risk, 0.50 [95% CI, 0.43–0.57]; P<.001).
To reduce the potential selection bias for the use of surgery, propensity score adjustment (area under the curve, 0.797 for the multivariable model) by inverse probability weighting was performed (Table 3). In the Cox proportional hazards model with surgery included as a time-dependent covariate to account for survivor treatment bias, severity of HF (NYHA class III or IV), age older than 70 years, causative microorganism, duration of infective endocarditis symptoms before diagnosis, diabetes mellitus, stroke, and paravalvular complications were independently associated with in-hospital death (Table 3). Surgery during the initial hospitalization was statistically associated with a lower risk of in-hospital mortality (OR, 0.66 [95% CI, 0.56–0.77]).
Table 3.
Cox Proportional Hazards Modeling of Variables Independently Associated With In-Hospital and 1-Year Mortality, With Propensity Adjustment for Cardiac Surgery
| In-Hospital Mortality | 1-Year Mortality | |||
|---|---|---|---|---|
| Variable | No./Total (%) [95% CI] | HR (95% CI) | No./Total (%) [95% CI] | HR (95% CI) |
| Age, y | ||||
| ≤45 | 104/1036 (10.0) [8.2–11.9] | 1 [Reference] | 158/1040 (15.2) [13.0–17.4] | 1 [Reference] |
| 46–60 | 165/1071 (15.4) [13.2–17.6] | 2.06 (1.49–2.90) | 234/1071 (21.8) [19.4–24.3] | 1.44 (1.13–1.84) |
| 61–70 | 159/840 (18.9) [16.3–21.6] | 2.37 (1.70–3.36) | 208/840 (24.8) [21.8–27.7] | 1.62 (1.26–2.09) |
| >70 | 359/1209 (29.7) [27.1–32.3] | 3.76 (2.79–5.17) | 455/1213 (37.5) [34.8–40.2] | 2.40 (1.92–3.02) |
| ≥1 mo from symptoms of infective endocarditis to diagnosis |
||||
| No | 647/3075 (21.0) [19.6–22.5] | 1 [Reference] | 864/3081 (28.0) [26.5–29.6] | 1 [Reference] |
| Yes | 101/909 (11.1) [9.1–13.2] | 0.81 (0.66–0.99) | 138/911 (15.1) [12.8–17.5] | 0.75 (0.62–0.91) |
| Geographic region | ||||
| Europe | 446/2156 (20.7) [19.0–22.4] | 1 [Reference] | 553/2162 (25.6) [23.7–27.4] | 1 [Reference] |
| North America | 129/709 (18.2) [15.4–21.0] | 1.19 (0.95–1.48) | 228/710 (32.1) [28.7–35.5] | 0.98 (0.82–1.17) |
| South America | 73/372 (19.6) [15.6–23.7] | 1.40 (1.08–1.80) | 87/372 (23.4) [19.1–27.7] | 1.03 (0.82–1.29) |
| Other | 139/919 (15.1) [12.8–17.4] | 0.49 (0.37–0.62) | 187/920 (20.3) [17.7–22.9] | 0.47 (0.38–0.59) |
| Diabetes mellitus | ||||
| No | 560/3388 (16.5) [15.3–17.8] | 1 [Reference] | 762/3394 (22.5) [21.0–23.9] | 1 [Reference] |
| Yes | 208/700 (29.7) [26.3–33.1] | 1.33 (1.10–1.58) | 272/702 (38.7) [35.1–42.4] | 1.34 (1.14–1.57) |
| Health care–associated infection | ||||
| No | 436/3002 (14.5) [13.3–15.8] | 1 [Reference] | 584/3007 (19.4) [18.0–20.8] | 1 [Reference] |
| Yes | 306/949 (32.2) [29.3–35.2] | NAa | 412/951 (43.3) [40.2–46.5] | 2.02 (1.62–2.53) |
| Causative microorganism | ||||
| Viridans group streptococcus | ||||
| No | 727/3431 (21.2) [19.8–22.6] | 1 [Reference] | 964/3437 (28.0) [26.5–29.5] | 1 [Reference] |
| Yes | 60/725 (8.3) [6.3–10.3] | 0.65 (0.48–0.86) | 91/727 (12.5) [10.1–14.9] | 0.77 (0.59–0.98) |
| Streptococcus bovis | ||||
| No | 760/3884 (19.6) [18.3–20.8] | 1 [Reference] | 1015/3892 (26.1) [24.7–27.5] | 1 [Reference] |
| Yes | 27/272 (9.9) [6.4–13.5] | 0.45 (0.28–0.68) | 40/272 (14.7) [10.5–18.9] | 0.58 (0.40–0.82) |
| Staphylococcus aureus | ||||
| No | 458/2916 (15.7) [14.4–17.0] | 1 [Reference] | 623/2921 (21.3) [19.8–22.8] | 1 [Reference] |
| Yes | 329/1240 (26.5) [24.1–29.0] | NAa | 432/1243 (34.8) [32.1–37.4] | 1.31 (1.12–1.53) |
| Fungi | ||||
| No | 758/4086 (18.6) [17.4–19.7] | 1 [Reference] | 1016/4094 (24.8) [23.5–26.1] | 1 [Reference] |
| Yes | 29/70 (41.4) [29.9–53.0] | NAa | 39/70 (55.7) [44.1–67.4] | 1.77 (1.09–2.71) |
| NYHA class III or IV | ||||
| No | 382/2957 (12.9) [11.7–14.1] | 1 [Reference] | 560/2959 (18.9) [17.5–20.3] | 1 [Reference] |
| Yes | 316/910 (34.7) [31.6–37.8] | 3.38 (2.54–4.60) | 385/910 (42.3) [39.1–45.5] | 3.03 (2.45–3.80) |
| Paravalvular complication | ||||
| No | 521/3093 (16.8) [15.5–18.2] | 1 [Reference] | 720/3099 (23.2) [21.7–24.7] | 1 [Reference] |
| Yes | 250/1009 (24.8) [22.1–27.4] | 1.66 (1.42–1.95) | 315/1011 (31.2) [28.3–34.0] | 1.48 (1.28–1.70) |
| Stroke | ||||
| No | 485/3284 (14.8) [13.6–16.0] | 1 [Reference] | 704/3285 (21.4) [20.0–22.8] | 1 [Reference] |
| Yes | 276/800 (34.5) [31.2–37.8] | 1.61 (1.36–1.89) | 323/801 (40.3) [36.9–43.7] | 1.49 (1.28–1.72) |
| Surgery | ||||
| No | 463/2092 (22.1) [20.4–23.9] | 1 [Reference] | 634/2094 (30.3) [28.3–32.2] | 1 [Reference] |
| Yes | 321/2044 (15.7) [14.1–17.3] | 0.76 (0.58–0.99) | 415/2047 (20.3) [18.5–22.0] | 0.44 (0.34–0.56) |
Abbreviations: HR, hazard ratio; NYHA, New York Heart Association; NA, no association.
Variable not statistically associated with in-hospital mortality in the model (but associated with 1-year mortality in subsequent model).
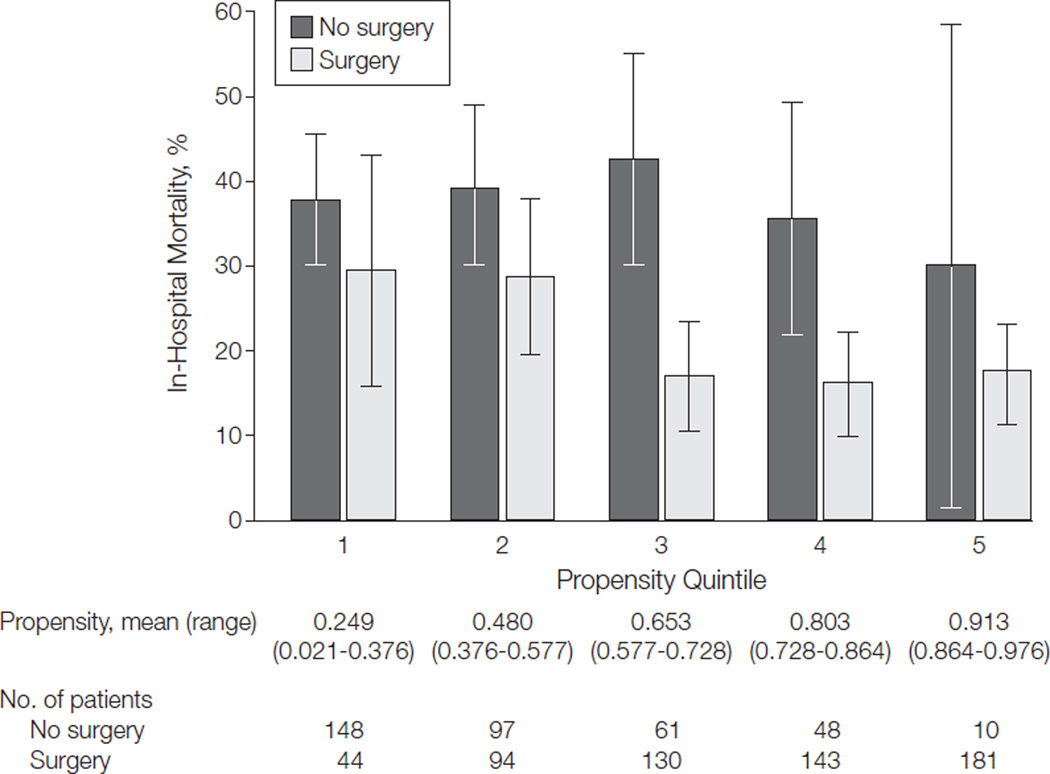
The association between surgery and lower in-hospital mortality was evident across the quintiles of surgical propensity and most prominent in quintiles 3 and 4 (Figure 3). The distribution of propensity scores for surgically and nonsurgically treated patients demonstrated that 29% of patients with propensity scores in quintiles 3, 4, or 5 (propensity score >0.6) did not have surgery during the index hospitalization (eFigure, available at http://www.jama.com). In a manner similar to that for in-hospital outcome, 1-year mortality was independently associated with age older than 70 years, diabetes mellitus, and paravalvular complications of infective endocarditis, as well as health care–associated infection, causative microorganism, and severity of HF, with a higher survival rate for patients having surgery during the index hospitalization in a propensity-adjusted analysis (Table 3).
Figure 3.
In-Hospital Mortality Rates for Surgically vs Nonsurgically Treated Patients Across Propensity Quintiles
Fisher exact P<.001 for surgery vs no surgery in propensity quintile 3; P<.01 for surgery vs no surgery in propensity quintile 4. Error bars indicate 95% confidence intervals.
COMMENT
Heart failure is a common complication of infective endocarditis and a major influence on the high morbidity and mortality associated with this serious condition. The main findings of the current study, to our knowledge the largest prospective, multinational evaluation of HF in patients with infective endocarditis to date, are that (1) HF was strongly related to new or worsening left-sided valvular regurgitation, rather than to predisposing heart conditions (eg, previous native-valve disease, presence of a prosthetic valve, or congenital heart disease) or causative microorganism; (2) despite a high incidence of severe HF and its poor prognosis, less than two-thirds of patients with infective endocarditis and HF underwent surgery, which was more frequently performed in younger patients with severe HF and paravalvular complications; and (3) surgery was associated with a significant reduction in in-hospital and 1-year mortality after adjustment for selection and survival biases and across the spectrum of HF severity and surgical propensity.
Previous studies have reported a prevalence of HF with left-sided infective endocarditis ranging from 19% to 44%.9,21–23 In the present work, HF occurred in 33% of definite cases of infective endocarditis, with a high percentage of severe (NYHA class III or IV) symptoms occurring shortly after diagnosis of endocarditis. Clinical characteristics previously associated with the development of HF in patients with infective endocarditis include new heart murmur, aortic valve infective endocarditis, high comorbidity index, and severe valvular regurgitation.22 Our findings confirm these earlier results and suggest that a greater degree of new valvular regurgitation was related to the development of HF. Of note, preexisting heart conditions, such as native-valve disease, presence of a prosthetic valve, congenital heart disease, and a causative microorganism such as Staphylococcus aureus, were not associated with HF in patients with infective endocarditis.
Heart failure in the setting of valvular dysfunction and left-sided infective endocarditis is a widely accepted indication for valvular surgery and is a class I guide-line recommendation from the American College of Cardiology/American Heart Association and the European Society of Cardiology.4,5 Surgical treatment of infective endocarditis and HF was performed in 62% of patients with active infection in this multicenter study, a rate higher than rates reported in other series,2,18 and early in the course of active infective endocarditis. In addition to the presence of heart failure alone as an indication for surgery, our study has identified a number of other factors that increased the likelihood of surgery for HF in patients with infective endocarditis, including severity of HF, younger age, paravalvular complication, and transfer from another hospital.
These factors suggest that surgery was performed in patients with the most serious complications of infective endocarditis (eg, severe HF, paravalvular complications) who had acceptable operative risk. Patients with less severe HF (NYHA class I or II) may have been treated medically with improvement or resolution of HF symptoms, thus attenuating the indication for surgery. Improved recognition of HF and institutional systems to promote appropriate treatment of infective endocarditis may enhance the rate of surgery for this indication. For instance, N-terminal pro-B-type natriuretic peptide level may be a more sensitive marker of HF presence and severity in patients with infective endocarditis, and recent small studies have found that patients with infective endocarditis and elevated levels of the peptide had poorer event-free survival.24,25 Earlier recognition of heart failure in infective endocarditis may expedite surgical intervention, including transfer to a facility with surgical capability and expertise, before hemodynamic status deteriorates or other complications develop. In addition, management- or protocol-based approaches to treatment of infective endocarditis have been found to reduce 1-year mortality of infective endocarditis and improve compliance with antimicrobial therapy and surgical indications but without increasing the overall surgery rate.26 Our finding that nearly one-third of patients with HF and high surgical propensity did not have surgery emphasizes the need for such multidisciplinary, guideline-based management of infective endocarditis.
The in-hospital mortality rates reported in smaller studies of left-sided infective endocarditis and HF have ranged from 24% to 43%7,21,22,27 and have been associated with uncontrolled infection, major neurologic event, and S aureus infective endocarditis.22 Later onset of HF in the course of infective endocarditis has also been associated with higher mortality.28 In the present study, severity of HF was the strongest predictor of both in-hospital and 1-year mortality, although surgical treatment significantly reduced mortality at early as well as later points after propensity adjustment for this intervention. In a recent, single-center study without adjustment for selection or survival bias, valvular surgery was performed in 46% of patients with left-sided infective endocarditis and HF, which was also associated with lower in-hospital and 1-year mortality but not related to the severity of HF.22 An earlier study used propensity matching to adjust for characteristics of patients treated with surgery and found that the survival benefit of surgery on 6-month outcome in infective endocarditis was limited to those patients with severe(NYHA class III or IV) HF, with no survival benefit in patients with no or mild HF.2
In the current study, the association between surgery and survival for HF in patients with infective endocarditis was apparent across the spectrum of HF severity. Although the relationship with absolute mortality risk reduction was greater for patients with advanced, NYHA class III or IV symptoms, an association with lower mortality was also present for patients with NYHA class I or II symptoms. However, the association between surgical treatment and 1-year survival was greatest in patients with higher propensity for surgery. The in-hospital mortality rate for surgically treated patients was 20%, higher than that reported in other studies (8%–15%),2,18,23 and potentially related to the severity of HF and other adverse prognostic factors. In a recent study of the Society of Thoracic Surgery Adult Cardiac Surgery Database of 19 543 operations performed for infective endocarditis from 2002–2008, operative mortality was 8.2%, but active endocarditis was present in only 52% of cases and was independently associated with a 2-fold higher mortality rate.29
Our study has several limitations. The diagnosis and severity of HF were determined by physicians at the individual centers using symptoms, signs, and/or radiographic findings at the time of study enrollment and are subject to variability and potential bias. Measurement of left ventricular ejection fraction was not collected in this registry, although the majority of patients in this study had left-sided infective endocarditis with acute valvular regurgitation, and the prevalence of HF in our population was consistent with previous studies of infective endocarditis.2,18 Furthermore, physician assessment of heart failure severity by NYHA classification correlated with radiographic evidence of pulmonary edema, a more specific but less sensitive diagnostic criterion. Time of heart failure symptom onset was not collected. Selection bias resulting from the nonrandomized use of surgery has the potential to influence the results of observational data analysis, and clinical reasons for lack of surgical treatment of HF in patients with infective endocarditis, including all variables needed to calculate operative risk by validated cardiac surgery models (eg, Society of Thoracic Surgery or euroSCORE), were not available. Although surgery was performed early in the treatment of infective endocarditis in our cohort, the association between surgical timing and outcome was not evaluated, although a recent study found higher operative mortality in urgent cases or active infective endocarditis.29
Despite the use of propensity score adjustment to reduce selection bias and proportional hazards modeling to reduce survival bias, other variables not evaluated may confound the results of this analysis. A nonmatching propensity score method was used to avoid a significant reduction in study sample size in light of the observed differences in baseline characteristics and predicted probability for surgery between the surgical vs nonsurgical groups. Although a randomized trial of surgical vs medical therapy in infective endocarditis would reduce selection bias as a factor in assessing outcome, it is highly unlikely that patients with HF, particularly acute, severe HF, could be ethically enrolled.
In conclusion, based on this large, prospective, international, multicenter analysis of definite infective endocarditis, HF complicates one-third of cases and typically is of advanced degree. In-hospital and 1-year mortality rates were high and were associated with HF severity, older age, paravalvular complications, diabetes mellitus, and stroke. Valvular surgery is strongly associated with lower in-hospital and 1-year mortality in patients with HF but is performed in only 62% of cases. Additional studies are needed to better risk-stratify patients with infective endocarditis and HF and optimize the use of surgery for this serious condition.
Acknowledgments
Dr Chu reported receiving a grant from the American Heart Association (0675027N). Dr Delahaye reported receiving grants from Novartis and the Fédération française de cardiologie. Dr Utili reported serving on the board of Novartis; receiving grants or grants pending from Wyeth; receiving payment for lectures, including service of speakers bureaus, from Novartis; receiving payment for manuscript preparation from Pfizer; and receiving travel/accommodations/meeting expenses from Pfizer, Wyeth, and Novartis. Dr Wang reported receiving grants or grants pending from Edwards Life-sciences, Abbott Vascular, and Gilead Sciences; receiving payment for lectures, including service on speakers bureaus, from American Physician Inc; receiving payment for development of educational presentations from the American Board of Internal Medicine and the American College of Cardiology Foundation; and serving as a defense reviewer (no expert testimony) for a legal case related to endocarditis.
Funding/Support: This work was supported in part by National Institutes of Health grant 2 T32 GM008600 to Dr Kiefer. Dr Miró was a recipient of an INT10/219 Intensification Research Grant (I3SNS & PRICS programs) from the Instituto de Salud Carlos III, Madrid, Spain, and the Departament de Salut de la Generalitat de Catalunya, Barcelona, Spain. Hospital Clinic of Barcelona (Spain) data were supported in part by Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III, and the Spanish Network for the Research in Infectious Diseases (REIPI RD06/0008), Madrid, Spain. No compensation for participation in the International Collaboration on Endocarditis–Prospective Cohort Study was provided to the investigators for their contributions.
Role of the Sponsor: The funding sources had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript.
International Collaboration on Endocarditis–Prospective Cohort Study (ICE-PCS) Investigators and Sites
Argentina: Hospital Italiano (Liliana Clara, MD, Marisa Sanchez, MD); Instituto Cardiovascular (Francisco Nacinovich, MD, Pablo Fernandez Oses, MD, Ricardo Ronderos, MD, Adriana Sucari, MD, Jorge Thierer, MD); Hospital Universitario de la Fundaciòn Favaloro (José Casabé, MD, PhD, Claudia Cortes, MD); Sanatorio de la Trinidad Mitre (Javier Altclas, MD, Silvia Kogan, MD). Australia: Alfred Hospital (Denis Spelman, MD); Barwon Health (Eugene Athan, MD, Owen Harris, MBBS); Canberra Hospital (Karina Kennedy, MBBS, Ren Tan, MBBS); Flinders Medical Centre (David Gordon, MBBS, PhD, Lito Papanicolas, MBBS); Royal Melbourne Hospital (Damon Eisen, MBBS, MD, Leeanne Grigg, MBBS, Alan Street, MBBS); Hons Southern Health (Tony Korman, MD, Despina Kotsanas, BSc); St George Hospital (Robyn Dever, MD, Phillip Jones, MD, Pam Konecny, MD, Richard Lawrence, MD, David Rees, MD, Suzanne Ryan, MHSc); St Vincent’s (Michael P. Feneley, MD, John Harkness, MD, Phillip Jones, MD, Suzanne Ryan, MHSc); The University of New South Wales (Phillip Jones, MD, Jeffrey Post, MD, Porl Reinbott, Suzanne Ryan, MHSc). Austria: Sutherland (Phillip Jones, MD, Suzanne Ryan, MHSc); Vienna General Hospital (Rainer Gattringer, MD, Franz Wiesbauer, MD). Brazil: Ana Neri Hospital (Adriana Ribas Andrade, Ana Cláudia Passos de Brito, Armenio Costa Guimarães, MD); Heart Institute Incor University of São Paulo Medical School (Max Grinberg, MD, PhD, Alfredo José Mansur, MD, PhD, Rinaldo Focaccia Siciliano, MD, Tania Mara Varejao Strabelli, MD, Marcelo Luiz Campos Vieira, MD); Hospital 9 de Julho (Regina Aparecida de Medeiros Tranchesi, MD, Marcelo Goulart Paiva, MD); Hospital Universitario Clementino Fraga Filho/UFRJ (Claudio Querido Fortes, MD); Instituto Dante Pazzanese de Cardiologia (Auristela de Oliveira Ramos, MD); Instituto Nacional de Cardiologi (Giovanna Ferraiuoli, MD, Wilma Golebiovski, MD, Cristiane Lamas, MD, PhD, Marisa Santos, MD, PhD, Clara Weksler, MD). Canada: University of Manitoba (James A. Karlowsky, MD, Yoav Keynan, MD, Andrew M. Morris, MD, Ethan Rubinstein, MD, LLB). Chile: Universidad Católica de Chile (Sandra Braun Jones, MD, Patricia Garcia, MD (Hospital Clínico Pont); Hospital Clinico Universidad de Chile (M. Cereceda, MD, Alberto Fica, Rodrigo Montagna Mella, MD). Croatia: University Hospital for Infectious Diseases (Bruno Barsic, MD, PhD, Suzana Bukovski, MD, PhD, Vladimir Krajinovic, MD, Ana Pangercic, MD, Igor Rudez, MD, Josip Vincelj, MD, PhD). Czech Republic: Centre for Cardiovascular Surgery and Transplantation (Tomas Freiberger, MD, PhD, Jiri Pol, MD, Barbora Zaloudikova, MSc). Egypt: Cairo University Medical School (Zainab Ashour, MD, Amani El Kholy, MD, Marwa Mishaal, MD, Hussien Rizk, MD). France: CHU Nancy-Brabois (Neijla Aissa, MD, Corentine Alauzet, MD, Francois Alla, MD, PhD, Catherine Campagnac, RN, Thanh Doco-Lecompte, MD, Christine Selton-Suty, MD); Faculté deMédecine de Marseille CHU, Nancy-Brabois (Jean-Paul Casalta, MD, Pierre-Edouard Fournier, MD, Gilbert Habib, MD, Didier Raoult, MD, PhD, Franck Thuny, MD); Hospital Louis Pradel (Francois Delahaye, MD, PhD, Armelle Delahaye, Francois Vandenesch, MD); Pontchaillou University (Erwan Donal, MD, Pierre Yves Donnio, PhD, Christian Michelet, MD, PhD, Matthieu Revest, MD, Pierre Tattevin, MD, PhD, Jé rémie Violette, MD); South Hospital Amiens (Florent Chevalier, MD, Antoine Jeu, MD, Dan Rusinaru, MD, Claire Sorel, MD, Christophe Tribouilloy, MD, PhD); University Medical Center of Besançon (Yvette Bernard, MD, Catherine Chirouze, MD, Bruno Hoen, MD, PhD, Joel Leroy, MD, Patrick Plesiat, MD). Germany: Universitaetskliniken Bergmannsheil Bochum (Christoph Naber, MD, PhD, Carl Neuerburg); University Essen (Bahram Mazaheri, PhD, Christoph Naber, MD, PhD, Carl Neuerburg). Greece: Attikon University General Hospital (Sofia Athanasia, MD, Efthymia Giannitsioti, MD); Evangelismos General Hospital of Athens (Elena Mylona, MD, Olga Paniara, MD, PhD, Konstantinos Papanicolaou, MD, John Pyros, MD, Athanasios Skoutelis, MD, PhD). India: All India Institute of Medical Sciences (Gautam Sharma, MD); Medical College Calicut (Johnson Francis, MD, DM, Lathi Nair, MD, DM, Vinod Thomas, MD, DM, Krishnan Venugopal, MD, DM). Ireland: Mater Hospitals (Margaret Hannan, MB, BCh, BAO, MSc, John Hurley, MB, BCh). Israel: Hadassah-Hebrew University (Dan Gilon, MD, Sarah Israel, MD, Maya Korem, MD, Jacob Strahilevitz, MD); Tel Aviv University School of Medicine (Ethan Rubinstein, MD, LLB, Jacob Strahilevitz, MD). Italy: Università di Napoli (Roberta Casillo, MD, PhD, Susanna Cuccurullo, MSc, Giovanni Dialetto, MD, Emanuele Durante-Mangoni, MD, PhD, Mattucci Irene, MD, Enrico Ragone, MD, PhD, Marie Françoise Tripodi, MD, Riccardo Utili, MD, PhD); Maria Vittoria Hospital (Enrico Cecchi, MD, Francesco De Rosa, MD, Davide Forno, MD, Massimo Imazio, MD, Rita Trinchero, MD); Ospedale di Circolo Varese (Alessandro Tebini, MD, Paolo Grossi, MD, PhD, Mariangela Lattanzio, MD, Antonio Toniolo, MD); Ospedali Riuniti di Bergamo (Antonio Goglio, MD, Annibale Raglio, MD, DTM&H, Veronica Ravasio, MD, Marco Rizzi, MD, Fredy Suter, MD); Spedali Civili–Università di Brescia (Giampiero Carosi, MD, Silvia Magri, MD, Liana Signorini, MD). Lebanon: American University of Beirut Medical Center (Tania Baban, MD, Zeina Kanafani, MD, MS, Souha S. Kanj, MD, Mohamad Yasmine, MD). Malaysia: University of Malaya Medical Center (Imran Abidin, MD); National Heart Institute (Syahidah Syed Tamin, MD). Mexico: Instituto Nacional de Cardiología Ignacio Chávez (Eduardo Rivera Martínez, MD, Gabriel Israel Soto Nieto, MD). The Netherlands: University of Amsterdam (Jan T.M. van der Meer, MD, PhD). New Zealand: University of Otago (Stephen Chambers, MD, MSc); Middle more Hospital (David Holland, MB, ChB, PhD); Diagnostic Medlab (Arthur Morris, MD); Wellington Hospital (Nigel Raymond, MB, ChB); North Shore Hospital (Kerry Read, MB, ChB); University of Otago (David R. Murdoch, MD, MSc, DTM&H). Romania: Victor Babes University of Medicine and Pharmacy (Stefan Dragulescu, MD, PhD, Adina Ionac, MD, PhD, Cristian Mornos, MD). Russia: Learning-Scientific Centre of Medical Centre of Russian Presidential Affairs Government Medical Centre of Russia (O.M. Butkevich, PhD); Russian Medical State University (Natalia Chipigina, PhD, Ozerecky Kirill, MD, Kulichenko Vadim, Tatiana Vinogradova, MD, PhD). Saudi Arabia: King Faisal Specialist Hospital & Research Center (Jameela Edathodu, MBBS, Magid Halim, MBBS). Singapore: National Heart Centre (Luh-Nah Lum, BSN, Ru-San Tan, MBBS). Slovenia: Medical Center Ljublijana (Tatjana Lejko-Zupanc, MD, PhD, Mateja Logar, MD, PhD, Manica Mueller-Premru, MD, PhD). South Africa: University of Cape Town and Groote Schuur Hospital (Patrick Commerford, MD, Anita Commerford, MD, Eduan Deetlefs, MD, Cass Hansa, MD, Mpiko Ntsekhe, MD). Spain: Hospital Clinic–IDIBAPS, University of Barcelona, Barcelona, Spain (Manuel Almela, MD, Yolanda Armero, MD, Manuel Azqueta, MD, Ximena Castañeda, MD, Carlos Cervera, MD, Ana del Rio, MD, PhD, Carlos Falces, MD, Cristina Garcia-de-la-Maria, PhD, Guillermina Fita, MD, Jose M. Gatell, MD, PhD, Francesc Marco, MD, PhD, Carlos A. Mestres, MD, PhD, José M.Miró, MD, PhD, Asuncion Moreno, MD, PhD, Salvador Ninot, MD, Carlos Paré, MD, PhD, Joan Pericas, MD, Jose Ramirez, MD, PhD, Irene Rovira, MD, Marta Sitges, MD); Hospitál de Sabadell (Ignasi Anguera, MD, PhD, Bernat Font, MD, Joan Raimon Guma, MD); Hospital General Universitario Gregorio Marañón (Javier Bermejo, Emilio Bouza, MD, PhD, Miguel Angel Garcia Fernández, MD, Victor Gonzalez-Ramallo, MD, Mercedes Marín, MD, Patricia Muñoz, MD, PhD, Miguel Pedromingo, MD, Jorge Roda, Marta Rodríguez-Créixems, MD, PhD, Jorge Solis, MD); Hospital Universitari Vall d’Hebron (Benito Almirante, MD, Nuria Fernandez-Hidalgo, MD, Pilar Tornos, MD); Hospital Universitario Virgen del Rocío (Arístides de Alarcón, Ricardo Parra). Sweden: Sahlgrenska Universitetssjukhuset/Ӧstra (Eric Alestig, MD, Magnus Johansson, MD, PhD, Lars Olaison, MD, PhD, Ulrika Snygg-Martin, MD). Thailand: Khon Kaen University (Orathai Pachirat, MD, Pimchitra Pachirat, MD, Burabha Pussadhamma, MD, Vichai Senthong, MD). United Kingdom: Queen Elizabeth Hospital (Anna Casey, MBBS, Tom Elliott, PhD, DSc, Peter Lambert, BSc, PhD, DSc, Richard Watkin, MBBS); St Thomas’ Hospital (Christina Eyton, John L. Klein, MD). United States: Ann Arbor VA Medical Center (Suzanne Bradley, MD, Carol Kauffman, MD); Dallas VA Medical Center (Roger Bedimo, MD, MS); Duke University Medical Center (Vivian H. Chu, MD, MHS, G. Ralph Corey, MD, Anna Lisa Crowley, MD, MHS, Pamela Douglas, MD, Laura Drew, RN, BSN, Vance G. Fowler, MD, MHS, Thomas Holland, MD, Tahaniyat Lalani, MBBS, MHS, Daniel Mudrick, MD, Zainab Samad, MD, MHS, Daniel Sexton, MD, Martin Stryjewski, MD, MHS, Andrew Wang, MD, Christopher W. Woods, MD, MPH); Emory University (Stamatios Lerakis, MD); Medical University of South Carolina (Robert Cantey, MD, Lisa Steed, PhD, Dannah Wray, MD, MHS); New York University Medical Center (Stuart A. Dickerman, MD); Summa Health System (Hector Bonilla, MD, Joseph DiPersio, MD, PhD, Sara-Jane Salstrom, RN); University of Alabama at Birmingham (John Baddley, MD, Mukesh Patel, MD); University of Texas–Southwestern Medical Center (Gail Peterson, MD, Amy Stancoven, MD); Wayne State University (Luis Afonso, MD, Theresa Kulman, RN, Donald Levine, MD, Michael Rybak, PharmD, MPH); Quintiles (Christopher H. Cabell, MD, MHS). ICE Coordinating Center: Khaula Baloch, MPH, Vivian H. Chu, MD, MHS, G. Ralph Corey, MD, Christy C. Dixon, Vance G. Fowler Jr, MD, MHS, Tina Harding, RN, BSN, Marian Jones-Richmond, Paul Pappas, MS, Lawrence P. Park, PhD, Thomas Redick, MPH, Judy Stafford, MS. ICE Publications Committee: Kevin Anstrom, PhD, Eugene Athan, MD, Arnold S. Bayer, MD, Christopher H. Cabell, MD, MHS, Vivian H. Chu, MD, MHS, G. Ralph Corey, MD, Vance G. Fowler Jr, MD, MHS, Bruno Hoen, MD, PhD, A. W. Karchmer, MD, José M. Miró, MD, PhD, David R. Murdoch, MD, MSc, DTM&H, Daniel J. Sexton, MD, Andrew Wang, MD. ICE Steering Committee: Arnold S. Bayer, MD, Christopher H. Cabell, MD, MHS, Vivian Chu, MD, MHS, G. Ralph Corey, MD, David T. Durack, MD, DPhil, Susannah Eykyn, MD, Vance G. Fowler Jr, MD, MHS, Bruno Hoen, MD, PhD, José M. Miró, MD, PhD, Phillipe Moreillon, MD, PhD, Lars Olaison, MD, PhD, Didier Raoult, MD, PhD, Ethan Rubinstein, MD, LLB, Daniel J. Sexton, MD.
Footnotes
Author Contributions: Dr Park had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Tribouilloy, Miró, Murdoch, Moreillon, Utili, Wang.
Acquisition of data: Tribouilloy, Cortes, Casillo, Delahaye, Durante-Mangoni, Edathodu, Falces, Logar, Miró, Naber, Tripodi, Murdoch.
Analysis and interpretation of data: Kiefer, Park, Chu, Durante-Mangoni, Falces, Miró, Murdoch, Wang.
Drafting of the manuscript: Kiefer, Park, Durante-Mangoni, Falces, Wang.
Critical revision of the manuscript for important intellectual content: Kiefer, Park, Tribouilloy, Cortes, Casillo, Chu, Delahaye, Durante-Mangoni, Edathodu, Falces, Logar, Miró, Naber, Tripodi, Murdoch, Moreillon, Utili, Wang.
Statistical analysis: Kiefer, Park, Miró.
Obtained funding: Chu.
Administrative, technical, or material support: Tribouilloy, Chu, Murdoch.
Study supervision: Tribouilloy, Falces, Miró, Tripodi, Utili.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Online-Only Material: The eFigure and the Author Video Interview are available at http://www.jama.com.
REFERENCES
- 1.Bashore TM, Cabell C, Fowler V., Jr Update on infective endocarditis. Curr Probl Cardiol. 2006;31(4):274–352. doi: 10.1016/j.cpcardiol.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Vikram HR, Buenconsejo J, Hasbun R, Quagliarello VJ. Impact of valve surgery on 6-month mortality in adults with complicated, left-sided native valve endocarditis: a propensity analysis. JAMA. 2003;290(24):3207–3214. doi: 10.1001/jama.290.24.3207. [DOI] [PubMed] [Google Scholar]
- 3.Thuny F, Habib G. When should we operate on patients with acute infective endocarditis? Heart. 2010;96(11):892–897. doi: 10.1136/hrt.2008.151936. [DOI] [PubMed] [Google Scholar]
- 4.Bonow RO, Carabello BA, Chatterjee K, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52(13):e1–e142. doi: 10.1016/j.jacc.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 5.Habib G, Hoen B, Tornos P, et al. ESC Committee for Practice Guidelines; Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC) Eur Heart J. 2009;30(19):2369–2413. doi: 10.1093/eurheartj/ehp285. [DOI] [PubMed] [Google Scholar]
- 6.Habib G, Tribouilloy C, Thuny F, et al. Prosthetic valve endocarditis: who needs surgery? a multicentre study of 104 cases. Heart. 2005;91(7):954–959. doi: 10.1136/hrt.2004.046177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delahaye F, Alla F, Béguinot I, et al. AEPEI Group. In-hospital mortality of infective endocarditis: prognostic factors and evolution over an 8-year period. Scand J Infect Dis. 2007;39(10):849–857. doi: 10.1080/00365540701393088. [DOI] [PubMed] [Google Scholar]
- 8.Lalani T, Cabell CH, Benjamin DK, et al. International Collaboration on Endocarditis–Prospective Cohort Study (ICE-PCS) Investigators. Analysis of the impact of early surgery on in-hospital mortality of native valve endocarditis: use of propensity score and instrumental variable methods to adjust for treatment-selection bias. Circulation. 2010;121(8):1005–1013. doi: 10.1161/CIRCULATIONAHA.109.864488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aksoy O, Sexton DJ, Wang A, et al. Early surgery in patients with infective endocarditis: a propensity score analysis. Clin Infect Dis. 2007;44(3):364–372. doi: 10.1086/510583. [DOI] [PubMed] [Google Scholar]
- 10.Cabell CH, Abrutyn E. Progress toward a global understanding of infective endocarditis: early lessons from the International Collaboration on Endocarditis investigation. Infect Dis Clin North Am. 2002;16(2):255–272. vii. doi: 10.1016/s0891-5520(01)00007-1. [DOI] [PubMed] [Google Scholar]
- 11.Cabell CH, Abrutyn E. Progress toward a global understanding of infective endocarditis: lessons from the International Collaboration on Endocarditis. Cardiol Clin. 2003;21(2):147–158. doi: 10.1016/s0733-8651(03)00033-x. [DOI] [PubMed] [Google Scholar]
- 12.Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30(4):633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 13.Cabell CH, Jollis JG, Peterson GE, et al. Changing patient characteristics and the effect on mortality in endocarditis. Arch Intern Med. 2002;162(1):90–94. doi: 10.1001/archinte.162.1.90. [DOI] [PubMed] [Google Scholar]
- 14.Fowler VG, Jr, Miró JM, Hoen B, et al. ICE Investigators. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA. 2005;293(24):3012–3021. doi: 10.1001/jama.293.24.3012. [DOI] [PubMed] [Google Scholar]
- 15.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285(26):1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 16.Anguera I, Miró JM, Cabell CH, et al. ICE-MD investigators. Clinical characteristics and outcome of aortic endocarditis with periannular abscess in the International Collaboration on Endocarditis Merged Database. Am J Cardiol. 2005;96(7):976–981. doi: 10.1016/j.amjcard.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 17.Anguera I, Miró JM, Vilacosta I, et al. Aortocavitary Fistula in Endocarditis Working Group. Aortocavitary fistulous tract formation in infective endocarditis: clinical and echocardiographic features of 76 cases and risk factors for mortality. Eur Heart J. 2005;26(3):288–297. doi: 10.1093/eurheartj/ehi034. [DOI] [PubMed] [Google Scholar]
- 18.Chu VH, Woods CW, Miró JM, et al. International Collaboration on Endocarditis–Prospective Cohort Study Group. Emergence of coagulase-negative staphylococci as a cause of native valve endocarditis. Clin Infect Dis. 2008;46(2):232–242. doi: 10.1086/524666. [DOI] [PubMed] [Google Scholar]
- 19.Benito N, Miró JM, de Lazzari E, et al. ICE-PCS (International Collaboration on Endocarditis Prospective Cohort Study) Investigators. Health care–associated native valve endocarditis: importance of non-nosocomial acquisition. Ann Intern Med. 2009;150(9):586–594. doi: 10.7326/0003-4819-150-9-200905050-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Austin PC. The performance of different propensity-score methods for estimating differences in proportions (risk differences or absolute risk reductions) in observational studies. Stat Med. 2010;29(20):2137–2148. doi: 10.1002/sim.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chu VH, Cabell CH, Benjamin DK, Jr, et al. Early predictors of in-hospital death in infective endocarditis. Circulation. 2004;109(14):1745–1749. doi: 10.1161/01.CIR.0000124719.61827.7F. [DOI] [PubMed] [Google Scholar]
- 22.Nadji G, Rusinaru D, Rémadi JP, Jeu A, Sorel C, Tribouilloy C. Heart failure in left-sided native valve infective endocarditis: characteristics, prognosis, and results of surgical treatment. Eur J Heart Fail. 2009;11(7):668–675. doi: 10.1093/eurjhf/hfp077. [DOI] [PubMed] [Google Scholar]
- 23.Hasbun R, Vikram HR, Barakat LA, Buenconsejo J, Quagliarello VJ. Complicated left-sided native valve endocarditis in adults: risk classification for mortality. JAMA. 2003;289(15):1933–1940. doi: 10.1001/jama.289.15.1933. [DOI] [PubMed] [Google Scholar]
- 24.Kahveci G, Bayrak F, Mutlu B, et al. Prognostic value of N-terminal pro-B-type natriuretic peptide in patients with active infective endocarditis. AmJ Cardiol. 2007;99(10):1429–1433. doi: 10.1016/j.amjcard.2006.12.071. [DOI] [PubMed] [Google Scholar]
- 25.Shiue AB, Stancoven AB, Purcell JB, et al. Relation of level of B-type natriuretic peptide with outcomes in patients with infective endocarditis. Am J Cardiol. 2010;106(7):1011–1015. doi: 10.1016/j.amjcard.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 26.Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290–1298. doi: 10.1001/archinternmed.2009.192. [DOI] [PubMed] [Google Scholar]
- 27.Gálvez-Acebal J, Rodríguez-Baño J, Martínez-Marcos FJ, et al. Grupo para el Estudio de las Infecciones Cardiovasculares de la Sociedad Andaluza de Enfermedades Infecciosas (SAEI) Prognostic factors in left-sided endocarditis: results from the Andalusian multicenter cohort. BMC Infect Dis. 2010;10:17. doi: 10.1186/1471-2334-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Røder BL, Wandall DA, Frimodt-Møller N, Espersen F, Skinhøj P, Rosdahl VT. Clinical features of Staphylococcus aureus endocarditis: a 10-year experience in Denmark. Arch Intern Med. 1999;159(5):462–469. doi: 10.1001/archinte.159.5.462. [DOI] [PubMed] [Google Scholar]
- 29.Gaca JG, Sheng S, Daneshmand MA, et al. Outcomes for endocarditis surgery in North America: a simplified risk scoring system. J Thorac Cardiovasc Surg. 2011;141(1):98–106. e1–e2. doi: 10.1016/j.jtcvs.2010.09.016. [DOI] [PubMed] [Google Scholar]