Abstract
Objective
To identify the determinants and measure the trends in health facility-based deliveries and caesarean sections among married adolescent girls in Bangladesh.
Methods
In order to measure the trends in health facility-based deliveries and caesarean sections, Bangladesh Demographic Health Survey (BDHS) data sets were analysed (BDHS; 1993–1994, 1996–1997, 1999–2000, 2004, 2007, 2011). The BDHS 2011 data sets were analysed to identify the determinants of health facility-based deliveries and caesarean sections. A total of 2813 adolescent girls (aged 10–19 years) were included for analysis. Bivariate and multivariate analyses were performed.
Results
Health facility-based deliveries have continuously increased among adolescents in Bangladesh over the past two decades from 3% in 1993–1994 to 24.5% in 2011. Rates of population-based and facility-based caesarean sections have increased linearly among all age groups of women including adolescents. Although the country's overall (population-based) caesarean section rate among adolescents was within acceptable range (11.6%), a rate of nearly 50% health facility level caesarean sections among adolescent girls is alarming. Among adolescent girls, use of antenatal care (ANC) appeared to be the most important predictor of health facility-based delivery (OR: 4.04; 95% CI 2.73 to 5.99), whereas the wealth index appeared as the most important predictor of caesarean sections (OR: 5.7; 95% CI 2.74 to 12.1).
Conclusions
Maternal health-related interventions should be more targeted towards adolescent girls in order to encourage them to access ANC and promote health facility-based delivery. Rising trends of caesarean sections require further investigation on indication and provider–client-related determinants of these interventions among adolescent girls in Bangladesh.
Keywords: Health facility-based delivery, Caesarean section, Adolescent girl, Bangladesh
Strengths and limitations of this study.
The main strength of this study is the use of nationally representative data sets of Bangladesh.
This study did not explain any programmatic factors (eg, quality of health services or cost of health facility delivery) which might affect delivery in a health facility as Bangladesh Demographic Health Survey (BDHS) did not capture indicators related to these factors.
This study did not capture information about the medical indications of caesarean sections because of the lack of relevant data in BDHS.
Background
Complications in pregnancy and childbirth are the leading causes of death among adolescents (aged 10–19 years) and young women in low-income countries (LICs).1 It is estimated that annually around 70 000 adolescent girls die from complications related to pregnancy and childbirth in LICs.2
Child marriage has a long tradition in Bangladesh and contributes to the incidence of adolescent pregnancies. Though the legal age of marriage for women is 18 years in Bangladesh, around 66% of the girls get married before that age and about 33% of them become pregnant by the age of 19.3 There is no official record of pregnancies among unmarried adolescents in Bangladesh.4
Several studies have shown that adolescents are less likely to seek skilled maternal health services such as attending antenatal care (ANC) and postnatal care (PNC) as well as delivering in facilities when compared to adults (women older than 19 years), despite their higher need of those services.5 6 In order to decrease maternal mortality ratios and to improve pregnancy outcomes, it is essential to increase the proportion of deliveries in health facilities. It is estimated that only about 29% of deliveries in Bangladesh take place in a health facility.7
Caesarean section is considered to be a life-saving procedure to overcome complications during labour. However, there is evidence that caesarean sections without medical indication are associated with increased maternal and newborn mortality and morbidity.8–13 In addition, the risk of maternal and newborn complications is higher following a caesarean section, which includes stillbirths, anomalies of the placenta and neonatal survival, particularly among adolescents.14 15 The tendency of repeated caesarean sections in subsequent births is higher among those adolescents who delivered their first child by caesarean section.16
In the last decade, population-based rates of caesarean deliveries have increased beyond the WHO recommended level of 15% in Bangladesh where the rate increased from 9% in 2007 to 17% in 2011.7 17–19 This study aims to assess the trends and identify the determinants of health facility-based deliveries and caesarean sections among married adolescent girls in Bangladesh.
Methods
Background information of the country
Bangladesh, located in the northeastern part of South Asia, is one of the most densely populated countries in the world. According to the 2011 Population and Housing Census (PHC), the population of the country reached close to 150 million. Almost 90% of them are Muslims and 9% are Hindus, with other religions constituting the remaining 1%. The country ranks 146th on the Human Development Index (HDI) among all nations. Twenty-seven per cent of the total population of Bangladesh live in urban areas. Despite prevailing problems such as poverty, political instability and income inequalities, Bangladesh's progress towards achieving the Millennium Development Goals (MDGs) is remarkable.20 The country's maternal mortality ratio has declined from 322 deaths in 2001 to 176 deaths in 2010 per 100 000 live births.21 Use of contraception among married women has increased from 8% in 1975 to 61% in 2011. About 26% of pregnant women report at least four ANC visits from a qualified provider.7
Data sources
This study used data sets from the Bangladesh Demographic and Health Surveys (BDHS). With the permission of MEASURE DHS, we downloaded publicly available BDHS data sets of 1993–1994, 1996–1997, 1999–2000, 2004, 2007 and 2011 from the website of MEASURE (http://www.measuredhs.com).
BDHS is a household survey of ever-married women aged 12–49 years and ever-married men aged 15–54 years. BDHS uses a multistage cluster-sampling method to obtain detailed information, including marriage, family planning, fertility preferences, infant and child mortality, maternal and newborn health, nutrition, HIV/AIDS-related knowledge, women's empowerment and health outcomes.
In order to identify the determinants of health facility-based deliveries and caesarean sections, we used data sets of the BDHS 2011 which surveyed 17 842 ever-married women aged 12–49 years and 3997 ever-married men over the age of 15 years from 17 141 households covering 600 clusters (207 in urban and 393 in rural areas) throughout Bangladesh. The survey recorded information from 8789 deliveries with a live birth as pregnancy outcome that occurred in the last 5 years preceding the 2011 survey, of which 2813 (32%) live births were reported among adolescent girls (age <20).
To examine the trends in facility-based deliveries and caesarean sections (population-based and facility-based) among married adolescent girls, we used data sets of BDHS 1993–1994, BDHS 1996–1997, BDHS 1999–2000, BDHS 2004, BDHS 2007 and BDHS 2011. In order to be consistent, we included all the deliveries (the most recent one when an adolescent girl had more than one delivery) that occurred during 5 years preceding each Demographic and Health Survey (DHS) except for the BDHS 1993–1994 that covered information of only 3 years preceding the survey.
Variables
Dependent variables
The dependent variables in this study are ‘health facility-based delivery’ and ‘caesarean section’. Health facility-based delivery refers to childbirths which took place in government hospitals, government medical colleges, district hospitals, maternal and child welfare centres, Upazila health complex (subdistrict level public health facility), health and family welfare centres, private hospitals/clinics, private medical colleges or non-governmental organization clinics. Population-based and facility-based caesarean sections were described using bivariate analysis.
Independent variables
The independent variables were maternal age (age of an adolescent girl at the time of childbirth) in years, place of residence, region, maternal education, wealth index (calculated based on the ownership of several household assets and categorised into five quintiles from the poorest to richest), husband's education, birth order (parity reported by the adolescent girls at the time of the survey) and ANC coverage (reported attendance to ANC). On the basis of the existing literature, the variable ‘decision-making power’ was categorised using the criteria whether an adolescent girl participated in decision-making related to (1) her own healthcare, (2) making major household purchases and (3) visits to her family and relatives.22 23 The category ‘no decision’ meant that none of the three decisions were taken by the woman, ‘1–2 decisions’ indicated that a woman participated in making at least one or two decisions in the three mentioned areas and ‘all three decisions’ reflected that a woman participated in decision-making in all the three areas.
Statistical analysis
Corresponding weighting factors were considered to weigh the clustered data for each of the respondents in the survey. Bivariate analysis (Pearson's χ2) was performed to assess the relationship between the dependent and independent variables. A binary logistic regression analysis was carried out to determine the adjusted effect of each factor on the dependent variables (‘facility-based delivery’ and ‘caesarean section’). Multicollinearity was checked before logistic regression. The results of the logistic regression analysis were presented by ORs with 95% CIs . All statistical analysis was performed using STATA 12.1 for windows.
Results
Characteristics of the study participants and patterns of health facility-based deliveries and caesarean sections
According to the BDHS 2011, in total 2813 childbirths were reported by married adolescent girls during the last 5 years preceding the survey. Of these, 1402 (49.9%) births occurred among girls aged <18 years and the remaining 1411 (50.1%) among girls aged between 18 and 19 years. Overall 24.5% (686/2813) of the childbirths reported by adolescent mothers occurred in health facilities. It was observed that 40% of the urban adolescents compared to only 20% of rural adolescents delivered in healthcare facilities (p<0.001) (table 1). Of all deliveries among adolescents that took place in health facilities, 47.4% (325/686) ended up with a caesarean section.
Table 1.
Baseline characteristics of adolescent girls who reported a childbirth and use of health facility-based deliveries and caesarean sections (BDHS 2011)
| % Health facility-based deliveries among all births |
% Population-based caesarean sections (caesarean sections among all births) |
% Facility-based caesarean sections (caesarean sections among all facility births) |
||||
|---|---|---|---|---|---|---|
| Yes | p Value | Yes | p Value | Yes | p Value | |
| Maternal age (years) | (n=2813) | 0.482 | (n=2812) | 0.059 | (n=686) | 0.050 |
| <18 | 23.8 | 10.7 | 45 | |||
| 18–19 | 25.1 | 13.4 | 53.5 | |||
| Residence | (n=2813) | <0.001 | (n=2769) | <0.001 | (n=686) | 0.0629 |
| Urban | 40 | 19.1 | 47.9 | |||
| Rural | 20.2 | 10.1 | 50.2 | |||
| Region | (n=2813) | <0.001 | (n=2812) | <0.05 | (n=686) | <0.01 |
| Barisal | 17.4 | 9.6 | 54.8 | |||
| Chittagong | 17.8 | 10 | 56 | |||
| Dhaka | 24.5 | 13.5 | 55.2 | |||
| Khulna | 39.5 | 15.6 | 39.4 | |||
| Rajshahi | 29.1 | 15.9 | 55.3 | |||
| Rangpur | 25.1 | 7.7 | 30.5 | |||
| Sylhet | 16.1 | 9.2 | 57.3 | |||
| Maternal education | (n=2813) | <0.001 | (n=2812) | <0.001 | (n=686) | 0.361 |
| No education | 9.3 | 3.7 | 39.6 | |||
| Primary | 17 | 8 | 46.9 | |||
| Secondary | 30 | 14.8 | 49.5 | |||
| Higher than secondary | 53.6 | 32.7 | 61 | |||
| Husband's education | (n=2811) | <0.001 | (n=2810) | <0.001 | (n=686) | 0.016 |
| No education | 13.1 | 5.2 | 39.5 | |||
| Primary | 19.9 | 9.3 | 46.7 | |||
| Secondary | 31.9 | 15.6 | 49 | |||
| Higher than secondary | 43.6 | 28 | 64 | |||
| Wealth index | (n=2813) | <0.001 | (n=2812) | <0.001 | (n=686) | <0.01 |
| Poorest | 11.5 | 3.2 | 27.6 | |||
| Poorer | 16.4 | 7.4 | 45.1 | |||
| Middle | 22.1 | 10.9 | 49.2 | |||
| Richer | 34.5 | 17.6 | 51.2 | |||
| Richest | 46.9 | 27.2 | 58.3 | |||
| Decision-making power | (n=2769) | 0.561 | (n=2767) | 0.904 | (n=676) | 0.550 |
| No decision | 23.8 | 11.6 | 48.9 | |||
| 1–2 decisions | 23.5 | 12.4 | 52.7 | |||
| All 3 decisions | 25.9 | 12.2 | 47 | |||
| Birth order | (n=2813) | <0.001 | (n=2812) | <0.001 | (n=686) | 0.312 |
| First | 27.9 | 14.1 | 50.5 | |||
| Second | 12.9 | 5.7 | 43.8 | |||
| Higher than two | 12.7 | 3 | 23.4 | |||
| ANC coverage | (n=2189) | <0.001 | (n=2188) | <0.001 | (n=576) | 0.805 |
| No ANC attendance | 10.8 | 5.8 | 53.4 | |||
| <4 ANC visits | 25.9 | 12.7 | 49.3 | |||
| At least 4 ANC visits | 46.4 | 24.1 | 52 | |||
| Total | 24.5 | 11.6 | 47.4 | |||
An adolescent girl was categorised as participating in decision-making if she reported that she usually makes decisions, either alone or jointly with her husband, in the following three areas: woman's own healthcare, making major household purchases and visits to her family and relatives.
ANC, antenatal care; BDHS, Bangladesh Demographic Health Survey.
The tendency to give birth in a facility was higher among adolescents aged 18–19 years compared to those younger than 18 years (p>0.05). Among all the seven regions (divisions) of Bangladesh, the lowest rate of facility-based deliveries was observed among adolescents in Sylhet division (16.1%) whereas Khulna division had the highest rate (39.5%). In terms of wealth, use of healthcare facilities for childbirth was higher among the richest adolescent girls compared to those belonging to the middle and poorer wealth bands. Rates of caesarean sections were also higher among richer adolescents compared to those belonging to the poorest or poorer wealth bands.
Birth order was significantly associated with the utilisation of health facilities for deliveries among adolescent girls (p<0.001). However, it was not significantly associated with caesarean sections at facility level (p>0.05). Adolescent girls who had attended at least four ANC consultations were more likely to use a health facility for the delivery of their child than those who had not received any ANC or had less than four ANC visits (46.4%, 10.8% and 25.9%). Decision-making autonomy of adolescent girls appeared to have no association with health facility-based delivery or caesarean section.
Determinants of health facility deliveries and caesarean sections
Urban residence, being part of the richest wealth band, being pregnant for the first time and attending four or more ANC consultations were associated with a greater likelihood of delivering in a health facility after adjusting for all other covariates in the multivariate model (table 2). Besides, adolescent girls in Khulna division and Rajshahi division were 2.6 times and 2.1 times, respectively, more likely to deliver their child in a facility compared to their counterparts in Barisal division.
Table 2.
Factor associated with health facility-based deliveries and caesarean section among adolescent girls; adjusted multivariate model
| Facility-based delivery |
Caesarean section |
|||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Maternal age (years) | 0.597 | 0.086 | ||
| <18 | 1 | 1 | ||
| 18–19 | 1.071 (0.829 to 1.385) | 1.323 (0.961 to 1.820) | ||
| Place of residence | <0.01 | 0.880 | ||
| Urban | 1 | 1 | ||
| Rural | 0.666 (0.503 to 0.881) | 1.027 (0.723 to 1.457) | ||
| Region | <0.001 | <0.05 | ||
| Barisal | 1 | 1 | ||
| Chittagong | 1.070 (0.663 to 1.728) | 0.978 (0.553 to 1.728) | ||
| Dhaka | 1.224 (0.770 to 1.945) | 1.103 (0.650 to 1.870) | ||
| Khulna | 2.615 (1.570 to 4.356) | 1.399 (0.819 to 2.388) | ||
| Rajshahi | 2.104 (1.302 to 3.398) | 1.876 (1.115 to 3.156) | ||
| Rangpur | 1.591 (0.958 to 2.643) | 0.767 (0.398 to 1.478) | ||
| Sylhet | 1.417 (0.777 to 2.585) | 1.146 (0.583 to 2.252) | ||
| Maternal education | 0.168 | 0.690 | ||
| No education | 1 | 1 | ||
| Primary | 1.220 (0.684 to 2.174) | 1.222 (0.560 to 2.666) | ||
| Secondary | 1.463 (0.822 to 2.604) | 1.334 (0.631 to 2.819) | ||
| Higher than secondary | 2.230 (1.041 to 4.778) | 1.730 (0.679 to 4.408) | ||
| Husband's education | 0.174 | 0.282 | ||
| No education | 1 | 1 | ||
| Primary | 0.834 (0.567 to 1.226) | 1.013 (0.570 to 1.800) | ||
| Secondary | 1.197 (0.813 to 1.763) | 1.259 (0.723 to 2.193) | ||
| Higher than secondary | 1.103 (0.642 to 1.896) | 1.633 (0.837 to 3.184) | ||
| Wealth index | <0.001 | <0.001 | ||
| Poorest | 1 | 1 | ||
| Poorer | 1.271 (0.851 to 1.899) | 2.560 (1.340 to 4.890) | ||
| Middle | 1.468 (0.964 to 2.236) | 3.103 (1.609 to 5.983) | ||
| Richer | 2.255 (1.462 to 3.477) | 3.711 (1.850 to 7.442) | ||
| Richest | 2.643 (1.583 to 4.414) | 5.763 (2.743 to 12.106) | ||
| Decisions making power | 0.780 | 0.612 | ||
| No power | 1 | 1 | ||
| 1–2 decisions power | 0.945 (0.691 to 1.292) | 1.208 (0.827 to 1.766) | ||
| All 3 decisions power | 1.046 (0.782 to 1.399) | 1.121 (0.777 to 1.617) | ||
| Birth order | <0.01 | 0.053 | ||
| First | 1 | 1 | ||
| Second | 0.547 (0.380 to 0.788) | 0.531 (0.318 to 0.886) | ||
| Higher than two | 0.948 (0.365 to 2.462) | 0.381 (0.048 to 2.972) | ||
| ANC coverage | <0.0001 | <0.001 | ||
| No ANC attendance | 1 | 1 | ||
| <4 ANC visits | 2.141 (1.483 to 3.093) | 1.638 (0.979 to 2.741) | ||
| At least 4 ANC visits | 4.040 (2.725 to 5.991) | 2.743 (1.605 to 4.685) | ||
ANC, antenatal care.
The odds of delivering in a health facility decreased by 33% among adolescent girls residing in rural areas compared to those residing in urban areas (OR: 0.67; 95% CI 0.50 to 0.88). Adolescent girls of the richest wealth quintile were 2.6 times more likely to deliver in a health facility compared to adolescents belonging to the poorest wealth quintile after adjusting for all other variables (OR: 2.64; 95% CI 1.58 to 4.41). Use of ANC services appeared as the most important determinant for health facility-based delivery and showed that adolescent girls with four or more ANC visits were four times more likely to deliver in a health facility than those having no ANC visit (OR: 4.04; 95% CI 2.73 to 5.99).
In the bivariate analysis, maternal education appeared to be associated with facility-based delivery while in the logistic model, no statistically significant association was found. However, a significant difference was observed between adolescent girls with no formal education and girls with higher than secondary level education. Adolescent girls having higher than secondary education were 2.2 times more likely to deliver in a health facility compared to those adolescents with no education (OR: 2.2; 95% CI 1.04 to 4.78).
The wealth index appeared as the most important determinant of delivering by caesarean section among adolescent girls. Adolescent girls belonging to the richest wealth quintile were almost six times more likely to deliver their child by caesarean section compared to adolescents belonging to the poorest wealth index (OR: 5.7; 95% CI 2.74 to 12.1). Adolescent girls who had received four or more ANC consultations were 2.7 times more likely to give birth by caesarean section compared to adolescents who had not received any ANC. Probability of childbirth by caesarean section was higher (about 47%) among adolescents who were pregnant for the first time than those pregnant for the second time.
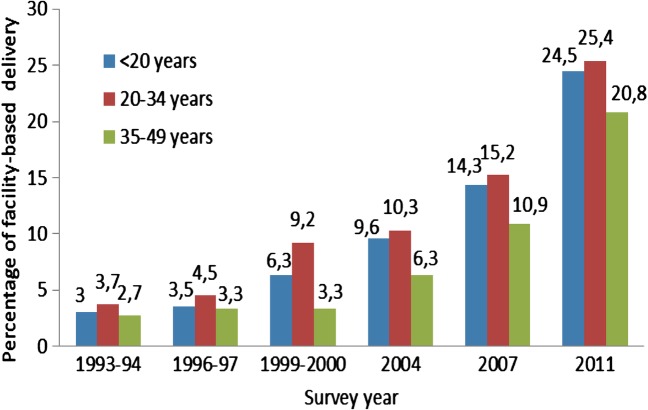
Trends in health facility-based deliveries
There has been a substantial increase in the use of health facilities for delivery among women in all age groups including adolescents (figure 1). Use of health facilities for childbirth has increased among adolescent girls more than eightfold from 3% in 1993–1994 to 24.5% in 2011. The most rapid increase among adolescent girls was observed between 2007 (14.3%) and 2011 (24.5%). Health facility-based delivery has increased more than 10% over this time period.
Figure 1.
Trends in health facility-based deliveries among women of different age groups by survey year, Bangladesh Demographic Health Survey 1993–2011.
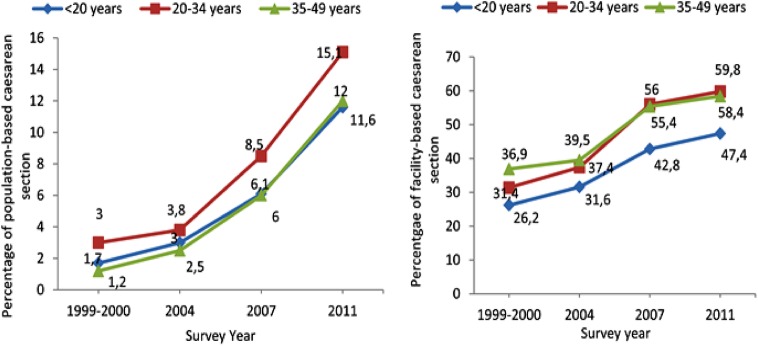
Trends in caesarean sections (population-based and health facility-based)
Figure 2 shows that population and facility level rates of caesarean sections have continuously increased in all age groups. Among adolescent girls, the rates of population-based caesarean sections have almost doubled since 2007 (from 6.1% to 11.6%), whereas rates of facility-based caesarean sections have increased from 26.2% in 1999–2000 to 47.4% in 2011, indicating a 20% increase in 10 years. Facility level rates of caesarean sections increased even more (about 28%) among women aged between 20 and 34 years and around 23% among women aged 35–49 years during the same period.
Figure 2.
Trends in population and facility-based caesarean section among women of different age groups by survey year, Bangladesh Demographic Health Survey 1999–2011.
Discussion
Over the past two decades, delivery rates in health facilities have increased among pregnant women of all ages in Bangladesh. Recently (from 2007 to 2011), the rate of facility-based deliveries among adolescent girls has increased by 10% (14.3% in 2007 to 24.5% in 2011).
This increased use of health facilities by adolescents could be associated with improvement in health service delivery, transition towards a pluralistic health system, deployment of more community health workers, economic transition in Bangladesh, decrease in total fertility rate and increasing levels of awareness among women and their family members about the importance of delivering with a skilled birth attendant.24–26 In addition, another reason for higher facility-based delivery rates particularly among adolescent girls could be explained by an increased rate of referrals of pregnant adolescent girls by community health workers to health facilities.25 This might be due to the fact that adolescent girls are at higher risk of pregnancy-related and delivery-related complications compared to adults.27 28
Despite the increasing trends in health facility-based delivery over the years, the rate is still low at only 24.5% for all deliveries while almost three-quarter of the adolescent girls give birth at home. Therefore, it is important to improve access to and availability of a skilled birth attendant at every delivery.
The findings of this study revealed existing inequalities in the use of maternal health services among adolescent girls in Bangladesh. Consistent with the findings of other studies, we found that adolescent girls residing in urban areas and those belonging to a higher wealth index are more likely to give birth in a health facility compared to those living in rural areas and belonging to a poorer wealth index.6 29 30 The reason for increased numbers of facility-based deliveries among urban adolescents may be better availability and accessibility of health services in urban areas compared to rural areas.29 Use of a health facility is often associated with higher costs which may restrict poor adolescent girls from delivering there.29
Several studies conducted in Bangladesh and in other LICs showed that women's education is an important determinant of facility-based delivery,31–34 whereas this study showed only a significant difference between girls with no formal education and those with a higher than secondary level of education regarding the use of health facilities for childbirth. No significant differences were observed in the use of health facilities among adolescents with a primary or secondary education. Lack of higher education may be related to less decision-making power of adolescent girls which may restrict them to use health services.2 35 36
In line with earlier findings, this study showed that adolescent girls who attended at least four or more ANC consultations are more likely to deliver at a facility than those girls who had not received any or had less than four ANC visits.30 37 Repeat counselling during ANC visits may raise awareness among adolescent girls of the importance of seeking care during delivery or may provide information of maternal health services available in their nearest health facilities.26
Rates of population-based and facility-based caesarean sections have increased over the past two decades in Bangladesh among women of all ages. Although the rates of population-based caesarean sections among adolescents are still within the WHO recommended levels, there is a disproportionately higher increase in health facility-based caesarean sections in Bangladesh that cannot be explained only by a self-selection of adolescents with complication. Previous studies conducted in Bangladesh have shown that factors such as provider-driven and patient-driven decisions in favour of a caesarean section that are not necessarily based on a medical indication as well as increased financial benefit for performing caesarean sections could be an explanation for increasing rates.38 Many factors may support the decision to perform a caesarean section, including the rapidity and the possibility of planning the intervention, a perceived lower health risk, financial benefits for the practitioner and the institution, the fear of litigation or women's demand resulting in, protocols and evidence-based guidelines regarding indications not being followed by the health providers.39–41
With regard to the caesarean section rate among all facility deliveries, there is no clear-cut standard but institutional caesarean section rates that are above 20% might be considered as high.42 This study found that about 57% of all births at the health facility were conducted by caesarean section. Chances to be delivered by caesarean section significantly differ according to factors such as region of residence, wealth index, birth order and use of ANC services, which are consistent with the results of previous studies.43–45
This study showed that adolescent girls are slightly less likely to get a caesarean section compared to adults, which is in line with the results of a recent study in Bangladesh.46 Although the rates of caesarean sections among adolescent girls are lower compared to adults, almost one of two facility-based deliveries ended in a caesarean section among this particular group. Therefore, it would be relevant to identify indications for caesarean sections in adolescent girls and to assess to what extent these interventions were medically justifiable in private and public health facilities.
The main strength of this study was the use of nationally representative data sets. A limitation was that the BDHS did not cover information about accessibility (ie, distance to a health facility) and the quality of healthcare provision which might have influenced the use of health facility delivery among adolescent girls. However, we believe that the findings of this study can still be relevant and useful for programme planners and policymakers not only to encourage health facility-based deliveries but also to address the high rates of caesarean sections among married adolescent girls in Bangladesh.
Conclusions
It is promising that health facility-based deliveries are increasing among adolescents in Bangladesh. However, in order to ensure that all adolescent pregnant girls have access to health services provided by qualified staff, more efforts need to be put into maternal health programmes that particularly target rural poor adolescents and encouraging them to attend all ANC sessions and to deliver at a health facility. Although current trends in facility-based deliveries are reassuring, the rising trend of facility-based caesarean sections is alarming and calls for further qualitative investigations to identify causes and to take appropriate actions by the respective authorities in Bangladesh. In addition, more qualitative research that focuses on health system aspects and explores maternal healthcare-seeking behaviour of married adolescent girls is needed.
Acknowledgments
The authors acknowledge the European Commission and the Department of Economy, Science and Innovation of Flemish Government, Belgium, for funding. They thank Tahrima Mridha for editing the manuscript and Sergi Sanz for helping in statistical data presentation. Besides, the authors are thankful to ‘The Demographic and Health Surveys (DHS) Program’ for providing the data.
Footnotes
Twitter: Follow ASM SHAHABUDDIN at @Shahabuddin_Asm and Vincent De Brouwere at @vdbrouwere
Contributors: ASMS, TD and VDB are responsible for the design and planning of the study. ASMS participated in extraction, analysis and interpretation of the data. ASMS drafted the article, on which all authors made important suggestions. TD, AB, BU and VDB revised the article for important intellectual content. All authors revised and approved the final version of the article for publication.
Funding: This study, part of a PhD research, was funded by the European Commission and the Department of Economy, Science and Innovation of Flemish Government, Belgium.
Competing interests: None declared.
Ethics approval: This study was exempted from review by the ethics committee as publicly available data were used, and no identifying participant information was obtained. With the permission of MEASURE DHS, the authors downloaded the Demographic and Health Survey (DHS) data sets of Bangladesh from the website of MEASURE (www.measuredhs.com).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Bangladesh Demographic and Health Survey data sets of 1993–1994, 1996–1997, 1999–2000, 2004, 2007 and 2011 were used for this study. These data are public and freely available to anyone from MEASURE DHS, on request. The website for MEASURE DHS is http://dhsprogram.com/Data/.
References
- 1.Patton GC, Coffey C, Sawyer SM et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 2009;374:881–92. 10.1016/S0140-6736(09)60741-8 [DOI] [PubMed] [Google Scholar]
- 2.United Nations Population Fund. State of world population 2013: motherhood in childhood. New York: UNFPA, 2013. [Google Scholar]
- 3.United Nations Children's Fund. Progress and prospects 2014.
- 4.Sayem AM, Nury ATM. Factors associated with teenage marital pregnancy among Bangladeshi women. Reprod Health 2011;8:16 10.1186/1742-4755-8-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kamal SM, Hassan CH, Islam MN. Factors associated with the timing of antenatal care seeking in Bangladesh. Asia Pac J Public Health 2015;27:NP1467–80. 10.1177/1010539513485786 [DOI] [PubMed] [Google Scholar]
- 6.Shahabuddin ASM, Delvaux T, Abouchadi S et al. Utilization of maternal health services among adolescent women in Bangladesh: a scoping review of the literature. Trop Med Int Health 2015;20:822–9. 10.1111/tmi.12503 [DOI] [PubMed] [Google Scholar]
- 7. National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International. Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh and Calverton, Maryland, USA, 2013. [Google Scholar]
- 8.Hansen AK, Wisborg K, Uldbjerg N et al. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ 2008;336:85–7. 10.1136/bmj.39405.539282.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu S, Liston RM, Joseph KS et al. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ 2007;176:455–60. 10.1503/cmaj.060870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller ES, Hahn K, Grobman WA. Consequences of a primary elective cesarean delivery across the reproductive life. Obstet Gynecol 2013;121:789–97. 10.1097/AOG.0b013e3182878b43 [DOI] [PubMed] [Google Scholar]
- 11.Quiroz LH, Chang H, Blomquist JL et al. Scheduled cesarean delivery: maternal and neonatal risks in primiparous women in a community hospital setting. Am J Perinatol 2009;26:271–7. 10.1055/s-0028-1103155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Souza JP, Gülmezoglu A, Lumbiganon P et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med 2010;8:71 10.1186/1741-7015-8-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Villar J, Valladares E, Wojdyla D et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet 2006;367:1819–29. 10.1016/S0140-6736(06)68704-7 [DOI] [PubMed] [Google Scholar]
- 14.Gurol-Urganci I, Cromwell DA, Edozien LC et al. Risk of placenta previa in second birth after first birth cesarean section: a population-based study and meta-analysis. BMC Pregnancy Childbirth 2011;11:95 10.1186/1471-2393-11-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang X, Lei J, Tan H et al. Cesarean delivery for first pregnancy and neonatal morbidity and mortality in second pregnancy. Eur J Obstet Gynecol Reprod Biol 2011;158:204–8. 10.1016/j.ejogrb.2011.05.006 [DOI] [PubMed] [Google Scholar]
- 16.da Gama SGN, Viellas EF, Schilithz AOC et al. Factors associated with caesarean section among primiparous adolescents in Brazil, 2011–2012. Cad Saude Publica 2014;30(Suppl 1):S1–11. 10.1590/0102-311X00145513 [DOI] [PubMed] [Google Scholar]
- 17.Vogel J, Betran AP, Vindevoghel N et al. Use of the robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Heal 2015;3:e260–70. 10.1016/S2214-109X(15)70094-X [DOI] [PubMed] [Google Scholar]
- 18.Gibbons L, Belizan JM, Lauer JA et al. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol 2012;206:331.e1-19 10.1016/j.ajog.2012.02.026 [DOI] [PubMed] [Google Scholar]
- 19.Sufang G, Padmadas SS, Fengmin Z et al. Delivery settings and caesarean section rates in China. Bull World Health Organ 2007;85:755–62. 10.2471/BLT.06.035808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chowdhury AMR, Bhuiya A, Chowdhury ME et al. The Bangladesh paradox: exceptional health achievement despite economic poverty. Lancet 2013;382:1734–45. 10.1016/S0140-6736(13)62148-0 [DOI] [PubMed] [Google Scholar]
- 21.WHO. Trends in maternal mortality: 1990 to 2015. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division WHO, 2015:1–38. ISBN: 978 92 4 150363 1. [Google Scholar]
- 22.Haque SE, Rahman M, Mostofa MG et al. Reproductive health care utilization among young mothers in Bangladesh: does autonomy matter? Women Health Iss 2012;22:e171–80. 10.1016/j.whi.2011.08.004 [DOI] [PubMed] [Google Scholar]
- 23.Adhikari R. Effect of Women's autonomy on maternal health service utilization in Nepal: a cross sectional study. BMC Womens Health 2016;16:26 10.1186/s12905-016-0305-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahmed SM, Evans TG, Standing H et al. Harnessing pluralism for better health in Bangladesh. Lancet 2013;382:1746–55. 10.1016/S0140-6736(13)62147-9 [DOI] [PubMed] [Google Scholar]
- 25.El Arifeen S, Christou A, Reichenbach L et al. Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. Lancet 2013;382:2012–26. 10.1016/S0140-6736(13)62149-2 [DOI] [PubMed] [Google Scholar]
- 26.Mostafa Kamal SM. Preference for institutional delivery and caesarean sections in Bangladesh. J Heal Popul Nutr 2013;31:96–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conde-Agudelo A, Belizan JM, Lammers C. Maternal-perinatal morbidity and mortality associated with adolescent pregnancy in Latin America: cross-sectional study. Am J Obs Gynecol 2005;192:342–9. 10.1016/j.ajog.2004.10.593 [DOI] [PubMed] [Google Scholar]
- 28.Ganchimeg T, Ota E, Morisaki N et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG 2014;121(Suppl 1):40–8. 10.1111/1471-0528.12630 [DOI] [PubMed] [Google Scholar]
- 29.Kamal SMM. Factors affecting utilization of skilled maternity care services among married adolescents in Bangladesh. Asian Popul Stud 2009;5:153–70. 10.1080/17441730902992075 [DOI] [Google Scholar]
- 30.Mosiur R. Deliveries among adolescent mothers in rural Bangladesh: who provides assistance? World Health Popul 2009;11:5–14. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med5&NEWS=N&AN=20057269E [DOI] [PubMed] [Google Scholar]
- 31.Anwar I, Sami M, Akhtar N et al. Inequity in maternal health-care services: evidence from home-based skilled-birth-attendant programmes in Bangladesh. Bull World Health Organ 2008;86:252–9. 10.2471/BLT.07.042754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haque MN. Individual's characteristics affecting maternal health services utilization: married adolescents and their use of maternal health services in Bangladesh. Internet J Health 2009;8:16. [Google Scholar]
- 33.Ikeako LC, Onah HE, Iloabachie GC. Influence of formal maternal education on the use of maternity services in Enugu, Nigeria. J Obstet Gynaecol 2006;26:30–4. 10.1080/01443610500364004 [DOI] [PubMed] [Google Scholar]
- 34.Koblinsky M, Matthews Z, Hussein J et al. Going to scale with professional skilled care. Lancet 2006;368:1377–86. 10.1016/S0140-6736(06)69382-3 [DOI] [PubMed] [Google Scholar]
- 35.Mahavarkar SH, Madhu CK, Mule VD. A comparative study of teenage pregnancy. J Obstet Gynaecol 2008;28:604–7. 10.1080/01443610802281831 [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. Adolescent pregnancy: fact sheet. Geneva: WHO, 2014. [Google Scholar]
- 37.Feyissa TR, Genemo GA. Determinants of institutional delivery among childbearing age women in Western Ethiopia, 2013: unmatched case control study. PLoS One 2014;9:e97194 10.1371/journal.pone.0097194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Utz B, Halim A. Improving midwifery care worldwide. Lancet 2015;385:26–7. 10.1016/S0140-6736(14)62473-9 [DOI] [PubMed] [Google Scholar]
- 39.Aminu M, Utz B, Halim A et al. Reasons for performing a caesarean section in public hospitals in rural Bangladesh. BMC Pregnancy Childbirth 2014;14:130 10.1186/1471-2393-14-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Béhague DP, Victora CG, Barros FC. Consumer demand for caesarean sections in Brazil: informed decision making, patient choice, or social inequality? a population based birth cohort study linking ethnographic and epidemiological methods. BMJ 2002;324:942–5. 10.1136/bmj.324.7343.942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Francome C, Savage W. Caesarean section in Britain and the United States 12% or 24%: is either the right rate? Soc Sci Med 1993;37:1199–218. 10.1016/0277-9536(93)90332-X [DOI] [PubMed] [Google Scholar]
- 42.Islam MT, Yoshimura Y. Rate of cesarean delivery at hospitals providing emergency obstetric care in Bangladesh. Int J Gynecol Obstet 2015;128:40–3. 10.1016/j.ijgo.2014.07.021 [DOI] [PubMed] [Google Scholar]
- 43.Barros FC, Vaughan JP, Victora CG et al. Epidemic of caesarean sections in Brazil. Lancet 1991;338:167–9. 10.1016/0140-6736(91)90149-J [DOI] [PubMed] [Google Scholar]
- 44.Collin SM, Anwar I, Ronsmans C. A decade of inequality in maternity care: antenatal care, professional attendance at delivery, and caesarean section in Bangladesh (1991–2004). Int J Equity Health 2007;6:9 10.1186/1475-9276-6-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Neuman M, Alcock G, Azad K et al. Prevalence and determinants of caesarean section in private and public health facilities in underserved South Asian communities: cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open 2014;4:e005982 10.1136/bmjopen-2014-005982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anwar I, Nababan HY, Mostari S et al. Trends and inequities in use of maternal health care services in Bangladesh, 1991–2011. PLoS One 2015;10:e0120309 10.1371/journal.pone.0120309 [DOI] [PMC free article] [PubMed] [Google Scholar]