Abstract
BACKGROUND
The rise in childhood eye diseases has become a matter of concern in Saudi Arabia, and hence a study has been conducted on the residents of Jazan. The aim of the research was to find out the root cause of such issues and provide a solution to prevent such circumstances for it may affect the vision of children. In this study, therefore, we aimed to determine the types of childhood eye diseases in Jazan and to discuss the best ways to prevent them or prevent their effect on the vision of our children. Our institutions are working toward the longevity and welfare of the residents, and healthcare is one of the important aspects in such a field.
METHODS
This is a retrospective review of all patients less than 18 years of age who presented to the pediatric ophthalmology clinic of Prince Mohammed Bin Nasser Hospital, Jazan, between October 2014 and October 2015. The data, collected on 385 cases, included the age at first presentation, sex, clinical diagnosis, refractive error (RE) if present, and whether the child had amblyopia. If the child did not undergo complete ophthalmic examination with cycloplegic refraction, he/she was excluded. All data were collected and analyzed using the software SPSS. A P-value < 0.05 was considered statistically significant.
RESULTS
We reviewed the files of 385 children, with a male/female ratio of 1.1:1.0. The group aged 0–6 years made up the largest group (P = 0.01), and the ratio is an expression to define the credibility of the study using a chi-squared test. Strabismus (36.9%), RE (26.5%), ocular trauma (7.5%), infection of cornea and conjunctiva (7.3%), and keratoconus (6.2%) were the most common conditions. There was no significant difference in presentation by age group and sex among children with REs and squint. Trauma was seen more commonly among males and in the group aged 12–18 years.
CONCLUSION
In this retrospective study, the focus was on the common childhood eye diseases that were considerably high. Hypermetropia was the predominant RE, which is in contrast to other studies where myopia was more common. However, it is important to promote public education on the significance of early detection of strabismus, REs, and amblyopia and have periodic screening in schools. The discussion of the various issues is aimed at increasing the awareness and building a support for the cause by creating the knowledge base to treat things on time and acknowledging the severity of the issues.
Keywords: strabismus, pediatric ocular disorders, Jazan, refractive errors, amblyopia, keratoconus
Introduction
Eye diseases in children are an important cause of permanent loss of vision. A large number of children living in different parts of the world suffer from visual impairment. An estimated 285 million people around the world are visually impaired. Of this, 19 million are children below the age of 14 years. Children should receive proper screening and treatment of their eye disease to prevent loss of vision in the long term. Strategies to improve visual acuity screening and providing education on the importance of timely follow-up for eye care are important to avoid vision problems and eye morbidities.
The pattern of ocular disease varies from country to country and even from region to region in the same country.2 In the United States, strabismus, amblyopia, and optical problems impacting visual acuity are the most common ocular problems seen among school-age children.7 Refractive errors (REs) (44.4%), strabismus (38%), and amblyopia (9.1%) were the leading causes of childhood eye morbidity reported in a Private Hospital in Dammam, the Kingdom of Saudi Arabia (KSA).11
Methods
This is a retrospective review of all patients less than 18 years of age who presented to the pediatric ophthalmology clinic of Prince Mohammed Bin Nasser Hospital (PMNH), Jazan, between October 2014 and October 2015.
We divided the patients into three groups according to their age, namely 0–6 years, 6–11 years, and 12–18 years. Some patients were excluded because of missing information in the files. The pediatric ophthalmology clinic of PMNH serves as a referral center for all communities of Jazan. We collected the data on age at first presentation, sex, clinical diagnosis, RE if present, and whether the child had amblyopia. If the child did not undergo complete ophthalmic examination with cycloplegic refraction, he/she was excluded. Patients were seen by the pediatric ophthalmology consultant, who was only involved in this study. We collected data on age at first presentation, sex, clinical diagnosis, RE if present, whether child had amblyopia, and decision taken at the last visit. Data were stored and analyzed using the Statistical Package of the Social Sciences (SPSS) software. A P-value < 0.05 was considered statistically significant. This study aimed to determine the types of childhood eye diseases in a Jazan, Saudi Arabia, and to discuss the best ways to prevent them or prevent their effect on the vision of our children, as the institutions are working toward the longevity and welfare of the residents, and healthcare is one of the important aspects in such a field.
Results
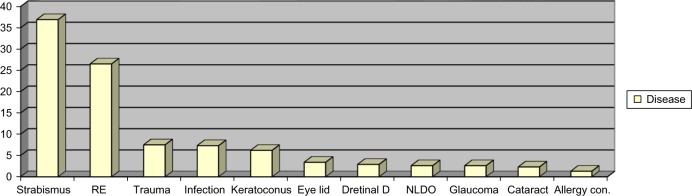
We reviewed 385 files of children who were seen in the pediatric ophthalmology clinic during the study period. There were 205 (53.2%) girls and 180 (46.8%) boys, resulting in a male/female ratio of 1.1:1.0, with no statistical significance. Figure 1 shows the age group and sex distribution of the children seen.
Figure 1.
Age group and sex distribution of children.
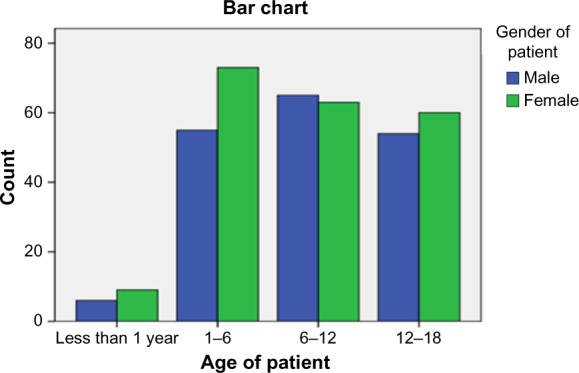
A common age group was 0–6 years. A female preponderance was seen in most age groups except in the group of 6–12 years. The highest frequency of consultation was recorded among younger children, constituting 143 (37.1%) of the patients (P = 0.01), and the ratio is an expression to define the credibility of the study using a chi-squared test. Strabismus was the most common disorder seen (36.9%), followed by RE (26.5%), which is the disorder where bending of light is a difficult task for the eye as the shape is not correct resulting in blurry images. There are various subgroups or types of RE, such as myopia, hyperopia, astigmatism, and presbyopia. Ocular trauma (7.5%), or eye injury, is a serious problem and a threat to vision, and it is more common in males than females (10.6% and 4.9%, respectively). Infection of the cornea and conjunctiva account for 7.3%, and keratoconus (KC) accounts for 6.2%. KC is a disorder caused by the thinning of the cornea, which results in visual distortion or blurry vision. KC cannot be cured simply by wearing glasses, and it starts during the late teenage, and hence the age bracket does qualify. The patient suffers from light sensitivity, eye strain, eye pain, and headaches, and cannot drive at night. Vernal keratoconjunctivitis (VKC) was seen in 1.3%. The lowest presentation was eyelid ptosis, which accounted for only 0.5% of all cases. Figure 2 shows the pattern of the common eye morbidities seen.
Figure 2.
Spectrum and frequency of eye morbidities seen.
Abbreviations: RE, refractive error; NLDO, nasolacrimal duct obstruction.
This table shows that there is a statistically significant difference in the prevalence of VKC according to the gender (male/female = 4:1) (P-value 0.025), the ratio expressing the credibility of the study using a chi-squared test. VKC is an allergic disease that affects the eye and is commonly found in boys, as suggested by the ratio of 4:1 and validated by the chi-squared test with a P-value of 0.025. The symptoms of VKC are burning sensation, tearing, itching of the eyes, and photophobia. The signs seen or noted are giant papillae, conjuctival hyperamia, and superficial keratitis. The patients who suffer from this disease are likely to have a history of atopic diseases in the family. This fact can be better established if the same is scrutinized for the 385 cases being looked into. However, due to the lack of time and resources, this could not be done.
There is no difference in presentation by age group and gender among children with REs and strabismus. The difference in presentation by age group was more prominent among children with KC, VKC, and nasolacrimal duct obstruction (NLDO). There were 24 (21.1%) cases of KC among older children, VKC also was recorded more frequently (3.5%) among older children, while NLDO was present only in the first age group (0–6 years); all of this is normal presentation of such diseases. Among the children who presented with infection, herpes stromal keratitis (HSK) is an inflammatory infection that causes damage to the ocular tissues. The damage can be severe, as it can affect the stroma, epithelium, or the endothelium and cause stromal opacity. HSK opacity is caused because of the immunopathology occurring within stroma, causing irreversible scarring of the stroma and leading to vision loss or blindness. Nineteen such patients (9.3%) were girls and nine (5%) were boys. All cases of childhood retinal disease were familial and due to retinal dystrophy diseases. Figure 3 illustrates the types of refractor error; the commonest refractor error is hyperopia, which was found in 138 children (35.8%) with approximately equal prevalence among both boys and girls. Table 2 shows the types of treatment that had been offered to the study population. Epidemic keratoconjunctivitis, or the pink eye, is an infection that is highly contagious and caused primarily by a virus called adenovirus. This, in conjunction with infections that affect the ocular surfaces, is the reason for infections spreading to the respiratory and the gastrointestinal tract. This particular infection causes inflammation of the conjunctiva. As a result of the inflammation of the membrane covering the sclera, the eye color turns pink or red. It is quite common in children and generally does not cause blindness. It has no effective treatment, and medicines are used only to reduce the inflammation.
Figure 3.
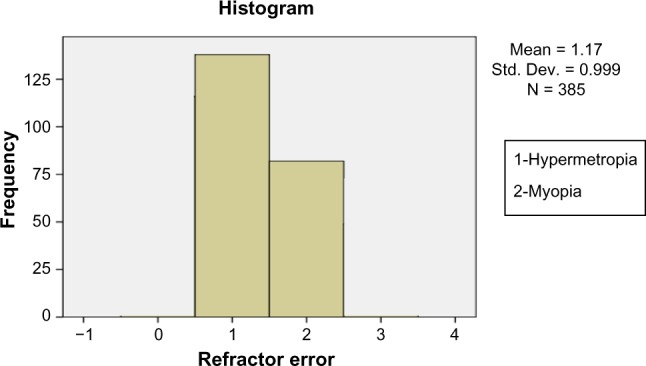
Types of refractor error.
Table 2.
Types of treatment.
| TREATMENT | FREQUENCY | PERCENT | VALID PERCENT | CUMULATIVE PERCENT |
|---|---|---|---|---|
| None | 24 | 6.2 | 6.2 | 6.2 |
| Amblyopia treatment (PTO + Botox) (Glasses + PTO) (med. + glass + PTO) (strab. Surgery + PTO + glass) (Botox + PTO + glasses) |
61 | 17.3 | 17.3 | 23.5 |
| Medication | 48 | 12.5 | 11.4 | 19.0 |
| CXL | 11 | 2.9 | 2.9 | 21.8 |
| Strab surgery | 17 | 4.42 | 3.4 | 25.2 |
| Botox | 5 | 1.3 | 3.1 | 28.3 |
| Surgery (cataract surgery) (probing) | 40 | 10.4 | 10.4 | 38.7 |
| Glasses | 156 | 40.5 | 40.5 | 79.2 |
| Contact lens | 9 | 2.3 | 2.3 | 81.6 |
| NLD massage | 4 | 1.0 | 1.0 | 82.6 |
| Total | 385 | 100.0 | 100.0 | 100 |
Abbreviations: PTO, part-time occlusion; CXL, corneal cross-linking; NLD, nasolacrimal duct.
In our study, the commonest cause of unilateral vision loss was amblyopia (15.3%) and that of bilateral blindness was retinal dystrophy (2.9%). The commonest treatment modality is glasses, which were offered to 156 (40.5%) of the children attending the eye clinic, followed by amblyopia treatment for 59 (15.3%) children.
Discussion
Any disease that curbs the development of a child affects his/her normal life, and pediatric ophthalmic disorders sabotage the growth years, as they curb not only the future prospects, educational capabilities, the child’s development, and the quality of life but also the opportunities that come in his/her way. These disorders mostly cause blindness or irregularities in vision, seriously affecting the daily chores. The rise in the number of the cases of blindness and its prevalence on a global scale are quite alarming, as they occur in 0.78 in 1000 people, which amounts to ∼1.5 million children who suffer from blindness, of which most hail from the developing countries. The reasons for such high prevalence are simply the lack of health care facilities, nutrition availability to children, and humid conditions. The issue of childhood blindness is on the rise, with ∼70 million blind years caused by childhood blindness, and it is the second highest cause for blindness, followed by cataract. It is seen that ∼500,000 children experience blindness every year, which means that one child becomes blind every minute, and the tragedy is that halfof this population dies within the first two years of becoming blind.1
Such alarming figures have been the driving force for this particular study and research on blindness. As understood from the study conducted, mostly the solution provided is glasses of some kind. The children who were brought to medical care facilities were mostly in the age group 0–6 years, their number being 143 of the 385 cases that were considered in this study. The higher number of younger children can be simply as a result of the facilities of the ophthalmology clinic that scrutinizes them, as well as the accessibility to a medical unit. The families are quite concerned about the child’s education and want to take good care of the child to provide him/her with a bright future; hence, they are very alert and keen on providing treatment for the child. However, the case is quite different in other countries such as in Nigeria, where the age group noted is completely different, with age as high as 11 years.2
According to our study, we find that strabismus is the most prominent disorder among the children in the 0–18 age bracket, with as high as 36.9% of the cases being studied. It is an important observation, because in most other case studies carried out in a holistic manner, it holds the second3 or third4 position. The reason for such high occurrence of this particular disorder needs to be further analyzed, as it is not quite clear in the study, because the environment does not clearly indicate it to be appropriate to lead to such a disorder. The relationship is mostly between strabismus and genetic factors.5 It is known that it can be caused as a result of genetic disorders, and in this particular case study the inappropriate development of the fusion center causes a lot of trouble, as brain functions change the way it is considered. As the study has shown that amblyopia is also a prevalent problem, it is highly likely that it can be caused from strabismus, as an outcome of brain functions ignoring the eye’s functionality, leading to amblyopia, which is the result of failure of both or one eye to achieve any normal functional behavior despite being deemed normal as well as structurally healthy. The visual development in the brain takes place between 0 and 8 years of age and hence it is extremely important for the brain of the child to interpret signals that originate in the eye, which is known as the process of visual development. This particular development is curbed when a child fixates on one particular eye and it does not really work with the other one. In the long run, the signals from the deviated or the lazy eye get suppressed by the good eye, which results as a failure in visual development. Our study concentrates on the interconnection between the concepts and disorders to derive a link to support the concepts being speculated.
RE is the most common morbidity disorder in children in the eastern province of Saudi Arabia,3 according to various case studies, while North India,4 Ethiopia,6 and Nigeria are the other countries exhibiting similar disorders.7 The incidence of REs in this study may have been underestimated since it was a hospital-based study. Uncorrected REs cause immediate and long-term problems such as poor educational performance, missed employment opportunities, and impaired quality of life.8 Vision 2020 (Global initiative of World Health Organization for the prevention of avoidable blindness) has identified uncorrected REs in children as a major area that needs immediate action.9
Early screening of school-age children is an important measure to discover the magnitude of RE and take immediate corrective action.10 In this study, the REs were almost equally distributed among boys and girls. This is in contrast to previous studies in Al Hassa and Riyadh, KSA, where the errors were more prevalent in females than in males.10,11 This study aimed to determine the types of childhood eye diseases in a Jazan and discuss the best ways to prevent it or prevent their effect on the vision of our children, as the institutions are working toward the longevity and welfare of the residents and healthcare is one of the important aspects in such a field.
In this study, RE was found in 26.5% of the children. This frequency is higher than that in some studies conducted in KSA,10,11 but less than that in some other studies also conducted in KSAs.12 The reported prevalence of RE in different parts of the world show a variation from 7.0% to 19.8%, as shown in Table 3.
Table 3.
Distribution of RE subtypes among school-age children in different studies from Saudi Arabia.
| STUDIES | YEAR | AGE GROUP | SAMPLE SIZE | PREVALENCE OF RE. (%) | MYOPIA (%) | HYPEROPIA (%) |
|---|---|---|---|---|---|---|
| Abu-shagra et al.20 | 1991 | 6–9 | 1188 | 10 | 50 | 15 |
| Ali et al.21 | 2007 | 10–16 | 540 | 19.8 | 43 | 21.5 |
| Hashim et al.22 | 2008 | 10–15 | 840 | 7.0 | 77.5 | 14.3 |
| Al-Nuaimi.23 | 2010 | 6–13 | 670 | 19.7 | 73 | 17 |
| Al-Rowaily and Alainizi.18 | 2010 | 12–13 | 1536 | 9.8 | 57.6 | 15.2 |
| Al-Wadaani et al.17 | 2013 | 6–14 | 2002 | 13.7 | 65.7 | 12.4 |
| Al-Tmimi and Shakeel.11 | 2013 | 5–15 | 1350 | 44.4 | 13.3 | 83 |
| Current study | 2016 | 0–18 | 385 | 26.5 | 21.3 | 35.8 |
However, the distribution of subtypes of RE among children shows that hypermetropia is more common than myopia. This is in contrast to some other studies in which myopia was the predominant type of RE,13–16 but is the same compared to some others.3 The predominance of hypermetropia in this study could be attributed to the sample selection criteria and to the high number of patients with esotropia and amblyopia, who were seeking medical care since simple myopic cases are usually dealt with by optometrists. Eye infections or retinal diseases are less fatal, as they do not lead to blindness, but they can cause damage that is repairable. Our study is aimed at creating awareness in people of the importance of eye care in children who are in the age bracket 0–18 years and more specifically the age bracket 0–6 years.
Eye injuries remain a major cause of unilateral visual impairment worldwide17,18 and a common cause of non-congenital unilateral blindness.19 But it is not the case in our city, where amblyopia is the most common one due to poor compliance of family and children with treatment to correct their vision. Amblyopia showed a prevalence of 27% and 31% among children with anisomatropia and in those with strabismus, respectively,20 and ∼1.6%–3.6% in another study.21 In our study, it is about 15.3% in all the morbidity diseases present in our community. The reasons range from the child’s cooperation to a lack of family education and the low socioeconomic status of some children involved, because some of them need more than three changes of glasses per month due to breakage. Amblyopia is one of the most common causes of visual deficit in childhood, and since it is treatable, at least in children, considerable efforts have been made to detect it as early as possible.22
The best approach to managing amblyopia is to detect amblyogenic factors before the age of two years and prevent it by eliminating the causes of visual deprivation.23 Screening programmes for amblyopia among preschool and school children have been widely organized throughout the world, although questions remain about their utility.22 In fact, the relationship between strabismus, hypermetropia, and amblyopia is complex. A significant bilateral hypermetropia or ocular misalignment presenting during the critical period of visual development (from birth to the age of seven years) will lead to development of amblyopia.3
The findings of present study validate the implementation of the fundamental guidelines including the recommendations that the parents of children with REs, strabismus, and amblyopia should have their children screened, promoting parent education, and distributing brochures on amblyopia and strabismus at the ophthalmology center at PMBN hospital. Periodic awareness campaigns on pediatric visual problems and the importance of early detection and management including screening examination when feasible should be carried out at different places, including schools, shopping malls, and through social media.
KC prevalence in our study is 6.2%, being equal in boys and girls, but it is present in older children as shown by a previous study in KKESH (King Khaled Eye Specialist Hospital). Its incidence is 23.75% in the age group 16–20 years.24 In India2 and Nigeria,25,26 allergic conjunctivitis is quite common owing to the climatic conditions. Allergic conjunctivitis is the most common disease all over the world, but is more common in hot climates.27 But in our study, it is low in the list of morbidity diseases attended to in our clinic though we have the same communities with largely agrarian labor and a dusty environment.25,28
In summary, this study was aimed at determining the types of childhood eye diseases in Jazan and discussing the best ways to prevent them or prevent their effect on the vision of our children.
Limitations
The study was conducted keeping in mind the types of disorders that are prevalent and noticed over the years in various places. The age group selected was 0–18 years, which is quite a wide range for any survey or study, especially while studying the various disorders and ophthalmological issues noted at the nascent stages or in childhood. There is scope for various other studies within the same age group, but to explain the categories being targeted, the age group has to be specified rather than simply excluding the disorders from the study. The number of cases studied was 385, and we have thoroughly justified the categories that have been considered, and the sample size does justify the entire population of the patients who have been enrolled in the hospital in the age bracket of 0–18 years.
Conclusion
In this retrospective study, the frequency of strabismus, REs, and amblyopia has been highlighted since their prevalence was considerably high. Hypermetropia was the predominant RE, which is in contrast to the findings of other studies where myopia was more common. However, there should be an emphasis on educating the public on the significance of early detection of strabismus, REs, and amblyopia and on periodic screening in schools. Meanwhile, trachoma (33.7%), REs (6.3%), and non-trachomatous conjunctivitis (5.9%) were the most common childhood eye disorders reported in Ethiopia.9 This will help in the early detection and treatment of REs, strabismus, and amblyopia and thereby reduce the prevalence of strabismus and amblyopia in children, and consequently improve their educational opportunities and quality of life.
Table 1.
Spectrum of childhood eye disorders according to the gender and age groups.
| DIAGNOSIS | GENDER OF PATIENT | TOTAL (%) | 0–6 (%) | 60–12 (%) | 120–18 (%) | TOTAL (%) | |
|---|---|---|---|---|---|---|---|
| MALE (%) | FEMALE (%) | ||||||
| Strabismus | 66 | 76 | 142 | 65 | 54 | 23 | 142 |
| 36.70% | 37% | 36.90% | 45.50% | 42.20% | 20.20% | 36.90% | |
| Infection | 9 | 19 | 28 | 12 | 7 | 9 | 28 |
| 5.00% | 9.30% | 7.30% | 8.40% | 5.50% | 7.90% | 7.30% | |
| Trauma | 19 | 10 | 29 | 8 | 5 | 16 | 29 |
| 10.60% | 4.90% | 7.50% | 5.60% | 3.90% | 14.00% | 7.50% | |
| Cataract | 6 | 3 | 9 | 7 | 1 | 1 | 11 |
| 3.30% | 1.50% | 2.30% | 4.90% | 0.80% | 0.90% | 2.30% | |
| Glaucoma | 3 | 7 | 10 | 3 | 2 | 5 | 10 |
| 1.70% | 3.40% | 2.60% | 2.10% | 1.60% | 4.40% | 2.60% | |
| Refractive error | 44 | 58 | 102 | 26 | 49 | 27 | 102 |
| 24.40% | 28.30% | 26.50% | 18.20% | 38.30% | 23.70% | 26.50% | |
| Eyelid disease | 4 | 9 | 13 | 6 | 5 | 2 | 13 |
| 2.20% | 4.40% | 3.40% | 4.20% | 3.90% | 1.80% | 3.40% | |
| Keratoconus | 13 | 11 | 24 | 0 | 0 | 24 | 24 |
| 7.20% | 5.40% | 6.20% | 0.00% | 0.00% | 21.10% | 6.20% | |
| Allergic conjunctivitis/VKC | 4 | 1 | 5 | 1 | 0 | 4 | 5 |
| 2.20% | 0.50% | 1.30% | 0.70% | 0.00% | 3.50% | 1.30% | |
| Retinal disease | 8 | 3 | 11 | 4 | 4 | 3 | 11 |
| 4.40% | 1.50% | 2.90% | 2.80% | 3.10% | 2.60% | 2.90% | |
| NLDO | 4 | 6 | 10 | 10 | 0 | 0 | 10 |
| 2.20% | 2.90% | 2.60% | 7.00% | 0.00% | 0.00% | 2.60% | |
| Ptosis | 0 | 2 | 2 | 1 | 1 | 0 | 2 |
| 0.00% | 1% | 0.50% | 0.70% | 0.80% | 0.00% | 0.50% | |
| Total | 180 | 205 | 385 | 143 | 128 | 114 | 385 |
| 46.80% | 53.20% | – | 37.10% | 33.20% | 29.60% | – | |
Note: The spectrum and frequency of eye morbidities are given according to the gender and age groups.
Footnotes
ACADEMIC EDITOR: Joshua Cameron, Editor in Chief
PEER REVIEW: Four peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1596 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: AD, SB, WB, MK, RS, AK, A Makin, A Mohanna. Analyzed the data: AOY. Wrote the first draft of the manuscript: AD. Contributed to the writing of the manuscript: SB. Agree with manuscript results and conclusions: MK. Jointly developed the structure and arguments for the paper: SB. Made critical revisions and approved final version: AD, WB, MK, RS, AK, SB, A Makin, A Mohanna. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Nwosu SNN. Childhood eye diseases in Anambra State, Nigeria. Niger J Ophthalmol. 1999:34–8. [Google Scholar]
- 2.Pratab VB, Lai HB. Pattern of pediatric ocular problem in north India. Indian J Ophthalmol. 1989;37:171–2. [PubMed] [Google Scholar]
- 3.Adegbehingbe BO, Adeoye AO, Onakpoya OH. Refractive errors in childhood. Niger J Surg Sci. 2005;15:19–25. [Google Scholar]
- 4.Narayana KM, Bora A, Biswas J. Pattern of uveitis in children presenting at a tertiary eye care centre in south India. Indian J Ophthalmol. 2003;52:129–32. [PubMed] [Google Scholar]
- 5.Gilbert C. Childhood blindness. In: Johnson G, Minassan D, Wealle R, editors. Epidemiology of Eye Diseases. London: Chapmann and Hall; 1998. pp. 183–8. [Google Scholar]
- 6.King RA. Common ocular signs and symptoms in childhood. Pead Cli North Am. 1993;40:753–66. doi: 10.1016/s0031-3955(16)38585-6. [DOI] [PubMed] [Google Scholar]
- 7.Castenes MS. Major review: the underutilization of vision screening (for amblyopia, optical anomalies and strabismus) among preschool age children. Binocul Vis Strabismus Q. 2003;18:217–32. [PubMed] [Google Scholar]
- 8.Ajaiyeoba AA. Childhood eye disease in Ibadan. Afr J Med Sci. 1994;23:227–32. [PubMed] [Google Scholar]
- 9.Mohammed S, Abebe B. Common eye diseases in children of rural community in Goro district, Central Ethiopia. Ethiopia J Health Dev. 2005;19:148–52. [Google Scholar]
- 10.Onakpoya OH, Adeoye AO. Childhood eye diseases in southwestern Nigeria: a tertiary hospital study. Clinics (Sao Paulo) 2009;64(10):947–52. doi: 10.1590/S1807-59322009001000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Tamimi ER, Shakeel A, Yassin SA, Ali SI, Khan UA. A clinic-based study of refractive errors, strabismus, and amblyopia in pediatric age-group. J Family Community Med. 2015;22(3):158–62. doi: 10.4103/2230-8229.163031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Michaelides M, Moore AT. The genetics of strabismus. J Med Genet. 2004;41(9):641–6. doi: 10.1136/jmg.2004.021667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al Wadaani FA, Amin TT, Ali A, Khan AR. Prevalence and pattern of refractive errors among primary school children in Al Hassa, Saudi Arabia. Glob J Health Sci. 2013;5:125–34. doi: 10.5539/gjhs.v5n1p125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al Rowaily M, Alanizi B. Prevalence of uncorrected refractive errors among adolescents at king Abdul-Aziz Medical City, Riyadh. J Clin Exp Ophthalmol. 2010;1:114. [Google Scholar]
- 15.Bardisi WM, Bin Sadiq BM. Vision screening of preschool children in Jeddah, Saudi Arabia. Saudi Med J. 2002;23(4):445–9. [PubMed] [Google Scholar]
- 16.Abu-Shagra S, Kazi G, Al-Rushood A, Yassin S. Prevelance and causes of visual acuity defect in male school children in Al-Khobar area. Saudi Med J. 1991;12:397–402. [Google Scholar]
- 17.Ali A, Ahmed I, Ayub S. Prevalence of undetected refractive errors among school children. Biomedica. 2007;23:96–101. [Google Scholar]
- 18.Hashim SE, Tan HK, Wan-Hazabbah WH, Ibrahim M. Prevalence of refractive error in malay primary school children in suburban area of Kota Bharu, Kelantan, Malaysia. Ann Acad Med Singapore. 2008;37:940–6. [PubMed] [Google Scholar]
- 19.AL-Nuaimi A, Salama R, Eljack I. Study of refractive errors among school children Doha. World Fam Med J. 2010;8:41–8. [Google Scholar]
- 20.Padhye AS, Khandekar R, Dharmadhikari S, Dole K, Gogate P, Deshpande M. Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East Afr J Ophthalmol. 2009;16:69–74. doi: 10.4103/0974-9233.53864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bataineh A, Khatatbeh E. Prevalence of refractive errors in school children of Tafila city. Rawal Med J. 2008;33:85–7. [Google Scholar]
- 22.Pokharel A, Pokharel PK, Das H, Adhikari S. The patterns of refractive errors among the school children of rural and urban settings in Nepal. Nepal J Ophthalmol. 2010;2:114–20. doi: 10.3126/nepjoph.v2i2.3717. [DOI] [PubMed] [Google Scholar]
- 23.Yared AW, Belaynew WT, Destaye S, Ayanaw T, Zelalem E. Prevalence of refractive errors among school children in Gondar Town, Northwest Ethiopia. Middle East Afr J Ophthalmol. 2012;19:372–6. doi: 10.4103/0974-9233.102742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niiranem M, Ratvio I. Eye injuries in children. Br J Ophthalmol. 1981;65:436–8. doi: 10.1136/bjo.65.6.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tabbara KF, El-Sheikh HF, Shawaf SS. Pattern of childhood blindness at a referral center in Saudi Arabia. Ann Saudi Med. 2005;25(1):18–21. doi: 10.5144/0256-4947.2005.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization . Prevention of childhood blindness Causes of Childhood Blindness and Current Control Measures. Geneva: WHO Study Group; 1992. pp. 21–2. [Google Scholar]
- 27.Abolfotouh MA, Badawi I, Faheem Y. Prevalence of amblyopia among schoolboys in Abha city, Asir Region, Saudi Arabia. J Egypt Public Health Assoc. 1994;69(1–2):19–30. [PubMed] [Google Scholar]
- 28.Simons K. Amblyopia characterization, treatment, and prophylaxis. Surv Ophthalmol. 2005;50(2):123–66. doi: 10.1016/j.survophthal.2004.12.005. [DOI] [PubMed] [Google Scholar]