Abstract
Background: Symbrachydactyly is a unilateral congenital hand malformation characterized by failure of formation of fingers and the presence of rudimentary digit nubbins. The management is variable and are investigated in this review. Methods: A detailed review of the literature was compiled into succinct clinically relevant categories. Results: Etiology, classification, non-surgical management, surgical intervention, and patient oriented outcomes are discussed. Conclusions: All interventions should prioritize realistic, evidence-supported appearance and functional gains. Studies of the baseline function and quality of life of children with symbrachydactyly would allow surgeons to better understand functional changes associated with various interventions and would help surgeons and parents to make the best treatment decisions.
Keywords: congenital hand, symbrachydactyly, Poland syndrome
Introduction
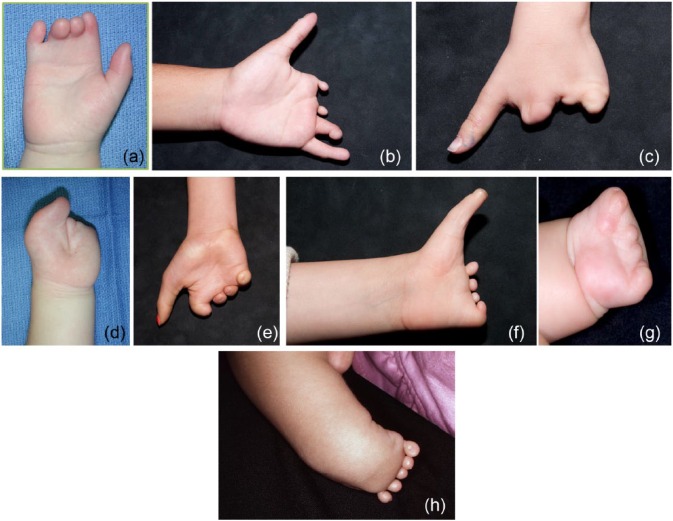
Symbrachydactyly is a unilateral hand malformation characterized by failure of formation of fingers and presence of rudimentary nubbins that include elements of nail plate, bone, and cartilage. Typically, the central digits are absent and the border digits are relatively spared, and syndactyly may be present27 (Figure 1).
Figure 1.

A typical hand with symbrachydactyly.
The incidence of symbrachydactyly is approximately 0.6/10 000 live births. It is usually isolated, but can be associated with Poland syndrome, in which hypoplasia or absence of the pectoralis major occurs with additional variable abnormalities13 (Figure 2). In fact, Poland first described symbrachydactyly in 1841.51
Figure 2.

The chest in Poland syndrome, with hypoplasia of the pectoralis major muscle.
Etiology
The etiology of symbrachydactyly is unknown, but vascular dysgenesis during fetal development (“subclavian artery supply disruption sequence”) is a leading hypothesis.2 Based on this hypothesis, isolated transverse terminal limb deficiencies are associated with interruption of the subclavian artery distal to the internal thoracic artery before a gestational age of 42 days, leading to a failure of outward limb growth and interdigital tissue degeneration. In support of this theory, a study of 8 patients with Poland syndrome showed decreased blood flow velocity in affected limbs, likely from a subclavian malformation.5
Based on the current understanding of upper limb development, symbrachydactyly likely arises through disruption of the apical ectodermal ridge (AER) of the developing limb bud. The AER, a thickening of ectodermal cells at the distal end of the limb bud, directs proximal-distal limb development through a complex cascade of growth factors and genetic signaling, while controlling aspects of mesenchyme cell differentiation.15 In animal models, disruption of the AER and its signaling pathways causes transverse deficiencies, including symbrachydactyly.60,66
Although limb development occurs in a proximal-distal direction, there may be some regenerative capacity of distal limb elements after a partial or complete insult to the AER that may result in the characteristic “nubbins” or rudimentary digits seen in symbrachydactyly.23
Clinical Presentation and Differential Diagnosis
The term symbrachydactyly has been used to describe hand malformations that overlap with transverse deficiency, central deficiency, brachymetacarpia, brachyphalangism, and hypodactyly.38 Symbrachydactyly was previously called “atypical cleft hand” due to morphological similarities with central deficiency,16 but this terminology has been abandoned41; central deficiency is an autosomal dominant condition in which the central rays are absent; it is usually bilateral and often associated with cleft feet. Other conditions in the differential diagnosis of symbrachydactyly include Apert syndrome, amniotic constriction bands, ulnar longitudinal deficiency, and hypodactyly38 (Table 1).
Table 1.
Differential Diagnosis of Symbrachydactyly.
| Symbrachydactyly | Apert syndrome | Amniotic constriction band | Central deficiency | Ulnar longitudinal deficiency | Hypodactyly | |
|---|---|---|---|---|---|---|
| Origin | Sporadic | Mutation, FGFR2 | Sporadic | Heritable, multiple loci | Generally sporadic, occasionally syndromic | Sporadic |
| Upper extremities | Unilateral | Bilateral, complex syndactyly | Usually bilateral, unilateral is rare | Generally bilateral | Unilateral | Unilateral |
| Lower extremities | Not affected | Affected | Affected (constriction bands and talipes equinovarus) | Affected | Not affected | Not affected |
| Thumb involvement | Least likely digit to be involved (peromelic and monodactylous forms) | Commonly involved in complex syndactyly | Equally likely to be involved as other digits | First web space commonly shallow/narrow. Thumb rarely suppressed | Least likely digit to be involved, but can be affected | Least likely digit to be involved, but can be affected |
| Shape of hand defect | U-shaped cleft | Cup like | Amputations common distal to bands | V-shaped cleft | Missing ulnar-sided structures, smooth contours on hand | Missing terminal elements only, deficiency may be more severe at ulnar digits |
| Unique features | Rudimentary nubbins with ectodermal tissue. Metacarpals present | Facial features (craniosynostosis, acrocephaly) | Visible scarring/depression from amniotic band | Absent metacarpals | Proximal structures (ie, elbow) more likely affected than wrist | Multiple shortened digits without terminal ectodermal elements |
Confusion surrounding the definition of symbrachydactyly is due to variability in clinic presentation, including the amount of hypoplasia of the central digits, affected hand size, and the function of border digits. We will use “symbrachydactyly” to describe the unilateral, sporadic presence of shortened or absent central digits with relative sparing of the border digits.
Classification
The International Federation of Societies for Surgery of the Hand (IFSSH) has recently adopted the Oberg, Manske, and Tonkin (OMT) classification system,30 which incorporates current understanding of embryology and molecular biology. Under the previous IFSSH system, symbrachydactyly was categorized as an undergrowth61; in the OMT system, symbrachydactyly is categorized as failure of formation of the proximal-distal axis, which can involve the entire upper limb or the hand plate.63
Several classifications of symbrachydactyly have been described. Blauth4 refined Müller’s original concepts47 into a classification system for symbrachydactyly that included 4 phenotypes:
Short finger type
Cleft hand type
Monodactyly type: absence of digits 2 to 5, with the thumb present
Peromelic type: adactyly with rudimentary nubbins.
Yamauchi and Tanabu68 described a more elaborate classification of 7 types based on the morphological and radiographic bony deficiency, allowing for precise description of skeletal elements of the affected hand and extremity, but not providing guidance for treatment. Foucher19 modified the Blauth classification to make it more useful in this regard, based on a series of 117 patients. The presence of a thumb, the stability of joints, and the patient-specific needs were used to recommend surgical treatment (see Table 2 and Figure 3).
Table 2.
Foucher’s Classification.
| Type | Features | Thumb | Ulnar digit | Interventions |
|---|---|---|---|---|
| I | All bones and digits present, brachydactyly and syndactyly | Normal | Bones present, brachydactyly or syndactyly | Syndactyly release |
| IIA | ≥2 fingers. Normal thumb, hypoplastic fingers | Normal | Hypoplastic, syndactyly | Nonvascularized toe phalanx transfers, ablation, or stabilization |
| IIB | Functional border digits, variable central nubbins | Normal | Present, variable hypoplasia and stability | Surgery rarely indicated |
| IIC | “Spoon hand,” thumb conjoined with hypoplastic ulnar digits | Present (± stability) | Hypoplastic, clinodactyly | Variable |
| IIIA | Monodactyly | Normal | Absent | Vascularized toe-to-hand transfer |
| IIIB | Monodactyly | Hypoplastic and/or unstable | Absent | Variable, vascularized toe-to-hand transfer, thumb stabilization, thumb lengthening |
| IVA | Peromelic, wrist mobility | Absent | Absent | |
| IVB | Peromelic, no wrist mobility | Absent | Absent | Surgery not indicated |
Figure 3.
The spectrum of symbrachydactyly as classified by Foucher: (a) type I, (b) type IIA, (c) type IIB, (d) type IIC, (e) type IIIA, (f) type IIIB, (g) type IVA, and (h) type IVB.
Note. A description of each type is listed in Table 2.
Treatment Goals
The goals of treating congenital hand differences are to maximize function, normalize appearance, and help the child and family accept the difference to the extent that it cannot be “normalized.” Selection of a specific treatment for symbrachydactyly depends on the clinical and radiological findings, the ability of the child to meet developmental milestones and perform activities of daily living, and the expectations of the child and family regarding the appearance of the hand. Treatment is grounded in the framework of realistic functional goals, with a reasonable expectation that the treatment can achieve that goal.
Nonoperative Management
Function is classified according to the World Health Organization International Classification of Functioning and Disability (http://www.who.int/classifications/icf/en/).67 Activity, participation, and quality of life may be very close to normal for children with unilateral hand absence.32 Often the biggest challenge to the child and family is the psychological burden of appearing different to others.1
Nonoperative interventions, such as therapy, prostheses, and orthotics, have been used to treat children with symbrachydactyly. An occupational therapist can help children with unilateral malformations master activities of daily life while increasing self-esteem and gaining independence.39
Because they cannot provide sensation, prostheses have limited applications for children with unilateral conditions, especially when the affected side has wrist motion and/or at least one sensate digit that can assist the contralateral hand with bimanual activities. Opposition paddles or partial hand prostheses may be helpful for patients with a stable monodactyly because they provide a surface to pinch against (Figure 4). Customized passive hand prostheses may provide relief from unwelcome questions and comments. As technology improves so that components can be made smaller, less expensive, and more durable, myoelectric partial hand prostheses may become useful to children with symbrachydactyly.
Figure 4.

A patient with symbrachydactyly wearing an opposition paddle.
Peer groups and hand camps may improve the child’s quality of life more than medical or surgical treatment.44,59 Camps exist for children with various chronic illnesses and congenital conditions; these have been shown to provide short-term psychosocial benefits, including improved social interaction and acceptance.46,49 Camps for children with congenital hand differences include Camp Winning Hands in Livermore, California (http://www.shrinersinternational.org/Press/Camp_Winning_Hands.aspx) and Hand Camp in Meridian, Texas (http://www.tsrhc.org/camp).
Operative Treatment
Surgical treatments are categorized by the specific aspect of symbrachydactyly that the treatment addresses: syndactyly and web contracture, brachydactyly and digit instability, and lack of opposition.
Syndactyly and Web Contracture
Syndactyly and web contractures are treated to improve independent digital function, grasp span, and appearance. For incomplete simple syndactyly of the digits, 2-fold or 4-fold Z-plasty is usually sufficient26 (Figure 5). Options for deepening the first web space include multiple Z-plasties, local rotational flaps, and more complex advancement techniques6,8,10-12,17,21,65 (Figure 6). Release of the first web space in symbrachydactyly can be more challenging than similar releases done for other diagnoses due to a lack of local skin available.21
Figure 5.
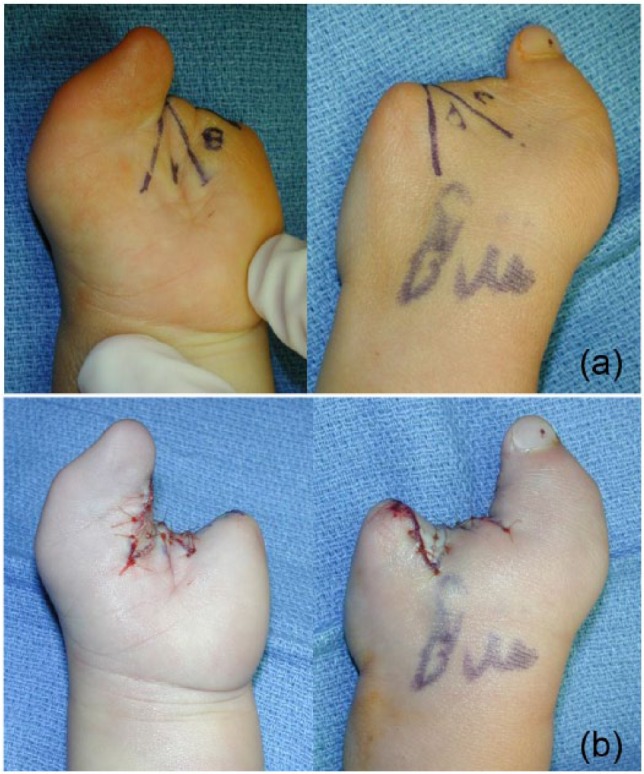
Fourfold Z-plasty to open the web space of the patient with type IIC symbrachydactyly. (a) Preoperative planning of the flaps. (b) Postoperative appearance.
Figure 6.

A dorsal rotational flap for more severe deficiency of the first web space. (a) Preoperative and (b) Postoperative.
Brachydactyly and Digit Instability
Nonvascularized free toe phalanx transfers
This operation is intended to augment the length and stability of the fingers to improve prehension and appearance. It has been advocated for short metacarpals or phalanges with an adequate distal soft-tissue envelope to receive the transferred phalanx; toe proximal phalanges must be available for transfer50 (Figure 7). The literature reveals variable results, with longer term follow-up showing more disappointing outcomes.
Figure 7.
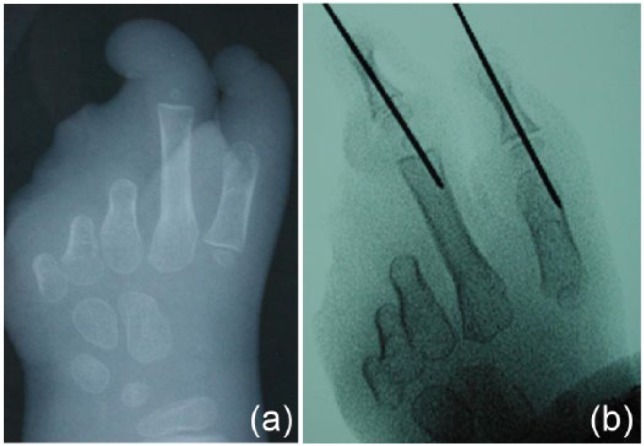
(a) Preoperative and (b) postoperative radiographs of nonvascularized toe phalanx transfers.
The technique includes preserving the volar plate, collateral ligaments, physis, and periosteum of the transferred phalanx, as described by Goldberg.25 In that series of 15 patients, the authors found that physes were more likely to remain radiographically open in children who were younger at the time of the transfer.25
Buck-Gramcko reported similar outcomes in 97 extraperiosteal nonvascularized proximal toe phalanx transfers in 57 children,7 and Radocha52 reported that the preservation of the periosteum contributed to the growth of the transferred segment in children younger than 12 months at the time of surgery.
More recently, however, Cavallo9 studied 64 nonvascularized toe phalanx transfers in 22 children, 18 with symbrachydactyly, and concluded that little longitudinal growth occurred but transverse growth did occur, and contributed stability to the digits. In 11 cases, the transfer was unstable; this complication was most common in patients with symbrachydactyly.
Tonkin62 reported on 10 children treated with nonvascularized toe phalanx transfers, with a mean follow-up of 7 years. Function testing showed that 5 could use their digit for complex activities, 2 for simple tasks, and 3 for assisting the other hand. Parents reported satisfaction with appearance of the hand and feet, but felt there was no improvement in the hand’s function. Most recently, Garagnani22 studied 40 children with a mean follow-up of 10 years, and found ubiquitous donor site morbidity that increased with growth, along with a high rate of emotional problems with foot appearance and functional problems with footwear.
None of these studies followed children to skeletal maturity and few offered thorough assessments of the function and appearance of the hand following surgery, making evaluation of this procedure difficult. Complete resorption of the transferred phalanx has been observed, as might be expected with a terminal bone graft, and claims of advantages of performing this operation early have not held up. Furthermore, claims of growth of the transferred phalanx are often based on radiographic patency of the physis, but animal studies have shown that radiolucency does not necessarily indicate that a physis is growing.55 If surgery is postponed until the child is older they can participate in the decision making, the phalanx is larger, and there is less growth potential to lose.
This operation may be useful in type IIA symbrachydactyly, when the base of the proximal phalanx is present along with a generous soft-tissue envelope. The cartilage at the base of the transferred phalanx can be debrided allowing bony healing between the ossific nucleus and the phalanx, reducing the likelihood of instability. When considering this operation, the surgeon should counsel parents and patients to adjust their expectations for cosmetic and functional outcomes, including foot appearance.33
Distraction lengthening
Lengthening a bone by distraction osteogenesis with or without secondary intercalary bone grafting is potentially useful for the treatment of short fingers in symbrachydactyly, but the indications for lengthening are unclear.42 This treatment rarely normalizes appearance and is fraught with complications. The literature shows mixed results with little information to indicate whether this procedure improves function and appearance.
Hulsbergen-Kruger’s series of 3 patients with symbrachydactyly indicated that attempts to lengthen hypoplastic bones, including transferred toe proximal phalanges, resulted in pseudarthroses, infections, and resorption with no reported improvement in function.29 Foucher20 reviewed results of distraction lengthening in 41 patients (22 with symbrachydactyly) and reported an average gain of 2.3 cm over 4 months. Complications included infection, nonunion, or fracture in 32%. Miyawaki45 reported 4 successful cases of metacarpal lengthening in patients with types IIA, IIB, and IIIA, noting improved pinch strength with no major complications; others43 have reported angulation of the lengthened bones, with unsatisfactory appearance. Heo28 reported a series of 24 metacarpal and 27 phalangeal lengthening procedures with a 31% complication rate, including nonunion, fracture, premature consolidation, angulation, and hardware failure.
Seitz57 has reported a large series reflecting his long-term experience with distraction lengthening in the arm, forearm, and hand for children with a wide range of conditions. He acknowledges that this treatment is complex and arduous and has a high complication rate (50% minor, 9% major) but reports that in most cases increased length is achieved and the family and child are satisfied.
Given the high rates of complications reported for distraction lengthening and the paucity of evidence to support significant functional gains, we rarely perform this procedure and do not advocate it for symbrachydactyly.
Free vascularized toe-to-hand transfer
Although toe-to-hand transfer is well accepted for the treatment of traumatic amputations in adults and children, its indications for reconstruction of congenital malformations remain more nuanced.
In 1988, Lister40 described 12 toe-to-hand transfers in children with various congenital hand differences, including 3 cases of symbrachydactyly, and noted unique neurovascular anatomic variations in each patient. Others have reinforced that there is a wide variation in the neurovascular structures in symbrachydactyly.35,40,53 In 2001, Foucher18 reported on 51 toe transfers in 45 patients with symbrachydactyly. Transfers to types IIIA and IIIB were the most common, followed by type IVA. In children with type IIIB, a combination of toe transfers to finger positions with vascularized epiphysis and nonvascularized toe phalanx transfer to the thumb was done. They found no functional problems with donor feet. At 5-year follow-up, range of motion (ROM) was adequate, and most participants reported that they used the affected hand in daily activities.
In 2004, Richardson53 described the results of 18 free toe transfers in 13 patients with symbrachydactyly. The results of a bimanual hand function questionnaire indicated that 61% could lift a cup, 54% could button, 38% could cut paper, and 30% could use a knife and fork; 85% of parents were happy with the appearance of the hand and 77% were happy with the function of the hand. Because of diverse vascular anatomy, the authors recommended obtaining an angiogram preoperatively.
Schenker56 evaluated grip function after free toe transfer in children with hypoplastic digits, finding that the participants could use the transferred digit to lift a small object with a precision grip, but only one-third modulated their grip in proportion to the load being grasped. They found increased forces on the fingertips of transplanted digits during grasp, and concluded that this was due to misalignment of the finger during the grasp.
Bellew3 reported 10-year follow-up of 33 children (21 with symbrachydactyly) who had toe-to-hand transfers focusing on psychological outcomes. Children and their parents reported psychological well-being, satisfaction with the appearance of the transferred digit and the donor site, and positive reactions from others, and felt that the transferred digit served a functional role in daily activities.
Kaplan36 administered the Pediatric Outcome Data Collection Instrument (PODCI) to 15 children who had toe-to-hand transfers and found that scores for self-reports of upper extremity function and transfer/mobility, and parent reports of global function, upper extremity function, and sports/physical function, were lower than normative scores (they did not compare postoperative with preoperative scores). They also found that parents underestimated sports/physical function and happiness compared with the patient reports; this has been shown for other congenital conditions as well.58
Anatomical variation in vascular structures engenders concern about potential effect of these anomalies on the viability of the vascular anastomoses and survival of the transferred toe. A review of toe-to-hand transfers in congenital hand differences, however, found an average transplant survival rate of more than 96%.34 Other issues include unpredictable range of motion in the transferred digit; as some surgeons have noted, the vascularized toe transfer often results in a sensate post for prehension by another digit.24,48,64
Jones35 proposed a morphologic framework of indications for vascularized toe transfer for thumb and finger reconstruction in congenital conditions, including “complete absence of the thumb and all four fingers” and finger reconstruction when there is “absence of all four fingers but with normal thumb function,” which correspond to types IIIA and IVA symbrachydactyly. However, the indications for toe-to-hand transfers are still being established for unilateral symbrachydactyly. Creating opportunities for pinch and grip are important but should be weighed against the risks of surgery, and parental expectations must be aligned with realistic outcomes. Further research is needed to determine whether this operation improves function from baseline and to distinguish any postoperative functional changes from normal child development.
Future Directions
The advent of composite tissue transplantation has led to the reality of hand transplantation for adults with traumatic hand loss. There are many risks to this operation, including the long-term need for immunosuppressive medication; in addition, psychological counseling is imperative beforehand.14,37,54 These challenges, along with the uncertainty of growth potential, contraindicate this operation in children with unilateral hand conditions. Tissue engineering has the potential to address the challenge of limited tissue availability for reconstructing the congenitally malformed hand. Engineering de novo tendons or augmenting tendon regeneration has the potential to overcome the lack of suitable donor tendons for use in the hand.69 The creation of composite tissues could someday mean that patient-derived digits could be grown ex vivo and transplanted.31
Conclusion
Symbrachydactyly is an uncommon unilateral congenital malformation of the hand in which the fingers are variably hypoplastic. There is no well-accepted classification for symbrachydactyly that guides treatment and provides prognosis, although Foucher’s classification may prove useful. The clinical evaluation of the patient with symbrachydactyly should include a multidimensional analysis of the child’s functional abilities as well as the appearance of the hand. Thumb function, including prehension (pinch and grasp), is a priority for assessment and reconstruction.
Currently available surgical treatments of symbrachydactyly address hand structure by treating the individual components of the condition: web space contracture, unstable digits, short digits, and inability to pinch. Some surgeons have expanded the indications of free toe-to-hand transfer to provide children with symbrachydactyly with an additional sensate and variably mobile digit. However, given the high level of functioning of children with a unilateral congenital hand difference who have not undergone surgery, and the improved abilities that accrue with normal development, it has not yet been determined whether surgical treatment of this condition improves function and quality of life for the child.
Parents of infants with symbrachydactyly may underestimate their child’s potential and request complex procedures such as lengthening and toe-to-hand transfer because they hope that these will make their child’s hand “normal.” Surgery for this condition cannot achieve normal appearance; the pediatric hand surgeon must help parents reconcile their desires and expectations with their child’s potential, by discussing goals and expectations of surgery. Early functional assessments by a pediatric occupational therapist, and peer contacts with older children with similar conditions can help the parents accept their child’s condition and make informed decisions about surgery.
All interventions should prioritize realistic, evidence-supported appearance and functional gains. Studies of the baseline function and quality of life of children with symbrachydactyly would allow surgeons to better understand functional changes associated with various interventions and would help surgeons and parents to make the best treatment decisions.
Footnotes
Authors’ Note: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH).
Ethical Approval: Ethical approval for this study was waived by our institutional review board. There was no study of patients associated with this article.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through grant (UL1 TR000002) and linked award (TL1 TR000133).
References
- 1. Andersson GB, Gillberg C, Fernell E, Johansson M, Nachemson A. Children with surgically corrected hand deformities and upper limb deficiencies: self-concept and psychological well-being. J Hand Surg Eur Vol. 2011;36(9):795-801. [DOI] [PubMed] [Google Scholar]
- 2. Bavinck JN, Weaver DD. Subclavian artery supply disruption sequence: hypothesis of a vascular etiology for Poland, Klippel-Feil, and Möbius anomalies. Am J Med Genet. 1986;23(4):903-918. [DOI] [PubMed] [Google Scholar]
- 3. Bellew M, Haworth J, Kay SP. Toe to hand transfer in children: ten year follow up of psychological aspects. J Plast Reconstr Aesthet Surg. 2011;64(6):766-775. [DOI] [PubMed] [Google Scholar]
- 4. Blauth W, Gekeler J. [Morphology and classification of symbrachydactyly]. Handchirurgie. 1971;3(4):123-128. [PubMed] [Google Scholar]
- 5. Bouvet JP, Leveque D, Bernetieres F, Gros JJ. Vascular origin of Poland syndrome? a comparative rheographic study of the vascularisation of the arms in eight patients. Eur J Pediatr. 1978;128(1):17-26. [DOI] [PubMed] [Google Scholar]
- 6. Brown PW. Adduction—flexion contracture of the thumb: correction with dorsal rotation flap and release of contracture. Clin Orthop Relat Res. 1972;88:161-168. [DOI] [PubMed] [Google Scholar]
- 7. Buck-Gramcko D. The role of nonvascularized toe phalanx transplantation. Hand Clin. 1990;6(4):643-659. [PubMed] [Google Scholar]
- 8. Caroli A, Zanasi S. First web-space reconstruction by Caroli’s technique in congenital hand deformities with severe thumb ray adduction. Br J Plast Surg. 1989;42(6):653-659. [DOI] [PubMed] [Google Scholar]
- 9. Cavallo AV, Smith PJ, Morley S, Morsi AW. Non-vascularized free toe phalanx transfers in congenital hand deformities—the Great Ormond Street experience. J Hand Surg Br. 2003;28(6):520-527. [DOI] [PubMed] [Google Scholar]
- 10. Chang SM, Hou CL, Zhang F, Lineaweaver WC, Chen ZW, Gu YD. Distally based radial forearm flap with preservation of the radial artery: anatomic, experimental, and clinical studies. Microsurgery. 2003;23(4):328-337. [DOI] [PubMed] [Google Scholar]
- 11. Coombs CJ, Thomas DJ. The Manta Ray flap: a technique for first web space release. Tech Hand Up Extrem Surg. 2010;14(1):41-45. [DOI] [PubMed] [Google Scholar]
- 12. de Bree R, Hartley C, Smeele LE, Kuik DJ, Quak JJ, Leemans CR. Evaluation of donor site function and morbidity of the fasciocutaneous radial forearm flap. Laryngoscope. 2004;114(11):1973-1976. [DOI] [PubMed] [Google Scholar]
- 13. Ekblom AG, Laurell T, Arner M. Epidemiology of congenital upper limb anomalies in 562 children born in 1997 to 2007: a total population study from Stockholm, Sweden. J Hand Surg Br. 2010;35(11):1742-1754. [DOI] [PubMed] [Google Scholar]
- 14. Errico M, Metcalfe NH, Platt A. History and ethics of hand transplants. JRSM Short Rep. 2012;3(10):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fernandez-Teran M, Ros MA. The apical ectodermal ridge: morphological aspects and signaling pathways. Int J Dev Biol. 2008;52(7):857-871. [DOI] [PubMed] [Google Scholar]
- 16. Flatt AE. The Care of Congenital Hand Anomalies. St. Louis, MO: Quality Medical Publishing; 1994. [Google Scholar]
- 17. Flatt AE, Wood VE. Multiple dorsal rotation flaps from the hand for thumb web contractures. Plast Reconstr Surg. 1970;45(3):258-262. [DOI] [PubMed] [Google Scholar]
- 18. Foucher G, Medina J, Navarro R, Nagel D. Toe transfer in congenital hand malformations. J Reconstr Microsurg. 2001;17(1):1-8. [DOI] [PubMed] [Google Scholar]
- 19. Foucher G, Medina J, Pajardi G, Navarro R. [Classification and treatment of symbrachydactyly. A series of 117 cases]. Chir Main. 2000;19(3):161-168. [DOI] [PubMed] [Google Scholar]
- 20. Foucher G, Pajardi G, Lamas C, Medina J, Navarro R. [Progressive bone lengthening of the hand in congenital malformations. 41 cases]. Rev Chir Orthop Reparatrice Appar Mot. 2001;87(5):451-458. [PubMed] [Google Scholar]
- 21. Friedman R, Wood VE. The dorsal transposition flap for congenital contractures of the first web space: a 20-year experience. J Hand Surg Br. 1997;22(4):664-670. [DOI] [PubMed] [Google Scholar]
- 22. Garagnani L, Gibson M, Smith PJ, Smith GD. Long-term donor site morbidity after free nonvascularized toe phalangeal transfer. J Hand Surg Br. 2012;37(4):764-774. [DOI] [PubMed] [Google Scholar]
- 23. Gardiner DM, Holmes LB. Hypothesis: terminal transverse limb defects with “nubbins” represent a regenerative process during limb development in human fetuses. Birth Defects Res A Clin Mol Teratol. 2012;94(3):129-133. [DOI] [PubMed] [Google Scholar]
- 24. Gilbert A. Reconstruction of congenital hand defects with microvascular toe transfers. Hand Clin. 1985;1(2):351-360. [PubMed] [Google Scholar]
- 25. Goldberg NH, Watson HK. Composite toe (phalanx and epiphysis) transfers in the reconstruction of the aphalangic hand. J Hand Surg Br. 1982;7(5):454-459. [DOI] [PubMed] [Google Scholar]
- 26. Gulgonen A, Gudemez E. Reconstruction of the first web space in symbrachydactyly using the reverse radial forearm flap. J Hand Surg Am. 2007;32(2):162-167. [DOI] [PubMed] [Google Scholar]
- 27. Gupta A, Kay SP, Scheker LR. The Growing Hand: Diagnosis and Management of the Upper Extremity in Children. Mosby; Maryland Heights, MO: 2000. [Google Scholar]
- 28. Heo CY, Kwon S, Back GH, Chung MS. Complications of distraction lengthening in the hand. J Hand Surg Eur Vol. 2008;33(5):609-615. [DOI] [PubMed] [Google Scholar]
- 29. Hulsbergen-Kruger S, Preisser P, Partecke BD. Ilizarov distraction-lengthening in congenital anomalies of the upper limb. J Hand Surg Br. 1998;23(2):192-195. [DOI] [PubMed] [Google Scholar]
- 30. International Federation of Societies for Surgery of the Hand. IFSSH scientific committee on congenital conditions. J Hand Surg Eur Vol. 2014;39(6):676-678. [DOI] [PubMed] [Google Scholar]
- 31. Isogai N, Landis W, Kim TH, Gerstenfeld LC, Upton J, Vacanti JP. Formation of phalanges and small joints by tissue-engineering. J Bone Joint Surg Am. 1999;81(3):306-316. [DOI] [PubMed] [Google Scholar]
- 32. James MA, Bagley AM, Brasington K, Lutz C, McConnell S, Molitor F. Impact of prostheses on function and quality of life for children with unilateral congenital below-the-elbow deficiency. J Bone Joint Surg Am. 2006;88(11):2356-2365. [DOI] [PubMed] [Google Scholar]
- 33. James MA, Durkin RC. Nonvascularized toe proximal phalanx transfers in the treatment of aphalangia. Hand Clin. 1998;14(1):1-15. [PubMed] [Google Scholar]
- 34. Jones NF, Hansen SL, Bates SJ. Toe-to-hand transfers for congenital anomalies of the hand. Hand Clin. 2007;23(1):129-136. [DOI] [PubMed] [Google Scholar]
- 35. Jones NF, Kaplan J. Indications for microsurgical reconstruction of congenital hand anomalies by toe-to-hand transfers. Hand. 2013;8(4):367-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kaplan JD, Jones NF. Outcome measures of microsurgical toe transfers for reconstruction of congenital and traumatic hand anomalies. J Pediatr Orthop. 2014;34(3):362-368. [DOI] [PubMed] [Google Scholar]
- 37. Klapheke MM, Marcell C, Taliaferro G, Creamer B. Psychiatric assessment of candidates for hand transplantation. Microsurgery. 2000;20(8):453-457. [DOI] [PubMed] [Google Scholar]
- 38. Knight JB, Pritsch T, Ezaki M, Oishi SN. Unilateral congenital terminal finger absences: a condition that differs from symbrachydactyly. J Hand Surg Br. 2012;37(1):124-129. [DOI] [PubMed] [Google Scholar]
- 39. Lake A. Hand therapy for children with congenital hand differences. Tech Hand Up Extrem Surg. 2010;14(2):78-84. [DOI] [PubMed] [Google Scholar]
- 40. Lister G. Microsurgical transfer of the second toe for congenital deficiency of the thumb. Plast Reconstr Surg. 1988;82(4):658-665. [DOI] [PubMed] [Google Scholar]
- 41. Manske PR. Symbrachydactyly instead of atypical cleft hand. Plast Reconstr Surg. 1993;91(1):196. [DOI] [PubMed] [Google Scholar]
- 42. Matev IB. Thumb reconstruction in children through metacarpal lengthening. Plast Reconstr Surg. 1979;64(5):665-669. [PubMed] [Google Scholar]
- 43. Matsuno T, Ishida O, Sunagawa T, Ichikawa M, Ikuta Y, Ochi M. Bone lengthening for congenital differences of the hands and digits in children. J Hand Surg Br. 2004;29(4):712-719. [DOI] [PubMed] [Google Scholar]
- 44. McConachie H, Colver A, Forsyth R, Jarvis SN, Parkinson KN. Participation of disabled children: how should it be characterised and measured? Disabil Rehabil. 2006;28(18):1157-1164. [DOI] [PubMed] [Google Scholar]
- 45. Miyawaki T, Masuzawa G, Hirakawa M, Kurihara K. Bone-lengthening for symbrachydactyly of the hand with the technique of callus distraction. J Bone Joint Surg Am. 2002;84-A(6):986-991. [DOI] [PubMed] [Google Scholar]
- 46. Moola F, Faulkner G, White L, Kirsh JA. The psychological and social impact of camp for children with chronic illnesses: a systematic review update. Child Care Health Dev. 2013;40:615-361. [DOI] [PubMed] [Google Scholar]
- 47. Müller W. Die angeborenen Fehlbildungen der menschlichen Hand: Erb-und Konstitutionsbiologie der Hand. Thieme; New York, NY: 1937. [Google Scholar]
- 48. O’Brien BM, Black MJ, Morrison WA, MacLeod AM. Microvascular great toe transfer for congenital absence of the thumb. Hand. 1978;10(2):113-124. [DOI] [PubMed] [Google Scholar]
- 49. Odar C, Canter KS, Roberts MC. Relationship between camp attendance and self-perceptions in children with chronic health conditions: a meta-analysis. J Pediatr Psychol. 2013;38(4):398-411. [DOI] [PubMed] [Google Scholar]
- 50. Patterson RW, Seitz WH., Jr. Nonvascularized toe phalangeal transfer and distraction lengthening for symbrachydactyly. J Hand Surg Am. 2010;35(4):652-658. [DOI] [PubMed] [Google Scholar]
- 51. Poland A. Deficiency of the pectoral muscles. Guys Hosp Rep. 1841;6:191. [Google Scholar]
- 52. Radocha RF, Netscher D, Kleinert HE. Toe phalangeal grafts in congenital hand anomalies. J Hand Surg Am. 1993;18(5):833-841. [DOI] [PubMed] [Google Scholar]
- 53. Richardson PW, Johnstone BR, Coombs CJ. Toe-to-hand transfer in symbrachydactyly. Hand Surg. 2004;9(1):11-18. [DOI] [PubMed] [Google Scholar]
- 54. Sarhane KA, Tuffaha SH, Broyles JM, et al. A critical analysis of rejection in vascularized composite allotransplantation: clinical, cellular and molecular aspects, current challenges, and novel concepts. Front Immunol. 2013;4:406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Savarese JJ, III, Brinken BW, Zaleske DJ. Epiphyseal replacement in a murine model. J Pediatr Orthop. 1995;15(5):682-690. [DOI] [PubMed] [Google Scholar]
- 56. Schenker M, Wiberg M, Kay SP, Johansson RS. Precision grip function after free toe transfer in children with hypoplastic digits. J Plast Reconstr Aesthet Surg. 2007;60(1):13-23. [DOI] [PubMed] [Google Scholar]
- 57. Seitz WH, Jr, Shimko P, Patterson RW. Long-term results of callus distraction-lengthening in the hand and upper extremity for traumatic and congenital skeletal deficiencies. J Bone Joint Surg Am. 2010;92(suppl 2):47-58. [DOI] [PubMed] [Google Scholar]
- 58. Sheffler LC, Hanley C, Bagley A, Molitor F, James MA. Comparison of self-reports and parent proxy-reports of function and quality of life of children with below-the-elbow deficiency. J Bone Joint Surg Am. 2009;91(12):2852-2859. [DOI] [PubMed] [Google Scholar]
- 59. Simeonsson RJ, Leonardi M, Lollar D, Bjorck-Akesson E, Hollenweger J, Martinuzzi A. Applying the International Classification of Functioning, Disability and Health (ICF) to measure childhood disability. Disabil Rehabil. 2003;25(11-12):602-610. [DOI] [PubMed] [Google Scholar]
- 60. Summerbell D. A quantitative analysis of the effect of excision of the AER from the chick limb-bud. J Embryol Exp Morphol. 1974;32(3):651-660. [PubMed] [Google Scholar]
- 61. Swanson AB. A classification for congenital limb malformations. J Hand Surg Am. 1976;1(1):8-22. [DOI] [PubMed] [Google Scholar]
- 62. Tonkin M, Deva A, Filan S. Long term follow-up of composite non-vascularized toe phalanx transfers for aphalangia. J Hand Surg Br. 2005;30(5):452-458. [DOI] [PubMed] [Google Scholar]
- 63. Tonkin MA, Tolerton SK, Quick TJ, et al. Classification of congenital anomalies of the hand and upper limb: development and assessment of a new system. J Hand Surg Am. 2013;38(9):1845-1853. [DOI] [PubMed] [Google Scholar]
- 64. Vilkki SK. Advances in microsurgical reconstruction of the congenitally adactylous hand. Clin Orthop Relat Res. 1995(314):45-58. [PubMed] [Google Scholar]
- 65. Waters PM, Bae DS. Pediatric Hand and Upper Limb Surgery: A Practical Guide. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 66. Winkel A, Stricker S, Tylzanowski P, et al. Wnt-ligand-dependent interaction of TAK1 (TGF-beta-activated kinase-1) with the receptor tyrosine kinase Ror2 modulates canonical Wnt-signalling. Cell Signal. 2008;20(11):2134-2144. [DOI] [PubMed] [Google Scholar]
- 67. World Health Organization. ICIDH-2: International Classification of Functioning, Disability and Health: Final Draft, Full Version. Geneva, Switzerland: Classification, Assessment, Surveys and Terminology Team, World Health Organization; 2001. [Google Scholar]
- 68. Yamauchi Y, Tanabu S. Symbrachydactyly. In: Congenital Malformations of the Hand and Forearm. Buck-Gramcko D. (ed). London, England: Churchill Livingstone; 1998:149-158. [Google Scholar]
- 69. Zhang AY, Chang J. Tissue engineering of flexor tendons. Clin Plast Surg. 2003;30(4):565-572. [DOI] [PubMed] [Google Scholar]