Abstract
Background: The etiology of multifocal osteonecrosis is not definitively known; however, hypercoagulable state is a very plausible cause. Methods: We present an unusual case of a 12-year-old boy with a history of Legg-Calve-Perthes disease presenting with right wrist pain who was subsequently diagnosed with Kienbock’s disease. The finding of multifocal osteonecrosis prompted testing for a hypercoagulable state that was positive for Factor V Leiden thrombophilia. A thorough literature review using Medline database was conducted to investigate associations between inherited hypercoagulable states and multifocal osteonecrosis. Results: Our literature review identified 2 similar cases of multifocal osteonecrosis associated with a hypercoagulable disorder in adult patients. There were no reports among the pediatric patient population. Meta-analysis has demonstrated a potential link between Legg-Calve-Perthes disease and Factor V Leiden thrombophilia. Conclusions: This study offers further evidence to support the theory that multifocal osteonecrosis may be linked to a hypercoagulable state. Patients presenting with multifocal osteonecrosis should undergo screening for hypercoagulable states. Further investigation is needed to ascertain the potential benefit of prophylactic anticoagulation in patients with a known hypercoagulable state and multifocal osteonecrosis.
Keywords: Factor V Leiden, Kienbock’s, Legg-Calve-Perthes disease, avascular necrosis, lunate
Introduction
The genetic and environmental variables that predispose to atraumatic osteonecrosis of bone are poorly understood. Hypercoagulable states have been hypothesized to be a contributing factor in the development of osteonecrosis due to the implicated effects on vascular thrombosis and impaired blood flow to bone.2 There have been conflicting reports in the literature regarding the association between osteonecrosis and thrombophilias. Several studies have linked osteonecrosis to hypercoagulable states including Factor V Leiden thrombophilia.1,3,5,12 Other studies have failed to find any correlation between hypercoagulable states and the development of osteonecrosis.10,11,13,14 Here we present a case of an 18-year-old boy with attention deficit hyperactivity disorder (ADHD) and Asperger syndrome, who developed bilateral Legg-Calve-Perthes disease and Kienbock’s disease (avascular necrosis of the lunate) of the right wrist. The finding of multifocal osteonecrosis prompted testing for hypercoagulability that revealed Factor V Leiden thrombophilia.
Case Presentation
At first encounter with our service, a 12-year-old obese, white male presented for the complaint of right wrist pain. A brief overview of the patient’s past medical history included a diagnosis of ADHD and Asperger syndrome and obesity secondary to the limitations of his bilateral Legg-Calve-Perthes disease. The patient lived with his grandparents. His mother had severe diabetes and died 9 months after he was born and his father died 3 years ago from a bone malignancy. According to the patient’s grandparents, the father walked with a limp but the cause was never investigated. There was no known family history of deep vein thrombosis, pulmonary embolism, or other blood clotting disorders. The patient had taken Memantine in the past for his ADHD; his current medications included Tylenol and Ibuprofen as needed for pain. He underwent a sleep study several months ago that did not reveal any evidence of sleep apnea. Informed consent was obtained from the patient to be included in this study.
The patient was first evaluated for problems related to osteonecrosis at the age of 4 when he presented with complaints of intermittent pain in his left hip and an associated limp. The patient was generally healthy with no history of trauma to his hip. On physical examination he had an antalgic gait and pain with internal rotation of the left hip. Radiographs that included anterior-posterior and frog views of the pelvis showed both hips to be symmetric with no obvious pathology; however, subsequent magnetic resonance imaging revealed asymmetry of the hips and changes consistent with Legg-Calve-Perthes disease of the left hip. He was treated with traction and a physical therapy program aimed at improving range of motion.
Four years after being diagnosed with Legg-Calve-Perthes of the left hip, the patient presented to the clinic at the age of 8 with new complaints of right hip and thigh pain. There was again no history of trauma or other obvious risk factors for the development of hip osteonecrosis aside from his previous diagnosis of Legg-Calve-Perthes disease. Radiographs of both hips revealed preexisting left-sided Legg-Calve-Perthes disease with a bilobed femoral head and a very short flat epiphysis. His right hip showed signs of early Legg-Calve-Perthes disease that included sclerosis and flattening of the femoral head. The patient was followed for a period of 1 year, during which time his right hip pain worsened significantly and his range of motion continued to decrease. Due to the degree of degeneration and symptoms, a right hip valgus osteotomy with adductor tenotomy was performed. Following the surgery, he had improvement in pain symptoms, but continued to walk with a limp. There was persistent right hip pain, which was addressed with a hardware removal at 9 months postoperatively. Subsequently, the patient was pain free, but with a persistent limp. During this period, he was able to participate in physical education classes at school and has joined the school wrestling team.
At age 12 at a routine follow-up of his bilateral Legg-Calve-Perthes disease, the patient reported persistent pain and clicking in his right wrist after falling onto his outstretched hand. He did not have any pain immediately after the fall; the pain began a few weeks after his fall and progressively worsened over a period of 8 weeks. The patient is right-hand dominant and the pain significantly impaired activities at school, such as writing and using the computer. On physical exam, there was tenderness over the lunate and increased pain with grip. Wrist radiographs demonstrated loss of lunate height and sclerosis without carpal collapse relative to the left wrist (Figure 1). The patient underwent a revascularization procedure to address the osteonecrosis and collapse of the lunate, which involved debridement of necrotic portions of the lunate and vascularized bone graft inset. One-year follow-up radiographs demonstrate restoration in lunate height (Figure 2).
Figure 1.
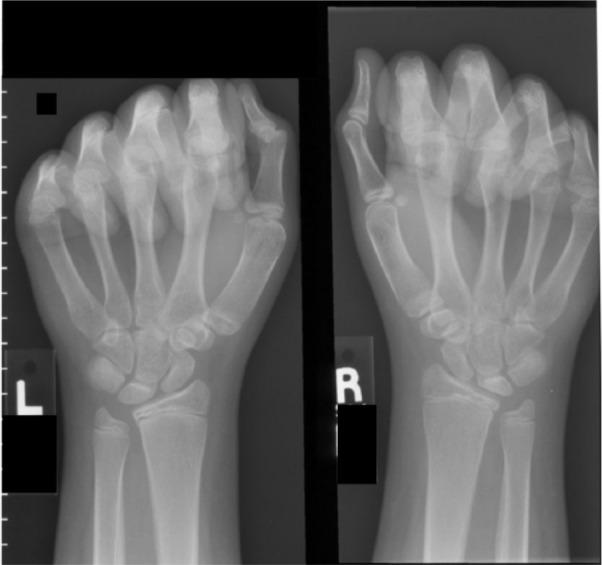
Bilateral wrist radiographs demonstrate right lunate sclerosis and proximal flattening consistent with Stage 3A Kienbock’s disease on the right.
Figure 2.

Radiographs reveal a stable lunate at 1 year postoperatively with no evidence of ongoing collapse.
After the diagnosis of Kienbock’s disease was made, a hypercoagulability workup was performed to look for abnormalities that might be contributing to the development of osteonecrosis. Studies were performed to assess for multiple hypercoagulable states including abnormalities of protein C and S, hyperhomocysteinemia, antithrombin III deficiency, factor II abnormalities, and Factor V Leiden thrombophilia. Genetic testing revealed that he was a carrier of an F5 gene mutation, consistent with Factor V Leiden thrombophilia. He was started on a daily aspirin for prophylaxis against future episodes of osteonecrosis. Anticoagulation therapy with warfarin was considered but was decided against due to a lack of evidence supporting its use for this indication, its associated risk of bleeding, and need for close follow-up.
The patient is now 6 years following the vascularized bone graft procedure and continues to do well in regard to wrist motion. Overall wrist motion on the effected side is 70° of flexion and 40° of extension compared with 70° of flexion and 50° of flexion on the contralateral side. Grip strength (as measured by the Jamometer) is 24 kg on the right and 29 kg on the left. Radiographs reveal a stable lunate with excellent maintenance of lunate height (Figure 3). Pain is improved with a VAS of 0 at rest but can rise to a 2 with strenuous activities. The patient does not take medication to control wrist pain and has returned to normal activities with the upper extremity. His bilateral hip pain has persisted and worsened, for which a plan has been made to proceed with bilateral total hip arthroplasties.
Figure 3.

AP radiographs of left (unaffected) and right (affected) wrist. Radiographs reveal a stable lunate in the right wrist 6 years following surgery. Notice improvement in lunate height when compared to 1 year postoperative image in Figure 2.
Discussion
Kienbock’s disease and Legg-Calve-Perthes disease are both rare disorders. The incidence of Legg-Calve-Perthes disease varies geographically and has its highest reported incidence in Ireland with an incidence of 1 per 607 children.6 Bilateral disease is significantly less common than unilateral disease accounting for about 10% of total cases.7 Kienbock’s disease is extremely uncommon in the pediatric population, and its true incidence is unknown.1,4,8 The presence of bilateral Legg-Calve-Perthes disease and Kienbock’s disease in our patient suggests an intrinsic predisposition to multifocal osteonecrosis. Factor V Leiden thrombophilia may be a contributing factor to this predisposition. While a clear association has yet to be reported in any large series, a recently case of bilateral Kienbock’s disease, bilateral Legg-Calve-Perthes disease and a history of transient ischemic attack in a 35 year old male, has been reported.14
In a case report published by Rostom et al, a 50-year-old female with antiphospholipid antibody syndrome developed bilateral osteonecrosis of the hips and lunate.2 This unusual presentation of multifocal osteonecrosis is similar to what was seen in our patient with Factor V Leiden thrombophilia. The fact that osteonecrosis occurred at similar anatomical locations may indicate that a common mechanism of pathogenesis is at work, with hypercoagulability being an important factor in the development of multifocal disease.
The risk of venous thrombotoembolism (VTE) is an important consideration among patients with a known hypercoagulable state. Gomez-Puerta and colleagues recently reviewed a series of patient with multifocal osteonecrosis and found that 48% had a detectable coagulation abnormality.7 Of these patients, 28% had a VTE (similar to the general population), compared with 60% in the multifocal osteonecrosis group lacking a hypercoagulable state. However, Factor V Leiden was the most common hypercoagulable state among patients who had a VTE. These findings do not suggest that patients with multifocal osteonecrosis and hypercoagulability are necessarily at an increased risk of VTE and further longitudinal studies are warranted to better delineate the presence of this risk.
The lunate has been considered to be a bone “at risk” due the anatomy of its vascular supply. Previous vascular studies by Gelbermann found that 12% of lunates had a single site of arterial inflow, potentially placing it at higher risk of injury and subsequent vascular compromise.13 Other theories of the etiology of Kienbock’s disease have focused on mechanical predisposition to repetitive injury. However, surgical techniques which have attempted to restore lunate blood flow following the development of Kienbock’s disease have been shown to be very successful at relieving pain and preventing progression of disease.9,10,12
To date there have been few studies specifically looking at the association between multifocal osteonecrosis and hypercoagulable states. A recent meta-analysis has demonstrated that the Factor V Leiden mutation is significantly related to Perthes disease.15 A case series of 26 patients also suggested that thrombophilia was associated with both idiopathic multifocal osteonecrosis and secondary multifocal osteonecrosis, as was the eNOS T-786C polymorphism.6 The current case report also indicates that hypercoagulability may play a prominent role in the development of multifocal osteonecrosis. Further research is needed to determine the role of hypercoagulability in the development of osteonecrosis. If a clear association with multifocal osteonecrosis is found, then there may be a role for routine screening of patients with a single episode of osteonecrosis to determine those at higher risk of development of subsequent episodes of osteonecrosis. Those who are identified to be at high risk may benefit from long-term prophylactic anticoagulation with medications such as aspirin, or warfarin.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ando Y, Yasuda M, Kazuki K, Hidaka N, Yoshinaka Y. Temporary scaphotrapezoidal joint fixation for adolescent Kienbock’s disease. J Hand Surg Am. 2009;34(1):14-19. [DOI] [PubMed] [Google Scholar]
- 2. Balasa VV, Gruppo RA, Glueck CJ, et al. Legg-Calve-Perthes disease and thrombophilia. J Bone Joint Surg Am. 2004;86-A(12):2642-2647. [DOI] [PubMed] [Google Scholar]
- 3. Chang JD, Hur M, Lee SS, Yoo JH, Lee KM. Genetic background of nontraumatic osteonecrosis of the femoral head in the Korean population. Clin Orthop Relat Res. 2008;466(5):1041-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. De Smet L. Kienbock’s disease in a 12-year-old girl. Acta Orthop Belg. 2003;69(4):361-362. [PubMed] [Google Scholar]
- 5. Gallistl S, Reitinger T, Linhart W, Muntean W. The role of inherited thrombotic disorders in the etiology of Legg-Calve-Perthes disease. J Pediatr Orthop. 1999;19(1):82-83. [PubMed] [Google Scholar]
- 6. Glueck CJ, Freiberg RA, Boppana S, Wang P. Thrombophilia, hypofibrinolysis, the eNOS T-786C polymorphism, and multifocal osteonecrosis. J Bone Joint Surg Am. 2008;90(10):2220-2229. [DOI] [PubMed] [Google Scholar]
- 7. Gómez-Puerta JA, Peris P, Reverter JC, et al. High prevalence of prothrombotic abnormalities in multifocal osteonecrosis: description of a series and review of the literature. Medicine (Baltimore). 2013;92(6):295-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Irisarri C, Kalb K, Ribak S. Infantile and juvenile lunatomalacia. J Hand Surg Eur Vol. 2010;35(7):544-548. [DOI] [PubMed] [Google Scholar]
- 9. Moran SL, Cooney WP, Berger RA, Bishop AT, Shin AY. The use of the 4 + 5 extensor compartmental vascularized bone graft for the treatment of Kienbock’s disease. J Hand Surg Am. 2005;30(1):50-58. [DOI] [PubMed] [Google Scholar]
- 10. Moran SL, Shin AY. Vascularized bone grafting for the treatment of carpal pathology. Orthop Clin North Am. 2007;38(1):73-85, vi. [DOI] [PubMed] [Google Scholar]
- 11. Rosendorff A, Dorfman DM. Activated protein C resistance and factor V Leiden: a review. Arch Pathol Lab Med. 2007;131(6):866-871. [DOI] [PubMed] [Google Scholar]
- 12. Simmons SP, Tobias B, Lichtman DM. Lunate revascularization with artery implantation and bone grafting. J Hand Surg Am. 2009;34(1):155-160. [DOI] [PubMed] [Google Scholar]
- 13. Williams CS, Gelberman RH. Vascularity of the lunate. Anatomic studies and implications for the development of osteonecrosis. Hand Clin. 1993;9(3):391-398. [PubMed] [Google Scholar]
- 14. Wollstein A, Tantawi D, Wollstein R. Bilateral Kienbock’s disease concomitant with bilateral Legg-Calve-Perthes disease: a case report. Hand. 2013;8(1):120-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Woratanarat P, Thaveeratitharm C, Woratanarat T, Angsanuntsukh C, Attia J, Thakkinstian A. Meta-analysis of hypercoagulability genetic polymorphisms in Perthes disease. J Orthop Res. 2014;32(1):1-7. [DOI] [PubMed] [Google Scholar]


