Abstract
Background: Approximately 33% of Americans have inadequate health literacy, which is associated with infrequent use of preventative services, increased hospitalization and use of emergency care, and worse control of chronic diseases. In this study, the Literacy in Musculoskeletal Problems (LiMP) questionnaire was used to evaluate the prevalence of limited musculoskeletal literacy in patients undergoing carpal tunnel release (CTR), as these individuals may be at increased risk of inferior outcomes. Methods: This cross-sectional study included individuals older than or equal to 18 years of age who were scheduled for elective CTR. Participants completed a demographic survey and the LiMP questionnaire during their preoperative office visit. The prevalence of limited health literacy was determined, with chi-square analysis used to determine the influence of demographic parameters. Results: The mean LiMP score was 6 ± 1.40. Limited musculoskeletal literacy was seen in 34% of participants (22/65). Analysis identified race (Caucasian), gender (female), higher education levels (≥college), current or prior employment in a health care field, and a prior physician visit for a non–carpal tunnel musculoskeletal complaint as being associated with higher literacy rates. Conclusions: Approximately one-third of patients scheduled for elective CTR have limited musculoskeletal literacy and may lack the necessary skills required for making informed decisions regarding their care. This is concerning, as CTR is performed in the United States on roughly 500 000 individuals annually, at an estimated cost of 2 billion dollars. The identification of those most at risk is thus crucial, and will facilitate the development of education campaigns and interventions geared toward those who are most vulnerable.
Keywords: health literacy, musculoskeletal health literacy, carpal tunnel syndrome, Literacy in Musculoskeletal Problems Survey, LiMP Survey
Introduction
Health literacy is a measure of an individual’s ability to obtain, process, and understand basic health information and services needed to make appropriate health decisions and is the most important predictor of one’s health status.3,11,19,33 Those with inadequate health literacy are more frequently associated with decreased medical knowledge, infrequent use of preventative services, increased hospitalization and use of emergency care, worse control of chronic diseases, and bad disease outcomes.11,19,33 Conversely, patients with adequate health literacy experience more effective and meaningful interactions with their physicians and are better equipped to make informed and appropriate treatment decisions.5,25
In the United States, studies of health literacy have estimated that between 33% and 48% of Americans possess inadequate health literacy.2,8,15,24 This is troubling, as the annual cost of low health literacy is estimated to range from $106 to $238 billion.31 This represents an amount equal to the cost of insuring each of the more than 47 million Americans who lacked health insurance in 2006.31
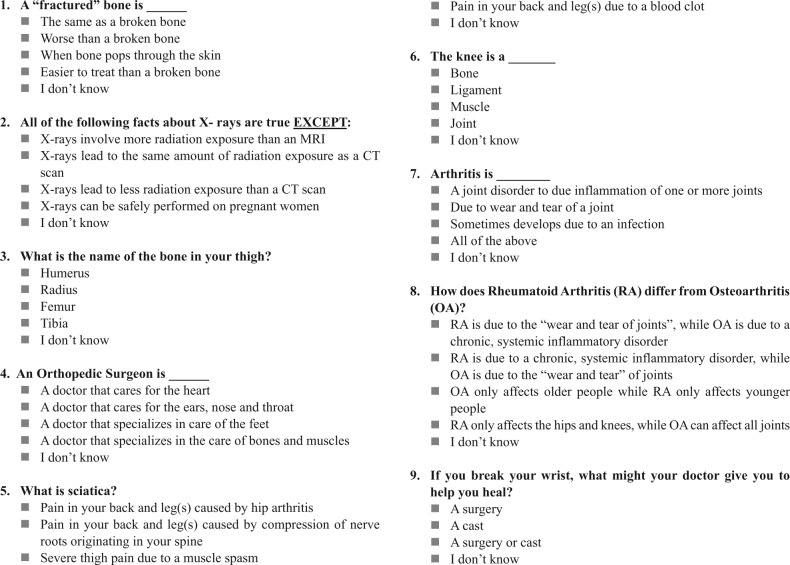
Although a wide variety of established tools for assessing general health literacy are available, few are specific to particular medical specialties or disease processes.4,7,9,21,23,34 As such, we developed and validated the Literacy in Musculoskeletal Problems (LiMP) questionnaire, a 9-question survey that evaluates patients’ knowledge of musculoskeletal anatomy and terminology, as well as their familiarity with various diagnostic tools and treatment modalities for some of the more common musculoskeletal conditions (Figure 1).18,27
Figure 1.
The LiMP questionnaire.
Note. Questions 3, 4, and 6 assess each patient’s knowledge of anatomy and terminology. Questions 1, 5, 7, and 8 evaluate each patient’s familiarity with musculoskeletal conditions. And questions 2 and 9 measure each patient’s understanding of diagnostic tests and treatment modalities.
LiMP, Literacy in Musculoskeletal Problems.
In this study, the LiMP questionnaire was used to evaluate the prevalence of limited musculoskeletal health literacy in patients undergoing elective carpal tunnel release (CTR), which is performed more than 500 000 times annually in the United States at an estimated cost of 2 billion dollars.17 Given the significant health consequences and economic impact of carpal tunnel syndrome (CTS), it is crucial that we identify afflicted individuals who also possess limited musculoskeletal literacy, as they may be susceptible to inferior outcomes and a more complicated recovery following surgery.8
Materials and Methods
Setting and Study Sample
This cross-sectional study was approved by the Institutional Review Board of our medical center. A convenience sample of 65 English-speaking adults (18 years of age or older) was obtained from our institution’s orthopedic surgery outpatient practice. Inclusion was limited to patients presenting for their routine presurgical office visit prior to elective, primary CTR. Patients were excluded if they did not meet the aforementioned criteria, if they had any cognitive impairment, were unable to read English, or unable sign their own consent.
Research assistants approached patients once they were brought into examination rooms, asking them if they would like to participate in the study. Research staff then informed patients of the purpose of the study, and the risks and benefits of participation. It was emphasized that participation was both voluntary and in no way related to the care they would receive. It was further explained that all results of the survey were anonymous. More than 90% of the patients approached were amenable to participation and provided written consent for participation.
Data Collection and Literacy Assessment
Participants first completed a 5-minute demographic questionnaire, in which they were asked to identify their age, sex, race, highest level of education, whether or not they had ever worked in a health care field before, and whether or not they had been seen in the past by a physician for a musculoskeletal complaint. The validated, 9-question, self-administered LiMP questionnaire was then given to participants, which took 5 to 7 minutes to complete. The LiMP scores ranged from 0 to 9, with scores more than or equal to 6 indicative of adequate musculoskeletal health literacy. This cutoff was determined in an earlier work, in which the LiMP survey was validated based on the techniques described by Pendlimari et al.25,27
Statistics
Performance on the LiMP survey was evaluated as a function of the mean score and the prevalence of adequate and inadequate musculoskeletal literacy among participants. A chi-square analysis was performed to assess whether demographic parameters significantly correlated with categorical outcome variables (limited or adequate musculoskeletal health literacy). P values less than .05 were considered significant.
Results
A total of 65 participants completed both the demographic and LiMP surveys. Table 1 summarizes the demographic characteristics of the study participants. Participants were predominantly Caucasian (94%), female (62%), and had some college education (74%). In addition, 69% reported that they had been seen in the past for a non–carpal tunnel related musculoskeletal complaint. Less than one-third of the participants were either currently or previously employed in the health care industry (29%).
Table 1.
Demographic Information of Study Participants.
| Demographics | % |
|---|---|
| Mean age (years) | 60.2 |
| Gender | |
| Male | 38 |
| Female | 62 |
| Race | |
| Caucasian | 94 |
| African American | 6 |
| Other | 0 |
| Education | |
| ≥College | 73 |
| ≤College | 27 |
| Health care employee/profession (currently or previously) | |
| Yes | 29 |
| Prior physician visit for musculoskeletal complaint | |
| Yes | 69 |
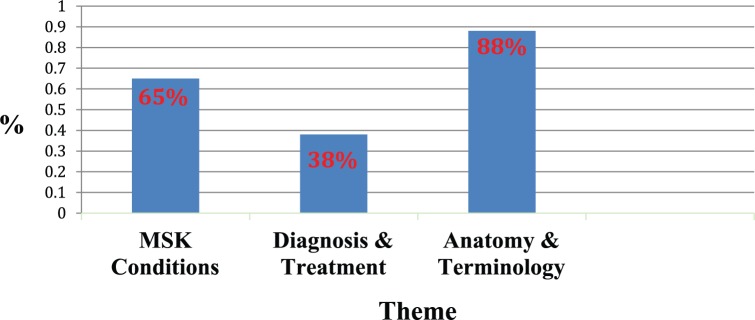
The mean LiMP score was 6 ± 1.4. The prevalence of inadequate musculoskeletal literacy among participants was 34% (22/65). The theme assessed by each question as well as the percentage of respondents who answered each question correctly is displayed in Table 2. The percentage of correct responses for each LiMP assessed musculoskeletal theme is depicted in Figure 2. There was no significant correlation between the prevalence of adequate musculoskeletal health literacy and participants’ gender, race, level of education, or history of health care employment (P > .05; Table 3). However, females, Caucasians, participants with a level of education more than or equal to college, and those with a current or prior occupation in health care experienced higher rates of adequate musculoskeletal literacy, as compared with the other study participants. A significant correlation between literacy and demographics was only demonstrated between those individuals who had previously seen a physician for a musculoskeletal complaint, as they were significantly more likely to possess adequate musculoskeletal literacy (P = .0001; Table 3).
Table 2.
A Listing of Each Question, Corresponding Theme, and Percentage of Respondents Who Answered It Correctly.
| Question | Theme |
|---|---|
| 1 | MSK conditions |
| 2 | Diagnosis and treatment |
| 3 | Anatomy and terminology |
| 4 | Anatomy and terminology |
| 5 | MSK conditions |
| 6 | Anatomy and terminology |
| 7 | MSK conditions |
| 8 | MSK conditions |
| 9 | Diagnosis and treatment |
Note. MSK, musculoskeletal.
Figure 2.
Theme-based breakdown of participants’ correct responses on the LiMP survey.
Note. MSK, musculoskeletal; LiMP, Literacy in Musculoskeletal Problems.
Table 3.
The Rates of Adequate Musculoskeletal Health Literacy Among Subjects as a Function of Demographic Characteristics.
| Percentage with adequate literacy (%) | |
|---|---|
| Gender | |
| Male | 60 |
| Female | 70 |
| Race | |
| Caucasian | 68 |
| African American | 50 |
| Other | N/A |
| Education | |
| ≥College | 70 |
| <College | 58 |
| Health care employee/profession (currently or previously) | |
| Yes | 85 |
| No | 58 |
| Prior physician visit for the musculoskeletal complaint | |
| Yes | 80 |
| No | 35 |
Note. Those values highlighted in green represent demographic characteristics associated with statistically significant (P < .05) differences in literacy.
Discussion
CTS is the most common compressive neuropathy of the upper extremity, with an incidence of 3.46 cases per 100 000 individuals.20 CTR, which is required in an estimated 43% to 71% of patients with CTS, is performed over 500 000 times a year, at a cost of approximately 2 billion dollars.1,22,28 Although the reported success rates of CTR have ranged from 70% to greater than 90%, patient selection remains important as complications do occur.16,22 Factors that have been shown to correlate with suboptimal outcomes include poor scores on patient-reported measures of upper extremity function and mental health status, pending legal action, and excessive alcohol intake.13
Health literacy in patients with CTS has never been assessed. This is problematic, as it is only with adequate health literacy that patients can truly make informed decisions regarding their care.5,25 Furthermore, patients with limited health literacy have been shown to experience inferior outcomes with regard to their given conditions.11,19,33 This was the impetus for our investigation into the prevalence of and factors related to inadequate health literacy in patients undergoing elective CTR, as the identification of such patients will enable orthopedic surgeons to identify this subset of at-risk individuals.
Determining those at risk of limited health literacy can be challenging. In a study by Kelly and Haidet, physicians were found to overestimate health literacy in 54% of African Americans, 11% of Caucasians, and 36% of other races/ethnicities.14 Further complicating this is the lack of specialty-specific assessment tools available, as those instruments currently used have been designed to assess general health literacy and are not applicable to all clinical situations.4,7,9,21,23,34
The LiMP questionnaire was therefore developed to aide clinicians in accurately evaluating musculoskeletal health literacy. The questionnaire is based on the most commonly emphasized themes within the internet-based patient education materials produced by the American Academy of Orthopaedic Surgeons (AAOS). Knowledge of anatomy and terminology, musculoskeletal conditions, and diagnosis and treatment are assessed in the LiMP survey’s 9 multiple-choice questions, which are written at a Flesch-Kincaid grade level of 4.2. This is important, as health care organizations such as the National Work Group on Cancer and Health, American Medical Association, and National Institutes of Health recommend the readability of patient education material to be no higher than sixth-grade level.27,33
In this investigation, the prevalence of inadequate musculoskeletal literacy was 34%. This is consistent with the lower end of national estimates of limited general health literacy and greater than that seen in other specialty-specific literacy studies related to diabetes and heart disease, which found 15.1% and 17.5% of afflicted patients to have low health literacy, respectively.2,8,10,15,24,26 Admittedly, we believe that the actual rate of limited musculoskeletal literacy may be even higher, as the participants in our study were predominantly Caucasians and had received at least part of a college education (Table 1). Several studies have identified increased rates of adequate health literacy in such individuals, supporting our findings.12,29
There was a significantly higher proportion of adequate musculoskeletal literacy observed in those participants who had previously seen a physician for an orthopedic related problem. This is consistent with the added familiarity one would presumably have with the musculoskeletal system and orthopedic conditions after such an interaction.
This study has several limitations. As a cross-sectional study utilizing a convenience sample, patients were not randomly selected. Response bias could have also occurred, as some patients may have been reluctant to truthfully answer questions regarding educational background, despite being informed of the confidentiality of their responses. If only those patients who were confident in their baseline musculoskeletal knowledge agreed to participate, volunteer bias could have also occurred. Although this could have led to an underestimation of the actual rates of inadequate musculoskeletal literacy, our greater than 90% participation rate makes such bias unlikely.
Our study suggests that approximately one-third of patients scheduled for elective CTR may lack the necessary skills required for making informed decisions regarding their care. In addition, these patients may be at risk of suboptimal outcomes, as poor health literacy has also been found to correlate with this.
Although patient education materials are widely available for patients with CTS through the AAOS and American Society of Surgery of the Hand websites, it has been shown that the readability of these materials may be too difficult for many to comprehend.32 It is therefore essential that revised education campaigns be developed and geared toward those individuals most at risk of limited musculoskeletal health literacy, such as those identified in this work.
The successful implementation of novel approaches to patient education has been described in several studies.30,35 Pictorial-enhanced discharge instructions have been shown to lead to improved patient comprehension in the orthopedic trauma setting, as compared with patients receiving standard instructions.30 In the setting of hip and knee osteoarthritis, a shared decision-making (SDM) tool, consisting of a booklet and DVD, was deemed more beneficial to patients than the standard 2-page brochure typically used for counseling.35 Other means of enhancing patient comprehension include the use of anatomic models and diagrams during patient encounters, which can supplement brochures, information packets, and the internet, which many patients rely on for information.6
In this study, we identify some of the risk factors for limited musculoskeletal health literacy in patients with CTS. Additional studies must be done to further delineate the factors associated with inadequate musculoskeletal literacy and to evaluate whether inadequate musculoskeletal literacy correlates with inferior outcomes following CTR.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Akalin E, El O, Peker O, et al. Treatment of carpal tunnel syndrome with nerve and tendon gliding exercises. Am J Phys Med Rehabil. 2002;81(2):108-113. [DOI] [PubMed] [Google Scholar]
- 2. Andrus MR, Roth MT. Health literacy: a review. Pharmacotherapy. 2002;22(3):282-302. [DOI] [PubMed] [Google Scholar]
- 3. Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87(6):1027-1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33-42. [DOI] [PubMed] [Google Scholar]
- 5. Basarudeen S, Sabharwal S. Assessing readability of patient education materials: current role in orthopaedics. Clin Orthop Relat Res. 2010;468(10):2572-2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Educ Res. 2001;16(6):671-692. [DOI] [PubMed] [Google Scholar]
- 7. Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391-395. [PubMed] [Google Scholar]
- 8. Dewalt DA, Berkman ND, Sheridan S, Lohr K, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Inter Med. 2004;19(12):1228-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gottfredson L. Why g matters: the complexity of everyday life. Intelligence. 1997;24(1):79-132. [Google Scholar]
- 10. Jeppesen KM, Coyle JD, Miser WF. Screening questions to predict limited health literacy: a cross-sectional study of patients with diabetes mellitus. Ann Fam Med. 2009;7(1):24-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Johnson K, Weiss BD. How long does it take to assess literacy skills in clinical practice? J Am Board Fam Med. 2008;21(3):211-214. [DOI] [PubMed] [Google Scholar]
- 12. Kadakia RJ, Tsahakis JM, Issar NM, et al. Health literacy in an orthopedic trauma patient population: A cross-sectional survey of patient comprehension. J Orthop Trauma. 2013;27(8):467-471. [DOI] [PubMed] [Google Scholar]
- 13. Katz JN, Losina E, Amick BC, Fossel AH, Bessette L, Keller RB. Predictors of outcomes of carpal tunnel release. Arthritis Rheum. 2001;44(5):1184-1193. [DOI] [PubMed] [Google Scholar]
- 14. Kelly PA, Haidet P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. 2007;66(1):119-122. [DOI] [PubMed] [Google Scholar]
- 15. Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006-483. http://nces.ed.gov/pubs2006/2006483.pdf. Published September, 2006. Accessed April 4, 2014.
- 16. Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg. 1993;75(11):1585-1592. [DOI] [PubMed] [Google Scholar]
- 17. Malibray HM, Al-Najjar AT, Yassen DM, Abuhussain HAA, Radhwi OO, Alfares ZR. Clinical profile of carpal tunnel syndrome in a teaching hospital. Pak J Med Sci. 2013;29(1):119-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mulligan M, Rosenbaum A, Phillips N, et al. Assessment of orthopaedic literacy in an urban emergency department: pilot results of the literacy in musculoskeletal problems (LiMP) project. Presented at the 126th Annual Meeting of The American Orthopaedic Association June 11-15, 2013; Denver, CO. [Google Scholar]
- 19. Nielsen-Bohlman L, Panzer AM, Kindig DA. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 20. Nordstrom DL, DeStefano F, Vierkant RA, Layde PM. Incidence of diagnosed carpal tunnel syndrome in a general population. Epidemiology. 1998;9(3):342-345. [PubMed] [Google Scholar]
- 21. Nurss J, Parker R, Williams M, Baker D. TOFHLA Test of Functional Health Literacy in Adults. Show Camp, NC: Peppercorn Books and Press; 2001. [Google Scholar]
- 22. Palmer AK, Toivonen DA. Complications of endoscopic and open carpal tunnel release. J Hand Surg Am. 1999;24(3):561-565. [DOI] [PubMed] [Google Scholar]
- 23. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537-541. [DOI] [PubMed] [Google Scholar]
- 24. Parker RM, Ratzan SC, Lurie N. Health literacy: a policy challenge for advancing high-quality health care. Health Aff. 2003;22(4):147-153. [DOI] [PubMed] [Google Scholar]
- 25. Pendlimari R, Holubar SD, Hassinger JP, Cima RR. Assessment of colon cancer literacy in screening colonoscopy patients: a validation study. J Surg Res. 2012;175(2):221-226. [DOI] [PubMed] [Google Scholar]
- 26. Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305(16):1695-1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rosenbaum AJ, Phillips N, Patel N, et al. Assessment of orthopaedic literacy in an urban emergency department: pilot results of the literacy in musculoskeletal problems (LiMP) project. Curr Orthop Pract. 2013;24(4):400-405. [Google Scholar]
- 28. Rozmaryn LM, Dovelle S, Rothman ER, Gorman K, Olvey KM, Bartko JJ. Nerve and tendon gliding exercises and the conservative management of carpal tunnel syndrome. J Hand Ther. 1998;11(3):171-179. [DOI] [PubMed] [Google Scholar]
- 29. Shea JA, Beers BB, McDonald VJ, Quistberg DA, Ravenell KL, Asch AA. Assessing health literacy in African American and Caucasian adults: disparities in rapid estimate of adult literacy in medicine (REALM) scores. Fam Med. 2004;36(8):575-581. [PubMed] [Google Scholar]
- 30. Tsahakis JM, Issar NM, Kadakia RJ, Archer KR, Barzyk T, Mir HR. Health literacy in an orthopaedic trauma patient population: improving patient comprehension with informational intervention. J Orthop Trauma. 2014;28(4):e75-e79. [DOI] [PubMed] [Google Scholar]
- 31. Vernon JA, Trujillo A, Rosenbaum S, DeBuono B. Low health literacy: Implications for national health policy. http://publichealth.gwu.edu/departments/healthpolicy/CHPR/downloads/LowHealthLiteracyReport10_4_07.pdf. Published 2007. Accessed March 5, 2014.
- 32. Wang SW, Capo JT, Orillaza N. Readability and comprehensibility of patient education material in hand-related web sites. J Hand Surg Am. 2009;34(7):1308-1315. [DOI] [PubMed] [Google Scholar]
- 33. Weiss BD. Health Literacy: A Manual for Clinicians. Chicago, IL: American Medical Association, American Medical Foundation; 2003. [Google Scholar]
- 34. Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Youm J, Chan V, Belkora J, Bozic KJ. Impact of socioeconomic factors on informed decision making and treatment choice in patients with hip and knee OA. J Arthroplasty. 2015;30(2):171-175. [DOI] [PubMed] [Google Scholar]