Abstract
Pruritus is a common complaint associated with many conditions. It negatively impacts sleep, quality of life, and mortality. Itch is transmitted along both histaminergic and non-histaminergic pathways with a complex interplay between keratinocytes, immune cells and cutaneous neurons. Individuals who present with pruritus should undergo a thorough assessment, especially those over 65 years old, to exclude underlying malignancy. Treatment no longer consists of antihistamines alone. Physicians now have an array of therapies in their armamentarium, to help alleviate this distressing symptom.
Keywords: Pruritus, histaminergic, non-histaminergic, unmyelinated C-nerve fibers, immune cells, keratinocytes, neurobiology, neuropathic, malignancy
INTRODUCTION
Pruritus is a common complaint with many aetiologies. It is defined as a sensation that drives the urge to scratch.1 It can be acute (less than 6 weeks) or chronic (greater than 6 weeks). Pruritus severely impacts upon quality of life affecting activities of daily living and sleep.2 It is important when assessing patients to take a detailed history, perform a focused physical examination, form a structured differential diagnosis and request appropriate investigations.
CASE REPORT
A 45-year-old woman presents to clinic with generalised itch, which has been present for 1 year but has increased in severity over the last few weeks. It is worse at night. On questioning, she states that while she is itchy everywhere it is worse on the palms and soles. She also complains of fatigue and nausea. Family have commented that recently her skin has turned yellow. She has a past history of hypothyroidism, controlled with thyroxine and she has not been started on any new medications.
On general inspection there is evidence of jaundice and scleral icterus. On full skin examination there are excoriations and lichenification, pronounced on her hands and feet. There is no evidence of a primary skin rash and she is clinically euthyroid.
What is the diagnosis and what would be the management plan for this patient? (Answer at the end of this review)
PATHOPHYSIOLOGY
Pruritus originates in the epidermis and dermo-epidermal junction. There is a complex interplay between activated un-myelinated C nerve fibers, immune cells and keratinocytes. There is release of several pruritogens, including proteases, cytokines, prostaglandins, neuropeptides, nerve growth factor and histamine. There is also activation of several pruritic receptors including protease-activated receptors and ion channel receptors. (TRPV1, TRPV3, TRPA1, TRPM8) Opioids and the different receptors are known to be involved in pruritus. Activation of the μ opioid receptor (e.g with morphine) causes pruritus. Conversely, antagonism of the κ-opioid receptor is pruritogenic.
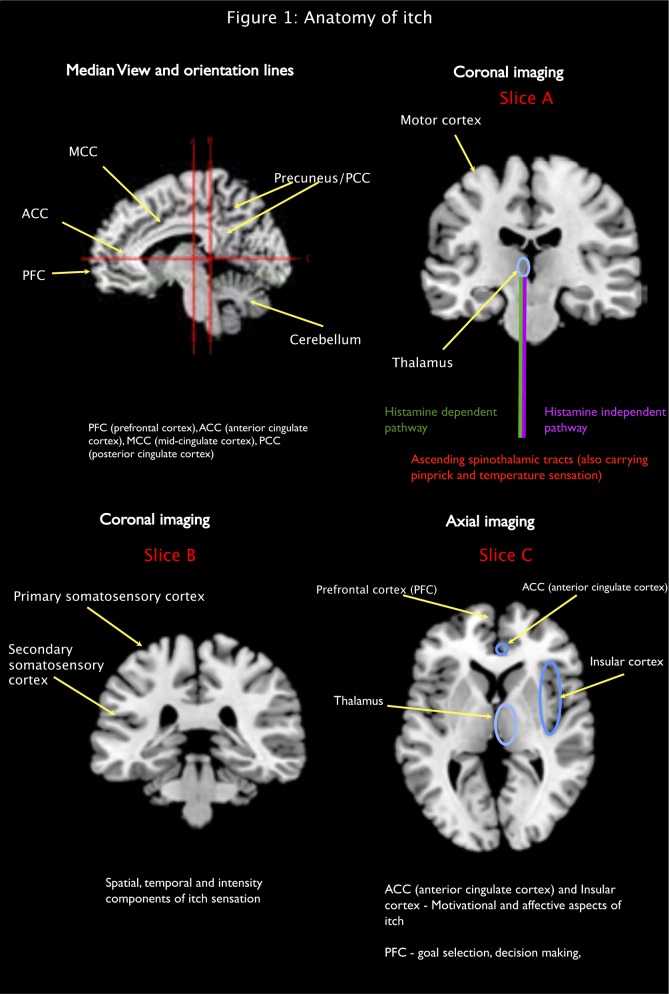
The pruritic nerve impulse is propagated along C nerve fibers to the dorsal root ganglion at the spinal cord. Here the nerve impulse crosses to the contralateral spinothalamic tract, where the impulse then ascends to the laminar nuclei of the thalamus.3, 4 It is interesting to note that the histamine dependent and histamine independent pathways have separate projections in the spinothalamic tracts. Scratching activity has been shown to inhibit activation of spinothalamic tract neuronal activity in primate models and experimental evidence suggests that scratching activates inhibitory interneurons to release glycine and gamma-aminobutyric acid (GABA) and inhibit itch neurons.5, 6
NEUROBIOLOGY OF ITCH
From the thalamus, the pruritic nerve impulse is transmitted to different regions of the brain. Functional neuroimaging studies have identified many different subcortical and cortical areas involved in itch.7–10 These areas relate to the sensory perception of itch, evaluation of the sensation, motivation, attention, emotion, and motor functions, such as motor planning.7–9
In addition, the precuneus, involved in memory, visual-spatial awareness and consciousness, is activated after acute itch stimulation.11 In contrast, no activation of the precuneus was identified, after application of an acute painful stimulus.12
Once scratching begins, imaging shows activation of the reward system due to the feeling of pleasure.10
In one study, the cerebellum, which is involved in the coordination of motor-related activity, showed no activation during both itch-induced scratching and scratching alone, in chronic itch subjects; however in healthy subjects, cerebellar activation was observed.9 This suggests decreased control of motor-related activity in patients suffering from chronic pruritus.
This pattern of neuronal network activation is different from that of pain perception, although there is significant overlap. Early studies have shown that when patients experience itch, activation of the ipsilateral motor areas, which plan the scratching response, occurs. (e.g, allowing the right hand to scratch the left forearm) This is in contrast to a painful stimulus where there is activation of the contralateral motor areas, in order to withdraw the limb from the painful stimulus.8
Two mechanisms have been postulated that contribute to chronic itch, namely peripheral and central sensitisation.7 In peripheral sensitisation there is a reduced threshold at which itch sensation is perceived along with a higher basal activity of pruritogenic receptors and nerve fibres. Central sensitisation results from the effects of neural plasticity, whereby non-itch stimuli exacerbate and are perceived as an itch sensation.
There is also a complex interplay between itch and sleep mechanisms.2 Pruritus may be experienced throughout the sleep cycle, with a predilection for the lightest stages. There is a complex interaction between circadian factors, and inflammatory mediators as well as psychological factors that can exacerbate nocturnal itch. This is a neglected area, which has already been shown to have a huge impact on mortality in patients with hemodialysis dependent renal failure.13
CAUSES
A myriad of conditions can cause chronic pruritus. Table 1 outlines a short list of different dermatologic and non-dermatologic causes.14–16
Table 1.
Common causes of pruritus.
| Common causes of itch | ||
|---|---|---|
| Dermatological | Non-dermatological | |
| Atopic dermatitis | Cholestasis
|
|
| Seborrheic dermatitis | Kidney
|
|
| Contact dermatitis | Neurological
|
|
|
|
|
| Psoriasis | Hematopoietic disease
|
|
| Urticaria | Endocrine
|
|
Infestations
|
Connective tissue disorders
|
|
Dermatophytosis
|
Psychological
|
|
Bullous disorders
|
Medications (some examples)
|
|
| Lichen planus; lichen sclerosus | Neoplasia/Paraneoplastic phenomenon | |
| Lichen simplex chronicus | HIV | |
| Cutaneous T-cell lymphoma | Advanced age (senile) | |
| Xerosis | Pregnancy associated cutaneous disorders | |
| Stasis dermatitis (venous eczema) | Post transplant | |
| Mastocytosis (cutaneous & systemic) | Hypereosinophilic syndrome | |
Abbreviations: CNS = central nervous system. PNS = peripheral nervous system. ACE = angiotensin converting enzyme. ARB = angiotensin II receptor blocker (antagonist). HIV = human immunodeficiency virus
DERMATOLOGICAL DISORDERS
Numerous dermatological disorders are associated with chronic itch. Some important examples are provided below.
ATOPIC DERMATITIS
Pruritus is the hallmark of atopic dermatitis (AD) and has a significant impact on sleep and quality of life.2, 17 Atopic dermatitis is an immune-mediated inflammatory skin disease with damage to the skin barrier. Epidermal barrier dysfunction has been associated with both decreased expression of filaggrin (an important protein involved in epidermal structure) and a reduced amount of epidermal lipids such as ceramides, aiding the entry of different pruritogens.18 Repetitive scratching may also disrupt the epidermal barrier, and further contribute to the resultant immune response. Activation of T-lymphocytes results in the release of several cytokines, such as the Th2 cytokines IL-31, IL-4 and IL-13. Targeting these cytokines is revolutionising the treatment of atopic dermatitis.19 Alloknesis, a phenomenon in which a normally innocuous stimulus induces itch, such as changes in temperature or contact with clothing, is a prominent feature in atopic eczema.
Finally, patients with atopic dermatitis have an altered microbiome favouring growth of staphylococcus aureus. These organisms release molecules which further contribute to the resultant inflammation and pruritus.(20)
There are many cutaneous findings in patients with AD – e.g. predominant flexural cutaneous involvement, hyperlinearity of the skin on the palms and soles and Dennie-Morgan folds (creases on the skin below the eyelashes).21 In addition, an infra-auricular fissure (fissure present on the posterior aspect of the ear lobe) may be present, the severity of which correlates with AD severity.22
PSORIASIS
Psoriasis is a chronic immune-mediated inflammatory disorder, occurring in genetically predisposed individuals, with different environmental factors attributed to the disease and its flares. (e.g infections, medications, stress) Pruritus is reported in approximately 60-90% of psoriatic patients23, 24 and has only recently been recognized as a major symptom in this chronic disease that affects 2-3% of the population.25 In psoriasis, a dysregulated immune system is related to the overproduction of pro-inflammatory cytokines, including TNF-α, IL-12, IL-17, IL-23, which have a pruritic effect. In addition, the neural system is activated, with release of multiple substances, (in particular nerve growth factor (NGF) and Substance P), along with abnormal psoriatic skin innervation, imbalance in kappa- and mu-opioid pathways and increased levels of gamma-aminobutyric acid (GABA) and its receptor (GABAA).24 These have all been shown to contribute to pruritus in psoriatic patients.
INFESTATIONS
Patients suffering from scabies infestation often complain of severe (predominantly nocturnal) itch. The pruritus occurs through the release of proteases excreted in the mite’s faeces. The release of pruritic cytokines, from the activation of T-helper 2 lymphocytes, is also attributed to the pruritus in scabies, pediculosis (lice) and pinworm infestations. The movement of enterobius vermicularis (the causative agent in pinworm infestations) on the skin, as well as the release of eggs, commonly causes intense peri-anal pruritus. Subsequent scratching deposits these eggs under the fingernails and the pinworm may therefore re-enter the oral cavity and gastrointestinal tract, if patients exhibit poor hand hygiene.26, 27 Finally bed bugs are attracted to carbon dioxide and heat, and commonly feed on humans while they are sleeping at night.28
ADVANCED AGE PRURITUS
Pruritus is a common symptom in the elderly. A detailed history, examination and appropriate investigations must be performed, but often, no cause is identified. Patients exhibit xerosis (dry skin) with epidermal barrier dysfunction (with increased trans-epidermal water loss), alterations in pH, release of molecules (e.g proteases) and decreased estrogen levels. In addition there is immunosenescence (dampening of the immune system during the aging process) and neural degeneration comprising neuropathic itch (e.g. post herpetic neuralgia) and nerve compression (radiculopathy)29
CHRONIC URTICARIA
Urticaria is a disorder associated with mast cell degranulation releasing substances including histamine, leukotrienes and prostaglandins. It has a prevalence of 0.5-1%.30 Clinically, this manifests with wheals, angioedema or both, and usually lasts less than 24 hours. Urticaria is divided into acute (duration <6 weeks) or chronic (duration >6 weeks). New classification subdivides chronic urticaria into chronic inducible urticaria (CINDU) and chronic spontaneous urticaria (CSU).31 There are many different triggers for CINDU including cold, sunlight, contact and aqueous. In many cases, a specific cause may not be identified.
The arms, back and legs are commonly affected. The accompanying pruritus is described as stinging, tickling or burning.32
Second generation, non-sedating antihistamines are currently recommended as first-line therapy for chronic urticaria.33. Other treatments include doxepin, leukotriene antagonists, histamine-2 antagonists, ciclosporin and mycophenolate mofetil. Omalizumab, a monoclonal antibody that targets and neutralizes free IgE, is a useful alternative antipruritic medication in unresponsive patients.34 Its use is restricted to physicians with experience in prescribing this medication.
NON-DERMATOLOGICAL DISORDERS CHOLESTATIC ITCH
Cholestatic pruritus may be subdivided into intra-hepatic, (e.g chronic hepatitis, carcinoma, primary biliary cirrhosis, intrahepatic cholestasis of pregnancy, Alagille syndrome) extra-hepatic (e.g cholelithiasis/choledocholithiasis, primary sclerosing cholangitis, bile duct stricture, cholangiocarcinoma, pancreatic carcinoma) and drug-induced. (e.g macrolides, chlorpromazine)35 Patients classically complain of itch affecting the palms and soles of the feet.
The exact pathophysiology is not fully known, however cholestatic pruritus has been associated with accumulation of bile salts, bile acids as well as increased levels of bilirubin and endogenous opioids. Elevated levels of a phospholipid (lysophosphatidic acid) and autotaxin, the enzyme that forms LPA, have been found in this cohort. Autotaxin has been shown to be a biomarker for cholestatic pruritus.36
Therapies such as bile acid sequestrants, mu-opioid antagonists, sertraline and rifampicin have been shown to improve cholestatic pruritus.36, 37
CKD ASSOCIATED PRURITUS
End stage renal disease patients, particularly those requiring haemodialysis, may suffer from chronic pruritus. The Dialysis Outcomes and Practice Patterns study (DOPPS) showed an increased mortality risk of 17% among 18,801 pruritic haemodialysis patients. This was in part attributed to a decreased quality of sleep.13 Around 50-90% of patients on dialysis suffer from pruritus.38 The pathophysiology is uncertain. There are several hypotheses, including abnormal calcium, phosphate and parathyroid levels, an imbalance among opioids, central neuropathy and a pro-inflammatory state.39 Pruritus is usually only observed in patients with chronic (rarely acute) kidney disease.40
Itching commonly involves the back, but the head, neck and torso may also be affected.4, 40–42 Treatment involves adequate skin hydration and optimization of renal status. Antihistamines tend not to be effective. Gabapentin has been shown to improve CKD itch,43 but care should be taken in monitoring renal function. Nalfurafine, a kappa opioid agonist, has also shown to improve CKD pruritus but is currently unlicensed for this indication.19,44 Ultraviolet light therapy is another modality that may be employed. 39 Other opioid therapies are undergoing trials for this condition.45-47
HAEMATOLOGICAL
Itch may be a prominent feature in haematological disorders e.g Hodgkin’s lymphoma, chronic lymphocytic leukemia, multiple myeloma, cutaneous T-cell lymphoma (CTCL) and polycythemia vera. Pruritus is present in around 19% of patients with Hodgkin’s lymphoma48 and approximately 15% of patients with non-Hodgkin’s lymphoma.49 The pruritus in Hodgkin’s lymphoma is usually associated with disease activity.14 IL-31 has been shown to be significantly increased in the epidermis and dermis of patients with CTCL.50 There have been reports of patients who have chronic pruritus with no cutaneous manifestations, but with underlying mycosis fungoides.51–53 This highlights the necessity to constantly review the diagnosis in patients with chronic pruritus. Finally, while water may also aggravate pruritus in patients with urticaria, aquagenic pruritus warrants investigation for evidence of polycythemia vera.
NEUROPATHIC ITCH
Neurological disorders may also display pruritus. Neuropathic itch has been defined as “an itch initiated or caused by a primary lesion or dysfunction at any point along the afferent pathway of the nervous system.”54 Brachioradial pruritus (BRP) usually presents with itch affecting dermatomes C4-C7. Compression of nerve fibers from cervical disc degeneration, spinal stenosis or malignancy may be the underlying cause. Notalgia paresthetica is another form of radiculopathy that may present with unilateral localized pruritus in the mid back, following a T2-T6 distribution. It may be associated with a sensory neuropathy and burning pain.54
Post-herpetic neuralgia can cause significant pruritus in up to 48% of patients. The itch commonly involves the face and neck.55, 56
Topical capsaicin, which decreases Substance P release from C-nerve fibers, and GABAergic medications, may help.57
Central nervous system (CNS) disorders causing itch are usually due to brainstem or subcortical lesions.7 Unilateral itch has been reported following cerebral infarction, as well as in patients with a cortical stroke.7 Pruritus associated with multiple sclerosis is rare, occurring in only 4.5% of patients.58
INVESTIGATIONS
If pruritus is acute (< 6 weeks) one should determine if any new medications have been prescribed and check for any associated rash – e.g. urticaria causes itch and an erythematous rash but generally does not persist for >24 hours.
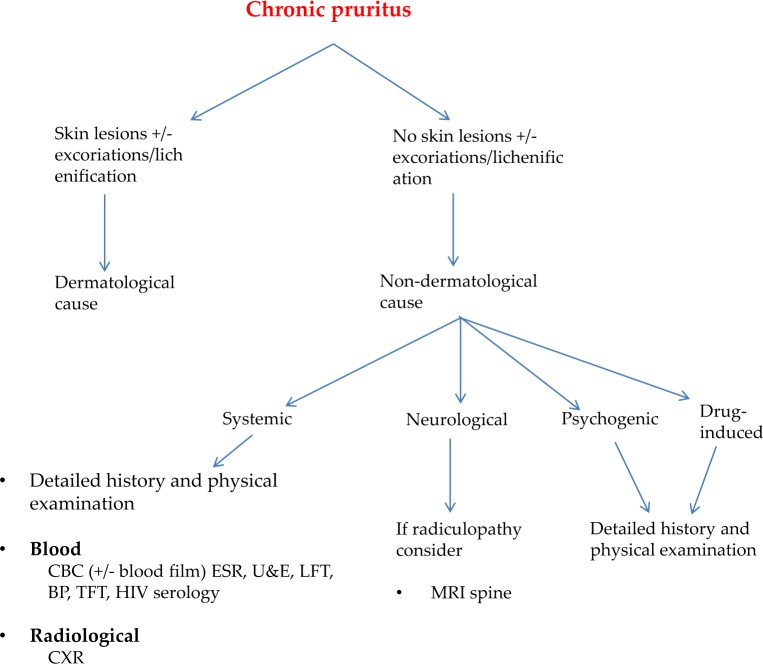
If the pruritus is chronic (> 6 weeks), then a comprehensive review is required. In the elderly, it is important to consider underlying malignancy. The presence of a rash may be pivotal in determining the diagnosis; however not every patient will have a rash and often there may just be excoriations or lichenification. Figure 2 outlines a flowchart for the management of patients who present with chronic pruritus.
Fig 2.
Chronic pruritus algorithm
Fig 1.
highlights these activated brain regions.
TREATMENT
Before commencing treatment, it is important to determine if the patient has acute or chronic pruritus, and then investigate for the cause and evidence of any underlying malignancy; however, while results are awaited, therapy may be initiated.
Treatment can be divided into topical or oral therapy. Antihistamines are generally not effective in chronic pruritus. Topical therapies such as moisturizers, low pH cleansers, short-term use of topical corticosteroids, menthol, capsaicin, strontium and topical anesthetic agents may be employed. Oral medications, such as low dose mirtazapine and gabaergic agents (gabapentin, pregabalin) have been shown to be beneficial. Therapies to treat the underlying condition are also important.
Major pharmacological treatment modalities, both topical and systemic, are discussed below and summarized in Table 3 and 4.
Table 3.
Examples of systemic therapies to treat chronic pruritus
| Systemic medications | Mode of action | Dose |
|---|---|---|
Sedating antihistamines e.g.
|
H1 antagonist |
|
Non-sedating antihistamines e.g.
|
H1 antagonist |
|
| Mirtazapine | SNRI, SSRI |
|
| Gabapentin Pregabalin |
Modulate GABA |
|
Opioids
|
|
|
|
|
|
Abbreviations: H1 = histamine 1. SNRI = serotonin noradrenaline re-uptake inhibitor. SSRI = selective serotonin re-uptake inhibitor. GABA = gamma-aminobutyric acid
Table 2.
Examples of topical therapies to treat chronic pruritus
| Topical Medications | Mode of action | Dose |
|---|---|---|
| Emollients | Improve barrier function | Apply as needed |
| Oat meal extracts | Anti-inflammatory Anti-oxidant |
Apply as needed |
| Corticosteroid | Anti-inflammatory | As prescribed Short-term use advocated |
| Tacrolimus Pimecrolimus |
Calcineurin inhibitor | 0.03%; 0.1% ointment 1% cream |
| Menthol | TRPM8 agonist | 1-2% cream |
| Capsaicin | TRPV1 agonist Reduces Substance P release from C-nerve fibers |
0.025% - 0.1% Transdermal patch 8% |
| Pramoxine (with hydrocortisone) |
Ion channel blocker (anti-inflammatory) |
1% cream (2.5%) |
| Strontium 4% | Calcimimetic | 4% hydrogel |
| Ketamine/Amitriptyline/Lidocaine | Ion channel blocker | Ketamine 5-10%, Amitriptyline 2-5% Lidocaine 2.5-5% Apply during pruritic episode |
| Doxepin | H1 and H2 antagonist Tricyclic antidepressant |
5% cream |
Abbreviation: TRPM8 = Transient receptor potential subfamily M member 8. TRPV1 – Transient receptor potential subfamily V member 1. H1 = histamine 1. H2= histamine 2
Topical
An array of medications is available to treat pruritus. Basic skin care management cannot be over-emphasised. Simple treatment with moisturisers can have a huge impact upon the intensity of pruritus by improving skin barrier dysfunction and reducing the entry of pruritogens. Patients should use moisturisers liberally. For convenience, creams are usually applied during the day and greasier ointments at night. If patients are required to apply topical steroid creams, these should be applied before moisturisers. Wet pyjama therapy, whereby the patient applies a topical moisturiser with a corticosteroid and then dons ‘wet’ pyjamas (pyjamas that have been rinsed in water and then wrung out) has been shown to improve pruritus.59 Explanation of the efficacy of this treatment is recommended due to the lack of willingness to adopt this approach.
It now recognized that high skin pH results in the release of proteases and activation of proteinase activating receptors. (PAR-2) This leads to inflammation, an impaired skin barrier and decreased stratum corneum cohesion. As such, syndet (synthetic detergent) products, which have a lower pH, (4.5-6.0) should be favored.60, 61
Ion channels, such as TRPV1 and TRPM8 are known to be involved in the pathophysiology of chronic pruritus. Capsaicin, an ingredient of hot chili peppers, initially activates but over time desensitizes TRPV1 ion channels.62 It may be used to treat patients with notalgia paresthetica, CKD and prurigo nodularis.63, 64 The burning sensation that may occur after application of capsaicin may be reduced with pre-treatment with local anaesthetic cream.65 An 8% patch has also shown efficacy in patients with neuropathic pruritus.62, 66 Menthol, a TRPM8 agonist, evokes a cooling sensation and promotes repair of the skin barrier. 19 It may reduce pruritus in conditions such as lichen sclerosus and lichen amyloidosis.67
Other topical agents that are useful in reducing pruritus include pramoxine, strontrium and the compounded formulation of ketamine, amitriptyline and lidocaine. Pramoxine is a local anesthetic agent that reduces neuropathic, anogenital and CKD-associated pruritus.68, 69 It may also be combined with corticosteroids to reduce both inflammation and pruritus. Topical strontium 4% hydrogel (a calcimimetic) has been shown to reduce both histaminergic and non-histaminergic induced pruritus.70, 71
The compounded formulation of ketamine, amitriptyline and lidocaine, (KAL) in various dosing percentages, has been successfully used to treat localised neuropathic itch. (unpublished data, Yosipovitch)
Finally Crisaborole (a topical phosphodiesterase-4 inhibitor) has shown promise in early trials by reducing pruritus associated with AD.72
Oral
Traditionally, antihistamines have been used to treat pruritus. These can be helpful in treating urticaria, cutaneous mastocytosis and drug-induced pruritus.15 Antihistamines work by antagonizing the histamine-1 receptor and can have indirect effects on the TRPV1 ion channel.16 They can be divided into sedating (e.g chlorphenamine, diphenhydramine, hydroxyzine) and non-sedating (e.g cetirizine, levocetirizine, fexofenadine). Sedating antihistamines cause drowsiness and as such are generally taken at night. These medications can still exert adverse daytime effects and may lead to daytime somnolence and increased risk of accidents. Improvement of nocturnal pruritus is likely due to this sedating effect. Guidelines recommend use of non-sedating antihistamines if these agents are to be employed to treat pruritus associated with urticaria.33 There is a lack of data however on the efficacy of antihistamines to treat chronic pruritus. Given that the histaminergic pathway is not the main pathway involved in chronic pruritus, novel therapies have been sought.
Gabaergics, such as gabapentin and pregabalin, which are structural analogs of gamma-aminobutyric acid, have shown efficacy in treating pruritus in CKD patients43 as well as in patients with neuropathic itch. 3 They may also be effective in other causes of chronic pruritus. Side-effects include drowsiness, increased appetite, and lower limb edema.
Mirtazapine has been shown to improve nocturnal pruritus. It is an antagonist of alpha-2 noradrenergic receptors, as well as H1, 5HT-2 and 5HT-3 cutaneous receptors. It has been used successfully to treat pruritus associated with malignant cholestasis, uremia, lymphoma, atopic dermatitis, urticaria and carcinoma en cuirasse.73–75 Mirtazapine has a favorable safety profile. Side-effects include drowsiness, increased appetite and dry mouth. While patients may be hesitant to commence this medication due to fear of weight gain and drowsiness, these side-effects are also associated with sedating anti-histamines.
As noted above, there is a complex interaction between pain and itch – e.g. when patients scratch an itch it initially incites a pleasurable sensation. Medications, such as morphine, a μ-opioid receptor agonist, are known to cause pruritus. Conversely κ-opioid receptor antagonists will cause pruritus. It is therefore intuitive to prescribe patients either antagonists or agonists of the μ-/κ-opioid receptor, respectively. Naltrexone, a μ-opioid receptor antagonist, has been shown to reduce cholestatic pruritus and refractory itch in burn patients.76, 77 Its efficacy in CKD-associated pruritus has not always been reproduced.78, 79 Nalfurafine, a selective κ-opioid receptor agonist, has been shown to reduce CKD itch, however it is currently not licensed in the USA or Europe.44 Butorphanol, a partial μ receptor antagonist and κ receptor agonist, has been used for intractable chronic pruritus.80 It is an intranasal spray with 1 puff representing 1mg. Up to 4mg may be used over 24 hours if necessary. A recent study revealed that butorphanol deactivates areas of the brain that were initially activated during itch processing.81
Other
Immunosuppressants such as methotrexate, cyclosporine, azathioprine, mycophenolate mofetil have been used for inflammatory pruritic skin diseases.82–84
Novel medications that target specific pruritic cytokines and neurotrophins, are undergoing clinical trials, with promising results. Dupilumab, a monoclonal antibody that targets IL-4 and IL-13 has been shown to reduce pruritus in patients with moderate to severe atopic dermatitis. It has been assigned breakthrough status by the FDA.85 Monoclonal antibodies targeting the pruritic IL-31 cytokine have shown quantitative reduction in pruritus in early trials.19 Ustekinumab (IL-12 and IL-23 receptor antagonist) is currently licensed for use in psoriasis and psoriatic arthritis and has been shown to improve psoriatic pruritus. It is currently undergoing clinical trial evaluation in patients with atopic dermatitis.86 Secukinumab and Ixekizumab (targeting IL-17A) have shown significant anti-pruritic effect in psoriatic patients.87, 88 The oral phosphodiesterase-4 inhibitor, apremilast, has also shown an anti-pruritic effect in psoriasis.89
Non-pharmacological therapy
Non-pharmacological management of pruritus may also be employed. Psychological interventions such as progressive muscle relaxation and habit-reversal therapy may improve chronic pruritus.90 We have found at our institution (MJL, GY) that progressive muscle relaxation, subjectively improves pruritus.
Diet is a major concern for patients with chronic pruritus, especially those suffering with atopic dermatitis. While these patients often have associated food allergies, strict dietary practice is not advocated.18 The American Academy of Dermatology has recently produced guidelines on the management of atopic dermatitis, including dietary recommendations.91 These include avoidance of foods that cause a true IgE-mediated allergy; however it does not recommend eliminating foods, based on allergy tests alone.
CONCLUSION
Research has increased our understanding of the pathophysiology of pruritus. It is imperative that physicians investigate for underlying systemic disease and malignancy, especially in the elderly.
There is now awareness of the different brain pathways that are activated and further research into how this knowledge can be incorporated into treatments is warranted.
In addition, knowledge of the different pathways (histamine and non-histamine) and mediators involved in itch has changed the pharmacological management of pruritus. Histamine is no longer the only known mediator associated with pruritus, and therefore antihistamines used alone, may not be effective. Novel targeted therapies which not only reduce the severity of the disease, but also reduce pruritus have ushered in a new era. The aim of treatment for both patients and physicians is to reduce itch intensity. Completely curing the pruritus is unlikely and patients should recognise this.
Conflicts of interest
MJL, MOK, JC declare no conflict of interest. HM is principal investigator for the National Eczema Association. GY is consultant, principle investigator or scientific advisory board member for TREVI, Tioga, Hoffmann-LaRoche, Creabilis, Chugai, Pfizer, Anacor, Celgene, Eli Lily, Johnson & Johnson, Cara, Allergan, GSK-Stiefel and LEO Foundation.
Case report answer
The patient requires immediate investigation for symptoms of chronic pruritus. Given the description of her itch and evidence of jaundice on examination, cholestatic pruritus is high on the list of differential diagnoses. Initial investigation should include a full blood count with differential, erythrocyte sedimentation rate, liver function tests, urea and electrolytes and thyroid function tests. Radiological investigation should be requested following results of these tests or if there is clinical concern regarding underlying malignancy. As this patient is suffering from chronic pruritus, antihistamine therapy is unlikely to be helpful. Bile acid resins, (e.g cholestyramine) mirtazapine and sertraline may reduce the pruritus, however treatment of the underlying condition is important. A therapeutic ladder for the treatment of pruritus in chronic liver disease (as well as in end stage renal disease and lymphoma) has been proposed. 35
REFERENCES
- 1.Stander S, Weisshaar E, Mettang T, Szepietowski JC, Carstens E, Ikoma A, et al. Clinical classification of itch: a position paper of the International Forum for the Study of Itch. Acta Derm Venereol. 2007;87(4):291–4. doi: 10.2340/00015555-0305. [DOI] [PubMed] [Google Scholar]
- 2.Lavery MJ, Stull C, Kinney MO, Yosipovitch G. Nocturnal Pruritus: The battle for a peaceful night’s sleep. Int J Mol Sci. 2016;17(3):425. doi: 10.3390/ijms17030425. pii E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yosipovitch G, Bernhard JD. Clinical practice. Chronic pruritus. N Engl J Med. 2013;25(368(17)):1625–34. doi: 10.1056/NEJMcp1208814. [DOI] [PubMed] [Google Scholar]
- 4.Tarikci N, Kocaturk E, Gungor S, Topal IO, Can PU, Singer R. Pruritus in systemic diseases: a review of etiological factors and new treatment modalities. Scientific World Journal. 2015;2015:803752. doi: 10.1155/2015/803752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davidson S, Zhang X, Khasabov SG, Moser HR, Honda CN, Simone DA, et al. Pruriceptive spinothalamic tract neurons: physiological properties and projection targets in the primate. J Neurophysiol. 2012;108(6):1711–23. doi: 10.1152/jn.00206.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akiyama T, Iodi Carstens M, Carstens E. Transmitters and pathways mediating inhibition of spinal itch-signaling neurons by scratching and other counterstimuli. PLoS One. 2011;6(7):e22665. doi: 10.1371/journal.pone.0022665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dhand A, Aminoff MJ. The neurology of itch. Brain. 2014;137(Pt 2):313–322. doi: 10.1093/brain/awt158. [DOI] [PubMed] [Google Scholar]
- 8.Ikoma A, Steinhoff M, Stander S, Yosipovitch G, Schmelz M. The neurobiology of itch. Nat Rev Neurosci. 2006;7(7):535–47. doi: 10.1038/nrn1950. [DOI] [PubMed] [Google Scholar]
- 9.Mochizuki H, Papoiu AD, Nattkemper LA, Lin AC, Kraft RA, Coghill RC, et al. Scratching induces overactivity in motor-related regions and reward system in chronic itch patients. J Invest Dermatol. 2015;135(11):2814–23. doi: 10.1038/jid.2015.223. [DOI] [PubMed] [Google Scholar]
- 10.Mochizuki H, Papoiu ADP, Yosipovitch G. Brain processing of itch and scratching. In: Carstens E, Akiyama T, editors. Itch: mechanisms and treatment. Boca Raton (FL): Taylor & Francis Group; 2014. pp. 391–408. [PubMed] [Google Scholar]
- 11.Papoiu AD, Coghill RC, Kraft RA, Wang H, Yosipovitch G. A tale of two itches. Common features and notable differences in brain activation evoked by cowhage and histamine induced itch. Neuroimage. 2012 Feb 15;59(4):3611–3623. doi: 10.1016/j.neuroimage.2011.10.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Apkarian AV, Bushnell MC, Treede RD, Zubieta JK. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005 Aug;9(4):463–484. doi: 10.1016/j.ejpain.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Pisoni RL, Wikstrom B, Elder SJ, Akizawa T, Asano Y, Keen ML, et al. Pruritus in haemodialysis patients: International results from the Dialysis Outcomes and Practice Patterns Study (DOPPS) Nephrol Dial Transplant. 2006 Dec;21(12):3495–3505. doi: 10.1093/ndt/gfl461. [DOI] [PubMed] [Google Scholar]
- 14.Yosipovitch G. Pruritus. In: Callen J, Jorizzo J, Zone J, Piette W, Rosenbach M, Vleugels R, editors. Dermatological signs of systemic disease. 5th ed. Amsterdam: Elsevier; 2016. pp. 99–103. [Google Scholar]
- 15.Reich A, Stander S, Szepietowski JC. Drug-induced pruritus: a review. Acta Derm Venereol. 2009;89(3):236–244. doi: 10.2340/00015555-0650. [DOI] [PubMed] [Google Scholar]
- 16.Kremer AE, Feramisco J, Reeh PW, Beuers U, Oude Elferink RP. Receptors, cells and circuits involved in pruritus of systemic disorders. Biochim Biophys Acta. 2014;1842(7):869–892. doi: 10.1016/j.bbadis.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Mollanazar NK, Smith PK, Yosipovitch G. Mediators of chronic pruritus in atopic dermatitis: getting the itch out? Clin Rev Allergy Immunol. 2015 May;:1–30. doi: 10.1007/s12016-015-8488-5. [DOI] [PubMed] [Google Scholar]
- 18.Silverberg NB, Lee-Wong M, Yosipovitch G. Diet and atopic dermatitis. Cutis. 2016 Mar;97(3):227–232. [PubMed] [Google Scholar]
- 19.Stull C, Lavery MJ, Yosipovitch G. Advances in therapeutic strategies for the treatment of pruritus. Expert Opin Pharmacother. 2016;17(5):671–87. doi: 10.1517/14656566.2016.1127355. [DOI] [PubMed] [Google Scholar]
- 20.Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109–22. doi: 10.1016/S0140-6736(15)00149-X. [DOI] [PubMed] [Google Scholar]
- 21.Blanc S, Bourrier T, Albertini M, Chiaverini C, Giovannini-Chami L. Dennie-Morgan fold plus dark circles: suspect atopy at first sight. J Pediatr. 2015;166(6):1541. doi: 10.1016/j.jpeds.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 22.Kwatra SG, Tey HL, Ali SM, Dabade T, Chan YH, Yosipovitch G. The infra-auricular fissure: a bedside marker of disease severity in patients with atopic dermatitis. J Am Acad Dermatol. 2012;66(6):1009–10. doi: 10.1016/j.jaad.2011.10.031. [DOI] [PubMed] [Google Scholar]
- 23.Yosipovitch G, Goon A, Wee J, Chan YH, Goh CL. The prevalence and clinical characteristics of pruritus among patients with extensive psoriasis. Br J Dermatol. 2000;143(5):969–73. doi: 10.1046/j.1365-2133.2000.03829.x. [DOI] [PubMed] [Google Scholar]
- 24.Szepietowski JC, Reich A. Pruritus in psoriasis: an update. Eur J Pain. 2016;20(1):41–6. doi: 10.1002/ejp.768. [DOI] [PubMed] [Google Scholar]
- 25.Roblin D, Wickramasinghe R, Yosipovitch G. Pruritus severity in patients with psoriasis is not correlated with psoriasis disease severity. J Am Acad Dermatol. 2014;70(2):390–1. doi: 10.1016/j.jaad.2013.09.030. [DOI] [PubMed] [Google Scholar]
- 26.Raju K, Verappa S, Venkataramappa SM. Enterobius vermicularis infestation masquerading as cervical carcinoma: A cytological diagnosis. J Nat Sci Biol Med. 2015;6(2):476–9. doi: 10.4103/0976-9668.160047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patsantara GG, Piperaki ET, Tzoumaka-Bakoula C, Kanariou MG. Immune responses in children infected with the pinworm Enterobius vermicularis in central Greece. J Helminthol. 2016;90(3):337–41. doi: 10.1017/S0022149X15000334. [DOI] [PubMed] [Google Scholar]
- 28.Lavery MJ, Parish LC. Bed bugs revisited. Skinmed. 2011;9(1):6–8. [PubMed] [Google Scholar]
- 29.Valdes-Rodriguez R, Stull C, Yosipovitch G. Chronic pruritus in the elderly: pathophysiology, diagnosis and management. Drugs Aging. 2015;32(3):201–15. doi: 10.1007/s40266-015-0246-0. [DOI] [PubMed] [Google Scholar]
- 30.Maurer M, Weller K, Bindslev-Jensen C, Gimenez-Arnau A, Bousquet PJ, Bousquet J, et al. Unmet clinical needs in chronic spontaneous urticaria. A GA(2)LEN task force report. Allergy. 2011;66(3):317–30. doi: 10.1111/j.1398-9995.2010.02496.x. [DOI] [PubMed] [Google Scholar]
- 31.Moolani Y, Lynde C, Sussman G. Advances in understanding and managing chronic urticaria. F1000Res. 2016;5 doi: 10.12688/f1000research.7246.1. pii F1000 Faculty Rev-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yosipovitch G, Ansari N, Goon A, Chan YH, Goh CL. Clinical characteristics of pruritus in chronic idiopathic urticaria. Br J Dermatol. 2002;147(1):32–6. doi: 10.1046/j.1365-2133.2002.04758.x. [DOI] [PubMed] [Google Scholar]
- 33.Zuberbier T, Aberer W, Asero R, Bindslev-Jensen C, Brzoza Z, Canonica GW, et al. The EAACI/GA(2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy. 2014;69(7):868–87. doi: 10.1111/all.12313. [DOI] [PubMed] [Google Scholar]
- 34.Kaplan A, Ledford D, Ashby M, Canvin J, Zazzali JL, Conner E, et al. Omalizumab in patients with symptomatic chronic idiopathic/spontaneous urticaria despite standard combination therapy. J Allergy Clin Immunol. 2013;132(1):101–9. doi: 10.1016/j.jaci.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Yosipovitch G. New insights into the pathophysiology and treatment of chronic itch in patients with end-stage renal disease, chronic liver disease, and lymphoma. Int J Dermatol. 2010;49(1):1–11. doi: 10.1111/j.1365-4632.2009.04249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kremer AE, van Dijk R, Leckie P, Schaap FG, Kuiper EM, Mettang T, et al. Serum autotaxin is increased in pruritus of cholestasis, but not of other origin, and responds to therapeutic interventions. Hepatology. 2012;56(4):1391–400. doi: 10.1002/hep.25748. [DOI] [PubMed] [Google Scholar]
- 37.Kremer AE, Bolier R, van Dijk R, Oude Elferink RP, Beuers U. Advances in pathogenesis and management of pruritus in cholestasis. Dig Dis. 2014;32(5):637–45. doi: 10.1159/000360518. [DOI] [PubMed] [Google Scholar]
- 38.Narita I, Iguchi S, Omori K, Gejyo F. Uremic pruritus in chronic hemodialysis patients. J Nephrol. 2008;21(2):161–5. [PubMed] [Google Scholar]
- 39.Combs SA, Teixeira JP, Germain MJ. Pruritus in kidney disease. Semin Nephrol. 2015;35(4):383–91. doi: 10.1016/j.semnephrol.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patel TS, Freedman BI, Yosipovitch G. An update on pruritus associated with CKD. Am J Kidney Dis. 2007;50(1):11–20. doi: 10.1053/j.ajkd.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 41.Yosipovitch G, Zucker I, Boner G, Gafter U, Shapira Y, David M. A questionnaire for the assessment of pruritus: validation in uremic patients. Acta Derm Venereol. 2001;81(2):108–11. doi: 10.1080/00015550152384236. [DOI] [PubMed] [Google Scholar]
- 42.Zucker I, Yosipovitch G, David M, Gafter U, Boner G. Prevalence and characterization of uremic pruritus in patients undergoing hemodialysis: uremic pruritus is still a major problem for patients with end-stage renal disease. J Am Acad Dermatol. 2003;49(5):842–6. doi: 10.1016/s0190-9622(03)02478-2. [DOI] [PubMed] [Google Scholar]
- 43.Nofal E, Farag F, Nofal A, Eldesouky F, Alkot R, Abdelkhalik Z. Gabapentin: a promising therapy for uremic pruritus in hemodialysis patients: a randomized-controlled trial and review of literature. J Dermatolog Treat. 2016 Apr;4:1–5. doi: 10.3109/09546634.2016.1161161. [DOI] [PubMed] [Google Scholar]
- 44.Inui S. Nalfurafine hydrochloride to treat pruritus: a review. Clin Cosmet Investig Dermatol. 2015;8:249–55. doi: 10.2147/CCID.S55942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chalmers D. Cara therapeutics announces positive results from phase 2 trial in uremic pruritus (NASDAQ:CARA) Stamford, Connecticut: Cara Therapeutics; 2015. Available online from: http://ir.caratherapeutics.com/releasedetail.cfm?releaseid=923457. Last accessed July 2016. [Google Scholar]
- 46.U.S. National Institutes of Health. Clinicaltrials.gov. Study of Nalbuphine HCL ER tablets in hemodialysis patients with uremic pruritus. Bethesda: National Institutes of Health; 2016. Available online from: https://clinicaltrials.gov/ct2/show/NCT02143648?term=nalbuphine+pruritus&rank=1. Last accessed July 2016. [Google Scholar]
- 47.U.S. National Institutes of Health. Clinicaltrials.gov. Study of Nalbuphine HCL ER tablets in patients with prurigo nodularis. Bethesda: National Institutes of Health; 2016. Available online from: https://clinicaltrials.gov/ct2/show/NCT02174419?term=nalbuphine+pruritus&rank=5. Last accessed July 2016. [Google Scholar]
- 48.Rubenstein M, Duvic M. Cutaneous manifestations of Hodgkin’s disease. Int J Dermatol. 2006;45(3):251–6. doi: 10.1111/j.1365-4632.2006.02675.x. [DOI] [PubMed] [Google Scholar]
- 49.Kumar SS, Kuruvilla M, Pai GS, Dinesh M. Cutaneous manifestations of non-Hodgkin’s lymphoma. Ind J Dermatol Venereol Leprol. 2003;69(1):12–15. [PubMed] [Google Scholar]
- 50.Nattkemper LA, Martinez-Escala ME, Gelman AB, Singer EM, Rook AH, Guitart J, et al. Cutaneous T-Cell lymphoma and pruritus: the expression of IL-31 and its receptors in the skin. Acta Derm Venereol. 2016 Mar 22; doi: 10.2340/00015555-2417. [DOI] [PubMed] [Google Scholar]
- 51.Deen K, O’Brien B, Wu J. Invisible mycosis fungoides: not to be missed in chronic pruritus. Dermatol Ther (Heidelb) 2015;5(3):213–6. doi: 10.1007/s13555-015-0083-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pujol RM, Gallardo F, Llistosella E, Blanco A, Bernado L, Bordes R, et al. Invisible mycosis fungoides: a diagnostic challenge. J Am Acad Dermatol. 2000;42(2 Pt 2):324–8. doi: 10.1016/s0190-9622(00)90103-8. [DOI] [PubMed] [Google Scholar]
- 53.Dereure O, Guilhou JJ. Invisible mycosis fungoides: a new case. J Am Acad Dermatol. 2001;45(2):318–9. doi: 10.1067/mjd.2001.114561. [DOI] [PubMed] [Google Scholar]
- 54.Berny-Moreno J, Szepietowski JC. Neuropathic itch caused by nerve root compression: brachioradial pruritus and notalgia paresthetica. Serb J Dermatol Venereol. 2009;2:68–72. [Google Scholar]
- 55.Oaklander AL, Cohen SP, Raju SV. Intractable postherpetic itch and cutaneous deafferentation after facial shingles. Pain. 2002;96(1-2):9–12. doi: 10.1016/s0304-3959(01)00400-6. [DOI] [PubMed] [Google Scholar]
- 56.Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32–41. doi: 10.1111/j.1529-8019.2008.00167.x. [DOI] [PubMed] [Google Scholar]
- 57.Twycross R, Greaves MW, Handwerker H, Jones EA, Libretto SE, Szepietowski JC, et al. Itch: scratching more than the surface. QJM. 2003;96(1):7–26. doi: 10.1093/qjmed/hcg002. [DOI] [PubMed] [Google Scholar]
- 58.Elsone L, Townsend T, Mutch K, Das K, Boggild M, Nurmikko T, et al. Neuropathic pruritus (itch) in neuromyelitis optica. Mult Scler. 2013;19(4):475–9. doi: 10.1177/1352458512457720. [DOI] [PubMed] [Google Scholar]
- 59.Dabade TS, Davis DM, Wetter DA, Hand JL, McEvoy MT, Pittelkow MR, et al. Wet dressing therapy in conjunction with topical corticosteroids is effective for rapid control of severe pediatric atopic dermatitis: experience with 218 patients over 30 years at Mayo Clinic. J Am Acad Dermatol. 2012;67(1):100–6. doi: 10.1016/j.jaad.2011.06.025. [DOI] [PubMed] [Google Scholar]
- 60.Ali SM, Yosipovitch G. Skin pH: from basic science to basic skin care. Acta Derm Venereol. 2013;93(3):261–7. doi: 10.2340/00015555-1531. [DOI] [PubMed] [Google Scholar]
- 61.Mukhopadhyay P. Cleansers and their role in various dermatological disorders. Indian J Dermatol. 2011;56(1):2–6. doi: 10.4103/0019-5154.77542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zeidler C, Luling H, Dieckhofer A, Osada N, Schedel F, Steinke S, et al. Capsaicin 8% cutaneous patch: a promising treatment for brachioradial pruritus? Br J Dermatol. 2015;172(6):1669–71. doi: 10.1111/bjd.13501. [DOI] [PubMed] [Google Scholar]
- 63.Patel T, Yosipovitch G. Therapy of pruritus. Expert Opin Pharmacother. 2010;11(10):1673–82. doi: 10.1517/14656566.2010.484420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin: vehicle-controlled, double-blind, crossover study. J Am Acad Dermatol. 1995;32(2 Pt 1):287–9. doi: 10.1016/0190-9622(95)90152-3. [DOI] [PubMed] [Google Scholar]
- 65.Yosipovitch G, Maibach HI, Rowbotham MC. Effect of EMLA pre-treatment on capsaicin-induced burning and hyperalgesia. Acta Derm Venereol. 1999;79(2):118–21. doi: 10.1080/000155599750011327. [DOI] [PubMed] [Google Scholar]
- 66.Misery L, Erfan N, Castela E, Brenaut E, Lanteri-Minet M, Lacour JP, et al. Successful treatment of refractory neuropathic pruritus with capsaicin 8% patch: a bicentric retrospective study with long-term follow-up. Acta Derm Venereol. 2015;95(7):864–5. doi: 10.2340/00015555-2085. [DOI] [PubMed] [Google Scholar]
- 67.Valdes-Rodriguez R, Kaushik SB, Yosipovitch G. Transient receptor potential channels and dermatological disorders. Curr Top Med Chem. 2013;13(3):335–43. doi: 10.2174/15680266112129990090. [DOI] [PubMed] [Google Scholar]
- 68.Leslie TA, Greaves MW, Yosipovitch G. Current topical and systemic therapies for itch. Handb Exp Pharmacol. 2015;226:337–56. doi: 10.1007/978-3-662-44605-8_18. [DOI] [PubMed] [Google Scholar]
- 69.Weisshaar E, Szepietowski JC, Darsow U, Misery L, Wallengren J, Mettang T, et al. European guideline on chronic pruritus. Acta Derm Venereol. 2012;92(5):563–81. doi: 10.2340/00015555-1400. [DOI] [PubMed] [Google Scholar]
- 70.Papoiu AD, Valdes-Rodriguez R, Nattkemper LA, Chan YH, Hahn GS, Yosipovitch G. A novel topical formulation containing strontium chloride significantly reduces the intensity and duration of cowhage-induced itch. Acta Derm Venereol. 2013;93(5):520–6. doi: 10.2340/00015555-1564. [DOI] [PubMed] [Google Scholar]
- 71.Papoiu AD, Chaudhry H, Hayes EC, Chan YH, Herbst KD. TriCalm(®) hydrogel is significantly superior to 2% diphenhydramine and 1% hydrocortisone in reducing the peak intensity, duration, and overall magnitude of cowhage-induced itch. Clin Cosmet Investig Dermatol. 2015;8:223–9. doi: 10.2147/CCID.S78809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Anacor Pharmaceuticals announces positive results from phase 2 dose-ranging study of AN2728 in adolescents with atopic dermatitis. Palo Alto, California: Anacor Pharmaceuticals; 2013. Available online from: http://investor.anacor.com/releasedetail.cfm?releaseid=750026. Last accessed July 2016. [Google Scholar]
- 73.Davis MP, Frandsen JL, Walsh D, Andresen S, Taylor S. Mirtazapine for pruritus. J Pain Symptom Manage. 2003;25(3):288–91. doi: 10.1016/s0885-3924(02)00645-0. [DOI] [PubMed] [Google Scholar]
- 74.Lee JJ, Girouard SD, Carlberg VM, Mostaghimi A. Effective use of mirtazapine for refractory pruritus associated with carcinoma en cuirasse. BMJ Support Palliat Care. 2016;6(1):119–121. doi: 10.1136/bmjspcare-2014-000790. [DOI] [PubMed] [Google Scholar]
- 75.Hundley JL, Yosipovitch G. Mirtazapine for reducing nocturnal itch in patients with chronic pruritus: a pilot study. J Am Acad Dermatol. 2004;50(6):889–91. doi: 10.1016/j.jaad.2004.01.045. [DOI] [PubMed] [Google Scholar]
- 76.Mansour-Ghanaei F, Taheri A, Froutan H, Ghofrani H, Nasiri-Toosi M, Bagherzadeh AH, et al. Effect of oral naltrexone on pruritus in cholestatic patients. World J Gastroenterol. 2006;12(7):1125–8. doi: 10.3748/wjg.v12.i7.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jung SI, Seo CH, Jang K, Ham BJ, Choi IG, Kim JH, et al. Efficacy of naltrexone in the treatment of chronic refractory itching in burn patients: preliminary report of an open trial. J Burn Care Res. 2009;30(2):257–60. doi: 10.1097/BCR.0b013e318198a282. discussion 261. [DOI] [PubMed] [Google Scholar]
- 78.Peer G, Kivity S, Agami O, Fireman E, Silverberg D, Blum M, et al. Randomised crossover trial of naltrexone in uraemic pruritus. Lancet. 1996;348(9041):1552–4. doi: 10.1016/s0140-6736(96)04176-1. [DOI] [PubMed] [Google Scholar]
- 79.Pauli-Magnus C, Mikus G, Alscher DM, Kirschner T, Nagel W, Gugeler N, et al. Naltrexone does not relieve uremic pruritus: results of a randomized, double-blind, placebo-controlled crossover study. J Am Soc Nephrol. 2000;11(3):514–9. doi: 10.1681/ASN.V113514. [DOI] [PubMed] [Google Scholar]
- 80.Dawn AG, Yosipovitch G. Butorphanol for treatment of intractable pruritus. J Am Acad Dermatol. 2006;54(3):527–31. doi: 10.1016/j.jaad.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 81.Papoiu AD, Kraft RA, Coghill RC, Yosipovitch G. Butorphanol suppression of histamine itch is mediated by nucleus accumbens and septal nuclei: a pharmacological fMRI study. J Invest Dermatol. 2015;135(2):560–8. doi: 10.1038/jid.2014.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maley A, Swerlick RA. Azathioprine treatment of intractable pruritus: a retrospective review. J Am Acad Dermatol. 2015;73(3):439–43. doi: 10.1016/j.jaad.2015.05.025. [DOI] [PubMed] [Google Scholar]
- 83.Ko KC, Tominaga M, Kamata Y, Umehara Y, Matsuda H, Takahashi N, et al. Possible antipruritic mechanism of cyclosporine a in atopic dermatitis. Acta Derm Venereol. 2016;96(5):624–9. doi: 10.2340/00015555-2318. [DOI] [PubMed] [Google Scholar]
- 84.Simon D. Systemic therapy of atopic dermatitis in children and adults. Curr Probl Dermatol. 2011;41:156–64. doi: 10.1159/000323309. [DOI] [PubMed] [Google Scholar]
- 85.Beck LA, Thaci D, Hamilton JD, Graham NM, Bieber T, Rocklin R, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371(2):130–9. doi: 10.1056/NEJMoa1314768. [DOI] [PubMed] [Google Scholar]
- 86.U.S. National Institutes of Health. Clinicaltrials.gov. A study of Ustekinumab (STELARA®) in adult Japanese participants with severe atopic dermatitis. Bethesda: National Institutes of Health; 2016. Available at https://clinicaltrials.gov/ct2/show/study/NCT01945086?term=ustekinumab+atopic+dermatitis&rank= Last accessed July 2016. [Google Scholar]
- 87.Thaci D, Blauvelt A, Reich K, Tsai TF, Vanaclocha F, Kingo K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial. J Am Acad Dermatol. 2015;73(3):400–9. doi: 10.1016/j.jaad.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 88.Griffiths CE, Reich K, Lebwohl M, van de Kerkhof P, Paul C, Menter A, et al. Comparison of Ixekizumab with Etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet. 2015;386(9993):541–51. doi: 10.1016/S0140-6736(15)60125-8. [DOI] [PubMed] [Google Scholar]
- 89.Sobell JM, Foley P, Toth D, Mrowietz U, Girolomoni G, Goncalves J, et al. Effects of Apremilast on pruritus and skin discomfort/pain correlate with improvements in quality of life in patients with moderate to severe plaque psoriasis. Acta Derm Venereol. 2016;96(4):514–20. doi: 10.2340/00015555-2360. [DOI] [PubMed] [Google Scholar]
- 90.Schut C, Mollanazar NK, Kupfer J, Gieler U, Yosipovitch G. Psychological interventions in the treatment of chronic itch. Acta Derm Venereol. 2016;96(2):157–61. doi: 10.2340/00015555-2177. [DOI] [PubMed] [Google Scholar]
- 91.Sidbury R, Tom WL, Bergman JN, Cooper KD, Silverman RA, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: Section 4. Prevention of disease flares and use of adjunctive therapies and approaches. J Am Acad Dermatol. 2014;71(6):1218–33. doi: 10.1016/j.jaad.2014.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]