Abstract
The aim was to assess the efficacy of Syntometrine ® (500 micrograms ergometrine with 5 units oxytocin) as an appropriate alternative first-line uterotonic for use in elective caesarean section (CS) during a national shortage of UK-licensed IV oxytocin from April-June 2014. An observational study was performed involving 2 groups of 22 women undergoing elective CS in a UK DGH during this period. Primary endpoints included mean estimated blood loss (EBL), haemoglobin drop post-operatively and transfusion requirement. Secondary endpoints were use of antiemetics and mean post-operative nausea and vomiting (PONV) score.
Results for Syntometrine ® groups and syntocinon groups respectively: mean EBL (ml) 527.3 vs. 550.0 (p=0.5820), mean haemoglobin drop (g/dL) 0.977 vs. 0.982 (p=0.98), blood transfusion 1/22 vs. 0/22 (p=1). Intra-operative antiemetics 20/22 vs. 6/22 (p=<0.001), post-operative antiemetics 2/22 vs. 2/22 (p=1), mean PONV score 11.5 vs. 3.5 (p=0.099).
As no significant difference in primary endpoints or PONV scores was observed between regimes, we conclude Syntometrine ® was a safe first-line haemostatic agent for elective CS during oxytocin shortage.
Keywords: Drug shortages, patient safety, uterotonic, postpartum haemorrhage, post-operative nausea and vomiting
INTRODUCTION
The nonapeptide oxytocin acts on the uterine myocyte by causing release of prostaglandins leading to contraction of the uterus. It also has a role in cardiovascular regulation, as well as maternal and sexual behaviours. Major maternal adverse effects include hypotension, myocardial ischaemia, arrhythmias, nausea, vomiting, headache and flushing. Heart rate and blood pressure changes are less problematic after administration of a reduced dose of oxytocin (2 IU rather than 5IU) with no reported difference in requests for additional uterotonic agents.1
Ergometrine is a naturally occurring alkaloid, first isolated in 1932 and remains the second line intervention for atonic PPH persisting after administration of oxytocin at CS. Ergometrine causes a rapid and sustained contraction of both the pregnant and non-pregnant uterus. Its mode of action is thought to be via calcium channels or an a-receptor in the inner myometrium.2 Ergometrine causes an increase in mean arterial pressure and there are reported cases of renal and coronary artery spasm as well as myocardial infarction associated with its use. The high incidence of nausea and vomiting after the recommended 0.5 mg dose has discouraged its use as a first-line agent at CS.3
Active management of the third stage of caesarean delivery is relatively under-researched and it has been assumed that proven benefits in vaginal delivery are applicable to CS.4, 5, 6 The Royal College of Obstetricians and Gynaecologists (RCOG) recommend that oxytocin (5 IU by slow intravenous injection) should be used for women delivering by CS to reduce the frequency of post-partum haemorrhage (PPH).7 The recommendation goes on to state that Syntometrine ® (Alliance) may be used in the absence of contraindications as it reduces the risk of minor PPH but it does lead to increased reported nausea, vomiting and elevation in blood pressure.
Licensed medicine shortages are becoming a more frequent occurrence due to manufacturing and supply issues.8, 9, 10 This leads to consideration of unlicensed preparations or enforced change of perceived optimal patient management as dictated by the availability of safe alternatives. In April and May 2014 there was a UK-wide shortage of IV oxytocin (Syntocinon ®) licensed for UK use. This affected maternity departments where IV oxytocin is routinely used first-line for prevention of postpartum haemorrhage (PPH) during CS, as recommended by NICE.11 Having considered the options presented by the Department of Health,9 in our unit the protocol was changed from IV oxytocin to IM ergometrine and oxytocin (Syntometrine ® 500 micrograms ergometrine with 5 units oxytocin) as the first-line uterotonic agent in CS.
In order to assess the effect on patients of this enforced change in practice, we aimed to determine the suitability of Syntometrine ® as a first-line uterotonic agent for elective CS in terms of patient safety and outcomes. The primary endpoints of observed (operator estimated) bleeding; and secondary endpoints of post-operative nausea and vomiting and use of antiemetics were employed. These parameters were then compared to women receiving oxytocin when stocks were replenished.
METHODS
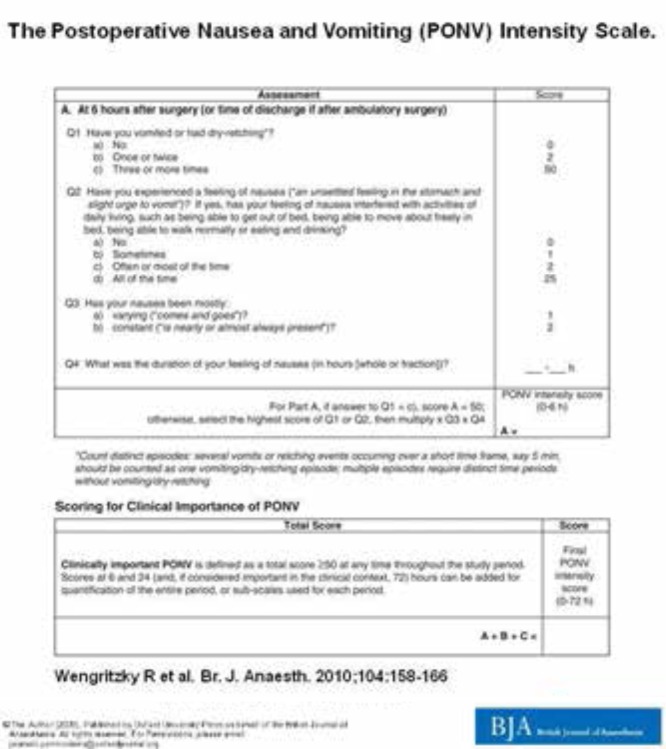
This was a prospective observational study, spanning a period of national shortage of Syntocinon ®. During the shortage period between April and May 2014, 22 women in a district general hospital underwent elective CS, facilitated by spinal anaesthesia. First-line PPH prophylaxis protocols were changed from 5 units IV oxytocin after delivery of the baby to 1ml of IM Syntometrine ® (500 micrograms ergometrine with 5 units oxytocin). Blood loss was recorded by surgeon estimated blood loss (EBL). Pre-operative and second day post-operative haemoglobin levels (g/dL) were checked, as well as any requirement for blood transfusion. Antiemetic use was recorded intra- and post-operatively. The incidence of post-operative nausea and vomiting (PONV) was recorded using a validated, standardised face-to-face questionnaire at 24 hours (Figure 1).12 Wengritzky et al. developed a validated PONV intensity scale to formally assess clinically important PONV, as defined by a score of ≥50 using this tool, as this score is associated with a poorer quality of recovery and more antiemetic use, as well as increased complications. 12 The same data was then collected for the subsequent 22 elective CSs when stocks of UK-licensed oxytocin were replenished in May and June 2014, reverting to the previous protocol for prevention of PPH as above.
Fig 1.
PONV score12 reproduced with permission from author P. Myles
Patient demographics in terms of age, BMI, parity, mode of previous deliveries, indication for CS and presence of risk factors for PPH such as placenta praevia were comparable for both groups.
Results were analysed using statistical methods to determine significance. The differences in mean estimated blood loss, post-operative haemoglobin drop and PONV scores between the Syntometrine ® and oxytocin groups were compared using t-test analysis. It was assumed that the two populations had the same variance, were normally distributed and that each value was sampled independently. Chi squared analysis was performed using a 2x2 contingency table for administration of intra-operative antiemetics.
An ethics waiver was issued by Southern Health and Social Care Trust Research and Development Committee as the work was considered as service evaluation.
RESULTS
The results in Table 1 show no significant difference in mean EBL between the Syntometrine ® and oxytocin groups, which is also reflected in a non-significant post-operative drop in haemoglobin between both groups. One woman in the Syntometrine ® group required blood transfusion during the study.
Table 1.
Observed Peri-Operative Outcomes
| Parameter | Syntometrine ® Group | Oxytocin Group | P value |
|---|---|---|---|
| Mean EBL (ml) | 527.3 | 550.0 | 0.582 |
| Mean haemoglobin drop post-operatively (g/dL) | 0.977 | 0.982 | 0.98 |
| Blood transfusion | 1/22 | 0/22 | 1 |
| Intra-operative antiemetics given | 20/22 | 6/22 | <0.001 |
| Post-operative antiemetics given | 2/22 * | 2/22 * | 1 |
| Mean 24 hour PONV score | 11.5 † | 3.5 † | 0.099 |
In the Syntometrine ® group one woman had clinically important PONV score ≥50; in the oxytocin group no women had clinically important PONV score ≥50
In the Syntometrine ® group four women had clinically important PONV score ≥50; in the oxytocin group one woman had clinically important PONV score ≥50
In terms of antiemetic use, significantly more women administered Syntometrine ® received intra-operative antiemetics. There was no statistically significant difference in PONV scoring between groups, or clinically important PONV as defined by a score ≥50 using the validated tool.
In order to ascertain the financial implications of changing CS protocols in favour of Syntometrine ® during the oxytocin shortage, the costs of the standard doses of oxytocin and Syntometrine ® as well as the type, route and number of doses of each antiemetic received by women in both groups during the study period were analysed.13 The total costs were then used to work out a mean cost per patient of uterotonic plus antiemetics for each group, as summarised in Table 2. This demonstrates a statistically significantly increased cost associated with changing protocols, due to the combined increased antiemetic use and the increased cost of Syntometrine ®.
Table 2.
Cost Analysis of Syntometrine ® vs Oxytocin
| Syntometrine ® Group | Oxytocin Group | P value | |
|---|---|---|---|
| Cost of uterotonic per patient | £ 1.31 | £ 0.89 | <0.0001 |
| No of patients receiving antiemetic during study | 20/22 | 8/22 | 0.0006 |
| Cost of antiemetics (total) | £249.38 | £76.20 | <0.0001 |
| Overall mean cost per patient (uterotonic+ antiemetics) | £12.65 | £4.35 | <0.0001 |
DISCUSSION
Patient safety had been a legitimate concern when news of the oxytocin shortage came to light. There was little notice of the supply issue and a change of practice had to be implemented with almost immediate effect.
Our data show that Syntometrine ® is a suitable alternative to oxytocin as a uterotonic for use in elective CS in terms of blood loss, haemoglobin drop and transfusion requirement. Available study (syntocinon) patients during this time were limited due to the opportunistic nature of the project and the fact that the control (syntometrine) group was matched 1:1. This left little scope to alter the sample sizes analysed. Although post-hoc power calculation has received criticism as a method for interpreting negative study results14, our study had 75% power to detect a statistically significant difference in mean estimated blood loss. Further reassurance regarding statistical validity of the project rests in the narrow 95% confidence limits reported (527ml +/- 24ml for the syntometrine group and 550ml +/- 33ml for the syntocinon group).
Intra-operative antiemetic was given more frequently to women who received Syntometrine ® compared to oxytocin, though there was no difference in clinically significant PONV scores.
The studies from which the Royal College of Obstetricians and Gynaecologists (RCOG) and NICE have based their guidelines on management of PPH and CS have consistently established that Syntometrine ® is as effective as IV oxytocin (5IU or 10IU) in preventing PPH >1000ml.7, 11 In fact, the Cochrane review referenced by the RCOG guideline states that there is a greater risk reduction of PPH for the definition of blood loss > 500ml, with Syntometrine ® versus IV oxytocin.15 The widely reported increase in unpleasant side-effects of nausea and vomiting with Syntometrine ® compared with oxytocin alone are derived from the same studies, but exhibit considerable heterogeneity in reporting of these symptoms.15 When examined in greater detail, the methods of reporting such symptoms are sub-optimal, with no validated tools used to score PONV.16 While our study involved a small number of patients, it does use a validated tool for assessing PONV, lending weight to the results. The Syntometrine ® group received significantly more intra-operative antiemetics. It is impossible to say if this was in response to reported symptoms, or merely reflective of an attempt by the anaesthetist to mitigate against predicted problems. It is noteworthy that the Oxford Handbook of Anaesthesia recommends prophylactic antiemetic when giving Syntometrine ®. 17
The practice of giving antiemetic along with ergometrine is also re-enforced in training manuals / protocols in UK obstetric departments. 18 The 2004 Cochrane review15 concluded that there was an increased rate of nausea and vomiting with Syntometrine ® – although the PONV scores were generally not using validated tools. The increased use of antiemetics therefore seems engrained in practice and needs to be factored into any economic cost calculation for syntometrine vs. syntocinon. As a result, it is impossible to accurately compare PONV rates between the two drugs due to the presence of bias. This is a clinical bias however, and it now would be unethical (based on well-established data that there is a 4 to 7 fold increase in nausea / vomiting) to withhold antiemetics in the syntometrine group of patients for research or cost reasons.
In the setting of increasingly frequent international drug shortages it is important to have contingency protocols in place. Supply chain issues can be unpredictable and there may be no reliable estimates of the duration of the shortage. In this particular case, there were additional concerns - existing stocks of oxytocin were reserved for circumstances where no alternative exists, e.g., augmentation of labour and for emergencies such as massive PPH.
The effectiveness of Syntometrine ® at preventing PPH at CS - without significantly increased side-effects - raises the possibility of using Syntometrine ® for elective cases where increased blood loss would be expected; for example placenta praevia. The cost issues would make it prohibitive for regular use however, due to the increased use of antiemetics.
We conclude that in the setting of a UK-wide shortage of IV oxytocin, Syntometrine ® is an appropriate safe alternative for first-line prevention of PPH at elective CS. It provides equal haemostasis. There was no significant increase in patient reported post-operative nausea and vomiting. Significantly more intra-operative antiemetic use was observed, though it is unclear if this was due to actual intra-operative nausea and vomiting, or merely reflective of a more aggressive prophylactic approach to antiemesis.
It can also be concluded that patient safety did not appear to be compromised when a shortage of oxytocin mandated the use of Syntometrine ® as an alternative for elective CS. However, the higher cost of Syntometrine ®, combined with the increased use of intra-operative antiemetics, suggests that this particular drug shortage may have had a significant financial consequence for the NHS.
REFERENCES
- 1.Sartain JB, Barry JJ, Howat PW, McCormack DI, Bryant M. Intravenous oxytocin bolus of 2 units is superior to 5 units during elective CS. Br J Anaest. 2008;101(6):822–6. doi: 10.1093/bja/aen273. [DOI] [PubMed] [Google Scholar]
- 2.Dyer RA, van Dyk D, Dresner A. The use of uterotonic drugs during CS. Int J Obstet Anesth. 2010;19(3):313–9. doi: 10.1016/j.ijoa.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 3.Balki M, Carvalho JC. Intraoperative nausea and vomiting during cesarean section under regional anesthesia. Int J Obstet Anesth. 2005;14(3):230–41. doi: 10.1016/j.ijoa.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Murphy J, Carey M, Montgomery AA, Sheehan S, ECSSIT Study Group Study Protocol. ECSSIT – Elective CS Syntocinon® Infusion Trial. A multi-centre randomised controlled trial of oxytocin (Syntocinon®) 5 IU bolus and placebo infusion versus oxytocin 5 IU bolus and 40 IU infusion for the control of blood loss at elective CS. BMC Pregnancy Childbirth. 2009;9:36. doi: 10.1186/1471-2393-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lokugamage AU, Paine M, Bassaw-Balroop K, Sullivan KR, Rafaey HE, Rodeck CH. Active management of the third stage at CS: a randomised controlled trial of misoprostol versus syntocinon. Aus NZ J Obstet Gynaecol. 2001;41(4):411–4. doi: 10.1111/j.1479-828x.2001.tb01319.x. [DOI] [PubMed] [Google Scholar]
- 6.Munn MB, Owen J, Vincent R, Wakefield M, Cheshunt DH, Hauth JC. Comparison of two oxytocin regimens to prevent uterine atony at caesarean delivery: a randomized controlled trial. Obstet Gynecol. 2001;98(3):386–90. doi: 10.1016/s0029-7844(01)01479-x. [DOI] [PubMed] [Google Scholar]
- 7.Royal College of Obstetricians and Gynaecologists . Postpartum Haemorrhage, Prevention and management. (Green-top Guideline No. 52) London: Royal College of Obstetricians and Gynaecologists; 2009. [Google Scholar]
- 8.European Association of Hospital Pharmacists. Medicines shortages in European hospitals: the evidence and case for action. London: EAHP; 2014. [Google Scholar]
- 9.NHS. Shortage of oxytocin (Syntocinon) injection. London: Department of Health; 2014. East & South East England Specialist Pharmacy Services. Medicines Information Division. Drug Discontinuation. Shortage of Supply Memos. [Google Scholar]
- 10.American Society of Health System Pharmacists. Bulletin 876. Oxytocin injection [24 May 2016] Bethesda, Maryland: ASHP; 2016. Drug Shortages. Current shortages. [Google Scholar]
- 11.NICE Clinical Guideline; 132. CS. London: National Institute for Health and Care Excellence; 2011. [Google Scholar]
- 12.Wengritzky R, Mettho T, Myles PS, Burke J, Kakos A. Development and validation of a postoperative nausea and vomiting intensity scale. British Journal of Anaesthesia. 2010 Feb;104(2):158–166. doi: 10.1093/bja/aep370. [DOI] [PubMed] [Google Scholar]
- 13.British Medical Association. British National Formulary No. 62: Oxytocin. London: BMJ Group and RPS Publishing; 2011. Royal Pharmaceutical Society of Great Britain. [Google Scholar]
- 14.Levine M, Ensom MH. Post-hoc power analysis; an idea whose time has passed? Pharmacotherapy. 2001;21(4):405–9. doi: 10.1592/phco.21.5.405.34503. [DOI] [PubMed] [Google Scholar]
- 15.McDonald SJ, Abbott JM, Higgins SP. Prophylactic ergometrine oxytocin versus oxytocin for the third stage of labour. Cochrane Database Systematic Reviews. 2004 doi: 10.1002/14651858.CD000201.pub2. Issue 1. Art No. CD000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choy CM, Lau WC, Tam WH, Yuen PM. A randomised controlled trial of intramuscular syntometrine and intravenous oxytocin in the management of the third stage of labour. BJOG. 2002;109(2):173–7. doi: 10.1111/j.1471-0528.2002.01204.x. [DOI] [PubMed] [Google Scholar]
- 17.Allman K, Wilson I. Oxford Handbook of Anaesthesia. 4th ed. Oxford: Oxford University Press; 2016. [Google Scholar]
- 18.NHS Networks (UK) Postpartum haemorrhage, PPH 2013–15. NHS Networks [internet] 2015. Available online from: https://www.networks.nhs.uk/nhs-networks/staffordshire-shropshire-and-black-country/documents/Postpartum%20Haemorrhage%202013.pdf. Last accessed July 2016.