Abstract
Background
The Regulation and Quality Improvement Authority (RQIA) monitors the administration of electroconvulsive therapy (ECT) in Northern Ireland (NI). As part of their inspection methodology RQIA wished to include feedback from ECT patients. The aim of this report is to summarise the opinions of ECT patients over a 1-year period and to compare their feedback about treatment with the standards of best practice, as defined by the Electroconvulsive Therapy Accreditation Service (ECTAS).
Method
RQIA was granted permission to use the ECTAS patient questionnaire. The questionnaire was distributed to all the ECT clinics in NI and staff were requested to give them to patients who had received a course of ECT.
Results
A total of 42 individuals returned questionnaires, 24 females (57.1%) and 18 (42.9%) males. The response rate was 26%. Almost half of respondents were detained under the Mental Health (Northern Ireland) Order 1986 (n=19, 45.2%), with one third receiving ECT as a day patient (n=14, 33.3%). Respondents reported having detailed information about ECT, with ECTAS standards 4.2 and 4.3 being affirmed in over 80% of cases. Eighty percent of respondents (n=34) believed they benefited from ECT.
Conclusion
The results are mainly favourable towards ECT. The majority felt they benefited from treatment.
Keywords: Electroconvulsive Therapy, User Experience/User Satisfaction, Semi-Structured Interview, Qualitative, Regulation and Quality Improvement Authority, Northern Ireland
INTRODUCTION
In 2012, the Regulation and Quality Improvement Authority1 (RQIA), Northern Ireland’s (NI) independent health and social care regulator, undertook a review of the practice of Electroconvulsive Therapy (ECT). RQIA used information from the Electroconvulsive Therapy Accreditation Service2 (ECTAS) to formulate their methodology. ECTAS was set up in England in 2003 by the Royal College of Psychiatrists with the aim of improving the quality of the administration of ECT within the United Kingdom (UK) through a process of assessment and accreditation with an established set of standards.
Despite 70 years of existence and substantial proof of efficacy, ECT still continues to be one of the most controversial and misunderstood treatments in medicine3. Convulsive therapy was first introduced in 1934 by Meduna, who believed schizophrenia and epilepsy were antagonistic disorders. He treated patients with chemically-induced seizures. In 1938 Cerletti, an Italian neurologist, successfully treated a patient with electrically-induced seizures and this form of treatment soon replaced chemically-induced seizures.
ECT was originally given “unmodified”, i.e., without anaesthesia or muscle relaxants. By the end of the 1950s most hospitals in the UK used “modified” ECT to avoid the serious complications of bone fracture or dislocation. The use of ECT spread throughout the world and was common in UK psychiatric practice during the 1960s and early 1970s. At that time, there began some professional and public disquiet over some aspects of its use.
The use of ECT in the UK has been steadily declining since 19854 due to the increasing use of effective pharmacotherapy for severe mental disorders. Over the years, many sets of guidelines have been produced by the National Health Service (NHS), the Royal College of Psychiatrists and the National Institute for Care and Excellence to improve standards of administration of ECT. In parallel, the main indication for ECT transformed from first-line to last-resort treatment for medication-resistant and very severe life-threatening conditions. Despite the improvement in all aspects of the delivery of ECT, considerable stigma still surrounds it which undermines public acceptance.
ECT is a safe and effective short-term treatment of depression5 and other severe psychiatric conditions. In NI it is currently administered to approximately 6 per 100,000 of the general population per year6. Recently, a number of reviews have summarised the available literature on patients’ experience of ECT3, 7; however there have been no published studies of local experience.
METHOD
RQIA obtained approval from ECTAS to adapt its patient questionnaire2 for the purposes of this study. The 32 questions contained in the questionnaire assess demographic details, information given about ECT, consent process, quality of care, side-effects and effectiveness. Questionnaires were distributed by the 7 clinical teams providing ECT within the 5 trusts in NI to patients who had received ECT. These were completed anonymously and returned directly to the RQIA office in Belfast. RQIA provided a stamped addressed envelope to make it easier for respondents.
The data was analysed quantitatively and responses were compared with ECTAS standards for the administration of ECT. The qualitative data was analysed thematically.
An analysis was also carried out, using Fisher’s Exact Test, to determine if there were any statistically significant differences between the voluntary group and the detained group of respondents.
RESULTS
A total of 163 patients received ECT in NI between 1 July 2013 and 30 June 2014 and 42 questionnaires were returned giving a response rate of 26%. The ages of the respondents ranged from 37 to 76 years, with a mean of 57 years. More females (n=24, 57.1%) than males (n=18, 42.9%) responded. Almost half of respondents (n=19, 45.2%) were detained under the Mental Health (Northern Ireland) Order 1986 (the Order), with one third (n=14, 33.3%) receiving ECT as a day patient. The majority (n=32, 76.2%) responded to the questionnaire within 6 months of receiving ECT.
Information offered prior to ECT
Almost all respondents indicated that they recall speaking to their doctor before having ECT (n=38, 90.4%); 80.9% (n=34) reported that they were given information about what would happen during ECT; 83.3% (n=35) reported receiving information about why they were having ECT and 83.3% (n=35) reported receiving information about what ECT was likely to do for them. Approximately two thirds of respondents (n=27, 64.3%) received information on side-effects and problems with ECT. Half of the respondents reported receiving information on alternative treatments (n=21, 50%) and information on what would happen if they did not have ECT (n=24, 57.1%). Two thirds of respondents (n=28, 66.7%) recall receiving written information on ECT.
Patient satisfaction with the information they received
The questionnaire invited open comments about how information about ECT could be improved. Of the 26 respondents who provided comment over half (n=16, 61.5%) were satisfied with the information that was given to them. Two respondents (n=2, 7.7%) requested further information on side-effects, while other individuals requested information about appropriate attire for the procedure and an opportunity to speak with those who had had successful treatment with ECT.
Quality of the therapeutic relationship with staff
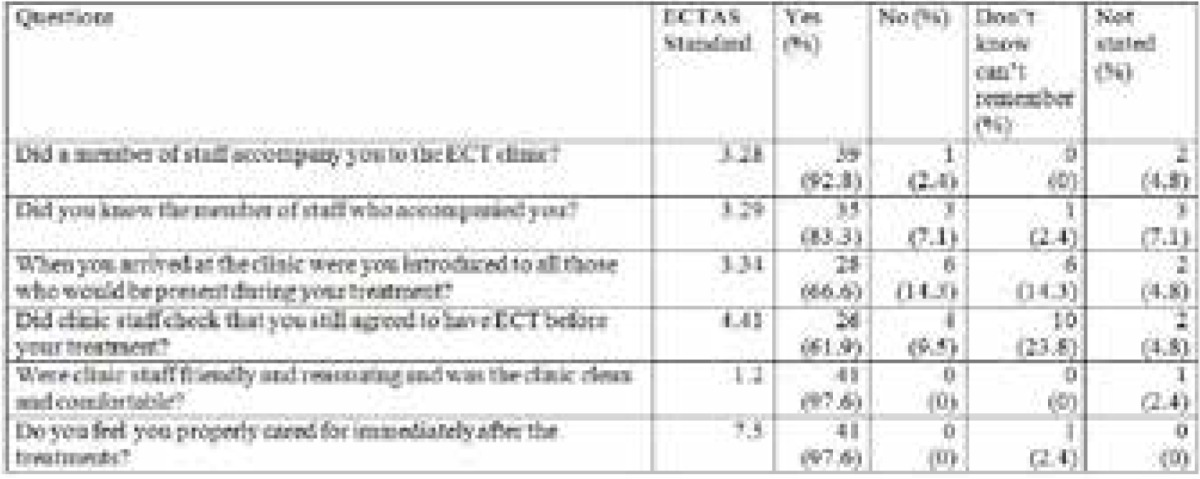
This study reports that a majority of respondents had a positive relationship with the staff involved in their care. They recalled being accompanied by a staff member to the ECT clinic (n=39, 92.9%); knowing this member of staff (n=35, 83.3%); being introduced to all those present in the theatre (n=28, 66.6%); and the same member of staff being present when they awoke (n=33, 78.6%). Almost all respondents agreed staff were friendly and reassuring and were satisfied the ECT clinic was clean and comfortable (n= 41, 97.6%) and recall being cared for immediately after having ECT (n=41, 97.6%).
Quality of care
Respondents were given the opportunity to provide open comments about the quality of care they felt they received. Twenty-one respondents commented. Almost three-quarters (n=15, 71.4%) stated the care was of the highest quality or could not be better; three (14.3%) found the care satisfactory; and two (9.5%) commented on the professional and competent nature of the staff. No negative comments about the quality of care were received.
The Consent Process
A majority of respondents (n=32, 76.2%) stated they had enough time to discuss their decision to have ECT with a doctor independently. Two-thirds (n=27, 64.3%) agreed to have ECT and recalled signing the consent form; twelve (28.6%) either did not know or did not state whether they signed a consent form and three (7.1%) did not recall signing a consent form. There were nineteen respondents (45.2%) who recalled having ECT as a detained patient, 15 of whom reported that they said to their doctor that they agreed to have the treatment. Whilst the majority recalled their consent for ECT being confirmed immediately prior to ECT, 12 (28.6%) either did not know or did not state whether they provided consent to treatment and 4 (9.5%) recalled that their consent was not checked.
In response to the question “Did you feel pressurised or forced to have ECT” 4 respondents (9.5%) affirmed that they did feel pressurised, 2 from the voluntary group and 2 from the detained group.
Of the respondents who provided open comments on the consent process, 14 (77.8%) were satisfied with the consent process; 2 respondents (11.1%) commented about feeling coerced and one (5.5%) stated it was a family decision.
Side-effects
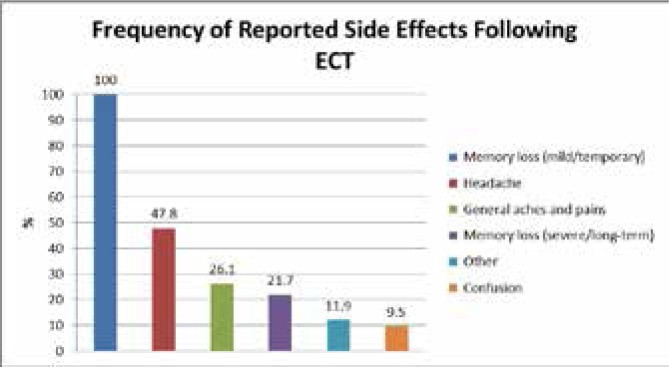
Approximately half of the respondents (n=23, 54.8%) reported side-effects with around one quarter (n=11, 26.2%) reporting no side-effects and fewer respondents (n=8, 19%) either not knowing or not stating. Of the 23 respondents reporting side-effects, all reported mild or temporary memory loss and 5 (21.7%) reported severe or long term memory loss. Memory loss was also the most frequent side-effect commented upon in the open question relating to side-effects (n=14, 63.3%). Graph 1 tabulates the frequency of reported side-effects.
Graph 1.
Frequency of Reported Side effects Following ECT
Patient Attitudes
Over four-fifths of respondents (n=34, 80.9%) said ECT was beneficial to them, 3 respondents (7.1%) stated it was not beneficial and 5 respondents (11.9%) either did not know or did not state. The qualitative results from the study reflects a highly confident view of ECT with 17 of the 18 comments portraying a positive view of the personal efficacy of ECT and 15 out of 21 commenting on the high quality of care.
Respondents were asked to comment on how their experience of ECT could be improved. The majority of respondents (n=29, 69%) did not provide any specific comment in this section, a small number (n=8, 19%) stated that their care was excellent and could not be improved, 4 respondents (9.5%) suggested “not having to travel” would be an improvement and one respondent (2.4%) commented that there were too many “consultations”.
Comparison of voluntary and detained groups of respondents
When the group of 16 voluntary respondents were compared with the group of 19 detained respondents (7 respondents did not give their status) it was found that the voluntary group were statistically significantly younger (p=0.002). There was no significant difference with regard to gender (p=0.841). The voluntary group were statistically significantly more able to recall the information given about problems and side-effects associated with ECT (p=0.010). Four respondents (11%), 2 from the voluntary group and 2 from the detained group admitted feeling pressurised to have ECT. Statistically, there no differences between the groups with regard to feeling pressurised to have the treatment (p=0.859). Almost all respondents in both groups felt that ECT helped them.
ECTAS standards
In relation to the information offered to patients about ECT (Table 1) when the responses obtained from the questionnaire were compared with key ECTAS standards over 80% of respondents affirmed 2 out of 6 standards as having been met. All 6 standards were met by 50% of respondents.
Table 1.
Questions asked, ECTAS standards and quantitative results for information offered to patients prior to ECT
| Questions | ECTAS Standards | Yes | No | Don’t know Can’t remember | Not |
|---|---|---|---|---|---|
| Were you given information about what would happen during the treatment? | 4.2 | 34 (81) |
1 (2.4) |
4 (9.5) |
3 (7.1) |
| Were you given information about why you were having ECT? | 4.3 | 35 (83.3) |
1 (2.4) |
2 (4.8) |
4 (9.5) |
| Were you given information about what ECT was likely to do for you? | 4.3 | 35 (83.3) |
1 (2.4) |
3 (7.1) |
3 (7.1) |
| Were you given information about problems and side effects? | 4.4 | 27 (64.3) |
10 (23.8) |
3 (7.1) |
2 (4.8) |
| Were you given information about other treatments you could have instead? | 4.6 | 21 (50) |
12 (28.6) |
7 (16.7) |
2 (4.8) |
| Were you given information about what would happen if you didn’t have ECT? | 4.5 | 24 (57.1) |
7 (16.7) |
8 (19.1) |
3 (7.1) |
| Did you receive any written information on ECT? | 4.11 | 29 (69) |
6 14.3 |
5 11.9 |
2 4.8 |
In relation to the quality of care (Table 2) over 80% of respondents affirmed 4 out of 6 standards. All 6 standards were affirmed by over 60% of respondents.
Table 2.
Questions asked, ECTAS standards and quantitative results for quality of care.
DISCUSSION
Strengths and weaknesses
The main strength of this study was its use of a national questionnaire developed by ECTAS to examine patient experience when assessing ECT centres in England and Wales for accreditation. The clinical teams administering ECT in NI were asked to invite all patients who had received a course of ECT to complete the questionnaire in order to obtain a representative sample. A further strength was that patients were made aware that their responses were anonymous.
The main limitation of the study is the low response rate of 26%. Although measures were put in place to try to maximise the response rate, RQIA were only indirectly involved in the administration of the questionnaires in order to preserve anonymity and were unable to do a re-mailing of the questionnaire. We cannot therefore be sure that all patients received the questionnaire. More active outreach to the ECT clinics might have increased response rate. The fact that ECT is often used for severely depressed patients who may have a degree of cognitive impairment could also have been a factor.
Main findings
Our response rate of 26% compares with 37% in a large study of patients attending ECTAS accredited clinics and a 57% response rate in an Irish ECT clinic.8, 9 Gathering the views of a representative sample of patients is challenging for organisations not directly providing clinical care. Coulter et al refer to surveys on patient experience by the NHS in England which have response rates similar to ours and found a falling response rate to postal surveys, suggesting an element of “survey fatigue”10.
Demographic analysis of our sample corresponds with the annual trend1 in NI for more females (67%) than males to receive ECT. The mean age of our respondents is also similar to the mean age of patients receiving ECT here. While our sample was not representative in terms of location or detained/voluntary/day patient status, it did contain patients who received their ECT under all of these circumstances.
The majority of respondents reported receiving general information about ECT. However, information about alternative treatments, possible outcomes if ECT was not given and side effects received lower ratings and were either less well recalled or were perhaps not always included in the discussions with doctors. Similar percentages recall receiving written information on ECT in our study and the study by Rush et al9; 69% and 68% respectively. The importance of detailed discussions with patients and their families, supported by written information in a patient-appropriate form, should be emphasised to clinicians.
Overall, with regard to the consent procedures, the majority of respondents felt they had time to discuss their decision with their doctor and were satisfied with the consent procedures. Again, the majority of respondents reported a good therapeutic relationship with staff (Table 2). The question with the fewest positive responses related to the recall of whether consent to ECT was checked immediately prior to the treatment. Difficulty with recall may be partly due to a degree of retrograde amnesia caused by the procedure.
Myers11 found refusal of or agreement to ECT on sufferance was linked to an unfavourable view of ECT so it was expected that patients in this study who were treated under the Order would have had a less favourable view. In fact, there were no differences between voluntary and detained groups when considering factors related to quality of care or the beneficial nature of treatment. Neither were there differences between groups with regard to feeling pressurised to have ECT. Of the 4 respondents who felt pressurised to have ECT, 2 were actually from the voluntary group. Therefore, it is likely that influences from sources other than detention under the Order can contribute to patients feeling under pressure to consent.
Clinicians may inadvertently put pressure on patients during discussions about treatment or patients may feel under obligation to accept the treatment being offered. One respondent commented that the decision to have treatment was made by the family.
This study revealed a relatively low level of perceived coercion by respondents (one tenth). The Irish study by Rush et al9 reported an even lower level of perceived coercion in contrast to others who reported coercion rates among respondents of about one fifth to one third. 3, 12
Chakrabarti et al3 reported that on average 2/3 of their patients reported adverse effects following ECT: roughly 60% in their review reported memory problems and in about 40%, this persisted from several weeks to several years. Philpott et al13 found that 45% of their patients reported persistent memory loss. In our study, 50% of the respondents reported side-effects and 21.7% reported long term memory loss. Whether ECT results in long-term changes in memory performance is a controversial issue14 which has not yet been resolved with any certainty. It is, therefore, important that clinicians attend to cognitive factors when recommending ECT and employ strategies within the treatment regime that minimise possible longer term effect on cognitive function.
Although some consider ECT to be effective and potentially life-saving, others regard it as harmful and campaign energetically for it to be banned15. An extensive review of the literature on the attitudes of patients to ECT by Chakrabarti et al3 found evidence that the vast majority of patients perceived ECT to be helpful and had positive views regarding treatment. In our study, 4/5 of respondents felt ECT was beneficial. The majority of open comments referred to the high quality of care received and a small number stated that their experience of ECT could not be improved. Not having to travel long distances for ECT was suggested as an improvement and this should be taken into account by those responsible for planning services.
Kershaw et al8 reported that the anxiety of patients having ECT may be reduced by personal attention and reassurance from clinical staff known to the patient. The importance of the continuity of staff accompanying the patient on the journey through ECT should be stressed.
Bias
Reliable interpretation of survey data depends on having full information about the survey population, the sample obtained and a high response rate10. Our study does not have a detailed profile of responders and non-responders and produced a relatively low response rate which carries a risk of producing bias. A further bias may be due an over representation of day patients amongst respondents who may have had a more positive attitude as they did not have to experience hospitalisation or may have been less ill than in-patients.
Memory loss, which is a frequent side effect of ECT, may have impacted on an individual’s ability to accurately recall the information sought by the questionnaire and may have been reflected in the number of “don’t know/can’t remember” or “not stated” replies. In light of the positive findings of our study, it is possible that patients whose attitude was more favourable towards ECT were more likely to return our questionnaire.
CONCLUSION
Although the majority of respondents were satisfied with the quality of care that they received, not all the selected ECTAS standards were affirmed by the respondents in this study.
REFLECTIONS ON THE PAST
There is no doubt that when senior psychiatrists reflect on the use of ECT, they feel that it was over-used in the 1960s and 1970s but it is important to understand that the range of treatment options was much lower at that time. During a session of ECT, up to 10 in-patients and 30 out-patients may have received ECT whereas now it is unusual to have more than 3 or 4 patients receiving ECT per session. Today, due to the stigma, ECT may in fact be under-used and patients whose depressive conditions could respond to ECT remain unwell despite high doses of medication. Standards of administration of ECT have certainly risen and the technical aspects of treatment have improved to achieve optimal clinical outcomes whilst minimising side-effects. Most psychiatrists would wish to retain the option of giving ECT and would hold the opinion that, in the severely depressed or suicidal patient, it is a life-saving treatment. When applied appropriately, the outcome of its use is very favourable in the short term but measures, including medication, must be put in place for the patient to maintain their recovery.
FUTURE CONSIDERATIONS
Two ECT suites in Northern Ireland have ECTAS accreditation and RQIA will continue to encourage the five other suites to apply for accreditation. RQIA will also seek to improve the patient journey through this treatment by continuing to monitor and inspect ECT services.
LEARNING POINTS
If appropriate, information about alternative treatments and the consequences of not having ECT should be discussed and recorded
If appropriate, consent to ECT should be sought prior to each treatment and recorded
The issue of perceived coercion merits further study.
Clinicians must take steps to minimise cognitive side-effects and monitor cognition with standardised tests
Distance to reach the ECT clinic and opportunities to meet those previously treated with ECT should be considered by those planning services
Continuity of nursing staff accompanying the patient through ECT should be ensured
The authors have no conflct of interest.
ACKNOWLEDGEMENTS
We would like to thank Mike Stevenson, Department of Statistics, Queen’s University, Belfast, for the statistical analysis, Professor R Murray and Dr Judy Laing, University of Bristol, Professor R McClelland and Dr C Kelly for their helpful contribution and Claire Henry for her secretarial support.
REFERENCES
- 1.RQIA Report on the review of electroconvulsive therapy in Bluestone Unit, Craigavon Area Hospital. Belfast: Regulation and Quality Improvement Authority (RQIA); 2013. Available from: http://www.rqia.org.uk/cms_resources/Craigavon%20Area%20Hospital,%20SHSCT%20-%203%20December%202013.pdf. Last accessed May 2016. [Google Scholar]
- 2.Buley N, Hailey E, Hodge S. ECT accreditation service (ECTAS): standards for the administration of ECT. 13th ed. London: Royal College of Psychiatrists; 2016. Available from: http://www.rcpsych.ac.uk/workinpsychiatry/qualityimprovement/ccqiprojects/ectclinics/ectas/ectasstandards.aspx. Last accessed May 2016. [Google Scholar]
- 3.Chakrabarti S, Grover S, Rajagopal R. Electroconvulsive therapy: a review of knowledge, experience and attitudes of patients concerning the treatment. World J Biol Psychiatry. 2010;11(3):525–37. doi: 10.3109/15622970903559925. [DOI] [PubMed] [Google Scholar]
- 4.Eranti SV, McLoughlin DM. Electroconvulsive therapy – state of the art. Br J Psychiatry. 2003;182(1):8. doi: 10.1192/bjp.182.1.8. [DOI] [PubMed] [Google Scholar]
- 5.UK ECT Review Group. Efficacy and safety of electro-convulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361(9360):799–808. doi: 10.1016/S0140-6736(03)12705-5. [DOI] [PubMed] [Google Scholar]
- 6.Rea S, Convery P. Report on the administration of electroconvulsive therapy in Northern Ireland. Belfast: Regulation and Quality Improvement Authority (RQIA); 2014. Available from: http://www.rqia.org.uk/cms_resources/ECT%20Report%202013_14.pdf. Last accessed May 2016. [Google Scholar]
- 7.Rose D, Fleischmann P, Wykes T, Leese M, Bindman J. Patients’ perspectives on electroconvulsive therapy: systematic review. Brit Med J. 2003;326(7403):1363. doi: 10.1136/bmj.326.7403.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kershaw K, Rayner L, Chaplin R. Patients’ views on the quality of care when receiving electroconvulsive therapy. Br J Psych Bull. 2007;31(11):414–7. [Google Scholar]
- 9.Rush G, McCarron S, Lucey J V. Consent to ECT: patients’ experiences in an Irish ECT clinic. Br J Psych Bull. 2008;32(1):15–7. [Google Scholar]
- 10.Coulter A, Locock L, Ziebland S, Calabrese J. Collecting data on patient experience is not enough: they must be used to improve care. Brit Med J. 2014;348:g2225. doi: 10.1136/bmj.g2225. [DOI] [PubMed] [Google Scholar]
- 11.Myers DH. A questionnaire study of patients’ experience of electroconvulsive therapy. J ECT. 2007;23(3):169–74. doi: 10.1097/yct.0b013e318093eecb0. [DOI] [PubMed] [Google Scholar]
- 12.Rose DS, Wykes TH, Bindman JP, Fleischmann PS. Information, consent and perceived coercion: patients’ perspectives on electroconvulsive therapy. Brit J Psychiatry. 2005;186(1):54–9. doi: 10.1192/bjp.186.1.54. [DOI] [PubMed] [Google Scholar]
- 13.Philpot M, Collins C, Trivedi P, Treloar A, Gallacher S, Rose D. Eliciting users’ views of ECT in two mental health trusts with a user-designed questionnaire. J Ment Health. 2004;13(4):403–13. [Google Scholar]
- 14.MacQueen G, Parkin C, Marriott M, Begin H, Hasey G. The long-term impact of treatment with electroconvulsive therapy on discrete memory systems in patients with bipolar disorder. J Psychiatry Neurosci. 2007;32(4):241–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Carney S, Geddes J. Electroconvulsive therapy. Brit Med J. 2003;326(7403):1343–4. doi: 10.1136/bmj.326.7403.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]